-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Validation of the Slovak Version of the SIBDQ Questionnaire in a Cohort of Inflammatory Bowel Disease Patients
Právoplatnosť slovenskej verzie dotazníka SIBDQ v kohorte pacientov s idiopatickými střevními záněty
Východiská: Zápalový dotazník o ochoreniach hrubého čreva (IBDQ – inflammatory bowel disease questionnaire) je široko používaný dotazník na hodnotenie kvality života u pacientov so zápalovým ochorením čriev (IBD – inflammatory bowel disease). Hoci bol tento dotazník prijatý a potvrdený v niekoľkých jazykoch, ešte nebol potvrdený v slovenskom jazyku.
Ciele: Cieľom tejto štúdie bolo aplikovať metódy a kritériá používané v niekoľkých adaptačných štúdiách na posúdenie platnosti a spoľahlivosti prispôsobeného IBDQ.
Metódy: V tejto prierezovej štúdii sme zhromaždili dáta pomocou 90 dotazníkov IBD (ulcerózna kolitída (UC) 39 a Crohnova choroba (CD) 51 dotazníkov) od 82 po sebe nasledujúcich pacientov z centra IBD v Ružinovskej fakultnej nemocnici v Bratislave. Všetkým pacientom boli poskytnuté tri dotazníky: krátka forma IBD dotazníka (SIBDQ – short inflammatory bowel disease questionnaire), prieskum Short Form (SF-36), Harvey-Bradshawov index (HBI) u pacientov s CD a parciálneho Mayo Score (pMayo) u pacientov s UC. Na základe údajov sme hodnotili slovenskú verziu SIBDQ pre platnosť s použitím miery konvergencie Pearsonova korelačného koeficientu, spoľahlivosť pomocou Cronbachovho interného testu konzistencie a prijateľnosti a zrozumiteľnosti jazyka pomocou stupnice Likert.
Výsledky: Slovenská verzia SIBDQ bola tiež vysoko korelovaná v porovnaní s SF-36 (UC r = 0,87 a CD r = 0,81; oba s p < 0,01), HBI (CD r = – 0,82; p < 0,01) a pMayo (UC r = –0,86; p < 0,01). Spoľahlivosť slovenskej verzie SIBDQ bola veľmi významná u UC (Cronbachov alfa koeficient 0,96 pre zložku klinickej prezentácie a 0,85 pre zložku sociálneho obmedzenia) a CD (0,92 pre zložku klinickej prezentácie a 0,84 pre zložku sociálneho obmedzenia). Percento akceptovateľnosti všetkých dotazníkov SIBDQ u UC a CD pacientov zostalo konštantné na 100 %. Zrozumiteľnosť jazyka bola hodnotená sedembodovou stupnicou Likert, v ktorej sa zistilo, že 93,15 % pacientov súhlasilo s tým, že dotazník bol jazykovo správny a zrozumiteľný.
Záver: Slovenská verzia SIBDQ je platný, spoľahlivý a vysoko prijateľný nástroj na meranie kvality života pacientov s UC a CD.
Klíčová slova:
SIBDQ – ulcerózna kolitída – zápalová choroba čriev – SF-36 – pMayo – HBI
Authors: Jalali Y; Sturdik I.; Adamcová M.; Krajcovicova A.; Huorka M.; Payer J.; Hlavaty T.
Authors place of work: -5th Department of Internal Medicine Faculty of Medicine Comenius University and University Hospital Bratislava, Slovak Republic
Published in the journal: Gastroent Hepatol 2019; 73(2): 138-142
Category: IBD: původní práce
doi: https://doi.org/10.14735/amgh2019138Summary
Background: The Short Inflammatory Bowel Disease Questionnaire (SIBDQ) is a widely used questionnaire for health-related quality of life assessment in patients with inflammatory bowel disease (IBD). Although this questionnaire has been adopted and validated in several languages, it has not yet been validated in the Slovak language.
Aims: The aim of this study was to apply the methods and criteria used by several adaptation studies for assessing the validity and reliability of the adapted SIBDQ.
Methods: In this cross-sectional study, we collected data using 90 IBD questionnaires (ulcerative colitis (UC) 39 and Crohn’s disease (CD) 51 questionnaires) from 82 consecutive patients from the IBD centre at the Ružinov University Hospital in Bratislava. All patients were given three questionnaires: SIBDQ, Short Form survey (SF-36), Harvey-Bradshaw index (HBI) for CD patients and partial Mayo Score (pMayo) score for UC patients. Based on the data, we assessed the Slovak version of the SIBDQ for validity using the convergence rate of the Pearson correlation coefficient, reliability using Cronbach’s alpha internal consistency test, and acceptance and linguistic understandability using the Likert scale.
Results: The Slovak version of the SIBDQ was also highly correlated when compared to SF-36 (UC r = 0.87 and CD r = 0.81; both with p < 0.01), HBI (CD r = – 0.82; p < 0.01), and pMayo (UC r = – 0.86; p < 0.01). Reliability of the Slovak version of the SIBDQ was highly significant in both UC (Cronbach’s alpha coefficient was 0.96 for clinical presentation component and 0.85 for psychosocial limitation component) and CD (0.92 for clinical presentation component and 0.84 for psychosocial limitation component). Acceptability percentage of all SIBDQ questionnaires in UC and CD patients stayed constant at 100%. Linguistic understandability was evaluated with a seven-point Likert scale, which found that 93.15% of the patients strongly agreed that the questionnaire was linguistically understandable.
Conclusion: The Slovak version of the SIBDQ is a valid, reliable, and highly acceptable instrument to measure quality of life of patients with UC and CD.
Keywords:
SIBDQ – Ulcerative colitis – inflammatory bowel disease – SF-36 – pMayo – HBI
Introduction
Health-related quality of life (HRQoL) is a measure commonly used in questionnaires to assess a patient’s perception of the impact of their disease on daily function. HRQoL instruments must include several properties to be useful, including acceptability, reliability, and validity [1]. Mitchell et al. [2] and Guyatt et al. [3] designed and validated the Inflammatory Bowel Disease Questionnaire (IBDQ), an IBD-specific HRQoL for patients with ulcerative colitis (UC) and Crohn‘s disease (CD). For more convenient daily clinical use, Love et al. [4] developed a short version of the questionnaire (SIBDQ). The application of the SIBDQ in patients with UC and CD has shown good reproducibility and better responsiveness than general health status measures [2–4].
The SIBDQ was designed and validated for a specific language and culture. The translation of this questionnaire into another language might impair its validity, even if the translation was comprehensive [5]. Therefore, translated questionnaires still require revalidation to demonstrate their conceptual equivalency to the original [6]. The SIBDQ has already been validated in the languages of many European countries (Spain, Great Britain, Germany, Sweden, Denmark, Norway, Belgium, The Netherlands, Greece, Portugal, and Italy). Our aim was to investigate the validity, reliability, linguistic understandability, and acceptance of the Slovak version of the SIBDQ.
Materials and methods
In this cross-sectional study, a cohort of 82 IBD patients from the IBD centre at the Ružinov University Hospital in Bratislava were randomly selected. Subjects consisted of all consecutive eligible patients arriving at the IBD centre. We included data from 90 IBD questionnaires (51 CD and 39 UC patients). Patients were handed three questionnaires: the SIBDQ, Short form (SF-36), and HBI (Harvey-Bradshaw index) for CD patients or partial Mayo Score (pMayo) (for UC patient) at the time of their visit. The patients included in our study were in various stages of IBD or in remission. We determined the validity of the questionnaire data using the convergence correlation test with other relative indices of clinical activity (namely HBI for CD patients and pMayo for UC patients) for clinical components of the disease, and the SF-36 for the psychosocial limitation components of the disease. Data collected from the SIBD questionnaires were assessed for reliability using the internal consistency test (Cronbach alpha), evaluated separately for the clinical and psychosocial limitation component of the questionnaire. Acceptance of the questionnaire was assessed by examining the percentage of questions answered. Linguistic understandability was tested with a seven-point Likert test. We used Microsoft Excel for the data collection and analysis.
Results
Patient Characteristics
Patient characteristics, including demographic data and disease state, are summarised in Tab. 1.
Graph 1. Negative linear correlation between SIBDQ clinical presentation component, pMayo score and Harvey-Bradshaw index.
Graf 1. Negatívne lineárna korelácia medzi zložkou klinickej prezentácie v SIBDQ, skóre pMayo a Harvey-Bradshaw index.
SIBDQ – short inflammatory bowel disease questionnaire, UC – ulcerative colitis, pMayo – partial Mayo score, HBI – Harve-Bradshaw index, CD – Crohn’s disease Tab. 1. Demographic data and disease state of patients.
Tab. 1. Demografické údaje a chorobný stav pacientov.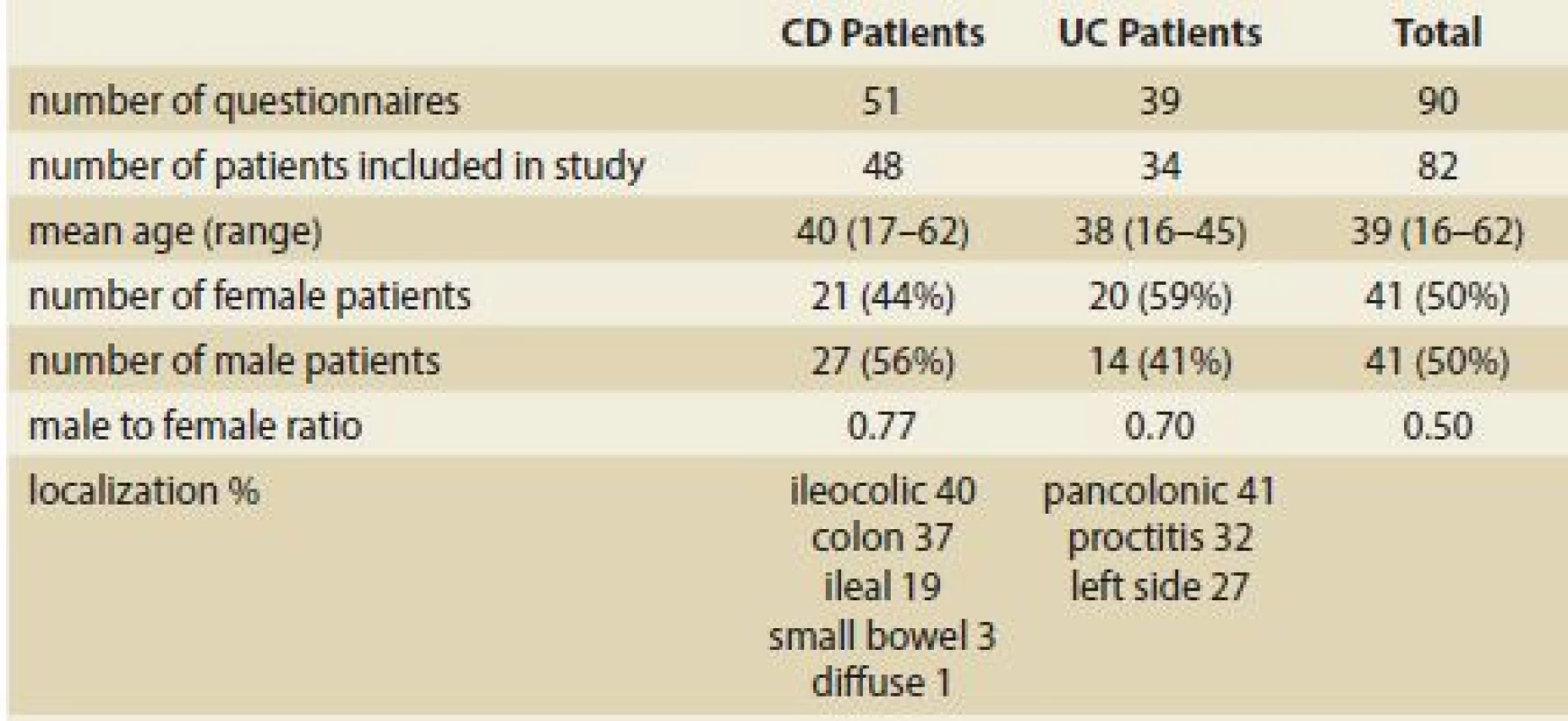
UC – ulcerative colitis, CD – Crohn’s disease Reliability
For the SIBDQ data from CD patients, Cronbach’s coefficient was 0.92 for the clinical presentation component and 0.84 for the psychosocial limitation component. For the SIBDQ data from UC patients, Cronbach’s coefficient was 0.96 for the clinical presentation component and 0.85 for the psychosocial limitation component. All relative data are summarised in Tab 2.
Tab. 2. Cronbach’s coeficient for the clinical and psychosocial components of the SIBDQ completed by Crohn´s disease and ulcerative colitis patients.
Tab. 2. Cronbachov koeficient pre klinické a psychosociálne zložky SIBDQ vyplneného pacientmi s Crohnovou chorobou a ulceróznou kolitídou.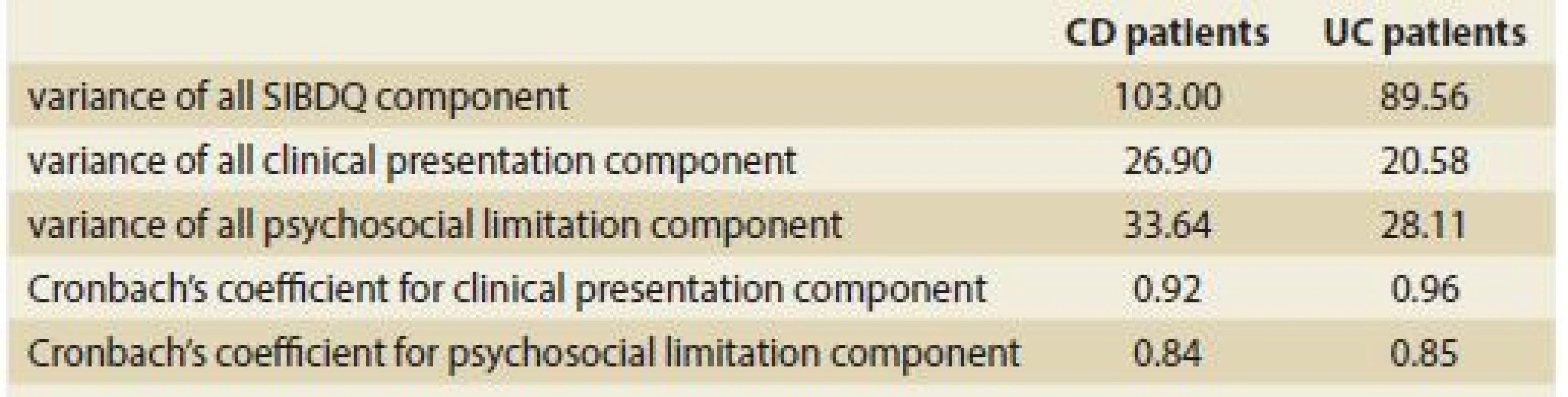
UC – ulcerative colitis, SIBDQ – Short Infl ammatory Bowel Disease Questionnaire, CD – Crohn’s disease Acceptability and Language understandability
The acceptability percentage for the SIBDQ in UC and CD patients was 100%. The seven-point Likert test, used to evaluate linguistic understandability, showed that 93.2% of the patients strongly agreed that the questionnaire was linguistically understandable.
Convergence Validity
Pearson correlation coefficients between the SIBDQ, clinical indices (pMayo and HBI), and psychosocial questionnaire SF-36 were calculated separately for UC and CD patients. As shown in Tab. 3, the correlations between the clinical presentation component of the SIBDQ and the disease activity indices, psychosocial limitation component and SF-36 were statistically significant (P < 0.01). Correlations between the SIBDQ clinical presentation component and clinical indices of activity (namely pMayo and HBI) were large for both UC (r = – 0.86; p < 0.01) and CD (r = – 0.82; p < 0.01) (Graph 1) patients. Similarly, we found large correlations between the psychosocial limitation component of the SIBDQ and the SF-36 (UC: r = 0.87 and CD: r = 0.81; both p < 0.01) (Graph 2A and 2B). Correlations between the clinical presentation component and psychosocial limitation component of the SIBDQ questionnaires were large for UC (r = 0.84) and CD (r = 0.70) patients (Tab. 3).
Tab. 3. Pearson correlation coeficient between the SIBDQ and Harvey-Bradshaw index, pMayo score, and Short Form SF-36.
Tab. 3. Pearsonův korelační koeficient mezi SIBDQ a Harvey-Bradshaw indexem, pMayo skóre a Short Form SF-36.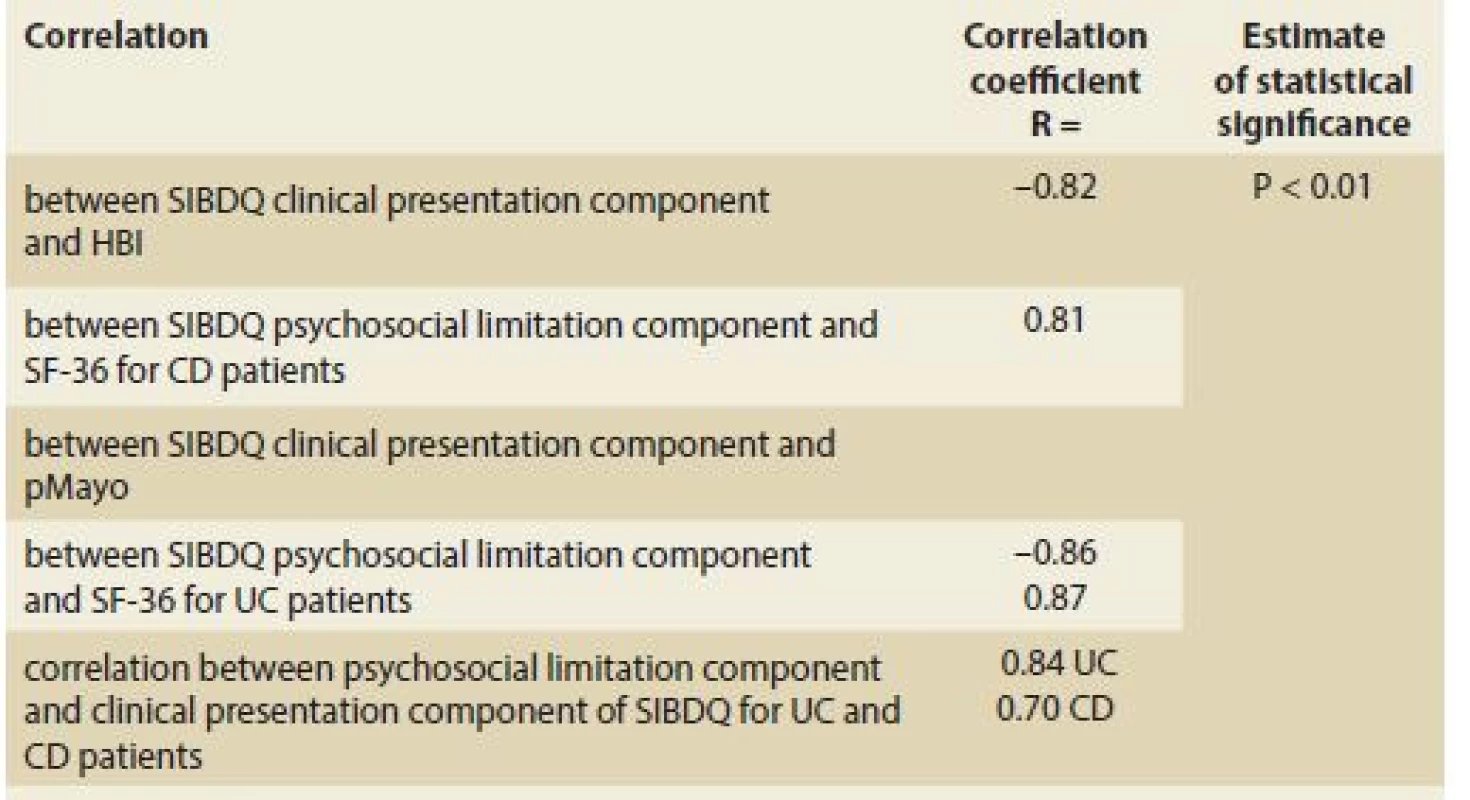
(R) – Pearson coefficient, CD – Crohn’s disease, UC – ulcerative colitis, SIBDQ – Short Inflammatory Bowel Disease Questionnaire, SF-36 – Short Form survey, pMayo – partial Mayo score, HBI – Harvey Bradshaw index Graph 2. Linear correlation between the SIBDQ and SF-36 in ulcerative colitis and Crohn’s disease patients, respectively.
Graf 2. Lineárna korelácia medzi SIBDQ a SF-36 u pacientov s ulceróznou kolitídou a Crohnovou chorobou.
SIBDQ – short inflammatory bowel disease questionnaire, UC – ulcerative colitis, SF-36 – Short Form, CD – Crohn’s disease Discussion
The present study analysed the psychosocial limitation and clinical presentation properties of the Slovak version of the SIBDQ. The results of our study suggest that the Slovak version of the SIBDQ has good convergence validity, reliable internal consistency, acceptability, and linguistic understandability. The validity results of the SIBDQ are similar for UC and CD patients, which suggests that the Slovak version of the SIBDQ is an equally appropriate clinical tool to measure the HRQoL in IBD patients in Slovakia. The SIBDQ has already been successfully validated and translated into several other languages without loss in content validity, reproducibility, and responsiveness [7–9].
When comparing our results with those described by other authors, some methodological differences should be considered. For instance, the studies may differ in the Likert scale range used (5-vs. 7-point) [7] and whether the 32-item IBDQ or the SIBDQ version is used [8]. To test the validity of the Slovak version of the SIBDQ, we compared our questionnaire with clinical indices of activity (namely HBI for CD patients and pMayo for UC patients) for clinical presentation, and with the SF-36 questionnaire for psychosocial limitation of the disease. In both UC and CD patients, the clinical presentation component and psychosocial limitation component of the SIBDQ was well correlated (with statistical significance P < 0.01) with clinical indices and scores of SF-36 (correlation coefficient of r = – 0.82 between SIBDQ and HBI; 0.81 between SIBDQ and SF-36 in CD patients; – 0.86 between SIBDQ and pMayo; and 0.87 between SIBDQ and SF-36 for UC patients). In our study, the internal consistency reliability coefficient was high for both clinical presentation and psychosocial limitation component in both UC and CD patients (namely Cronbach’s coefficient of 0.92 for clinical presentation and 0.84 for psychosocial limitation in CD patients and 0.96 for clinical presentation and 0.85 psychosocial limitation in UC patients). Considering that internal consistency coefficients above 0.84 are generally accepted as satisfactory [10], our results suggest that the Slovak version of the SIBDQ has excellent internal consistency for both UC and CD patients. Our data show that the Slovak version of the SIBDQ has a high rate of acceptability and linguistic understandability for IDB patients.
In conclusion, the results of the validation of the Slovak version of the SIBDQ support its validity, reliability, acceptability, and linguistic understandability. In addition, our study shows that the high clinical presentation properties of the test are comparable for UC and CD patients. Therefore, the test can be applied for the measurement of the HRQoL in either disease.
Submitted: 20. 11. 2018
Accepted: 3. 2. 2019
MUDr. Yashar Jalali
5th Department of Internal Medicine
Faculty of Medicine, Comenius University and University Hospital Bratislava
Ruzinovska 6
826 06 Bratislava
Slovak Republic
Zdroje
1. Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med 1993; 118 (8): 622–629.
2. Mitchell A, Guyatt G, Singer J et al. Quality of life in patients with inflammatory bowel disease. J Clin Gastroenterol 1988; 10 (3): 306–310.
3. Guyatt G, Mitchell A, Irvine EJ et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 1989; 96 (3): 804–810.
4. Love JR, Irvine EJ, Fedorak RN. Quality of life in inflammatory bowel disease. J Clin Gastroenterol 1992; 14 (1): 15–19.
5. Badía X, García-Losa M, Dal-Ré R. The language translation and harmonization of the International Prostate Symptom Score: developing a methodology for multinational clinical trials. Eur Urol 1997; 31 (2): 129–140.
6. Patrick DL, Wild DJ, Johnson ES et al. Cross-cultural validation of quality of life measures. In: Orley J, Kuykev W (eds). Quality of life assessment. Berlin: Springer 1995 : 19–32.
7. de Boer AG, Wijker W, Bartelsman JF. Inflammatory Bowel Disease Questionnaire: cross-cultural adaptation and further validation. Eur J Gastroenterol Hepatol 1995; 7 (11): 1043–1050.
8. Russel MG, Pastoor CJ, Brandon S et al. Validation of the Dutch translation of the Inflammatory Bowel Disease Questionnaire (IBDQ): a health-related quality of life questionnaire in inflammatory bowel disease. Digestion 1997; 58 (3): 282–288.
9. Kalafateli M, Triantos C, Theocharis G et al. Health-related quality of life in patients with inflammatory bowel disease: a single-center experience. Ann Gastroenterol 2013; 26 (3): 243–248.
10. McDowell I, Neweell C. The theoretical and technical foundations of health measurement. In: McDowell I, Neweell C (eds). Measuring Health: a guide to rating scales and questionnaires. New York: Oxford University Press 1987 : 12–35.
Štítky
Dětská gastroenterologie Gastroenterologie a hepatologie Chirurgie všeobecná
Článek vyšel v časopiseGastroenterologie a hepatologie
Nejčtenější tento týden
2019 Číslo 2- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
-
Všechny články tohoto čísla
- Kvíz z klinické praxe
- Clinical practice guidelines for chronic hepatitis C virus infection
- Laparoscopic liver resection for alveolar echinococcosis
- Inflammatory bowel disease and male fertility
- Ectopic pancreas as a cause of upper gastrointestinal bleeding
- Validation of the Slovak Version of the SIBDQ Questionnaire in a Cohort of Inflammatory Bowel Disease Patients
- A gastric Dieulafoy’s lesion
- Involvement of the gastrointestinal tract in amyloidosis: when to think about it and how to diagnose
- Part 2 – Epidemiology of inflammatory bowel diseases in the Czech population: available data sources, prevalence of treated patients and overall mortality
- The selection from international journals
- 23rd Days of Gastroenterology and Hepatology and 13th International Endoscopic Workshop in Hradec Kralove
- 5th IBD working days, Hořovice 2019
- Kreditovaný autodidaktický test
- Správná odpověď na kvíz
- Biosimilar adalimumab FKB327 (Hulio®)
- Editorial
- Vzácní a výjimeční jubilanti
- Gastroenterologie a hepatologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- A gastric Dieulafoy’s lesion
- Involvement of the gastrointestinal tract in amyloidosis: when to think about it and how to diagnose
- Ectopic pancreas as a cause of upper gastrointestinal bleeding
- Inflammatory bowel disease and male fertility
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



