-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Nanolaser in cataract surgery and its impact on corneal endotelium
Authors: T. Juhás; T. Juhás ml.
Authors place of work: Očná klinika OFTUM, Košice, Prednosta: prof. MUDr. Tomáš Juhás, DrSc.
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 5, p. 268-271
Category: Původní práce
doi: https://doi.org/10.31348/2019/5/4Summary
Purpose: To compare safety and efficacy of new nanolaser photofragmentation technique with standard ultrasound phacoemulsification cataract surgery technique.
Metods: A group of 20 patients - 40 eyes who underwent bilateral cataract surgery, one eye with ultrasound phacoemulsification (group I), n = 20 fellow eye with nanosecond laser framentation (group II ). Lens Opacities Classification System III was used to classify cataract stage. All 40 eyes had stage III cataract, Nucleus Opalescence was NO2 – NO3. Uncorrected visual acuity (UCVA), endothelial cells density (DEC), hexagonal cells rate, index of endothelial cells pleomorfism, and corneal thickness were evaluated prior to surgery and at day 7 follow up.
Results: All 40 eyes had uneventful surgery,without complications. Preoperative UCVA in group I was 0,70±0,07 and 0,68 ± 0,10 in group II. At follow up check 7 days after surgery UCVA was 0,98 ± 0,05 in group 1 and 0,98 ± 0,04 in group II (p-NS). The mean DEC (cells/mm2) before surgery was 2508 ± 205,54 in group 1 and 2472 ± 287,85 in group II. After surgery density decreased to 2024,92±271,50 in group 1 and 2138,5 ± 390,85 in group II. Difference in endothelial cells decrease between groups showed no statistical significance. There was no statistical significance in differences of hexagonal cells rate and corneal thickness between both groups pre and postoperatively.
Conclusion: Nanolaser lens photofragmentation and ultrasound phacoemulsification can be considered equal regarding impact on endothelial cells.
Keywords:
chirurgia katarakty – ultrazvuková fakoemulzifikácia – nanolaserová fotofragmentácia – endoteliáne bunky
Introduction
Cataract surgery is one of the most frequently performed operations worldwide. The method and techniques of the operation have undergone intensive development up to today’s standard stage of ultrasound phacoemulsification and implantation of various types of intraocular lenses.
Despite the sophisticated phacoemulsification technique, there is still an endeavour to improve the process. For example, to minimise the surgical trauma, improve perioperative intraocular stability, perfect intraocular lenses and so on.
The adverse effect of ultrasound on the ocular structures and its contribution to the onset of endothelopathy and cystoid macular edema is well known. The cause of these complications is not only the time, intensity of ultrasonic energy, mechanical and thermal damage upon phacoemulsification, but also the state of the cornea, hardness of the lens nucleus, axial length, traumatisation of the eye, experience of the surgeon and quality of the used material, such as viscomaterial.
This study compares the density of endothelial cells, their morphology and corneal thickness before and after surgery in two groups of operated-on eyes: in group I following ultrasound phacoemulsification and group II following nanolaser lens photofragmentation.
The use of laser energy for phacolysis of the human lens has been known for almost 30 years. Neodymium: YAG laser was first experimentally used in 1990 by Dodick (5). The technique was perfected up to the development of the commercially available nanosecond Cetus laser (Fig. 1).
Fig. 1. Nanolaser Cetus ARC Laser GmbH, Erlangen, Germany 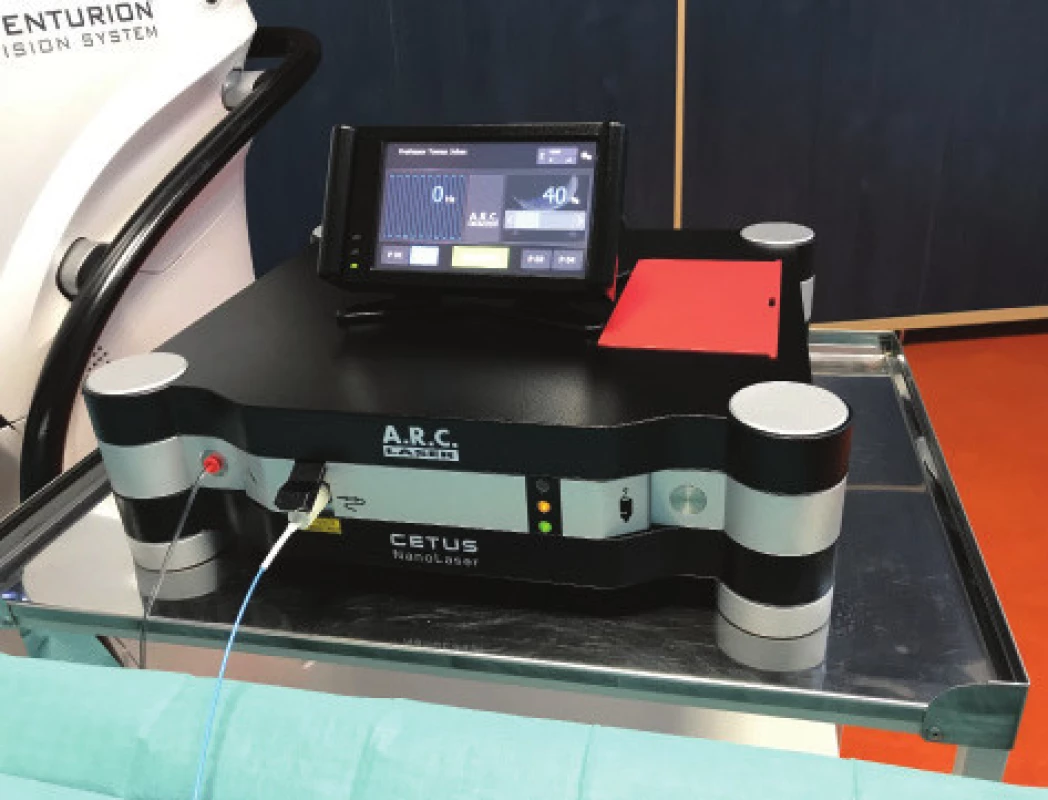
Material and methods
We began to perform cataract surgery with a nanolaser instrument at the beginning of 2018. Our cohort comprised 40 eyes of 20 patients aged between 55 and 70 years, featuring 9 women and 11 men. Cataract surgery was performed at the Oftum Eye Clinic in Košice, and all the operations were performed by a single surgeon (T.J. sr.). The cohort included patients with nuclear cataract up to the 3rd degree. The nuclear opalescence (NO) of the lens was assessed according to the established Lens Opacities Classification System III. A further condition was a number of endothelial cells larger than 1200 cells/mm2.
Excluded from the cohort were patients with a pathologically altered anterior segment of the eye, such as corneal opacities, keratoconus, symptoms of uveitis, pseudoexfoliation syndrome, zonular dialysis, glaucoma and diabetes.
The cohort was divided into 2 groups. In group I the eyes were operated on by ultrasound phacoemulsification in the right eye and in group II the contralateral eyes were operated on by nanolaser lens photofragmentation in the left eye.
Before surgery all the patients underwent an ophthalmological examination covering examination of visual acuity, examination by a slit lamp, applanation tonometry and fundus ophthalmoscopy. In addition, a specular microscope (Nidek CEM 530 Specular microscope, Japan) was used to examine endothelial cell density, corneal thickness and the percentage of hexagonal cells or the pleomorphism index.
Surgical technique
We performed cataract surgery using the nanolaser system Cetus, ARC Laser GmbH Germany (Fig. 1). The pulsing laser energy in this laser is conducted from the source via an optical fibre. Laser energy is usually 5 mJ with a time interval of 5ns. The optical fibre ends in the aspiration opening of the probe in a titanium disc, the aspiration and irrigation system is connected via the vitrectomy module of the Centurion (Alcon) phacoinstrument and ends in the same probe fitted with an irrigation silicone sleeve (Fig. 2) and (Fig. 3).
Fig. 2. Detail of end of nanosecond laser 
Fig. 3. View of connection of both instruments 
Fragmentation of lens matter takes place by means of laser pulses which form plasma and blast the lens matter. The laser probe has a diameter of 2.4 mm.
The Centurion phacoemulsification instrument was used for phacoemulsification. In both cases the traditional “clear cornea cataract surgery” technique was used, therefore with a corneal incision, viscomaterial into the anterior chamber, capsulorhexis, hydrodissection, hydrodelineation and fragmentation of the lens matter with the aid of irrigation and aspiration.
In group I, 40% energy was used, with vacuum 350 mm/Hg and aspiration flow 40 cc/min. In group II, 5 mj energy was used, with vacuum 350 mmPHg and aspiration 40 cc/min.
All patients were implanted with an identical monofocal hydrophobic IOL (iMedical Ophthalmic International Heidelberg GmbH, Mannheim, Germany).
All three parameters of early influence on the cornea by means of cataract surgery were measured before surgery and 7 days after surgery.
A statistical analysis was conducted with the use of SPSS software, accompanied by a paired T-test and Wilcoxon test.
Results
The cohort contained 20 patients, of whom 9 were women and 11 men. The average age was 65 ± 5.96 years.
Before surgery, uncorrected visual acuity (UCVA) in group I was 0.70 ± 0.07, in group II 0.68 ± 0.10. After surgery, BCVA in group I was 0.98 ± 0.05 and in group II 0.98 ± 0.04. There was no statistically significant difference between the individual groups (p = 0.65).
Average ECD before surgery in group I was 2508.50 ± 205.54 bb/mm2 and in group II 2472.50 ± 287.78 bb/mm2. In the same order these values 7 days after surgery were 2024.92 ± 271.50 bb/mm2 and 2138.50 ± 390.85 bb/mm2. In both groups the differences in the numbers of bb/mm2 before and after surgery were statistically significant (p ≥ 0.01). However, the difference between group I and group II was statistically insignificant.
Average corneal thickness before surgery in group I was 562.75 ± 22.07 µm and in group II 568 ± 31.14 µm. Corneal thickness 7 days after surgery in group I was 580.42 ± 28.53 µm and in group II 591.58 ± 36.38 µm. Changes in the individual groups were statistically significant (p-0.01), but the differences between both groups were not statistically significant (p-NS).
The average percentage of hexagonal cells before surgery in group I was 71.25 ± 3.79%, in group II 69.75 ± 4.35 in group II. One week after surgery the values were in group I 68.50 ± 4.52% and in group II 68.42 ± 5.66%. The changes in the individual groups were statistically insignificant, as were the differences between groups I and II (p-NS).
Discussion
The essence of this comparative study of contralateral eyes was to compare the phacoemulsification technique of cataract surgery with the nanolaser technique, upon use of the same flow system of the same phacoemulsification instrument (Centurion, Alcon) and its influence on the cornea in the early postoperative period. Both groups had approximately the same stage of lens opacification.
After 7 days, both groups had very similar results of improvement of UCVA, which attests to rapid rehabilitation of vision in both techniques. Similar results are also stated in the literary sources (1, 2, 3, 6).
At present, each cataract surgery may lead to corneal damage in the sense of a reduction and change of morphology of endothelial cells (7, 8, 12).
A loss of the number of endothelial cells following an intraocular procedure is virtually inexorable, and this is closely linked also to postoperative corneal edema. Change of the hexagonal shape of the endothelial cells is a more sensitive indicator than ECD, and its effect is manifested after a longer time (3).
Upon a comparison of our 2 groups, no statistically significant differences were recorded between the observed parameters, which attests to the efficacy of both methods.
Changes within the framework of the individual groups observed following surgery however attest to the fact that minimal impacts occur, involving negative consequences following intraocular manipulation in the anterior chamber of the eye, even despite the of both procedures.
The process of rehabilitation of the endothelial cells is specific. Undamaged endothelial cells fill in free areas so as to renew their normal function. The healing process takes place over a period substantially longer than 7 days, and continual loss of these cells continues for as long as several years following the implantation of an intraocular lens (4, 11). Kanellopoulos and Asmelilis compared normalisation of corneal thickness following cataract surgery after 3 months (10). In our observation, after surgery corneal thickness in group I was increased by 18.7 ± 6.46 µm and in group II by 22.1 ± 5.24 µm, which can be considered an expected change following cataract surgery by both techniques. Upon a comparison of all three observed indicators, the differences between them were statistically insignificant.
Conclusion
In conclusion it is possible to state that nanolaser in cataract surgery is a safe and effective alternative to phacoemulsification with the aid of ultrasound. It is minimally invasive, with comparable renewal of the function of the corneal endothelium.
It is necessary to emphasise that in principle laser fragmentation is different from ultrasound phacofragmentation, and the harder the nucleus of the opacified lens, the longer and more demanding the process. Further and more extensive studies should designate the indication spectrum of nanolaser technique in cataract surgery.
Received: 18. 3. 2019
Accepted: 30. 10. 2019
Available on-line: 17. 2. 2020
prof. MUDr. Tomáš Juhás, DrSc.
Očná klinika OFTUM
Moldavská 21/A,
040 11 Košice
Zdroje
1. Baradaran-Rafii A., Rahmati-Kamel M., Eslani-M. et al.: Effect of hydrodynamic parameters on corneal endothelial cell loss after phacoemulsification. J Cataract Refract Surg, 35; 2009 : 732-737.
2. Conrad-Hengerer I., Al Jubury M., Schultz T. et al.: Corneal endotelial cell loss and corneal thickness in conventional comparedwith femtosecond laser-assisted cataract surgery: three-month follow. J Cataract Refract Surg, 39; 2013 : 1307-1313.
3. DeBry, P., Olson, RJ., Crandall, AS.: Comparison of energy required for phaco-chop and divide and conquer phacoemulsification. J Cataract Refract Surg, 24; 1998 : 689-692.
4. Dick, HB., Kohnen, T., Jacobi, FK. et al.: Long-term endothelial cell loss following phacoemulsification through a temporal clear incision. J. Cataract Refract Surg, 22; 1996 : 22 : 71.
5. Dodick, JM., Christiansen, J.: Experimental studies on the development and propagation of shock wawes created by interaction of short Nd: YAG laser pulses with a titanium target;possible implications for Nd: YAG laser phacolysiss of the catarastous human lens. J Cataract Refract Surg, 17; 1991 : 794-797.
6. Ecsedy, M., Miháltz K., Kovács I. et al.: Effect of femtosecond laser cataract surgery on the macula. J Refract Surg, 27; 2011 : 717-722.
7. Hayashi K., Hayashi H., Nakao F. et al: Risks factor for corneal endothelial injury during phacoemulsification, 22; 1996 : 1079-1084.
8. Hayashi K., Manabe SI., Yoshimura K. et al.: Corneal endotelial damage after cataract surgery in eyes with pseudoexfoliation syndrome. J Cataract Surg, 139; 2013 : 881-887.
9. Huetz, WW., Eckhardt, HB.: Photolysis using the DodickARC lasersystem for cataract surgery. J Cataract Refract Surg, 27; 2001 : 208-2012.
10. Kanellopoulos, AJ., Dodick JM., Brauweiler P. et al.: Dodick photolysis for cataract surgery; early experience with the Q switched neodymium YAG laser in 100 consecutive patiens. Ophthalmology, 106; 1999 : 2197-2202.
11. Liesegang, TJ., Bourne, WM., Iistrup, DM.: Short and long -term endotelial cell loss associated with cataract extraction and intraocular lens implantation. Am J Ophthalmol, 97; 1984 : 32-39.
12. Pirazzoli, B., D´Eliseo D., Ziosi M. et al.: Effects of phacoemulsification time on the corneal endotelium using phacofracture and phaco chop techniques. J Cataract Refract Surg, 22; 1996 : 967-969.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 5- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- The long-term monitoring of sympathetic ophthalmia in the diagnostic and terapeutic view. Review Department of Ophthalmology
- The optic nerve drusen and haemodynamics
- Sensitivity and specificity of spectral OCT in patients with early glaucoma.
- Nanolaser in cataract surgery and its impact on corneal endotelium
- Molecular genetic cause of achromatopsia in two patients of Czech origin
- INTRAVITREAL THERAPY OF ENDOGENOUS ENDOPHTALMITIS DUE TO UROSEPSIS – A CASE REPORT
- Vodiace psy sa cvičia na Slovensku už 25 rokov
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Molecular genetic cause of achromatopsia in two patients of Czech origin
- INTRAVITREAL THERAPY OF ENDOGENOUS ENDOPHTALMITIS DUE TO UROSEPSIS – A CASE REPORT
- Sensitivity and specificity of spectral OCT in patients with early glaucoma.
- The long-term monitoring of sympathetic ophthalmia in the diagnostic and terapeutic view. Review Department of Ophthalmology
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




