-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaConjuctival lesions - the relationship of papillomas and squamous cell carcinoma to HPV infection
Authors: A. Furdová 1; A. Stopková 1; K. Kapitánová 2; D. Kobzová 3; P. Babál 3
Authors place of work: Klinika oftalmológie Lekárskej fakulty Univerzity Komenského a Univerzitná nemocnica, Nemocnica Ružinov, Bratislava 1; Klinika oftalmológie Jeseniova Lekárska fakulta Univerzity Komenského, Martin 2; Ústav patologickej anatómie LF UK a UNB, Bratislava 3
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 3, p. 92-97
Category: Původní práce
doi: https://doi.org/10.31348/2018/1/2-3-2018Summary
The etiology of papilloma formation is multifactorial. There is a strong association between human papillomavirus (HPV) and the development of these conjunctival lesions. HPV is tumorigenic and commonly produces benign tumors with low malignant potential. Papillomas rarely go through malignant transformation.
Material and methods:
Retrospective study of patients with a diagnosis of conjunctival papilloma or squamous cell carcinoma.
Results:
From a collection of 125 patients with conjunctival non-pigmented tumours in the period from 2007 to 2017, in 119 (95.2%) patients histological examination confirmed papilloma and in 6 (4.8%) patients it confirmed carcinoma.
Of the total number of patients, 39 were women (31.2%) and 86 men (68.8%). The mean age of patients was 68.4 years (range 20-94 years). Localization of lesions: bulbar conjunctiva - 65 (52.0%), upper eyelid tarsal conjunctiva + fornix - 6 (4.8%), lower eyelid + fornix - 27 (21.6%), caruncle - 20 (16.0%) and plica semilunaris - 7 (5.6%) patients.
In the patient cohort we recorded 2 papillomas that were transformed into squamous cell carcinoma. HPV16 was positive in these patients, the carcinomas were from the area of the bulbar conjunctiva, and the surgical solution was associated with the perioperative administration of Mitomycin C.
In one case, the inverted papilloma developed into orbital carcinoma within 2 years of primary excision, and the patient underwent radical surgical procedure (partial exenteration of the orbit) followed by radiotherapy.
Conclusion:
Transformation of the papilloma into the carcinoma is rare, but it must always be taken into consideration in case of a recurrence of the disease. HPV can infect the conjunctiva. The ophthalmologist, in collaboration with a pathologist, may recommend appropriate laboratory tests to confirm the diagnosis. Long-term outpatient follow-up of patients after excision of the conjunctival papilloma is also necessary.
Key words:
epibulbar tumors, conjunctival tumors, papilloma, carcinoma
Introduction
Papilloma is a histopathological term indicating a tumour from the surface epithelium. It may be solitary or multiple. It takes on a classic finger-like or cauliflower-like appearance. Conjunctival papillomas are not life threatening. However, they may be sufficiently large as to be unpleasant or cosmetically deforming. They are divided into squamous cell, limbal and inverted (Schneider) papillomas, depending on their appearance, location, the age of the patient, their tendency to recur after excision and according to histopathology. Limbal conjunctival papilloma is frequently referred to as a non-infectious inflammatory papilloma, because it is assumed that it originates as a consequence of exposure to ultraviolet radiation. Inverted conjunctival papillomas have a component of the mucosa and epidermis. They occur rarely. The etiology of papilloma formation is multifactorial. There is a strong association between human papillomavirus (HPV) and the development of these conjunctival lesions. The HPV virus is a pronounced tropism for the squamous cell epithelium. More than 100 different types of HPV have been identified. HPV is tumorigenic and commonly produces benign tumours with low malignant potential. The human papillomaviruses most commonly found in conjunctival papillomas are types 6 and 11, which are responsible for the occurrence of skin lesions and also affect the genital tract. HPV is transmitted via direct contact with people. This concerns auto-inoculation from contaminated fingers on the conjunctiva, but cases are known in which a mother with HPV infection of the vulva has given birth to a child in whom a conjunctival papilloma appeared within a short time. The primary method of treatment is excision, though recurrences are frequent (6, 8).
Material and method
A retrospective study of 125 patients with a diagnosis of conjunctival non-pigmented tumours – conjunctival papilloma or conjunctival squamous cell carcinoma – was conducted at the Department of Ophthalmology, Faculty of Medicine of Comenius University and University Hospital in Bratislava.
In January 2018 we called in 78 patients with a diagnosis of histologically verified conjunctival papilloma or conjunctival squamous cell carcinoma for a follow-up examination, and prepared a questionnaire for them. The questions in the questionnaire were focused on the possible relationship between HPV and conjunctival lesions. We clinically examined the patients.
Results
In a group of 125 patients from the period of 2007-2017 we recorded the incidence of conjunctival non-pigmented tumours, of which papilloma was confirmed by histological examination in 119 patients (95.2%), and carcinoma in 6 patients (4.8%).
Out of the total number of patients, 39 were women (31.2%) and 86 men (68.8%). The average age of the patients was 68.4 years (range 20-94 years). Localisation of lesions: bulbar conjunctiva in 65 (52.0%), upper eyelid, tarsal conjunctiva + fornix in 6 (4.8%), lower eyelid + fornix in 27 (21.6%), caruncula in 20 (16.0%) and plica semilunaris in 7 patients (5.6%) (graph 1).
Graph 1. Localisation of conjunctival lesions in a cohort of 125 patient 
Within the framework of the histological examination, all the patients were confirmed positive for HPV 16.
All 6 patients with verified carcinoma were men.
In 2013 we diagnosed inverted papilloma in one patient (fig. 1). In 2014 a transformation occurred of the inverted papilloma into a malignant form of carcinoma (fig. 2). Upon an examination by magnetic resonance imaging 2 years after the determination of diagnosis of inverted papilloma, there was a development of an extensive, non-sharply bordered infiltrate in the orbital region, which non-homogeneously saturated following the administration of a contrast substance and infiltrated the extraocular muscles (only the m rect. lat. was unaffected), had a deforming effect on the eyeball and caused protrusion. The sclera manifested signs of intrabulbar outgrowth in certain places, the lesion had an expansive effect on the eyeball with deformation of the contour, and caused protrusion. In certain places the sclera was blunted with signs of intrabulbar outgrowth 56x35x38 mm, previously 39x28x24 mm /ApxLLxCC/, in 10/2013 20x16x16 mm. The lesion had an expansive effect on the medial wall of the orbit. From 10/2013 the tumour increased in volume by more than 10 times. The patient was subsequently indicated for enucleation with partial exenteration of the orbit and radiotherapy.
Fig. 1. Clinical picture of a patient with inverted type of conjunctival papilloma in the nasal section of the bulbar conjunctiva (1/2013) 
Fig. 2. Clinical picture of the same patient in March 2014 – progression with tendency of infiltration into orbit 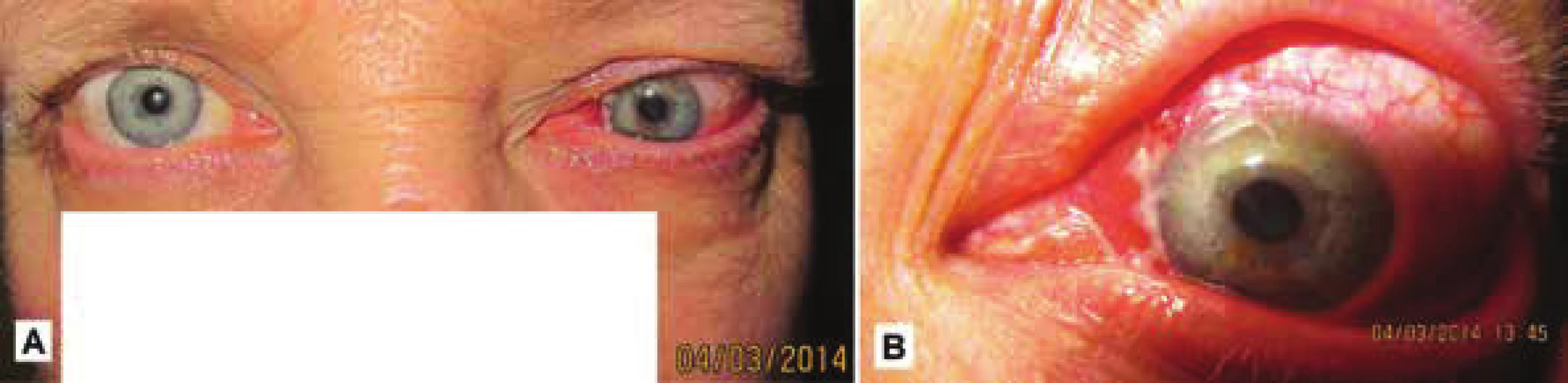
In the period of 2013-2015 we recorded a total of 78 patients with papilloma of the conjunctiva (fig. 3, 4, 5) or carcinoma (fig. 6), who we called for examination. Of the 78 patients addressed, 37 (47.4%) attended a follow-up examination in January 2018.
Fig. 3. Clinical picture of a patient with papilloma of conjunctiva on the inner side of lower eyelid 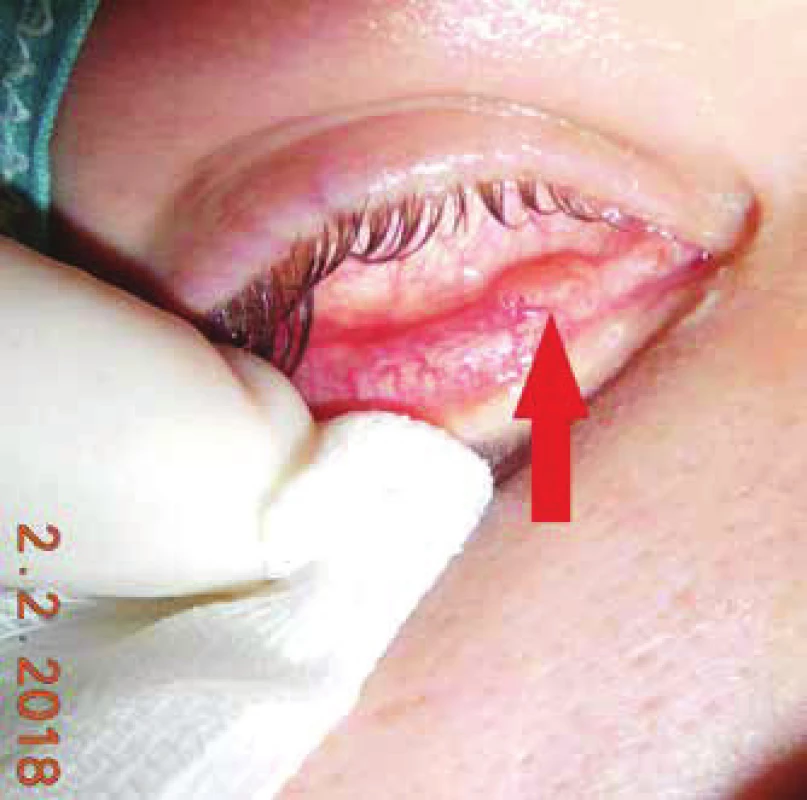
Fig. 4. Clinical picture of a patient with papilloma of caruncula 
Fig. 5. Clinical picture of a patient with papilloma of bulbar conjunctiva 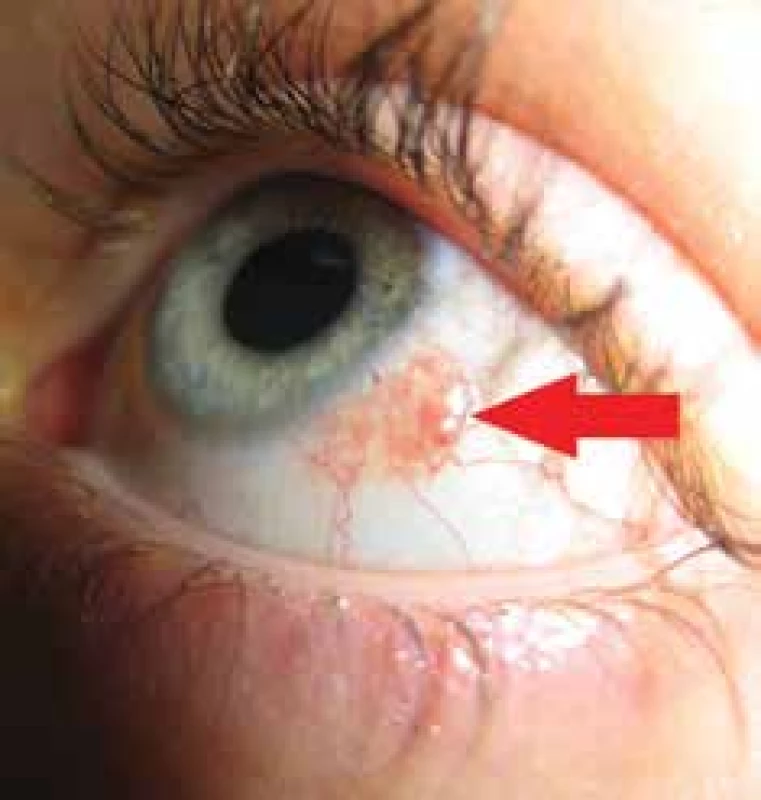
Fig. 6. Clinical picture of a patient with squamous cell carcinoma of bulbar conjunctiva 
We analysed the results of the completed questionnaires of 37 patients. In the group of patients who attended the examination, 31 (83.8%) were with diagnosed conjunctival papilloma and 6 (16.2%) with confirmed carcinoma. The presence of lesions in locations other than the conjunctiva was confirmed in 28 patients (75.7%), especially in the area of the chest, neck and face (table 1).
Tab. 1. Extraocular localisation of lesions in group of 37 patients who completed the questionnaire (some patients stated more than one localisation) 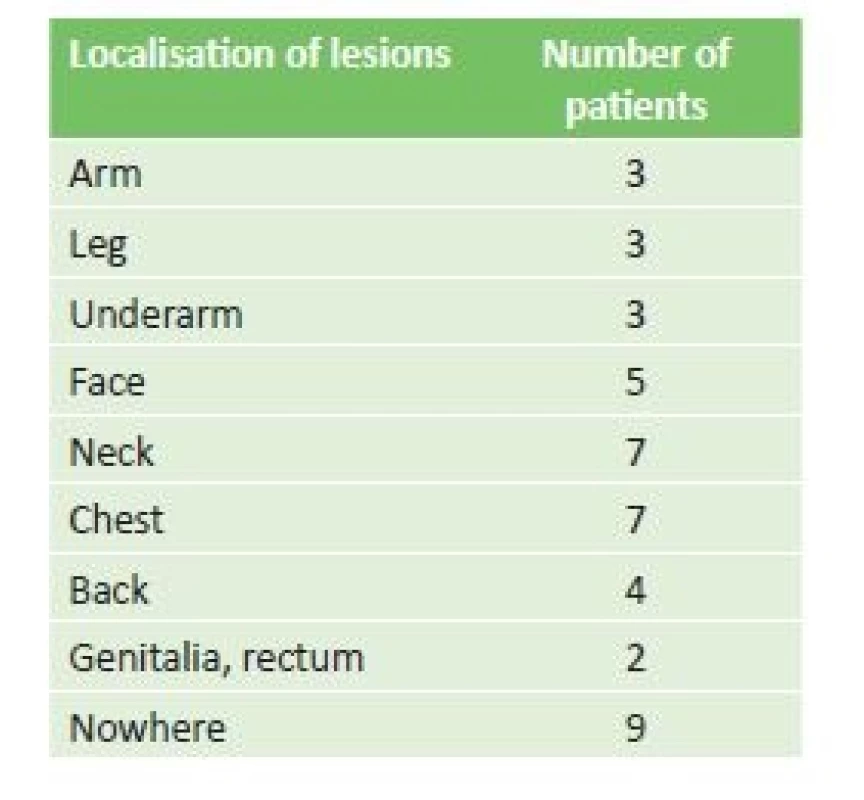
In 4 patients there was a positive personal anamnesis of cervical or prostate carcinoma. None of the patients had been vaccinated against HPV, and in no case had a similar ocular lesion occurred within the family. None of the patients had been born with the given ocular lesion, but this developed during the course of life. Vision did not deteriorate as a result of excision of the papilloma in any of the patients, with the exception of those who underwent enucleation due to carcinoma. In the examined patients we discovered 1 recurrence of conjunctival papilloma, which we subsequently surgically removed.
In our cohort of patients, in 2 cases we recorded papillomas of the bulbar conjunctiva which transformed into a carcinoma. Carcinomas recurred in two patients 2 years after primary excision. Positivity of HPV 16 was confirmed in these patients.
In all cases the carcinomas originated from the region of the bulbar conjunctiva. Surgical solution of conjunctival carcinomas was connected with perioperative application of Mitomycin C.
In the group of patients who attended the follow-up examination in January 2018, 31 (83.8%) were with diagnosed conjunctival papilloma and 6 (16.2%) with confirmed carcinoma. In this sub-group we determined 1 recurrence of conjunctival papilloma, which we subsequently surgically removed.
The presence of lesions in locations other than the conjunctiva was confirmed in 75% of patients, especially in the area of the chest, neck and face.
Discussion
The prevalence of conjunctival papillomas depends on geographical region, but in general it is higher than the prevalence of conjunctival carcinomas. There is a higher incidence in individuals of Caucasian race, male sex, and people aged between 50 and 75 years. In our cohort the highest incidence of lesions was in patients aged between 60 and 70 years, which is in accordance with the available publications. In our cohort we also recorded a higher percentage of papillomas (95.2%) in comparison with the number of carcinomas (4.8%). Carcinomas appeared more frequently in men than in women.
Conjunctival papillomas also occur in children and adolescents. In a comparison of groups of children and adults with occurrence of conjunctival papillomas, there was a markedly higher incidence in younger age groups, respectively in adolescents (5). Recurrences of papillomas are also recorded more frequently in young individuals (adolescents).
Detailed processing of the anamnestic data is important for determination of the diagnosis. The family anamnesis is generally positive, as is the incidence of lesions in locations outside the ocular region, which was confirmed by ¾ of our patients. It is possible to expect an anamnesis of excision of a lesion in the past in the case of possible recurrence. Change of the size and shape should always indicate possible neoplastic proliferation. The papilloma has a greyish-red appearance, a soft mass often reminiscent of cauliflower, and does not cause the patient problems with visual acuity, whereas carcinomas are of a gelatinous consistency and have a varying appearance, with a colour from pearl grey to reddish-brown. White plaque may appear on the surface of the lesion, which causes deterioration of vision in the patient. Clinically the symptoms may range from asymptomatic to chronically irritated red eyes (1).
However, the definitive result will be provided by a histological examination, which is the key to determining the diagnosis and provides a differentiation between a benign papilloma and an invasive carcinoma.
In the past HPV 16 was unequivocally considered a precondition for the incidence of carcinomatous lesions in the region of the oropharynx and genitalia. On the basis of the presence of HPV 16 in benign and malignant lesions, as well as the age distribution, it appears probable that HPV 16 alone cannot cause the development of conjunctival dysplasia and squamous cell carcinoma, and that the correlation between papilloma and carcinoma and HPV infection may be random (15). Conjunctival squamous cell carcinoma (SCC) is a relatively rare aggressive tumour with potential metastases into the regional lymph nodes. It originates from the layer of the epidermis (stratum spinosum), which is formed by a number of layers of polygonal squamous cells. It may occur de novo or from pre-existing actinic keratosis (3, 7). In our cohort of patients we identified one originally inverted and one atypical papilloma, which transformed into a carcinoma.
Risk factors for SCC include chronic infection by human papillomavirus (HPV), human immunodeficiency virus (HIV), vitamin A deficiency, chronic irritation and chronic epithelopathy. Immunodeficiency, whether due to organ transplant or secondarily in HIV, is significant especially in connection with one of the above-stated risk factors (1). We did not record the use of immunosuppressants or organ transplant in any of our patients. We did not conduct testing of the patients for HIV, but none of them stated this in their anamnesis.
Both forms of lesions are treated radically, but with markedly different expected therapeutic outcomes. In the case of less invasive lesions the endeavour is for complete eradication, whereas the goal in the case of invasive carcinomas is to minimise the spread of the pathology. Depending on the lesion and the histopathological finding, priority is given to excision in the treatment of conjunctival papillomas, with local use of Mitomycin C. In the case of SCC a combination of surgical excision, cryotherapy and chemotherapy is used. In rare cases radiotherapy may be necessary, and in extreme cases enucleation or even exenteration of the orbit (3).
Upon correct and timely therapy, the prognosis for patients is good and the mortality rate low, as evidenced also in our group of patients, in which we recorded only one death of a patient with SCC, who died of osteomyelofibrosis 2 years after excision.
In this study we focused also on the degree of repeated occurrence of conjunctival lesions after their excision. We confirm the level of recurrence stated in the professional literature – e.g. in the study by Sjö et al. (16), in a cohort of 165 patients the frequency of HPV was 81%, Eng et al. (2) in a cohort of 24 patients recorded HPV positivity in 58%, Sjö et al. (17) in a cohort of 55 patients recorded positivity in 92%, Nakamura et al. (14) in a cohort of 9 patients found positivity in 44%, Saegusa et al. (15) in a cohort of 16 patients had positivity in 75%, McDonnell et al. (10) in a cohort of 23 patients found positivity in 65%, Kalogeropoulos et al. (6) describe case reports of 2 patients. In the examined patients we identified 1 recurrence of conjunctival papilloma. Within the framework of our cohort of patients, 2 recurrent carcinomas appeared. All 3 recorded recurrences occurred during the course of the 2 years following their surgical removal.
Several studies have demonstrated a correlation of the majority of papilloma lesions of the conjunctiva and the lachrymal sac with HPV infection type 6 (13), as well as type 11 (10). By contrast, squamous dysplasia and conjunctival carcinoma are more often linked with HPV infection type 16 and 18 (9). According to a number of authors, koilocytosis – the main morphological marker of HPV infection in the histological finding – is an insufficiently sensitive diagnostic indicator (17). As a result the examination method currently used is primarily polymerase chain reaction (PCR). This concerns in vitro DNA amplification, which fundamentally contributes to the detection of specific DNA sequences (9).
In a study published in 2006 (11), the authors used PCR examination for identifying the type of HPV infection, demonstrating the presence of HPV type 11 in all the analysed samples.
Mlakar et al. (12) in 2015 published a study focusing on determining the overall prevalence of various types of HPV infection in squamous cell papillomas of the conjunctiva. HPV DNA was confirmed in 76% of papilloma samples, in which HPV type 6 was positive in 48% and HPV type 11 in 28% of samples out of a total number of 25 papillomas. The other samples corresponded to other types of HPV infection (HPV 9, 12, 20, 21, 22 and 24).
The majority of conjunctiva papillomas represent benign tumours with a minimal tendency to malignancy. Squamous cell papillomas with dysplasia have a tendency toward malignancy (6). In the case of lesions with inverted growth, as well as with recurrent lesions, their malignant transformation may occur (4). In our cohort we recorded one case of a transformation of an inverted papilloma into the form of a carcinoma, which infiltrated the orbit. A malignant transformation of a benign inverted papilloma occurred in this patient within 2 years of the primary excision from the conjunctiva. The scope of infiltration was determined by the indication of extended enucleation, and the patient subsequently underwent radiotherapy.
Conclusion
HPV infection is considered the most common sexually transmitted disease, and may also infect the mucosa and conjunctiva. Squamous cell papillomas of the conjunctiva are common benign epithelial tumours, and HPV infection is strongly associated with their incidence. On the basis of the clinical picture, the ophthalmologist in co-operation with a pathologist can recommend the relevant laboratory examinations in order to confirm the diagnosis, as well as the treatment of conjunctival papillomas in order achieve the best possible results and prevent recurrence.
The majority of conjunctiva papillomas represent benign tumours with a minimal tendency to malignancy. Squamous cell papillomas with dysplasia have a tendency toward malignancy (6). In the case of lesions with inverted growth, as well as with recurrent lesions, their malignant transformation may occur (4). In our cohort we recorded one case of a transformation of an inverted papilloma into the form of a carcinoma, which infiltrated the orbit. A malignant transformation of a benign inverted papilloma occurred in this patient within 2 years of the primary excision from the conjunctiva. The scope of infiltration was determined by the indication of extended enucleation, and the patient subsequently underwent radiotherapy.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
doc. Mgr. MUDr. Alena Furdová, PhD., MPH, FEBO
Klinika oftalmológie LFUK a UNB, nemocnica Ružinov
Ružinovská 6, 826 06 Bratislava
Zdroje
1. Boese, E., Rogers, G.M., Kitzmann, A.S.: A Very Unusual Case of Ocular Surface Squamous Neoplasia [Internet]. 2013 [cited 2018 May 8]; Available from: https://webeye.ophth.uiowa.edu/eyeforum/cases/163-OSSN.htm
2. Eng, H.-L., Lin, T.-M., Chen, S.-Y., et al.: Failure to detect human papillomavirus DNA in malignant epithelial neoplasms of conjunctiva by polymerase chain reaction. Am J Clin Pathol, 2002; 117 (3): 429–36.
3. Furdova, A.: Epibulbárne nádory [Internet]. 2016 [cited 2018 May 8];Available from: https://www.fmed.uniba.sk/fileadmin/lf/sluzby/akademicka_kniznica/PDF/Elektronicke_knihy_LF_UK/EPIBULBARNE_NADORY.pdf
4. Huang, Y.-M., Huang, Y.-Y., Yang, H.-Y., et al.: Conjunctival papilloma: Clinical features, outcome, and factors related to recurrence. Taiwan J Ophthalmol, 2018; 8 (1): 15–8.
5. Kaliki, S., Arepalli, S., Shields, C.L., et al.: Conjunctival papilloma: features and outcomes based on age at initial examination. JAMA Ophthalmol, 2013; 131 (5): 585–93.
6. Kalogeropoulos, C., Koumpoulis, I., Papadiotis, E., et al.: Squamous cell papilloma of the conjunctiva due to human papillomavirus (HPV): presentation of two cases and review of literature. Clin Ophthalmol Auckl NZ, 2012; 6 : 1553–61.
7. Kalogeropoulos, C., Moschos, M.: Advances in Diagnosis and Treatment of HPV Ocular Surface Infections. Med Hypothesis Discov Innov Ophthalmol, 2015; 4 (2): 31–5.
8. Manderwad, G.P., Kannabiran, C., Honavar, S.G., et al.: Lack of Association of High-Risk Human Papillomavirus in Ocular Surface Squamous Neoplasia in India. Arch Pathol Lab Med, 2009; 133 (8): 1246–50.
9. McDonnell, J.M., Mayr, A.J., Martin, W.J.: DNA of human papillomavirus type 16 in dysplastic and malignant lesions of the conjunctiva and cornea. N Engl J Med, 1989; 320 (22): 1442–6.
10. McDonnell, P.J., McDonnell, J.M., Kessis, T., et al.: Detection of human papillomavirus type 6/11 DNA in conjunctival papillomas by in situ hybridization with radioactive probes. Hum Pathol, 1987; 18 (11): 1115–9.
11. Minchiotti, S., Masucci, L., Serapiao Dos Santos, M., et al.: Conjunctival papilloma and human papillomavirus: identification of HPV types by PCR. Eur J Ophthalmol, 2006; 16 (3): 473–7.
12. Mlakar, J., Kocjan, B.J., Hošnjak, L., et al.: Morphological characteristics of conjunctival squamous papillomas in relation to human papillomavirus infection. Br J Ophthalmol, 2015; 99 (3): 431–6.
13. Naghashfar, Z., McDonnell, P.J., McDonnell, J.M., et al.: Genital tract papillomavirus type 6 in recurrent conjunctival papilloma. Arch Ophthalmol Chic Ill 1960, 1986; 104 (12): 1814–5.
14. Nakamura, Y., Mashima, Y., Kameyama, K., et al.: Detection of human papillomavirus infection in squamous tumours of the conjunctiva and lacrimal sac by immunohistochemistry,
in situ hybridisation, and polymerase chain reaction. Br J Ophthalmol, 1997; 81 (4): 308–13.15. Saegusa, M., Takano, Y., Hashimura, M., et al.: HPV type 16 in conjunctival and junctional papilloma, dysplasia, and squamous cell carcinoma. J Clin Pathol, 1995; 48 (12): 1106–10.
16. Sjö, N.C., von Buchwald, C., Cassonnet, P., et al.: Human papillomavirus in normal conjunctival tissue and in conjunctival papilloma: types and frequencies in a large series. Br J Ophthalmol, 2007; 91 (8): 1014–5.
17. Sjö, N.C., Heegaard, S., Prause, J.U., et al.: Human papillomavirus in conjunctival papilloma. Br J Ophthalmol, 2001; 85 (7): 785–7.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2018 Číslo 3- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Normotenzní glaukom: prevalence a zásady terapie
-
Všechny články tohoto čísla
- Ophthalmological finding in a patient with lowe syndrome
- Marshall and stickler syndrome in one family
- Congenital central toxoplasmic chorioretinitis - case study
- 24. výroční konference Eye Advance 2018
- Zemřela moje maminka, MUDr. Vlasta Doležalová, CSc.
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Conjuctival lesions - the relationship of papillomas and squamous cell carcinoma to HPV infection
- Ophthalmic manifestations of acute leukaemias
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ophthalmic manifestations of acute leukaemias
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Congenital central toxoplasmic chorioretinitis - case study
- Marshall and stickler syndrome in one family
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




