-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Cerebellar hydatid cyst – a rare case report
Cystická hydatidóza mozečku – vzácná kazuistika
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors: N. Jemel 1; G. Gader 1; K. Bahri 1; L. Rebaï 2; M. Rkhami 1; M. Badri 1; I. Zammel 1
Authors place of work: Department of Neurosurgery, Burns and, Trauma Center, Ben Arous, Tunisia 1; Department of Anesthesiology, Burns, and Trauma Center, Ben Arous, Tunisia 2
Published in the journal: Cesk Slov Neurol N 2020; 83(2): 203-204
Category: Dopis redakci
doi: https://doi.org/10.14735/amcsnn2020203Summary
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Dear editorial office,
Hydatid cyst (HC) or hydatidosis is a parasitic disease caused by the larval stage of Echinococcus granulosus tapeworms or cestodes [1,2]. It represents a major public health problem in developing countries [3]. Humans are accidental hosts with Echinococcus affecting primarily the liver and lungs. Only 1–2% of the cysts involve the brain. The cerebellar location is rare. Here we report the case with cerebellar involvement of Echinococcus granulosus.
A 31-year-old male without medical background presented with a 2-month history of gait disturbance, which increased in severity over the past weeks. He also reported a progressive left retroauricular headache without vomiting, fever or blurred vision. A detailed recollection of the history also revealed that the patient was in close contact with dogs as he lived in a rural environment. During neurological examination, the patient showed no deterioration in the level of consciousness. His gait was staggering, unsteady and wide-based with exaggerated difficulty in turns. The finger-nose test revealed dysmetria on the left upper limb. Deep tendon reflexes were exaggerated on the left side. These signs suggested static and kinetic cerebellar syndrome.
A brain MRI showed a left cerebellar cystic mass 34 mm in size with a thin layer of peripheral enhancement. The lesion compressed the fourth ventricle and the brainstem without hydrocephalus (Fig. 1).
Fig. 1. Sagittal, axial and coronal sections of a brain MRI on T1-WI after the administration of Gadolinium showing a left vermio-lobar cystic, homogenous, well-shaped lesion compressing the brain stem and the fourth ventricle.
Obr. 1. Sagitální, axiální a koronární řezy na MR mozku v T1 váženém obraze po aplikaci gadolina ukazují levostrannou vermio-lobární cystickou, homogenní, dobře ohraničenou lézi utlačující mozkový kmen a čtvrtou mozkovou komoru.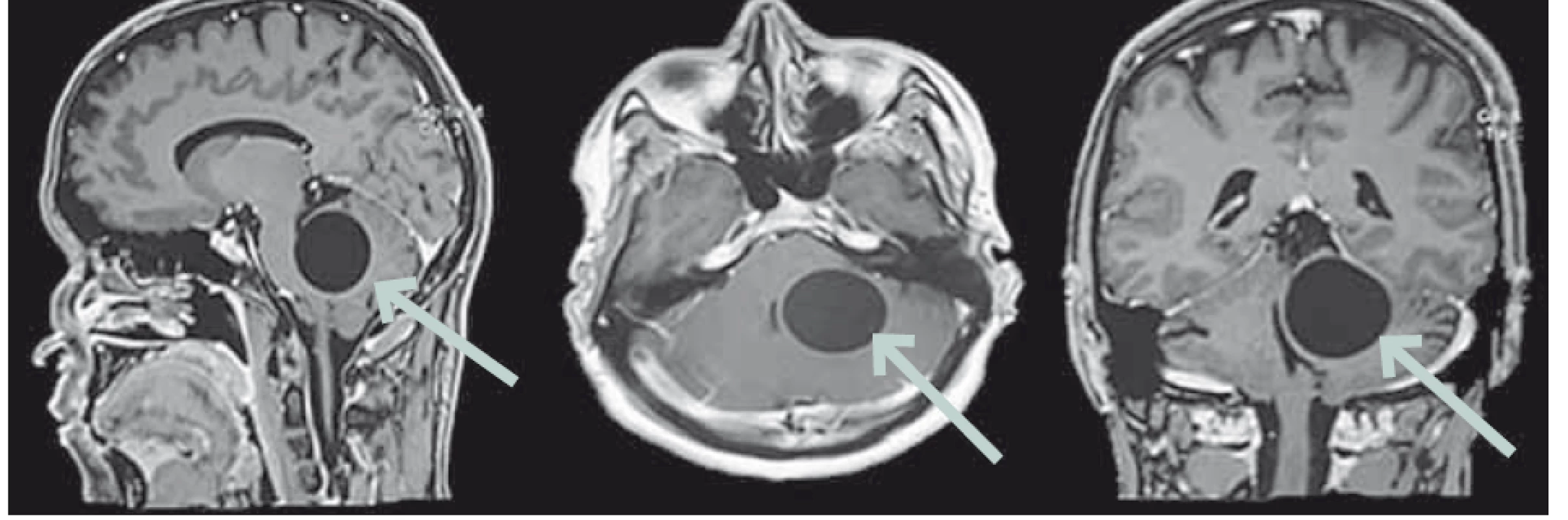
Neither biological tests nor chest X-ray and abdominal ultrasonography showed any abnormalities.
The patient underwent surgery for removal of the mass. He was placed in a park bench position. A suboccipital craniotomy extending from the midline to 2 cm over the left cerebellar hemisphere was performed. A transcortical transcerebellar approach ensured access to a deep and cystic lesion. Peroperatively, particular attention was paid to avoid cyst rupture because of the risk of dissemination of the cystic content through the basal cisterns and subarachnoid spaces. Due to the deep location of the cyst, a classic approach through Dowling’s technique associated with hydrodissection was not feasible. Instead, partial aspiration of the cyst contents through puncturing was performed to facilitate the extirpation of the cyst (Fig. 2). The lesion was totally removed. The postoperative course was uneventful, and the patient was discharged 5 days after surgery with moderate residual left kinetic cerebellar syndrome. Pathological examination of the cyst confirmed the preoperative presumption of a cerebellar hydatic cyst. Consequently, the patient received antiparasitic treatment with albendazole 400 mg twice a day during 1 month. Postoperative follow-up of 1 year did not show any clinical or radiological signs of recurrence.
Fig. 2. Peroperative photo showing the removal of the cyst after aspiration of its content.
Obr. 2. Peroperační fotografi e ukazující odstranění cysty po aspiraci jejího obsahu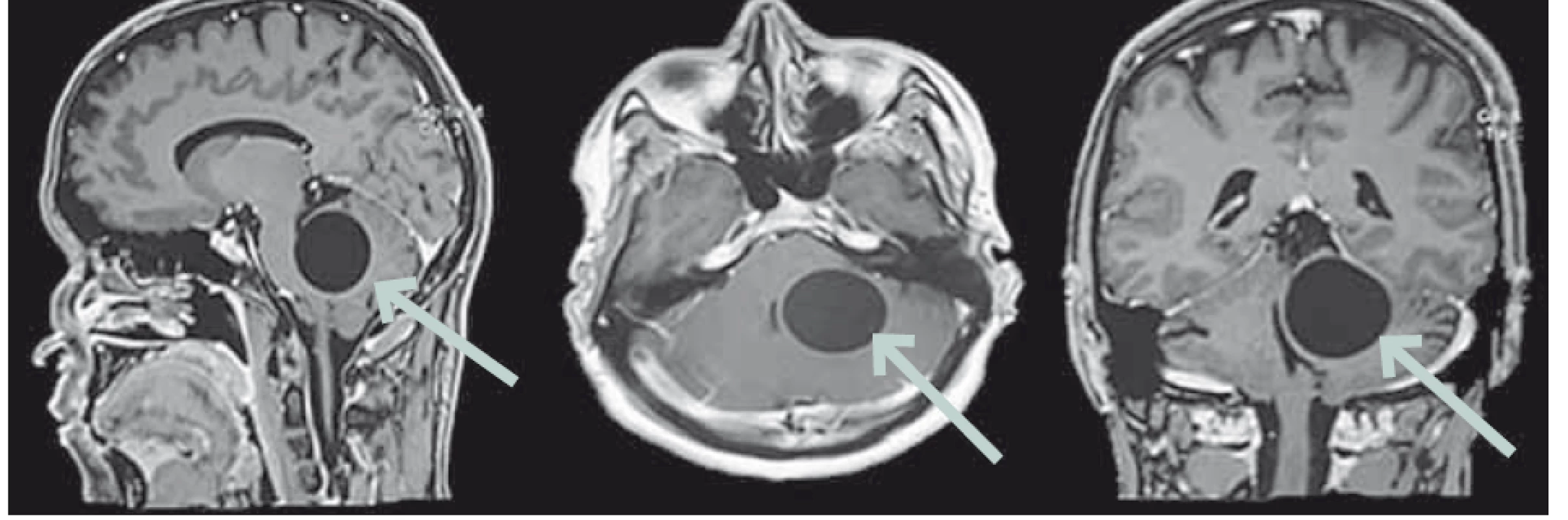
Hydatid disease is a zoonosis caused by encysted larvae of Echinococcus granulosus. It is endemic in the Middle East, Mediterranean countries, South America, North Africa and Australia, especially in rural areas [1]. Human contamination occurs accidentally through direct contact with dogs or by the ingestion of contaminated food. Frequent locations are hepatic (48%) and pulmonary (36%). Cerebral localization is rare and does not exceed 2% of cases [2–6]. The infrequent cerebral location of echinococcus is related to the passage of the parasite through two barriers (hepatic and pulmonary) before reaching the great circulation [3]. Cerebral HC is more common in the paediatric population, most likely related to patent ductus arteriosus [4]. Intracranial HC is mostly located in the supratentorial compartment, especially in the middle cerebral artery territory. The location in the posterior fossa is unusual [5–7]. All anatomical compartments of the posterior fossa can be concerned: cerebellar vermis and hemispheres, pons, fourth ventricle or even extradural. The growth of HC is usually slow, asymptomatic and clinical manifestations are usually the consequence of compression of the involved organ [6,8]. Hydrocephalus can also be observed either in cases of cysts located near the ventricular system, which may block the flow of the cerebrospinal fluid, or in the event of the rupture of the cyst in the subarachnoid space [5]. The mean growth rate of HC is between 1 and 10 cm per year [5,9]. Solitary intracranial HC are more common than multiple lesions. Multiple HC are found mainly in patients previously operated upon for such lesions, and whose procedures were complicated by a rupture of the cyst with dissemination of the cystic content in the subarachnoid space [9,10]. The typical radiological appearance of a HC is a spherical, well defined, thin-walled, homogeneous and non-enhancing cystic lesion without peripheral oedema [3,10]. On MRI, HC is hypointense on T1-WI and hyperintense on T2-WI. Considering a particular epidemiological context, these radiological features may orientate towards the diagnosis of HC, but do not provide specific elements for differential diagnosis of other intracranial cystic lesions. Infratentorial HC do not have any radiological specificities compared to the supratentorial ones, due to the fact that they are generally diagnosed in a smaller size as they manifest by clinical symptoms earlier [2]. Radical excision must be performed for all accessible surgical lesions [10]. The usual surgical procedure consists of extirpation of the cyst while preserving the integrity of the wall, through saline irrigation between the cyst wall and the adjacent nerve tissue. This approach is usually possible because of minimal adhesions around the cyst wall. Aspiration of the cyst contents through puncturing during the surgery is indicated for deep-seated cysts. In our case, the cyst was punctured, partially aspirated and then carefully extirpated. In the event of intraoperative rupture, hypertonic saline serum is used for its scolicidal effect in order to minimize the risk of local recurrence and dissemination [10]. Medical treatment using anthelminthics such as albendazole is always indicated postoperatively to reduce the risk of recurrence. However, controversies remain regarding the dose and duration of the treatment [10].
Cerebellar HC is an uncommon disease, very rare in forms located in the posterior fossa. Nevertheless, it should be considered in the differential diagnosis of posterior fossa cysts, mainly in endemic countries. Surgery is the treatment of choice and a surgical approach must be considered, depending on the location of the cyst.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Ghassen Gader, MD
Department of Neurosurgery
Burns and Trauma Center
Ben Arous
Tunisia
e-mail: gastghagad@yahoo.frAccepted for review: 30. 9. 2019
Accepted for print: 13. 1. 2020
Zdroje
1. Fakhouri F, Ghajar A, Mahli N et al. Shoumal giant hydatid cyst in the posterior fossa of a child. Asian J Neurosurg 2015; 10 (4): 322–324. doi: 10.4103/1793-5482.162 719.
2. Yeola-Pate M, Banode P, Bhole A et al. Different locations of hydatid cysts: case illustrations and review of literature. Infect Clin Pr 2008; 16 (1): 379–384.
3. Tlili-Graiess K, El Ouni F, Gharbi-Jemni H et al. Hydatidose cérébrale: aspects en imagerie. J Neuroradiol 2006; 33 (5): 304–318. doi: 10.1016/s0150-9861 (06) 77288-1.
4. Basraoui D, El Idrissi I, Jalal H et al. Kystes hydatiques cérébraux de l’enfant (à propos de 9 cas). J Radiol 2010; 91 (1): 293–296.
5. Lakhdar F, Arkha Y, Bougrine M et al. Kyste hydatique intra-et extracrânien de la fosse cérébrale postérieure (à propos d’un cas). J Neurochir 2010; 56 (5): 391–394. doi: 10.1016/j.neuchi.2010.01.001.
6. Braham E, Bellil S, Bellil K et al. Kyste hydatique de la fosse postérieure. Med Mal Infect 2007; 37 (5): 281–283. doi: 10.1016/j.medmal.2007.03.001.
7. Kayaoglu C. Giant hydatid cyst in the posterior fossa of a child: a case report. J Int Med Res 2008; 36 (1): 198–202. doi: 10.1177/147323000803600125.
8. Is M, Gezen F, Akyuz F et al. A 13-year-old girl with a cystic cerebellar lesion: consider the hydatid cyst. J Clin Neurosci 2009; 16 (5): 712–713. doi: 10.1016/j.jocn.2008.07.083.
9. Shahlaie K, Hawk MW, Hu BR et al. Parasitic central nervous system infections: echinococcus and schistosoma. Rev Neurol Dis 2005; 2 (4): 176–185.
Štítky
Dětská neurologie Neurochirurgie Neurologie
Článek vyšel v časopiseČeská a slovenská neurologie a neurochirurgie
Nejčtenější tento týden
2020 Číslo 2- Magnosolv a jeho využití v neurologii
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Zolpidem může mít širší spektrum účinků, než jsme se doposud domnívali, a mnohdy i překvapivé
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- Vascular morphology, symptoms, diagnostics and treatment of brainstem ischemic stroke
- Is the concept of vascular dementia sustainable? YES
- Is the concept of vascular dementia sustainable? NO
- Is the concept of vascular dementia sustainable? COMMENT
- The International Classification of Headache Disorders (ICHD-3) – the official Czech translation
- Schwannoma of the extracranial part of the trigeminal nerve
- Surgical treatment of brain metastases
- Cavum septi pellucidi, cavum vergae and cavum veli interpositi
- Cerebrospinal fluid ratio of phosphorylated tau protein and beta amyloid predicts amyloid PET positivity
- Provocative factors and treatment response in juvenile myoclonic epilepsy – experience from a tertiary epilepsy center
- Surgical treatment of benign mediastinal neurogenic tumors – a 7-year analysis
- Transcranial sonography of the medial temporal lobe in Alzheimer’s disease patients
- Endarterectomy of the external carotid artery
- Vestibular function in patiens with cochlear implant
- Cerebellar hydatid cyst – a rare case report
- A case of late brachial plexopathy after chemotherapy and radiotherapy
- Spontaneous vaginal extrusion of the distal catheter of a ventriculoperitoneal shunt
- Repeated thrombectomy in a patient with a rare combination of etiological factors
- Dopis redakci
- Komentář redakce
- Prof. Mraček oslavil 90 let
- Odešla MUDr. Olga Baudyšová
- K jubileu profesorky Soni Nevšímalové
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Cavum septi pellucidi, cavum vergae and cavum veli interpositi
- Vascular morphology, symptoms, diagnostics and treatment of brainstem ischemic stroke
- The International Classification of Headache Disorders (ICHD-3) – the official Czech translation
- Surgical treatment of brain metastases
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



