-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Evaluation of adherence to treatment in patients suffering from diabetes mellitus
Hodnotenie adherencie k liečbe u pacientov trpiacich diabetes mellitus
Úvod: Diabetes mellitus 2. typu (DM) je ochorenie, ktoré v súčasnosti nadobúda pandemický charakter. Základom úspešnej terapie tohto ochorenia je predovšetkým včasná diagnostika a vhodne nastavená liečba. Rovnako ako úloha lekára v terapii ochorenia je potrebná aj iniciatívnosť a snaha motivovať pacienta k dodržiavaniu jednotlivých režimov zo strany verejného lekárnika.
Cieľ: Cieľom výskumu bolo zanalyzovať a vyhodnotiť dodržiavanie farmakologickej a nefarmakologickej liečby u pacientov trpiacich diabetes mellitus a možnosti ovplyvnenia zo strany verejného lekárnika.
Metodika: Informácie potrebné k vyhodnoteniu sme získali prostredníctvom anonymného dotazníkového prieskumu realizovaného za obdobie 7 mesiacov a na základe osobných konzultácií lekárnika s pacientom.
Výsledky: Prieskumu sa zúčastnilo 117 respondentov, z toho 67 (57 %) žien a 50 (43 %) mužov. Najväčšie zastúpenie mali respondenti vo veku 60 – 74 rokov (48 %). Až 84 % respondentov trpelo diabetes mellitus 2. typu. Čo sa týka dodržiavania nefarmakologickej liečby (režimových a diétnych opatrení) väčšina respondentov či už pri porovnaní vzhľadom na pohlavie (96 % žien a 76 % mužov), alebo vzhľadom na vek (v každej vekovej kategórii nad 80 %) uviedla, že uvedené opatrenia dodržiavajú. Pri farmakologickej liečbe až 83 % žien a 79 % mužov dodržiavalo stanovenú farmakologickú liečbu. Takisto aj po vyhodnotení vzhľadom na vek bolo zistené, že v každej vekovej kategórii (okrem respondentov vo veku od 75 a viac rokov) stále dodržiavalo stanovenú farmakologickú liečbu viac než 70 % respondentov, vo veku od 60 do 74 rokov to bolo až 88 % respondentov. Čo sa týka hladiny glykémie nalačno u 49 % žien a 38 % mužov bola menej ako 7 mmol/l. Celkovo u 10 % pacientov na základe pravidelných konzultácii s lekárnikom prišlo k zlepšeniu hladín glykémie nalačno.
Záver: Na základe získaných výsledkov môžeme konštatovať, že v našej vybranej vzorke väčšina pacientov dodržiavala farmakologickú aj nefarmakologickú liečbu. Pri zlepšení adherencie k liečbe zohráva dôležitú úlohu aj lekárnik. Prostredníctvom poskytovania odborných vedomostí a znalostí pacientom pri výdaji lieku alebo poskytovaním individuálnych konzultácií pacientov môže lekárnik motivovať pacienta k dodržiavaniu nielen farmakologickej, ale aj nefarmakologickej liečby a tým zvýšiť aj samotnú adherenciu pacienta k liečbe.
Klíčová slova:
verejný lekárnik – diabetes – liečba – self-monitoring
Authors: Lucia Masaryková; Tomáš Tesař; Ubica Lehocká; Klaudia Bernáthová
Authors place of work: Department of Organisation and Management of Pharmacy, Faculty of Pharmacy, Comenius University in Bratislava
Published in the journal: Čes. slov. Farm., 2020; 69, 67-74
Category: Původní článek
Summary
Background: Diabetes mellitus type 2 (DM) is a disease which is becoming pandemic these days. A successful treatment of chronic diabetes mellitus depends on early diagnosis and proper treatment. Just as the role of the doctor in treating the disease is important, so the community pharmacist plays an important role in taking the initiative in motivating patients to adhere to individual treatment regimes.
Objective: The main aim of the study was to analyze and assess patient adherence to pharmacological or non-pharmacological treatment, including the influence of the community pharmacist on that.
Method: All necessary data for the assessment were collected by anonymous questionnaire survey methods conducted within 7 months, as well as by personal consulting among pharmacists and patients. The results were assessed according to patients’ gender and age.
Results: 117 respondents got involved in the survey, with 67 (57%) females and 50 (43%) males. The majority were aged 60–74 (48%), 84% suffered from diabetes mellitus type 2. Adherence to non-pharmacological treatment (regime and dietary measures) was 96% in females and 76% in males according to gender, and over 80% in each age category. Adherence to pharmacological treatment was up to 83% in females and 79% in males. According to age, over 70% adhered to pharmacological treatment all the time in each age category (except for 75+), with up to 88% aged 60–74.
Conclusion: According to the outcomes, we can observe that in our selected sample of patients the majority followed pharmacological or non-pharmacological treatment. The pharmacist also plays an important role in improving adherence to treatment. By providing patients with their expertise and professional knowledge while drug dispensing or individual conselling, the pharmacist can motivate the patient to follow not only pharmacological but also non-pharmacological treatment and thereby increase patient adherence itself to treatment.
Keywords:
diabetes – treatment – community pharmacist – self-monitoring
Introduction
Diabetes is a chronic disease, which can be treated and controlled effectively but cannot be totally cured. Diabetes mellitus type 2 is a disease which is becoming pandemic these days. According to the latest data given by the International Diabetes Federation (IDF) for 2017, approximately 425 million people (20–79 years) have diabetes worldwide. It is estimated that there will be 629 million diabetes cases worldwide by 20451). According to the NHANES, there is one diagnosed case of diabetes mellitus type 2 for one undiagnosed2). When compared to 2003, there were over 60,000 treated diabetics in the Slovak republic (SR) in 2013, which was a rise of 17.6%. On 31 December 2016 there were 368,084 people with diabetes mellitus in continuing healthcare, which was 6,772.0 patients per 100,000 inhabitants. Women represented 53.4% of all the patients. Most of the patients in continuing healthcare were those with DM type 2 (91.0%), followed by those with DM type 1 (7.3%), other types of DM (1.1%), and gestational DM (0.6%)3).
The role of the pharmacist in treating diabetes sufferers
The main goal of pharmaceutical care for diabetes sufferers is to prevent possible complications of treatment and minimize the risk of complications of diabetes mellitus. Of course, this requires a good knowledge of pathophysiology and diagnostics and strategy of diabetes treatment. The pharmacist is not only responsible for a proper drug dispensing and dosing, but also plays an important role in monitoring and motivating patients to comply with their pharmacological and regime treatment, as well as in revealing other risk factors (dyslipidemia, hypertension, smoking, etc.)4). The pharmacist may, within pharmaceutical care for diabetics, contribute to a maximum effect of prescribed therapies (for example an optimum dose of drugs and their timing within the day, a good strategy of medication-taking in relation to food, a proper administration of drugs, monitoring therapy goals and so on). Also, the pharmacist can reduce risks of the therapy (for example the management of drug interactions and adverse reactions, the identification and prevention of non-adherence, and the minimization of inadequate self-treatment). So pharmacists and other health professionals may dramatically contribute to normal levels of glycaemia and prevent diabetes-related complications from developing.
In Slovakia approximately every tenth pharmacy - goer is a diabetic. As for elderly patients, it is now even every third or so, and it is estimated that this number will rise. These people do not always confide their pains and symptoms to doctors but they may do so to pharmacists. The pharmacist is able to reveal the risk of diabetes or diabetes cases even from prescribed and over-the-counter drugs, as well as from various food supplements, vitamins or artificial sweeteners that the patient buys. Developing diabetes mellitus is common, for example when having hypertension for a few years. As for latent forms of diabetes mellitus, there are often signs of various skin infections and diseases. Patients who haven’t been diagnosed with diabetes mellitus type 2 yet may often buy dermatology products for infectious or mycotic skin diseases, food supplements and teas for dysuria or pollakiuria. Also, buying products that can alleviate gum inflammation may be a sign of diabetes. It’s very important to register such health conditions when dispensing antihypertensive drugs to a hypertensive patient. Generally, hypertensive people are the most predisposed to develop diabetes mellitus type 2. Normally, diabetes mellitus type 2 is developed after being treated for hypertension for a few years. There are, of course, diabetics who do not suffer from hypertension, however, most of the diabetics (over 70%) have hypertension and lipid metabolism disorders. Also, vision disorders are typical of them. Even with such a problem, patients can seek help of pharmacists. Today’s epidemiological situation in many ways enables pharmacists to inform patients about the risk of diabetes and advise them to undergo a medical examination4). The pharmacist plays an important role in regulating the level of glycaemia in patients, which is shown in some studies from the USA5–10), Australia11–13), Sweden14), Thailand15, 16), Spain17), and the United Arab Emirates18). Thanks to the pharmacist’s intervention in a selected group of patients, the level of HbA1C decreased by 0.76% and FBG (fasting blood glucose) by 29.32 mg/dL19). A positive influence of pharmacists on decreasing the level of glycated haemoglobin is also shown in a study conducted in Maryland, where 90% of the patients with diabetes mellitus aged 65+ had the level of glycated haemoglobin decreased below 9. Similarly, pharmacist interventions contributed to a decrease in the occurrence of adverse drug events (ADEs) by 49 % and potential adverse drug events (pADEs) by 67%20).
Experimental part
Materials and methods
The main aim of the study was to analyze and assess patient adherence to pharmacological or non-pharmacological treatment for diabetes mellitus, and how the pharmacist could influence the patient to adhere to the treatment. All necessary data for the assessment were collected by anonymous questionnaire survey methods. It has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The survey was conducted from 1 July 2016 to 31 January 2017 at two diabetologist offices and two community pharmacies. Our own questionnaire containing 15 questions was used. All the questionnaires in the survey were sorted out and every single question was assessed according to the gender and age of respondents.
Results and discussion
In total, 117 respondents got involved in the survey, with 67 (57%) females and 50 (43%) males. There were 5 age categories: 6 respondents (5%) aged 18–30, 20 respondents (17%) aged 31–45, 29 respondents (25%) aged 46–59, 56 respondents (48%) aged 60–74, and 6 respondents (5%) aged 75+. The respondents were also classified in regard to their completed education. 11 respondents (9%) completed primary education, 43 respondents (37%) secondary education, 37 respondents (32%) secondary education with the certificate of school-leaving exam, and 26 respondents (22%) university education.
According to respective types of diabetes mellitus, they were divided into 4 groups, where 15 respondents (13%) had type 1 diabetes, 98 respondents (84%) type 2 diabetes, 4 female respondents (3%) gestational diabetes, and none of them (0%) other or specific types of diabetes (Fig. 1).
Fig. 1. Respondents according to the type of diabetes mellitus 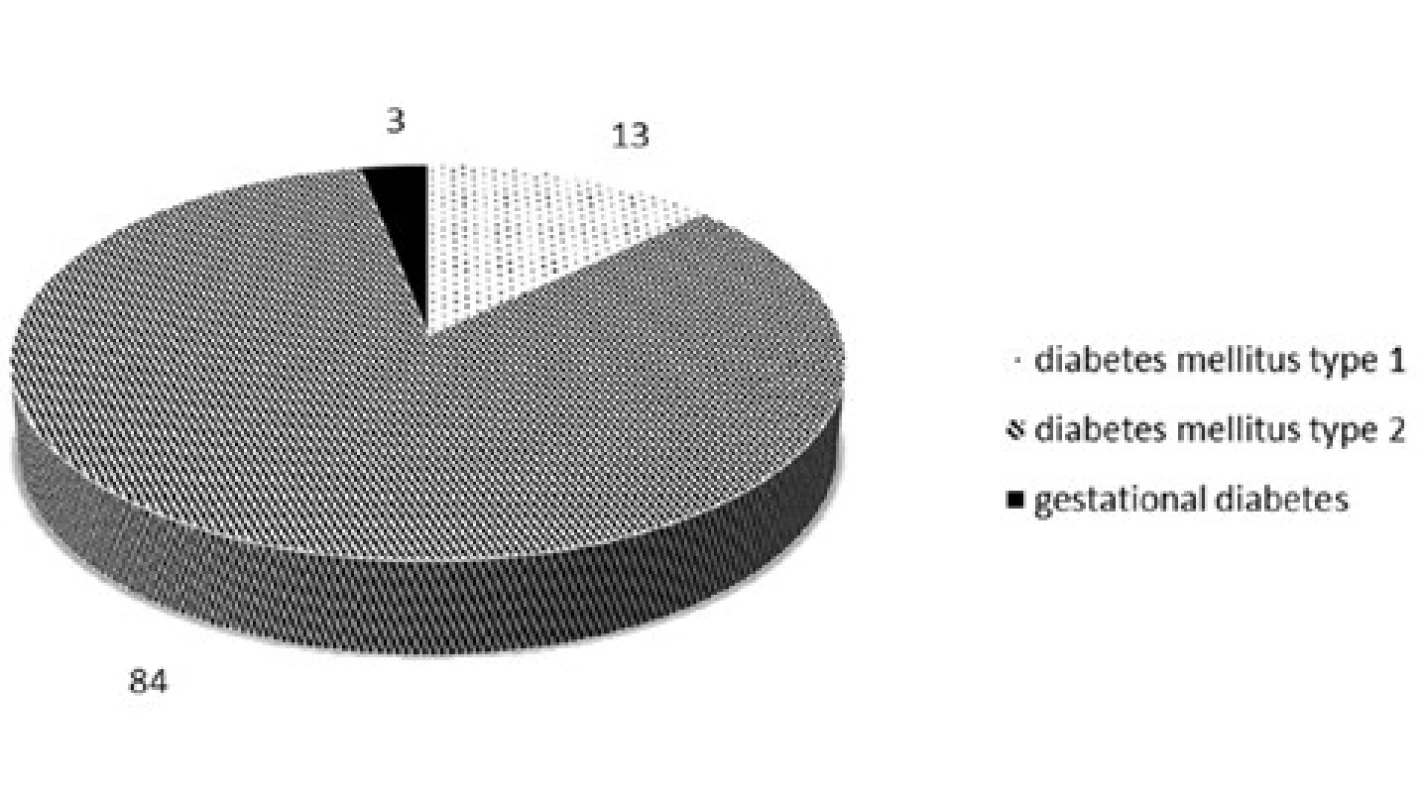
Responses of the respondents to particular questions according to their gender and age
QUESTION: Do you follow a diabetic diet (dietary and regime measures, appropriate eating habits) given by your doctor?
Yes/No tick box was available for this question, and 76% of males and 96% of females answered positively (Fig. 2).
Fig. 2. Dietary and regime measures 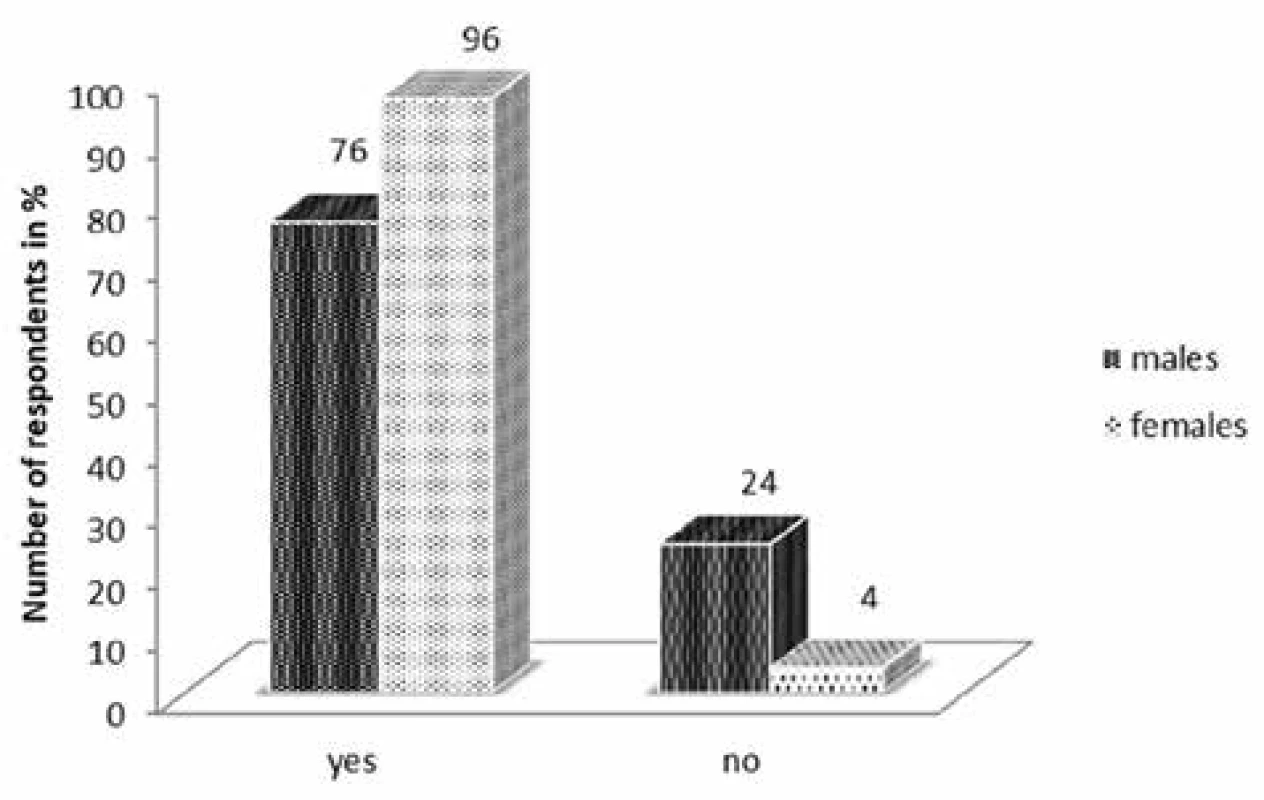
As for age categories, the most prevalent was the answer “Yes” in our respondents aged 60–74 (up to 89%), and those aged 31–45 (85%). All in all, in each age group the answer “Yes” (over 80%) was prevalent (Fig. 3).
Fig. 3. Dietary and regime measures in age categories 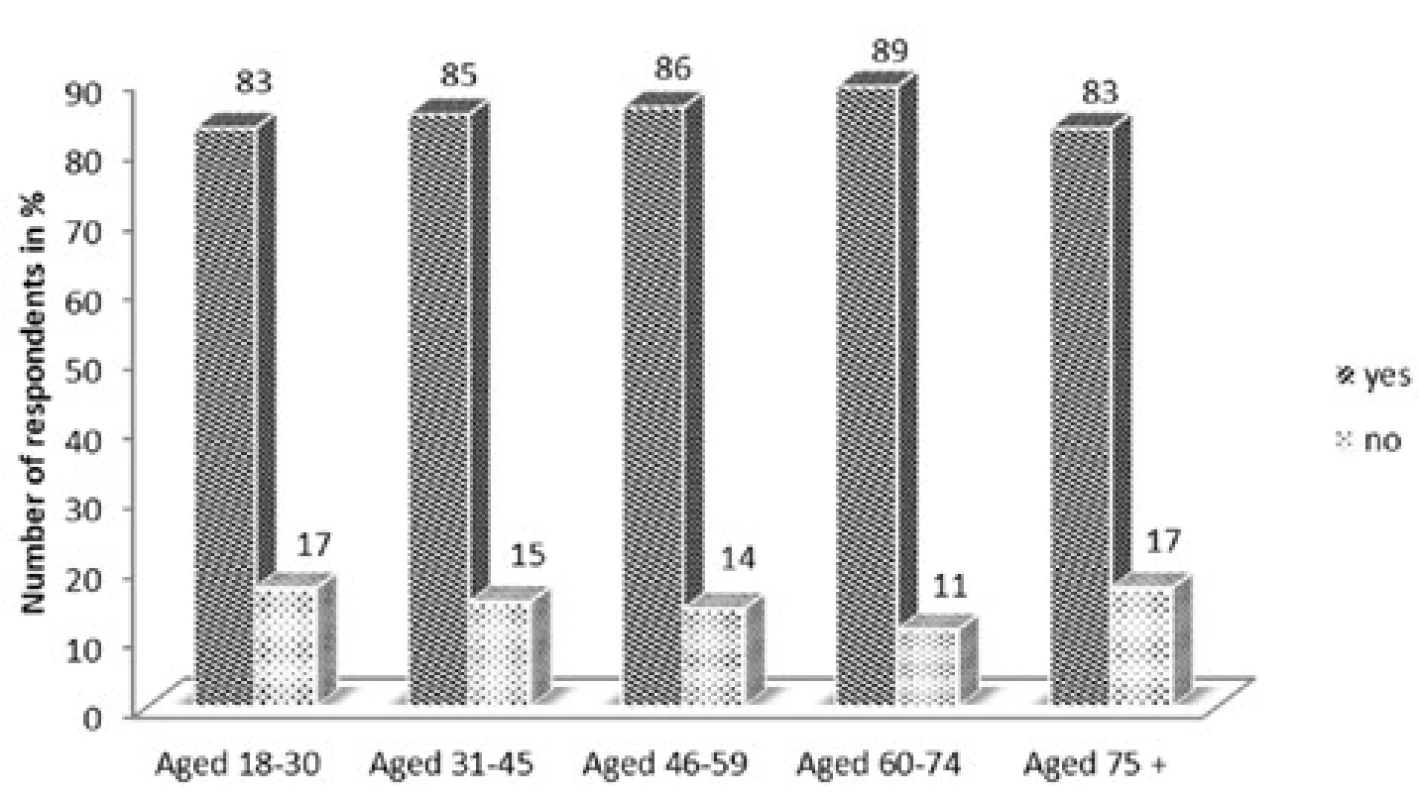
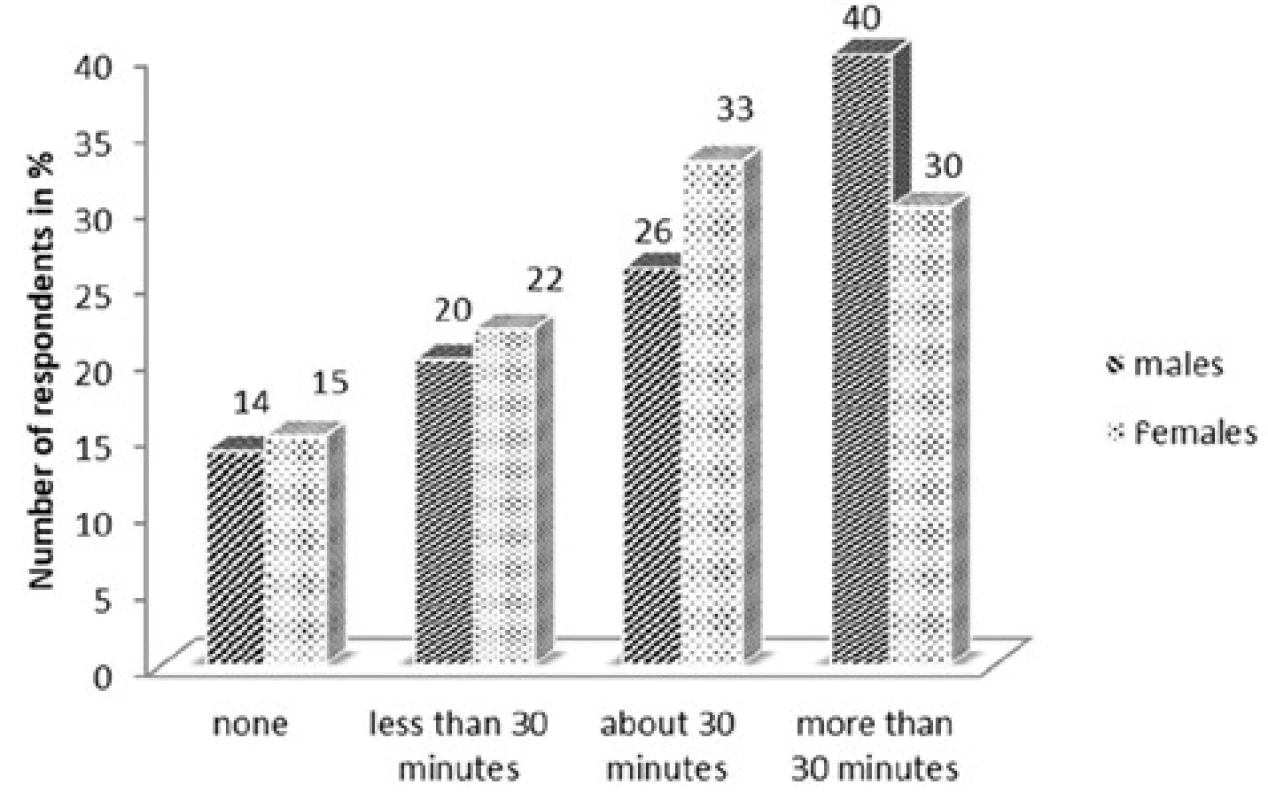
QUESTION: How much time do you devote to movement activities (walks, various sports activities)?
Our findings show that there is not a big percentage difference between male and female answers. The most prevalent was “more than 30 minutes a day”, which was ticked by 40% of male and 30% of female respondents (Fig. 4).
However, the percentage difference in age categories was significant. The answer “none” was ticked by no one aged 18–30 but by 67% aged 75+. Surprisingly, the answer “more than 30 minutes a day” was the most prevalent in those aged 60–74 (39%), aged 18–30 (33%), aged 31–45 (30%), and aged 46–59 (35%), but there was no one aged 75+ (Table 1).
Tab. 1. Movement activities in age categories 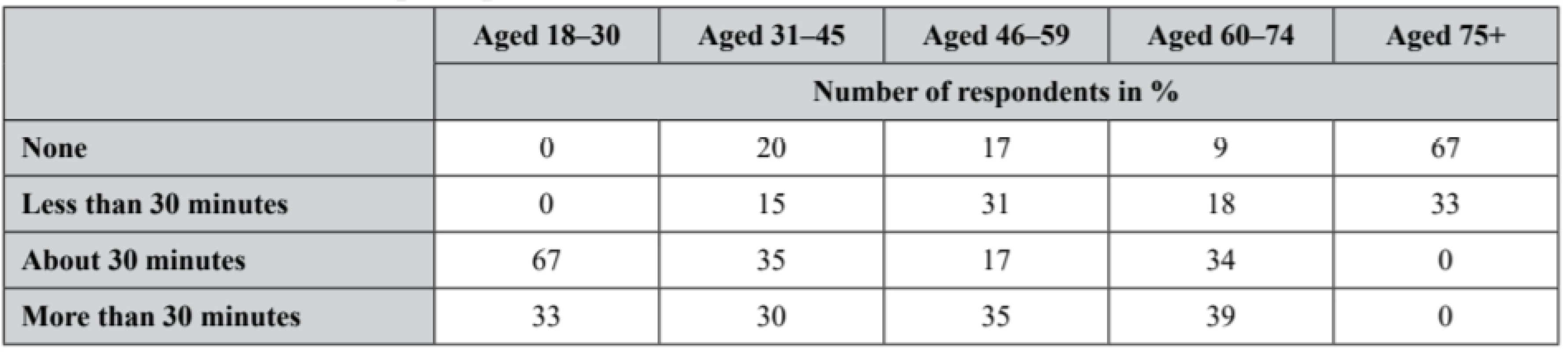
QUESTION: How often do you measure your glycaemia level?
The aim of this question was to find out whether patients check enough on their glycaemia level, which is important for a good compensation in diabetes. The most prevalent answer in females was “only at a medical examination” ticked by 39% of them. As for the answers of males, the most prevalent ones were “only at a medical examination” and “once a week”, both 32% (Fig. 5).
Fig. 5. Measurement of glycaemia level 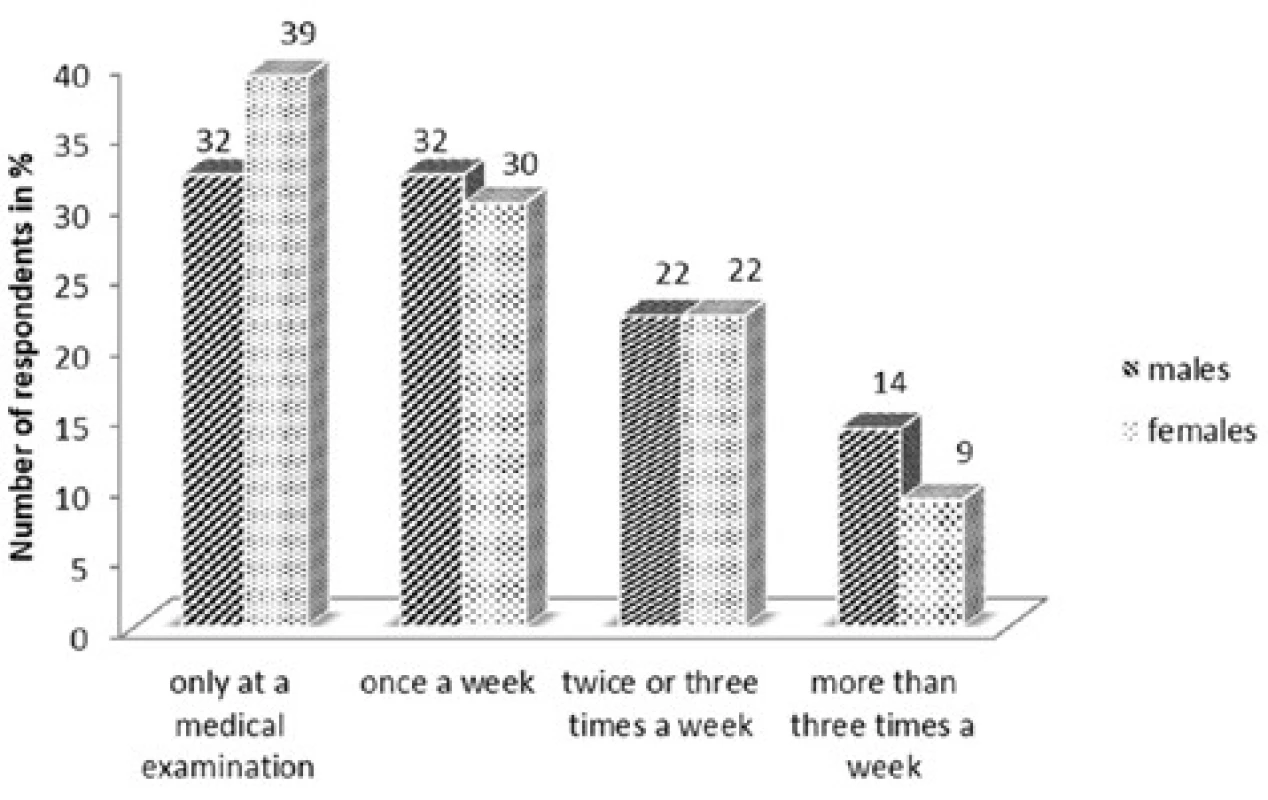
Similarly, we evaluated that question in terms of age categories. Our findings show that 20% aged 31–45 measure the level of glycaemia “more than three times a week”, with 14% aged 60–74, and only 3% aged 46–59, but no respondent in other two age categories (aged 18–30 and 75+). The answer “twice or three times a week” was chosen the most by those aged 75+ (33%), and the least by those aged 18–30 and 46–59 both with the same percentage (17%). The answer “once a week” was the most prevalent for those aged 46–59 (45%). The last answer “only at a medical examination” was the most common for those aged 18–30 (66%), followed by 50% aged 75+ (Table 2).
Tab. 2. Measurement of glycaemia level in age categories 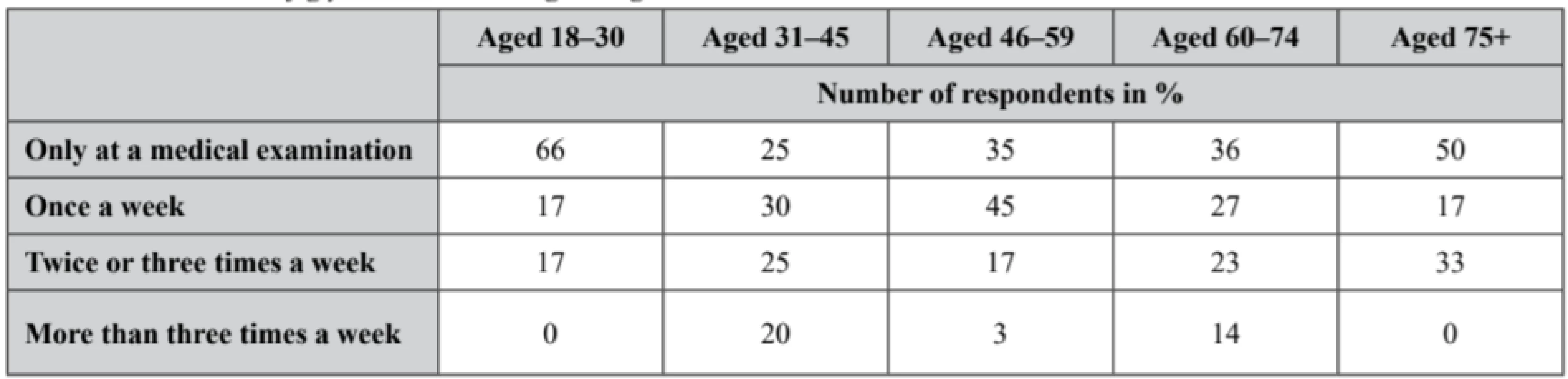
QUESTION: What are your usual readings of glycaemia level on an empty stomach?
The respondents had three options to choose. Accordingly, 49% of female and 38% of male respondents chose “less than 7 mmol/l”, the range “7–11 mmol/l” was more prevalent in males (52%) than in females (45%). The rest of them said “more than 11 mmol/l” that was in males 10% and in females 6% (Fig. 6).
Fig. 6. Glycaemia levels on an empty stomach 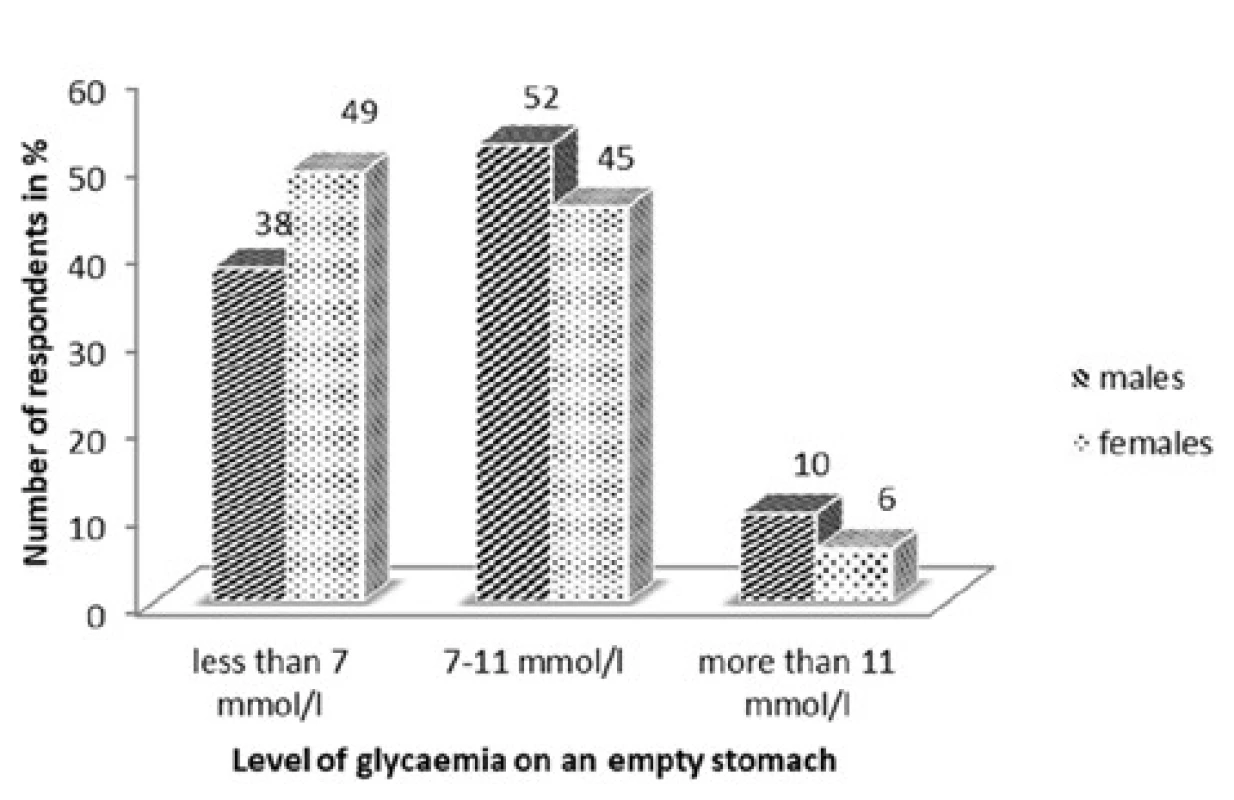
According to age, 83% of the respondents aged 18–30 but none aged 75+ said “less than 7 mmol/l”. The answer “7–11 mmol/l” had the highest percentage (83%) in the respondents aged 75+, and the lowest (17%) in those aged 18–30. Each age category said “more than 11 mmol/l” (below 20%), except for those aged 18–30 (0%) (Table 3).
Tab. 3. Glycaemia levels on an empty stomach in age categories 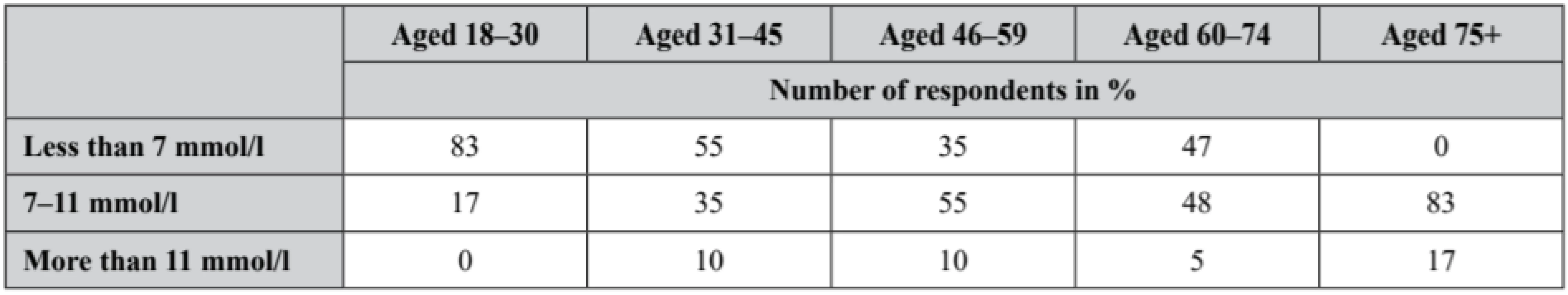
QUESTION: What medications do you use for diabetes?
Our respondents choose that kind of option that corresponded to their current therapy of diabetes mellitus, which is also depicted in the graph below. Most of them (44% of males and 46% of females) chose “oral antidiabetic drugs” (Fig. 7).
Fig. 7. Therapies for diabetes mellitus 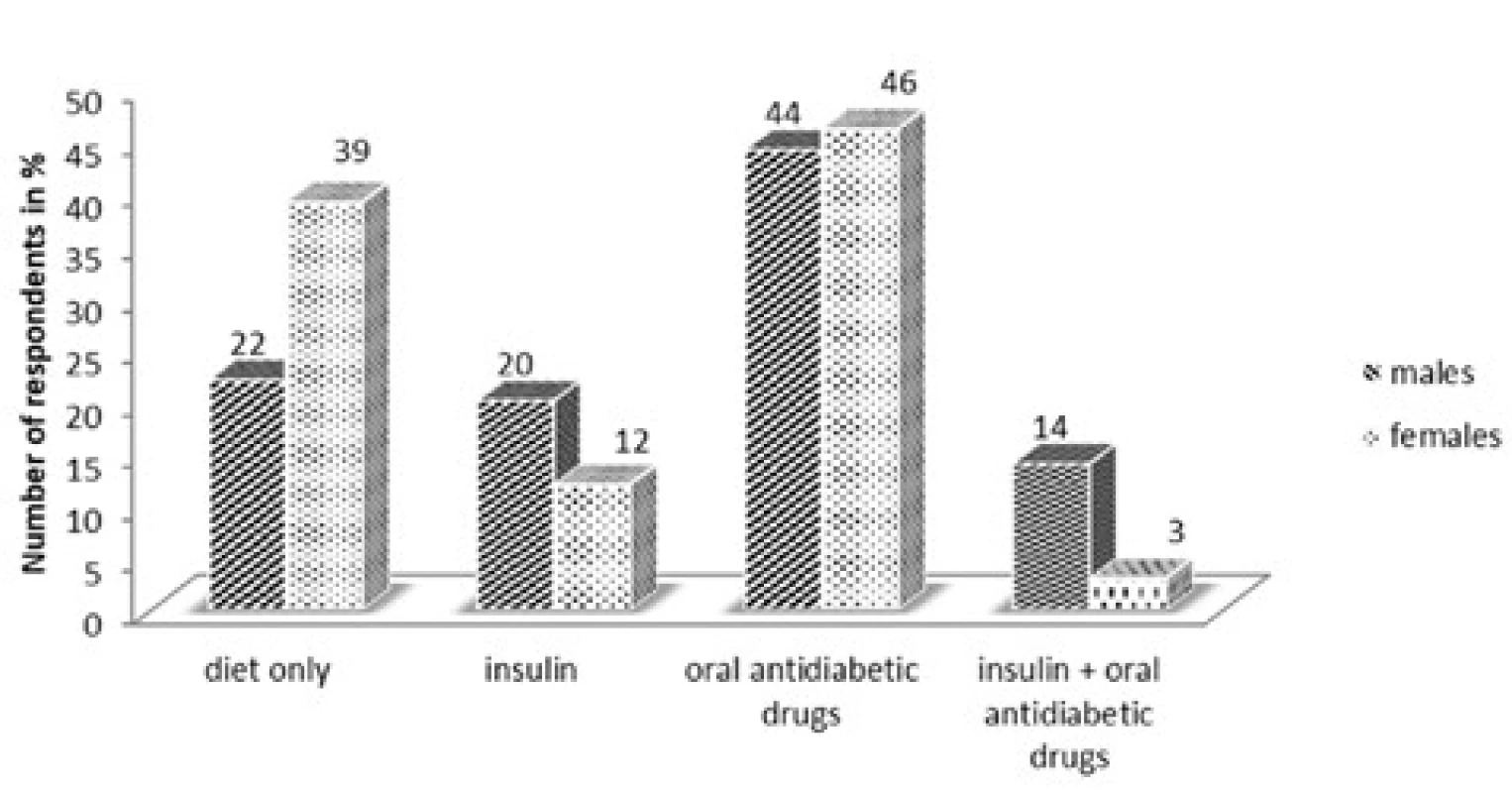
As for age categories, the answer “diet only” had the highest percentage in those aged 31–45 (45%) and the lowest in 75+ (17 %). Differently, another option “oral antidiabetic drugs” had an upward tendency from the age category of 18–30 to 60–74, with a slight drop in those aged 75+ with exactly 50% of them. None of the respondents aged 18–30 ticked “insulin + oral antidiabetic drugs” (Table 4).
Tab. 4. Therapies for diabetes mellitus in age categories 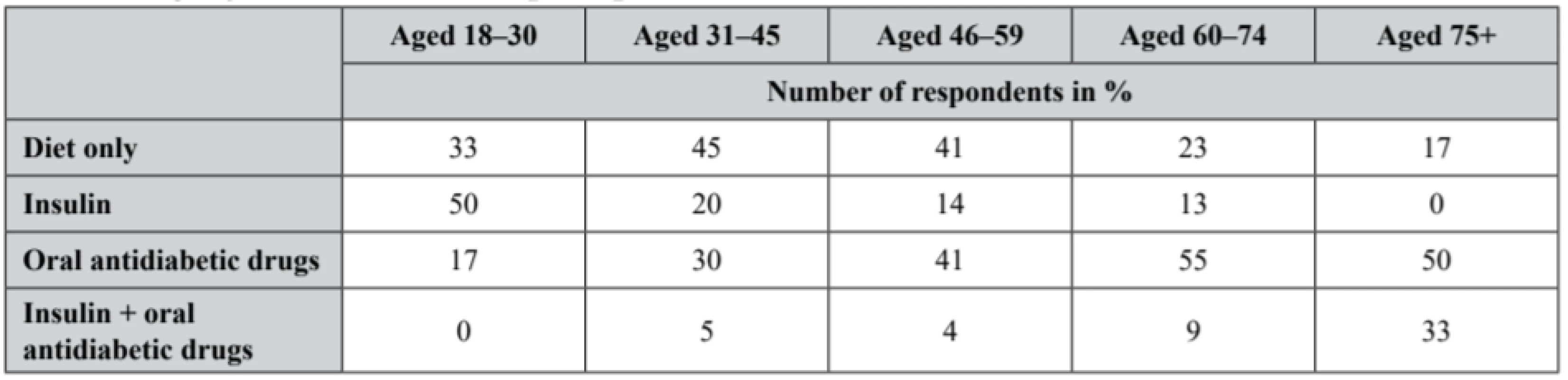
QUESTION: Do you adhere to time intervals – dosage schemes of your drugs (regular medication-taking at recommended hours, application options – with meals or after or with sufficient fluid intake)? THIS QUESTION IS FOR PATIENTS TREATED WITH INSULIN OR ORAL ANTIDIABETIC DRUGS OR BOTH INSULIN AND ORAL ANTIDIABETIC DRUGS
The aim of the question was to find out whether the patients undergoing insulin or oral antidiabetic drug or combination treatment adhere to their regime measures – medication time intervals and dosage schemes. Up to 79% of males and 83% females said “Yes, always”. None of the males (0%) but some females (2%) said “No, not at all” (Fig. 8).
Fig. 8. Medication time intervals and dosage schemes 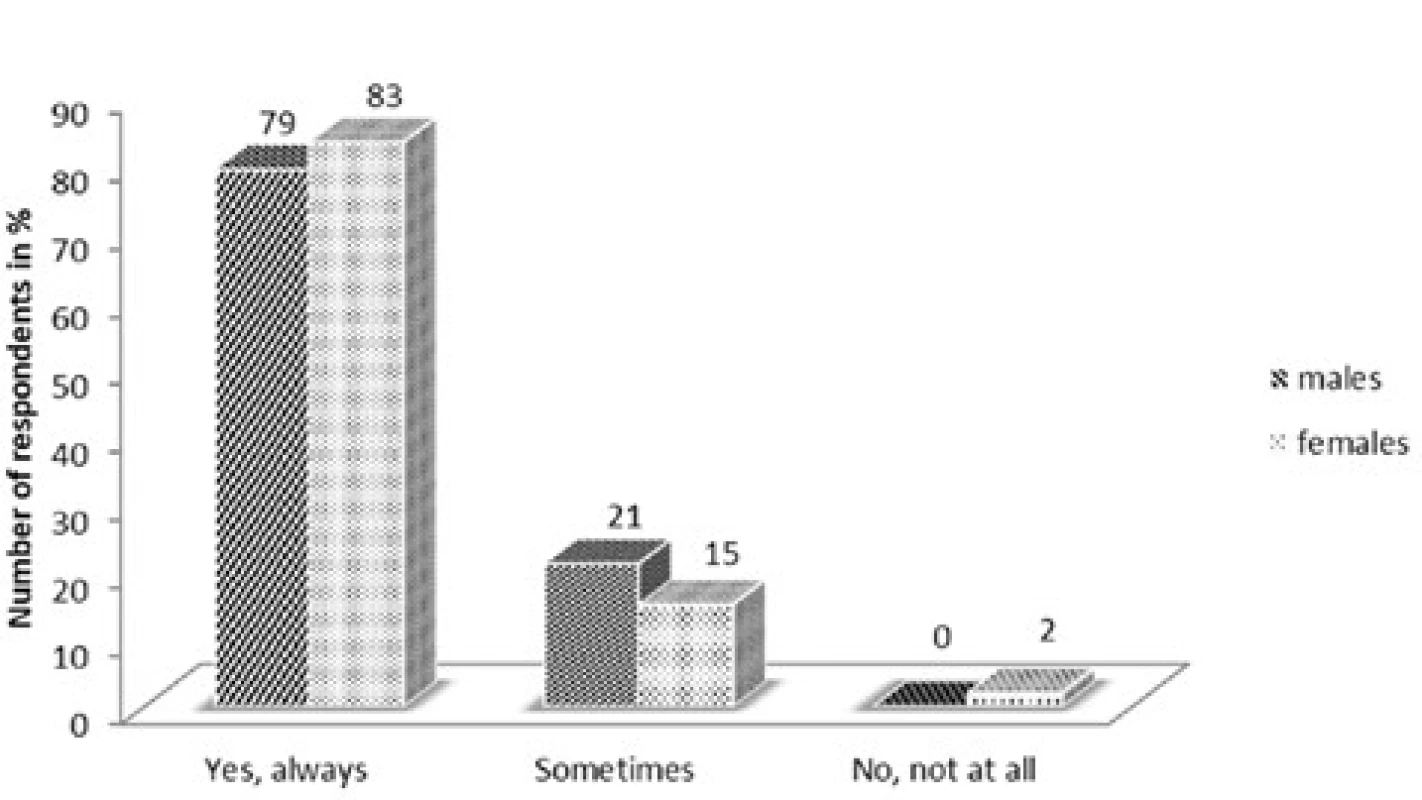
There are four age categories with a high percentage of the answer “Yes, always”, such as those aged 18–30 (75%), and 31–45 (82%), and 46–59 (77%), and 60–74 (88%). 25% of the respondents aged 18–30 but none in other age categories said “No, not at all” (Table 5).
Tab. 5. Medication time intervals and dosage schemes in age categories 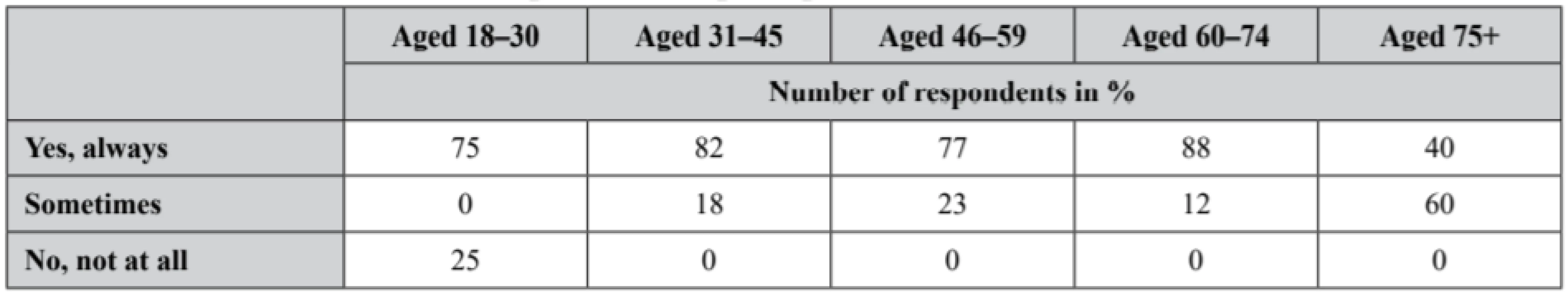
QUESTION: Have your disease or complications related to this disease had any impact on your quality of life?
The last question is about the impact of diabetes mellitus on the respondents’ quality of life. Accordingly, 50% of male and 34% of female respondents said “Yes” (Fig. 9).
Fig. 9. Quality of life in diabetes sufferers 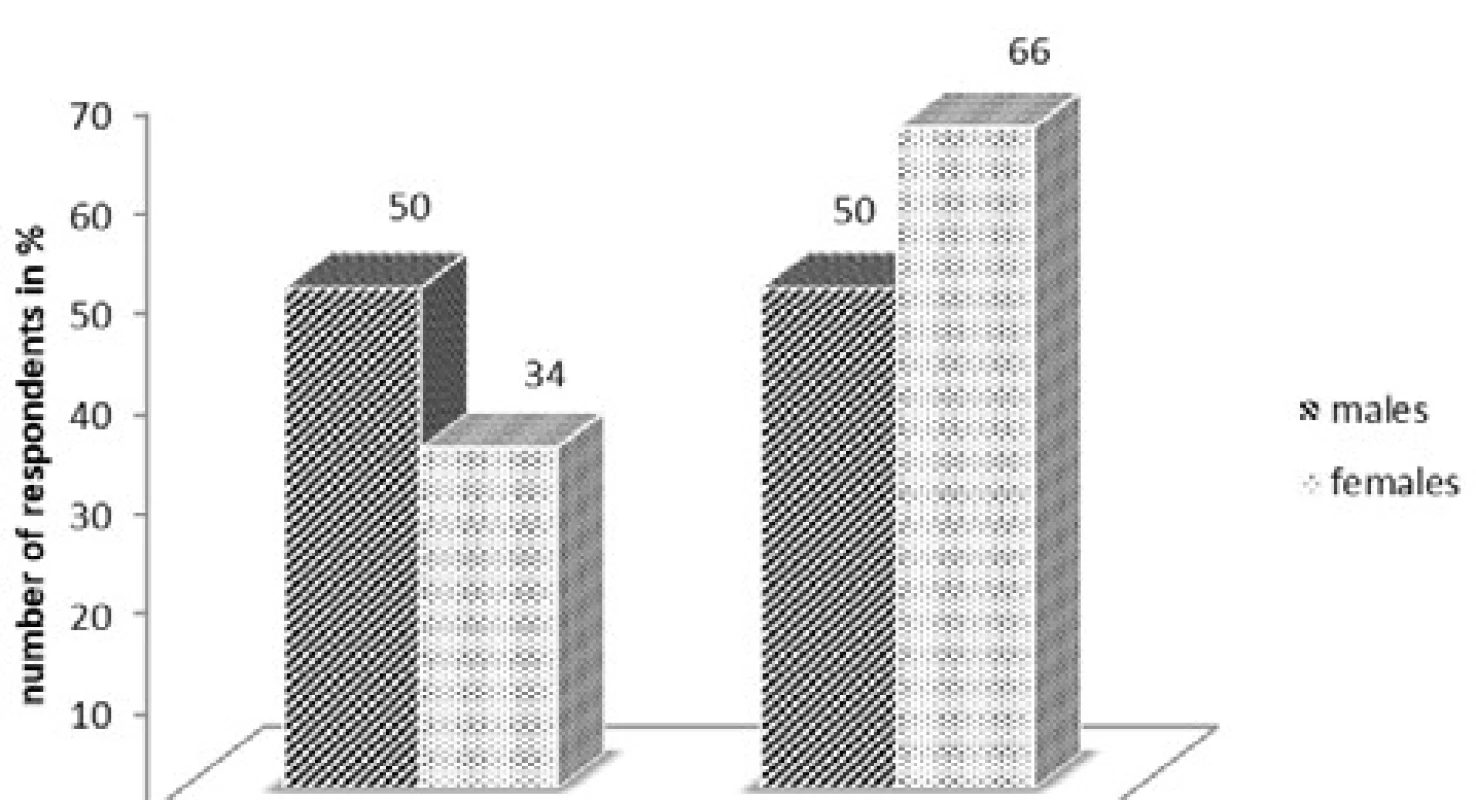
After evaluating the results of the previous question, we came to the conclusion that the older respondents we had, the higher percentage of “Yes” answers we got – 17% aged 18–30, 30% aged 31–45, 31% aged 46–59, 46% aged 60–74, and 100% aged 75+ (Fig. 10).
Fig. 10. Quality of life in diabetes sufferers according to age 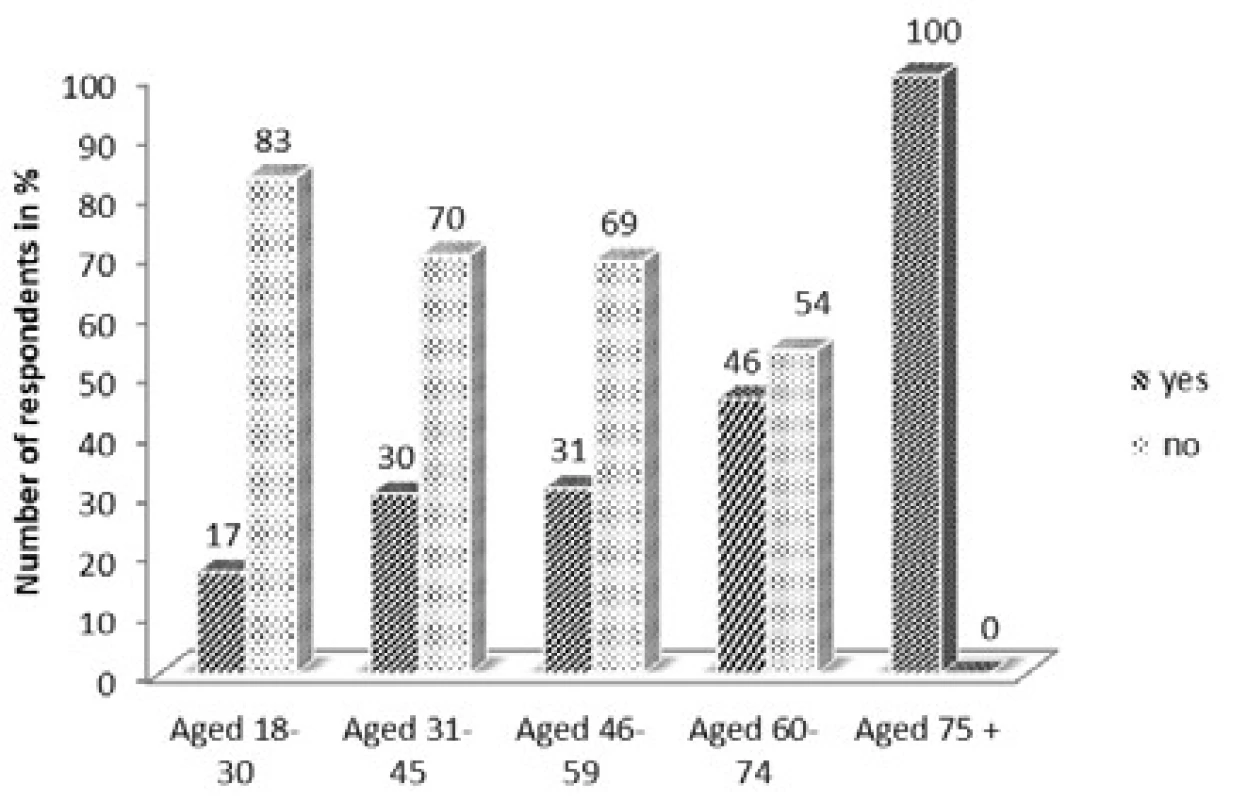
For treating any disease including chronic ones that diabetes mellitus refers to, patient adherence to treatment is very important for obtaining desired therapeutic outcomes. Doctors and nurses, as well as pharmacists play an important role in treating diseases. The findings about regime measures in men and women show that a high percentage of the females (up to 96%) and 76% of the males follow their dietary and regime measures recommended by the doctor. When considering age categories, the answer “Yes” was also prevalent - in each age category it was over 80%. The answers of both men and women regarding their current movement activities in per cent are very similar. In total, 63% of the females and 66% of the males, which means more than half of both genders, do movement activities about 30 minutes or more on a daily basis. As for movement activities in terms of age, the respondents aged 75+ do movement activities less frequently than younger respondents. This may be due to patients’ age itself or related diseases. A study, conducted in 2013 by Krass I. et al., shows that only 31.9% out of 540 respondents agreed to hear out the pharmacist’s advice on a special diet for a good compensation in diabetes. Another question regarding the pharmacist’s advice on the amount of physical activity necessary for a good compensation in diabetes, only 27.2% was willing to hear out21). Although we have succeeded in achieving a high percentage of affirmative answers to the first question in our questionnaire survey, it is necessary that also the pharmacist will contribute to a good compensation in diabetes by providing professional information and advice, including motivating patients to adhere to regime measures. In the questionnaire, we also asked our respondents about treatment methods for diabetes mellitus. The findings show that “oral antidiabetic drugs” were prevalent as a percentage for both genders - 44% of the males and 46% of the females, followed by “diet only” chosen by 39% of the females and 22% of the males. For both men and women, the lowest percentage had the answer “insulin + oral antidiabetic drugs”. According to age, the most prevalent treatment method was the one with oral antidiabetic drugs for those aged 60–74 and 75+. However, it was insulin for those aged 18–30, which indicates the occurrence of diabetes mellitus type 1 in this age category. According to clinical studies conducted in Slovakia, the number of patients being on a diet and having regime measures in Slovakia is lower than in other European countries. For example, the percentage of the patients with regime and dietary measures without any drug treatment was 10 % in Germany, 16.6 % in the Great Britain, 7.3 % in Italy, and only 5.5 % in Slovakia. The number of the patients treated with only oral antidiabetic drugs is higher, and the number of those treated with insulin (only insulin or a combination of insulin and oral antidiabetic drugs) is lower. During the clinical studies, oral antidiabetic drugs (including the combination with insulin) were taken by 70% of Germans, 74.2% of the British, 72.6% of Italians, and 87.8% of Slovaks22). So we can say that the number of the patients with regime and dietary measures is really lower than the number of those with some kind of drug treatment. We asked the respondents undergoing some kind of drug treatment whether they adhered to time intervals and dosage schemes for their medications. Up to 79% of the males and 83% of the females said “Yes, always”. Also, according to age, over 70% of the respondents in each age category (expect for those 75+) adhere to their medication regimens, for those aged 60–74 it was even 88%. Over half of those aged 75+ (60%) said “sometimes” so we can see that it is more difficult for elderly patients to adhere. The study show that patients appreciated when pharmacist had time to answer their questions and encouraged them or helped with problems related to their treatment, as stated by both pharmacists and patients. Patients think that pharmacists should play more important role in the management of their treatment23). For a good compensation in diabetes, glycaemia self-monitoring is of the same importance as adherence to pharmacological and non-pharmacological treatment. Next questions look into the frequency of glycaemia level measurements and the most common readings of glycaemia level on an empty stomach. It shows that 39% of the females and 32% of the males measure their glycaemia level only at a medical examination, and only 14% of the males and 9% of the females measure it more than three times a week. According to age, the percentage of answers “only at a medical examination” was the highest in the youngest age category (aged 18–30), and in two old age categories (aged 60–74 and 75+). Most of the females (49%) had their levels of glycaemia on an empty stomach below 7 mmol/l whereas most of the males (52%) 7–11 mmol/l. According to age, for the respondents under 45 the answer “less than 7 mmol/l” was the most prevalent, and for those 46+ it was 7–11 mmol/l. Surveys show that by clarifying the significance of self-monitoring in discussions between pharmacists and patients, patients have become aware of the importance of having optimal levels of glycaemia. By pharmacists’ interventions in support of self-management related to self-monitoring of glycaemia, 80% learnt about self-monitoring techniques, 65% about hypoglycaemia symptoms, and 72% about hyperglycaemia symptoms. Up to 97% of the patients were satisfied with the explanation when they should measure their level of glycaemia24). To have a desired effect of self-monitoring and motivating in patients, the communication between the patient and other health care providers, including the pharmacist is fundamental and important. Our sample of patients was small and relatively diverse in relation to the location of data collection and the age of the patients, which may somewhat distort the results.
Patient non-adherence to their therapy has got a consequential clinical impact. Life expectancy for diabetes sufferers is much lower than for non-diabetes patients. It is a significant indicator of the state of heath for diabetes patients, as well as it often means a lower quality of life25). Although their quality of life is often lower, especially due to other diseases and complications related to this disease, up to 66% of the female respondents and 50% of the male respondents still claim that diabetes mellitus hasn’t deteriorated their quality of life. According to age, 100% of the respondents aged 75+ and 46% aged 60–74 say that diabetes mellitus has deteriorated their quality of life.
Conclusions
According to the findings, we have come to the conclusion that most of our patients do not find it difficult to adhere to various measures of pharmacological and non-pharmacological treatment for diabetes mellitus. By providing patients with their expertise and professional knowledge while drug dispensing or individual conselling, the pharmacist can motivate the patient to follow not only pharmacological but also non-pharmacological treatment and thereby increase patient adherence itself to treatment.
Conflicts of interest: none.
PharmDr. Lucia Masaryková, PhD. (∗) • T. Tesař, • Ľ. Lehocká • K. Bernáthová
Department of Organisation and Management of Pharmacy
Faculty of Pharmacy, Comenius University in Bratislava
Odbojárov 10, 832 32 Bratislava, SR
e-mail: masarykova@fpharm.uniba.sk
Zdroje
1. IDF Diabetes Atlas, 8th ed. International Diabetes Federation 2017. Available at: www.idf.org [cit. 2019-10-10].
2. Quann E. E., et al. Consuming the daily recommended amounts of dairy products would reduce the prevalence of inadequate micronutrient intakes in the United States: diet modelling study based on NHANES 2007–2010. Nutrition Journal 2015; 14(1), 1–11.
3. Activity at the diabetologists in the Slovak Republic 2017. National Health Information Center 2016. Available at: http://www.nczisk.sk/Documents/publikacie/2016/zs1711.pdf [cit. 2019-10-07].
4. Šmahelová A., Lášticová M. Diabetology for pharmacy students. Praha: Mladá fronta 2011.
5. Choe H. M., et al. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. American Journal of Managed Care 2005; 11(4), 253–260.
6. Doucette W. R., et al. Community pharmacist-provided extended diabetes care. Annals of Pharmacotherapy 2009; 43(5), 882–889.
7. Jaber L.A., et al. Evaluation of a pharmaceutical care model on diabetes management. Annals of Pharmacotherapy 1996; 30(3), 238–243.
8. Jameson J., Baty P. Pharmacist collaboration management of poorly controlled diabetes mellitus: a randomized controlled trial. The American Journal of Managed Care 2010; 16(4), 250–255.
9. Odegard P. S., et al. Caring for poorly controlled diabetes mellitus: a randomized pharmacist intervention. Annals of Pharmacotherapy 2005; 29(3), 433–430.
10. Rothman R. L. et al. A randomized trial of a primary carebased disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. American Journal of Medicine 2005; 118(3), 276–284.
11. Clifford R. M., et al. A randomised controlled trial of a pharmaceutical care programme in high-risk diabetic patients in an outpatient clinic. International Journal of Pharmacy Practice 2002; 10(2), 85–89.
12. Clifford R. M., et al. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: The Fremantle Diabetes Study. Diabetes Care 2005; 28(4), 771–776.
13. Krass I., et al. The pharmacy diabetes care program: assessment of a community pharmacy diabetes service model in Australia. Diabetic Medicine 2007; 24(6), 677–683.
14. Sarkadi A., Rosenqvist U. Experience-based group education in type 2 diabetes: a randomised controlled trial. Patient Education and Counseling 2004; 53(3), 291–298.
15. Phumipamorn S., et al. Effects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetes. Primary Care Diabetes 2008; 2(1), 31–37.
16. Suppapitiporn S., et al. Effect of diabetes drug counselling by pharmacist, diabetic disease booklet and special medication containers on glycemic control of type 2 diabetes mellitus: a randomized controlled trial. Journal of the Medical Association of Thailand 2005; 88(4), S134–141.
17. Fornos J. A., et al. A pharmacotherapy follow-up program in patients with type 2 diabetes in community pharmacies in Spain. Pharmacy World & Science 2006; 28(2), 65–72.
18. Al Mazroui N. R., et al. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. British Journal of Clinical Pharmacology 2009; 67(5), 547–557.
19. Collins C., et al. Effect of pharmacist intervention on glycemic control in diabetes. Diabetes Research and Clinical Practice 2011; 92, 145–152.
20. Twigg G., et al. Pharmacist-managed diabetes center interventions ensure quality and safety in elderly patients. Consultant Pharmacist 2017; 32(5), 299–310.
21. Krass I., et al. Development and validation of the Attitudes to Pharmacist Services for Diabetes Scale (APSDS). Research in Social and Administrative Pharmacy 2015; 11(1), 74–84.
22. Doničová V. Health outcomes of treatment in patients with DM Type 2 nowadays in Slovakia and their other possibilities of improving. Medical letters: professional supplement in Health Newspaper 2015; 16, 18–19.
23. Tinelli M., et al. Patients’ preferences for an increased pharmacist role in the management of drug therapy. International Journal of Clinical Pharmacy 2013; 35(6), 1113–1119.
24. Mitchell B. et al. Diabetes Medication Assistance Service: The pharmacist’s role in supporting patient self-management of type 2 diabetes (T2DM) in Australia. Patient Education and Counselling 2011; 83(3), 288–294.
25. Gajdošík J., Dukát A. Does patient non-adherence to diabetes mellitus type 2 treatment have any clinical and economical impact? Current clinical practice 2014; 2, 13–17.
Štítky
Farmacie Farmakologie
Článek Nové knihy
Článek vyšel v časopiseČeská a slovenská farmacie
Nejčtenější tento týden
2020 Číslo 2- Psilocybin je v Česku od 1. ledna 2026 schválený. Co to znamená v praxi?
- Ukažte mi, jak kašlete, a já vám řeknu, co vám je
- Přerušovaný půst může mít významná zdravotní rizika
-
Všechny články tohoto čísla
- Rhabdomyolýza po chybném užívání rosuvastatinu – kazuistika
- Nové knihy
- Pokroky ve využití instrumentálního měření barevnosti ve vývoji, výrobě a v kontrole jakosti léčiv, léčivých přípravků a farmaceutických pomocných látek III*
- Hodnotenie adherencie k liečbe u pacientov trpiacich diabetes mellitus
- Vliv přípravku «Saprogel» na process hojetí ran u potkanů s modelem rány v plné tloušťce
- Analýza minimalizace nákladů α2b-interferoné suplementace v komplexní farmacoterapii rotavirové infekce u novorozenců
- Formulace a technologický vývoj vaginálních globulí s probiotickou aktivitou
- Česká a slovenská farmacie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Hodnotenie adherencie k liečbe u pacientov trpiacich diabetes mellitus
- Rhabdomyolýza po chybném užívání rosuvastatinu – kazuistika
- Formulace a technologický vývoj vaginálních globulí s probiotickou aktivitou
- Pokroky ve využití instrumentálního měření barevnosti ve vývoji, výrobě a v kontrole jakosti léčiv, léčivých přípravků a farmaceutických pomocných látek III*
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání