-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Correction of myopia and myopic astigmatism by femtosecond laser in situ keratomileusis
Authors: T. Řeháková; V. Veliká; N. Jirásková
Authors place of work: Oční klinika Fakultní nemocnice Hradec Králové, Sokolská 581, 500 05 Hradec Králové, přednostka: prof. MUDr. Naďa Jirásková Ph. D., FEBO
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 2, p. 65-71
Category: Původní práce
doi: https://doi.org/10.31348/2019/2/2Summary
Aim: We analysed one-year refractive results and the incidence of complications in patients with correction of low-to-high myopia or myopic astigmatism by femtosecond laser in situ keratomileusis (FS-LASIK) using femtosecond laser LenSx® (Alcon, Fort Worth, Texas, USA) a excimer laser Excimer Amaris 500 (Schwind eye-tech-solutions GmbH and Co KG, Kleinostheim, Germany).
Methods: To the retrospective study were included 171 eyes of 87 patients (38 men, 49 women) who underwent correction of myopia and myopic astigmatism by FS-LASIK in the outpatient Department of Ophthalmology, University Hospital in Hradec Králové between 2013-2017. We assessed uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA), subjective refraction, central corneal thickness (CCT) in the thinnest point, patient’s satisfaction and the incidence of complications in the one-year follow-up period.
Results: At the time of laser procedure the mean patient‘s age was 29,26 ± 6,47 years (range 18 to 46 years). In 21 eyes was corrected myopia (range -6,5 to -2,5 D sph) and in 150 eyes myopic astigmatism (range -8,75 to -0,25 D sph and -3,0 to -0,25 D cyl). The mean preoperative UCVA 0,06 ± 0,08 (range 0,02 to 0,8) got better to 1,12 ± 0,17 (range 0,8 to 1,5) at the end of follow-up period. There wasn’t statistically significant change in BCVA between preoperative and postoperative values. Preoperative mean value of subjective refraction was -4,14 ± 1,43 D sph (range -8,5 to -1 D sph) and -0,57 ± 0,58 D cyl (range -3 to 0 D cyl) and after 12 months -0,02 ± 0,16 D sph (range -0,1 to 0,75 D sph) and -0,01 ± 0,1 D cyl (range -0,5 to 0,5 D cyl). The initial mean CCT was 554,76 ± 30,07 μm (range 485 to 660 μm), after 6 months 494,06 ± 34,99 μm (range 421 to 594 μm) and after 12 months 492,92 ± 34,55 μm (range 411 to 592 μm). We observed peroperative complications in 3 eyes. The suction loss of femtosecond laser occurred during flap creation due to sudden eye movement. Postoperatively in one case we enrolled flap pucker first postoperative day. In other case flap dislocation occurred after abdonimal surgery under general anesthesia which was performed 3 months after refractive procedure and we had to indicate flap reposition. The mean grade of patient’s satisfaction was at the end of follow-up period 1,04. The most often complaints were the sensation of dry eye (10 patients) and blurry vision during computer working, inadequate lighting and fatique (6 pacients).
Conclusions: According to our experience correction of low-to-high myopia or myopic astigmatism by using FS-LASIK is an effective, relatively safe and predictable method. The basic assumption of good postoperative results and patient’s satisfaction is thorough and comprehensive preoperative examination with respect to indication criteria.
Keywords:
myopia – laser in situ keratomileusis – femtosecond assisted LASIK – refractive surgery
INTRODUCTION
At present, modern refractive surgery enables correction of the majority of ametropic conditions of the eye (from low to high myopia, hypermetropia, including combination with astigmatism). The surgical options for patients with preserved accommodation capacity and clear lens include laser refractive procedures on the cornea and implantation of phakic intraocular lenses (most often a posterior intraocular collamer lens – ICL – implanted into the capsule).
The oldest recorded procedure from the end of the 19th century is removal of a clear lens in the case of high myopia, which improved visual acuity (VA), but at the same time was hampered by a large risk of sight-threatening complications such as retinal detachment, decompensation of the cornea and endophthalmitis. Since the mid 20th century, attention has shifted to refractive procedures on the cornea with the aim of remodelling the shape of the cornea by flattening or steepening. This initially concerned procedures of a non-laser type, such as autoplastic myopic keratomileusis, epikeratoplasty and in situ keratomileusis. A period of dynamic progress in this branch of ocular medicine began in the 1980s with the introduction of laser technology into ophthalmological practice. An argon-fluoride excimer laser was first used on a blind eye by Seiler in Germany in 1985, and approved by the U.S. Food and Drug Administration in 1995. In the following years a number of laser methods have progressively developed, such as photoreactive keratectomy (PRK), laser assisted subepithelial keratomileusis (LASEK) and laser in situ keratomileusis (LASIK). A further advance was achieved with the introduction of the femtosecond laser (FSL) in the form of LASIK with the assistance of FLS (FemtoLASIK), femtosecond lenticule extraction (FLEx) and small incision lenticule extraction (SMILE). Each of the above methods has its advantages and disadvantages. The selection of a specific procedure depends on the result of a comprehensive preoperative examination, the technical equipment and experience of the centre in question and above all on the preference of the patient [8, 10].
Worldwide, the most widely used techniques for correction of refractive errors include the LASIK method and also, since 2011, its modification FemtoLASIK. In the FemtoLASIK procedure, the operating surgeon works with two types of laser – FSL (fig. 2) and excimer laser (fig. 3). The femtosecond laser works on the principle of molecular photodisruption. The appliance generates pulses with a wavelength of 1028-1053 nm at short intervals of 10-15s, on a very small area of corneal tissue (a point of a size of up to 2 μm) with minimal damage to the surrounding structures. The result of interaction of the laser pulse and tissue is the formation of plasma, a cloud of highly energetic electrons and ionised molecules. The plasma expands rapidly, and at a predefined depth of the corneal stroma forms numerous cavity bubbles on one level, interlinked by bridges of tissue (fig. 1). By mechanical disruption of the bonds, using a metal separator, a precise corneal lamella (flap) is created. The lamella is of a predefined thickness, which was previously in the case of LASIK performed manually by a microkeratometer, and in the LASEK method by alcohol. After uncovering the flap, the actual alteration of corneal curvature is performed by excimer laser, which functions on the principle of photoablation, or irradiation at a wavelength of 193 nm disrupts the bonds between the molecules, which subsequently disperse into the space. The second phase of the procedure with the aid of an excimer laser is identical to the previously mentioned techniques of laser treatment of the cornea [8, 10].
Fig. 1. Creation of corneal flap with femtosecond laser LenSx® (Alcon, Fort Worth, Texas, USA) 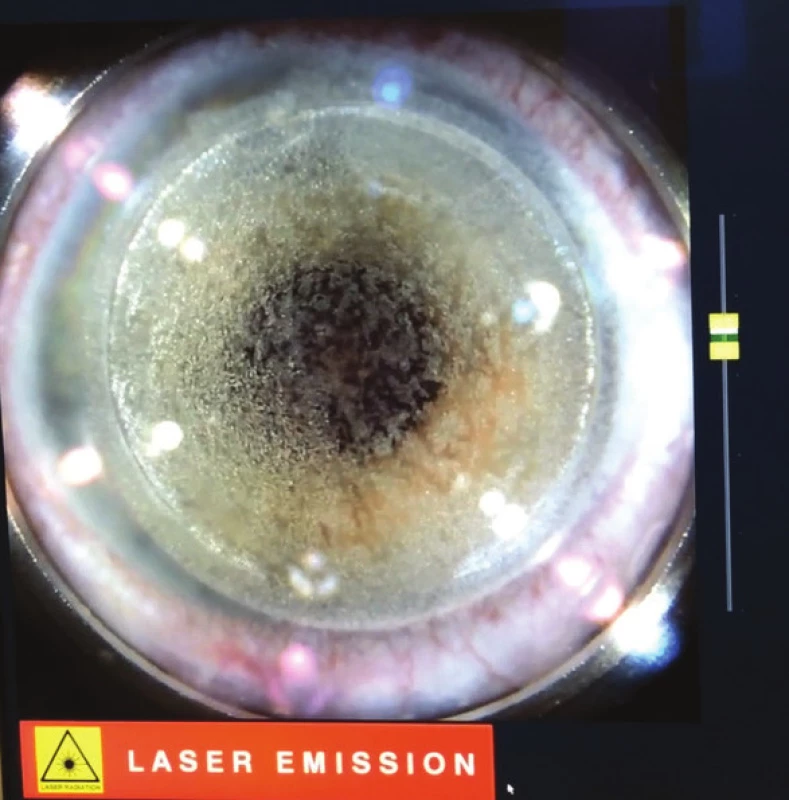
Fig. 2. Femtosecond laser LenSx® (Alcon, Fort Worth, Texas, USA) 
Fig. 3. Excmier laser Excimer Amaris 500 (Schwind eyetech- solutions GmbH and Co KG, Kleinostheim, Germany) 
The aim of the study is to evaluate refractive results obtained within one year and incidence of complications in patients who underwent correction of low, medium and high myopia or myopic astigmatism with the laser procedure FemtoLASIK with the aid of FSL LenSx® (Alcon, Fort Worth, Texas, USA) and excimer laser Excimer Amaris 500 (Schwind eye-tech-solutions GmbH and Co KG, Kleinostheim, Germany).
MATERIAL AND METHOD
The retrospective study incorporated a total of 171 eyes of 87 patients, comprising 49 women (56.3%) and 38 men (43.7%) who underwent correction of myopia or myopic astigmatism by the FemtoLASIK laser method at the Department of Ophthalmology of the University Hospital in Hradec Králové in the period of 2013-2017.
The entrance criteria for inclusion of patients in the cohort were minimum age of 18 years at the time of performance of the procedure, absence of ocular pathologies other than refractive error, absence of serious general pathologies (rheumatic diseases, diabetes mellitus) or signs of disorders of reparation mechanisms (tendency to formation of keloid scars), exclusion of pregnancy and lactation, residual stromal thickness of > 300 μm and stability of refractive error for at least 2 years. Patients who did not regularly attend postoperative follow-up examinations were excluded from the cohort.
Before the procedure patients underwent a comprehensive eye examination, i.e. recording of personal anamnesis, determination of dominant eye, Schirmer’s tear test, Worth 4-dot test, determination of uncorrected (UCVA) and best corrected visual acuity (BCVA) by LCD chart (NIDEK CP-90), manifest and cycloplegic refraction (autorefractometer, NIDEK AR 31OA), determination of value of intraocular pressure by noncontact tonometry (NIDEK NT-530), corneal topograhy (Pentacam, Oculus Inc.), biometry (IOLMaster, Carl Zeiss Meditec AG), endothelometry (noncontact endothelial microscope CEM-530, Nidek, Japan), examination of contrast sensitivity (CSV-1000, Vectorvision) and evaluation of the ocular finding on the anterior and posterior segment of the eye on a slit lamp.
The procedure was performed by a single operating surgeon (V.V.) using the standard procedure recommended by the manufacturer under local anaesthesia. In order to create the flap an FSL LenSx® was used, which creates pulses with energy of 15 μm, with a length of duration of 600-800 10-15 s and frequency of 50 kHZ [19]. The parameters of the flap were set as follows – thickness of flap 130 μm, diameter 9 mm. The actual treatment of the corneal tissue was performed by photoablation with the aid of an excimer laser Excimer Amaris 500 on a surface with a diameter of 6.0 to 7.0 mm. The target refraction was always emmetropia.
On 168 patients, correction was performed bilaterally on a single day, on 4 patients unilaterally (on 3 patients due to interrupted creation of the corneal flap, and on 1 patient the procedure on the second eye was not indicated). In the postoperative period, the patients applied local antibiotics in the form of drops every 2 hours for 4 days, and from the first postoperative day local corticosteroids were applied in drops, in a regime of 4x daily for one week, followed by 3x daily for one week, 2x daily for one week and 1x daily for one week. Regular postoperative follow-up examinations took place within 30 minutes after the procedure, then on the 1st day and 4th day after surgery and subsequently 1, 3, 6 and 12 months after the procedure. We observed UCVA, BCVA, subjective refraction, central corneal thickness (CCT) at the thinnest point, subjective patient satisfaction, which we evaluated on a scale of 1 to 5 (1 – very satisfied, 5 – very dissatisfied), and the incidence of complications during the procedure and over an observation period of one year.
The obtained data was statistically processed using the program SYSTAT 8.0. The significance of the differences between the individual measurements over time was tested with the use of a non-parametric paired Wilcoxon signed-rank test, the majority of parameters did not have normal distribution. The results were evaluated on a level of significance of 0.05.
RESULTS
The average age at the time of performance of the procedure was 29.26 ± 6.47 years (range of 18 to 46 years).
In 21 eyes (12.3 %) myopia was corrected (within the range of -6.5 to -2.5 D sph), in 150 eyes (87.7 %) myopic astigmatism was corrected (within the range of -8.75 to -0.25 D sph and -3.0 to -0.25 D cyl).The preoperative average value of UCVA (decimal values) was 0.06 ± 0.08 (within the range of 0.02 to 0.8), at the end of the observation period this improved to 1.12 ± 0.17 (within the range of 0.8 to 1.5) In the case of BCVA there was no statistically significant difference between the preoperative and final values. A comparison of UCVA and BCVA before surgery and after one year of observation is illustrated in graph 1. The initial mean value of subjective refraction was -4.14 ± 1.43 D sph (within the range of -8.5 to -1 D sph) and -0.57 ± 0.58 D cyl (within the range of -3 to 0 D cyl), at the last postoperative follow-up examination after 12 months -0.02 ± 0.16 D sph (within the range of -0.1 to 0.75 D sph) and -0.01 ± 0.1 D cyl (within the range of -0.5 to 0.5 D cyl), respectively 97.1 % of eyes acquired postoperative values of manifest spherical equivalent up to ± 0.5 D and 100% of eyes up to ± 1.0 D (graph 2). In both parameters there was a statistically significant improvement upon a comparison of the initial and final values. In no case was there a hypermetropic shift above +0.5 D.
Graph 1. Average values of uncorrected and best corrected visual acuity before surgery and during the course of the postoperative follow-up examinations. Statistically significant improvement of uncorrected visual acuity from the first postoperative follow-up one day after surgery. Best corrected visual acuity without statistically significant difference during the course of observation 
Graph 2. Mean values of subjective refraction before surgery and during the course of the postoperative follow-up examinations. Statistically significant improvement from the first postoperative follow-up examination one day after surgery and stable results postoperatively 
The mean CCT value before the procedure was 554.76 ± 30.07 μm (within the range of 485 to 660 μm), after 6 months 494.06 ± 34.99 μm (within the range of 421 to 594 μm) and one year after the procedure 492.92 ± 34.55 μm (within the range of 411 to 592 μm). Upon a comparison of the preoperative and first postoperative values we recorded a significant decrease. During the course of the observation period there was no statistically significant change of CCT (graph 3). We recorded a reduction below 450 μm in 21 eyes (12.3 %) of 12 patients (average value 435.95 ± 8.53 μm).
Graph 3. Value of central corneal thickness (CCT) at the thinnest point was significantly reduced only upon comparison of preoperative and first postoperative values, after which there was no change not only of the mean value of CCT, but also of the value measured in each patient 
We observed perioperative complications in 3 eyes. In all cases it concerned an interruption of the procedure due to loss of suction of the FSL during the creation of the corneal flap, due to sudden eye movement. Postoperatively a slight puckering of the flap occurred in one eye, and in one case dislocation of the flap in a patient following an abdominal operation under general anaesthesia 3 months after laser surgery. In this case repositioning of the flap was indicated due to deterioration of VA. The subsequent occurrence of fibrosis at the edge of the flap had no influence on the final VA.
The average score of patient satisfaction at the end of the observation period was 1.04. Of the subjective complaints, patients most frequently stated a feeling of dry eyes, with an improvement following the application of artificial tears (10 patients, i.e. 11.5%) and blurred vision during work on a computer, under dim lighting or during greater fatigue (6 patients, i.e. 6.9%).
DISCUSSION
The visual system is the most important sensory apparatus of all for humans, providing us with as much as 80% of the information we receive about our external environment. The lifestyle of modern advanced society in the last few decades has placed great demands on the individual in several respects, including good visual functions. Thus, poor quality visual perception may be a substantially limiting factor both in regular daily activities and in leisure pursuits. Refractive errors rank among the most common ocular pathologies with a detrimental effect on VA. A meta-analysis conducted by Hashemi et al. [6] from 2017 evaluated the incidence of individual refractive errors by means of an analysis of 163 articles from various geographical regions of the world. The conclusions of the study point to the fact that the percentage distribution of the individual types is not the same in the individual regions, similarly as between different ethnic groups of the population. A high prevalence of myopia occurs in the industrialised regions of East Asia. There is a certain controversy surrounding hypermetropia. Some studies point to a higher incidence in Europe and the advanced countries of the world, but the studies incorporated a group of older patients in whom the refractive condition may have been influenced by age-conditioned changes to the structure of the ocular lens. In Europe the prevalence of myopia was determined at 14.2 % (range 10.5 to 18.2 %) and astigmatism at 12.9 % (range 4.1 to 21.8 %) in children and 27 % (range 22.4 to 31.6 %) and astigmatism at 39.7 % (range 34.5 to 44.9 %) in adults. The study points to a linear increase in the incidence of short sightedness in the last 30 years, and above all in the countries of South East Asia it is becoming a significant problem of epidemic proportions. The authors state as the possible cause an increase in lifestyle changes in the last century, or a increase of long-term close-up work due to the technological progress of Western society in connection with a shortening of time spent doing outside activities. The European Eye Epidemiology study from 2015 states a prevalence of myopia in persons aged 25-29 years as follows: low myopia (≤ -0.75D to > -3D) 26.5 % (21.8 to 31.2 %), medium myopia (≤ -3D to > -6) 14.1 % (5.1 to 23.2 %), high myopia (≤ -6D) 5.3 % (2.9 to 7.7 %) [5, 6, 19].
The aim of our study was to evaluate the refractive results and incidence of complications in patients following correction of low to high myopia or myopic astigmatism using the FemtoLASIK laser method in one year observation. At our centre, for patients with preserved accommodation capacity we prefer adjustment of the refractive condition of the eye by laser procedure on the cornea, with targeted emmetropisation. According to the character of the refractive error, preoperatively determined anatomical ratios of the eye and patient’s preference, we choose either the surface laser method PRK, transPRK or the flap method FemtoLASIK.
The refractive postoperative results for the FemtoLASIK method are excellent [3, 9, 13-15, 18], and our results are in accordance with the previously published studies. On the first day after the procedure, UCVA and the value of subjective refraction were significantly improved, and in the further observation period they remained stable. Like every surgical procedure, FemtoLASIK also has its potential risks of perioperative or postoperative complications. In the literature the perioperative complications stated are for example formation of a total flap (i.e. loss of link between flap and remaining cornea), perforation of flap or cornea, haemorrhage during operation, decentration of zone of photoablation, while postoperative complications include decrease of corneal sensitivity and development of dry eye syndrome, corneal haze, striae of flap, growth of epithelium beneath flap, sterile infiltrates, and diffuse lamellar or infectious keratitis [1, 3, 4, 7, 12]. A part of these complications occurs in both classic LASIK, and in more modern FemtoLASIK. Some complications are specific only to FemtoLASIK, e.g. presence of an opaque layer of gas on the superficial layers of the stroma (0.6 – 2.36%), air bubbles beneath the conjunctiva (2%) or anterior chamber (1.18%) [3, 11, 14, 15]. The summary incidence of complications in the FemtoLASIK procedure is published within the range of 3.5 – 5% [11, 14, 15]. In our cohort we recorded perioperative complications in three eyes (loss of suction of FS laser upon sudden, sharp eye movement). The procedure was discontinued in all cases, and a decision was taken on the further solution after a time interval. In one case the patient did not wish to undergo reoperation and the resulting anisometropia was corrected by wearing a soft contact lens (CL), with which the patient was satisfied. In another two situations (interruption of creation of flap in approx. 2/3 of the surface and final side-cut) we performed reoperation after pacification of the ocular finding – in a patient in whom the refractive condition of the eye enabled the performance of a superficial procedure we used the transPRK method, and in the second patient the FemtoLASIK method was used again. In both cases, the final VA was 1.0. A slight puckering of the flap occurred postoperatively in one eye on the first postoperative day, which was adjusted after the application of a soft CL, and dislocation of the flap occurred in a patient at a follow-up examination after 3 months following an abdominal operation performed under general anaesthesia, as a result of which it was necessary to perform repositioning of the flap to restore the VA. The subsequent occurrence of fibrosis at the edge of the flap had no influence on the final VA.
The incidence of serious perioperative and postoperative complications leading to a deterioration of VA is decreasing with the length of use of the method. According to the study by Pokroy et al., over time the incidence of reLASIK (enhancement) is also being reduced as follows - 2000 16 %, 2003 10.5 %, 2009 6.3 %, 2010 3.8 % and 2012-14 0.38 %. The risk factors include higher degrees of hypermetropia and astigmatism, corneal steepness and age of patients (over 50 years), whereas a preventive factor is a smaller diameter of the ablation zone (7.0 mm) [16]. The decreasing trend has been enabled above all by technological advance and years of experienced gained with this method, and indication criteria adjusted on this basis. Modern corneal topographs are also capable of detecting forme fruste corneal pathologies preoperatively, and thus of contraindicating a laser procedure. This above all concerns ectatic pathologies such as keratokonus, which pronouncedly increases the risk of occurrence of one of the most feared complications – postoperative corneal ectasia. In our cohort the value of CCT at the thinnest point was significantly reduced only in a comparison of the perioperative and first postoperative values. Subsequently there was no statistically significant change, not only of the mean CCT value in the cohort, but also of the values measured in each patient separately. In the case of flap methods, the critical step is the creation of a precise corneal flap manually by microkeratome or more recently by FSL. Studies comparing classic LASIK with FemtoLASIK state better effectiveness and predictability in the use of FSL, as well as a lesser degree of induction of higher order aberrations, postoperatively more stable biomechanics of the cornea and more rapid visual rehabilitation. There is no significant difference in the safety profile of both procedures. Patient-paid refractive procedures, which are usually performed on young, active individuals without other ocular pathology, are linked with high demands from patients regarding the postoperative result, not only for UCVA, but also the degree of subjective satisfaction. In our cohort the average score in evaluation of satisfaction was 1.04. The high degree of satisfaction with the procedure which we determined is in accordance with other published studies [1, 3, 4, 7, 9, 12, 14, 15, 18]. The most frequent complaint from patients was a feeling of dry eyes (11.5 %) with improvement after the application of lubrications, and perception of blurred vision upon long-term work on a computer, under reduced lighting conditions or during fatigue (6.9 %).
CONSLUSION
On the basis of our experiences, correction of low to high myopia and myopic astigmatism with the aid of FemtoLASIK, using an FSL LenSx® and excimer laser Excimer Amaris 500 is an effective and relatively safe method, with a predictable refractive result. The fundamental prerequisite for attaining good postoperative results and patient satisfaction is primarily a thorough and comprehensive preoperative examination, respecting the indication criteria. In modern refractive surgery the method deservedly enjoys considerable popularity and high demand among patients.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received by the Editorial Department on: 14 January 2019
Accepted for printing on: 10 March 2019
Zdroje
1. Al Arfaj, K., Hantera, M.M.: Comparison of LASEK, mechanical microkeratome LASIK and Femtosecond LASIK in low and moderate myopia. Saudi J of Ophthalmol., 28 (3); 2014 : 214-219.
2. Arbelaez, M.C., Mosquera, S.A.: The SWIND AMARIS Total-Tech Laser as An All-Rounder in Refractive Surgery. Modele East Afr J Ophthalmol. 16 (1); 2009 : 46-53.
3. Cosar, C.B., Gonen, T., Moray, M. et al.: Comparision of visual acuity, refractive results and complications of femtosecond laser with mechanical microkeratome in LASIK. Inj J Ophthalmol. 6c(3); 2013 : 350-355.
4. Espandar, L., Meyer, J.: Intraoperative and Postoperative Complications of Laser in situ Keratomileusis Flap Creation Using IntraLase Femtosecond Laser and Mechanical Microkeratomes. Middle East Afr J Ophathalmol. 17 (1); 2010 : 56-59.
5. Foster, P.J., Jiang, Y.: Epidemiology of myopia. Eye. 28 (2); 2014 : 202-8.
6. Hashemi, H., Fotouhi, A., Yekta, A. et al.: Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophathalmol. 30 (1); 2018 : 3-22.
7. Hashmani, S., Hashmani, N., Rajani, H. et al.: Comparision of visual acuity, refractive outcomes, and satisfactory between LASIK performed with a microkeratome and femto laser. Clin Ophthalmol. 11; 2017 : 1009-1014.
8. Heissigerová, J. et al.: Oftalmologie. Praha, Maxdorf, 2018, 61-67s.
9. Kanellopoulos A.J., Asimellis, G.: Long-term bladeless LASIK outcomes with the FS200 Femtosecond and EX500 Excimer Laser workstation: the Refractive Suite. Clin Ophthalmol, 7; 2013 : 261-269.
10. Kuchynka, P. et al.: Oční lékařství. Praha, Grada Publishing, 2016, 222-234s.
11. Niparugs, M., Tananuvat, N., Chaidaroon, W. et al.: Outcomes of LASIK for Myopia and Myopic Astigmatism Correction with the FS200 Femtosecond Laser and EX500 Excimer Laser Platform. Open Ophthalmol J, 12; 2018 : 63-71.
12. Pajic, B., Vastardis, I., Eggspuehler, B. et al.: Femtosecond laser versus mechanical microkeratome-assisted flap creation for LASIK: a prospective, randomized, paired-eye study. Clin Ophthalmol, 8; 2014 : 1883-1889.
13. Piao, J., Li, Y.J., Whang, W.J. et al.: Comparative evaluation of visual outcomes and corneal asphericity after laser-assisted in situ keratomileusis with the six-dimension Amaris excimer laser system. PloS One. 12 (2); 2017: e0171851.
14. Pietila, J., Huhtala, A., Makinen, P. et al.: Flap characteristics, predictability, and safety of the Ziemer FEMTO LDV femtosecond laser with the disposable suction ring for LASIK. Eye (Lond). 28 (1); 2014 : 66-71.
15. Pietila, J., Huhtala, A., Makinen, P. et al.: Laser-assisted in situ keratomileusis flap creation with the three-dimensional, transportable Ziemer FEMTO LDV model Z6 I femtosecond laser. Acta Ophthalmol. 92 (7); 2014 : 650-655.
16. Pokroy, R., Mimouni, M., Sela, T.: Myopic laser in situ keratomileusis retreatment: Incidence and associations. J Cataract Refract Surg. 42 (10); 2016 : 1408-1414.
17. Rozskowska, A.M., Mosquera, S.A.: Use of the Femtosecond Lasers in Ophthalmology. The European Physical Journal Conferences 167 [Internet], Dostupné z https://doi.org/10.1051/epjconf/201816705004.
18. Tabacaru, B., Stanca, H.T.: One year refractive outcomes of Femtosecond LASIK in mild, moderate and high myopia. Rom J Ophthalmol, 61 (1); 2017 : 23-31.
19. Williams, K.M., Verhoeven, V.J., Cumberland, P. et al.: Prevalence of refractive error in Europe: the European Eye Epidemiology Consortium. Eur J Epidemiol. 30 (4); 2015 : 305-15.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 2- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- Normal tension vs high tension glaucoma: an – overview
- Correction of myopia and myopic astigmatism by femtosecond laser in situ keratomileusis
- Effect of Botulinum toxin A application in neuro-ophtalmologic indications on Schirmer’s test and tears osmolarity.
- Peripheral exudative hemorrhagic chorioretinopathy
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Očná klinika Lekárskej fakulty Univerzity Komenského v Bratislave oslavuje 100-TÉ VÝROČIE činnosti – 1. časť
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Normal tension vs high tension glaucoma: an – overview
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Peripheral exudative hemorrhagic chorioretinopathy
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



