-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Medical Termination of Pregnancy (MToP) in the 1st trimester – the role of human chorionic gonadotropin and ultrasound in pregnancy diagnosis and MToP follow-up
Umělé ukončení těhotenství farmakologickou metodou (UUT-F) v I. trimestru – význam stanovení lidského choriového gonadotropinu a ultrazvukového vyšetření při diagnostice těhotenství a hodnocení výsledku UUT-F
Cíl: V České republice lze ženě uměle ukončit těhotenství farmakologickou metodou (UUT-F) v I. trimestru do 49. dne sekundární amenorey. Cílem studie je analýza významu stanovení lidského choriového gonadotropinu (hCG) v séru/moči a ultrazvukového (UZ) vyšetření při diagnostice těhotenství a hodnocení výsledku UUT-F. Metodika: V letech 2017 a 2018 bylo na našem pracovišti provedeno UUT-F celkem u 109 žen sekvenčním podáním mifepristonu (600 mg perorálně) a misoprostolu (400 mcg perorálně). Stanovení hCG v séru/moči a UZ vyšetření byly provedeny při diagnostice těhotenství i hodnocení výsledku UUT-F. Výsledky: Při diagnostice těhotenství byla pozitivní a středně silná korelace mezi hCG v séru a průměrem gestačního váčku v dutině děložní (GS – gestational sac) (r = 0,711; p < 0,0001) i velikostí zárodku v dutině děložní (CRL – crown-rump length) (r = 0,605; p < 0,0001). Délka těhotenství byla 42–49 dní amenorey (průměr 45,6; medián 45), ženy byly ve věku 16–44 let (průměr 29,4; medián 29). Při kontrolním vyšetření po UUT-F byla u 13,8 % žen (15/109) hodnota hCG v séru > 1 000 IU/l a u 17,4 % (20/109) byl pozitivní low sensitivity urine pregnancy test (LSUP test). UZ vyšetření diagnostikovalo „Pokračující těhotenství“ u pěti žen a zamlklé těhotenství u jedné ženy (hCG v séru bylo vždy > 1 000 IU/l a LSUP test byl vždy pozitivní). U 5,5 % žen (6/109) byla provedena následná chirurgická intervence vč. „Pokračujícího těhotenství“ (n = 5); u zamlklého těhotenství (n = 1) byl podán další misoprostol a chirurgickou intervenci nebylo nutné provést. Závěr: Při diagnostice těhotenství je pozitivní a středně silná korelace mezi hCG v séru a CRL. Při kontrolním vyšetření po UUT-F umožní negativní LSUP test spolehlivě vyloučit pokračující těhotenství. V případě pozitivního LSUP testu by mělo být provedeno ultrazvukové vyšetření, nicméně chirurgická intervence by neměla být indikována pouze na základě rozšíření dutiny děložní.
Authors: V. Dvořák Jr. 1,2
; P. Slunska 1
; M. Maděrková Tozzi 1
; K. Langová 3
; V. Kroutilova 1; Radovan Pilka 1
; M. Ľubušký 1
Authors place of work: Department of Obstetrics and Gynecology, Faculty of Medicine, Palacky University Olomouc, Olomouc University Hospital, Czech Republic 1; Centre of Outpatient Gynecology, Clinic and Primary care, Brno, Czech Republic 2; Institute of Medical Biophysics, Faculty of Medicine, Palacky University Olomouc, Czech Republic 3
Published in the journal: Ceska Gynekol 2023; 88(6): 420-427
Category: Původní práce
doi: https://doi.org/10.48095/cccg2023420Summary
Objective: In the Czech Republic, it is possible, to carry out Medical Termination of Pregnancy (MToP) in the 1st trimester up until the 49th day of secondary amenorrhea. The aim of the study is to analyse the significance of serum/urine human chorionic gonadotropin (hCG) assessment and ultrasound (US) examination in pregnancy diagnosis and MToP follow-up. Methods: In 2017–2018, MToP was carried out in a total of 109 women by administering a combination of mifepristone (600 mg orally) and misoprostol (400 mcg orally). Serum/urine (LSUP – low sensitivity urine pregnancy test) hCG assessment and US examination were performed at pregnancy diagnosis and MToP follow-up. Results: At pregnancy diagnosis, there was a positive and medium strong correlation between serum hCG and size of the gestational sac – GS (R = 0.711; P < 0.0001) and crown-rump length of the embryo – CRL (R = 0.605; P < 0.0001). Gestational age was 42–49 days (average 45.6, median 45 days), the women were 16–44 years of age (average 29.4, median 29 years). In MToP follow-up, serum hCG level was > 1,000 IU/L in 13.8% of women (15/109) and a positive LSUP test in 17.4% (20/109). US examination diagnosed ongoing pregnancy in five women and missed abortion in one woman (serum hCG was always > 1,000 IU/L and LSUP test was always positive). In 5.5% of women (6/109), a subsequent surgical intervention was carried out including those with ongoing pregnancy (N = 5); missed abortion (N = 1) was treated by additional misoprostol, where surgical intervention was not necessary. Conclusion: At pregnancy diagnosis, there is a positive and medium strong correlation between serum hCG and CRL. In MToP follow-up, a negative LSUP test enables reliable exclusion of ongoing pregnancy and missed abortion. In case of a positive LSUP test, US examination should be performed; however, surgical intervention should not be indicated solely on the basis of uterine cavity dilatation.
Keywords:
ultrasound – human chorionic gonadotropin – medical termination of pregnancy – 1st trimester
Introduction
Medical Termination of Pregnancy (MToP) in the first trimester was first introduced in 1988 in France, followed by China [1]. Gradually this treatment method spread throughout the world and is preferred by many women [2]. The World Health Organisation (WHO) has found it to be a safe and effective method to terminate pregnancy [3]. Clients who select the pharmacological method over surgery prefer to avoid general anaesthesia, in favour of an overall more natural and intimate course of terminating pregnancy than with the surgical method [4–6]. MToP using the combination of mifepristone and misoprostol is available in the Czech Republic since 2014 and is being used increasingly [7,8].
Since its introduction in the Czech Republic, MToP has undergone modifications in an effort to simplify the conditions of use. This benefits the client as well as the physician providing the treatment. In the past, the following conditions had to be met – secondary amenorrhea 42–49 days and confirmation of a prosperous intrauterine pregnancy (2–9 mm embryo with present pulsation of the circulatory system). Currently, the lower limit has been eliminated, therefore this method may also be used to terminate very early pregnancies, in which ultrasound (US) is not able to confirm prosperous pregnancy (less than 6 weeks of amenorrhea); however, serum human chorionic gonadotropin (hCG) values may be used [9,10]. The method may also be used for unprosperous pregnancies. Even in such cases, MToP is considered effective and safe [11,12]. The pregnancy must be confirmed by US examination and/or hCG test. Being able to reliably evaluate the success of the method by ruling out continuing pregnancy is crucial [13] and again US examination and/or hCG test is used [14–16]. The objective of our study was to analyse and compare hCG values in serum/urine with ultrasound examination during pregnancy diagnosis and MToP follow-up.
Materials and methods
Prospective cohort study conducted during 2017–2018. The inclusion criteria were as follows: prosperous intrauterine pregnancy, singleton pregnancy, crown-rump length of the embryo – CRL 2–9 mm, secondary amenorrhea 42–49 days (average 45.6; median 45 days), and women 16–44 years of age (average 29.4; median 29 years).
Each pregnancy was diagnosed by transvaginal US examination and hCG blood draw. Initially there were 137 women interested in MToP and participation in the study. In 32 women there was no embryo present on the initial US examination (no prosperous intrauterine pregnancy was detected, which was one of the inclusion criteria). These women were invited for a follow-up examination and subsequently an unprosperous pregnancy was diagnosed in 7 of them, therefore they were excluded from the study. In the remaining 25 women, a prosperous intrauterine pregnancy was confirmed, and they were included into the study. In 10 women, the CRL was more than 9mm and they were also excluded from the study. In total, MToP was performed in 120 women. Follow--up is lacking in 11 women (MToP was performed but they did not attend the follow-up visits). Therefore, a total of 109 women who met the inclusion criteria, underwent MToP and completed follow-up were included in the study.
MToP was performed by administering oral mifepristone (Mifegyne 200 mcg®) 600 mcg and oral misoprostol (Mispregnol 400 mcg®) 400 mcg in a 36–48-h interval. Combining the two drugs is more effective than monotherapy [17].
MToP follow-up took place 2–5 weeks later, all women underwent US examination and serum hCG and urine hCG (LSUP test – low sensitivity urine pregnancy) values were determined.
Results
At pregnancy diagnosis, there was a medium strong positive correlation between serum hCG and the gestational sac – GS (R = 0.711; P < 0.0001) and CRL (R = 0.605; P < 0.0001). Gestational age was 42–49 days (average 45.6; median 45 days), and the women were 16–44 years of age (average 29.4; median 29 years). In MToP follow-up, serum hCG > 1,000 IU/L was present in 13.8% of women (15/109) with a positive LSUP test in 17.4% (20/109). US examination diagnosed ongoing pregnancy in five women and a missed abortion in one woman (serum hCG was always > 1,000 IU/L and LSUP test always positive). In 5.5% of the women (6/109), a subsequent surgical intervention was carried out, including in the women with ongoing pregnancy (N = 5); the case of the missed abortion (N = 1) was treated by additional misoprostol, not surgery.
Pregnancy diagnosis is clearly depicted in Fig. 1–4.
MToP follow-up is clearly depicted in Fig. 5–8.
Fig. 1. Pregnancy diagnosis – correlation between serum hCG and US fi nding in the uterine cavity. Intrauterine singleton pregnancy, the embryo with blood circulation pulsation was still not present (N = 32). In 21.9 % of women (7/32), a subsequent unprosperous pregnancy was diagnosed (red). The strength of association between hCG and GS was measured using Spearman correlation coefficient. There was a medium strong positive correlation: R = 0.600; P = 0.0003. The slope of regression line showed the trend, there is a regression equation and coefficient of determination, denoted R2. 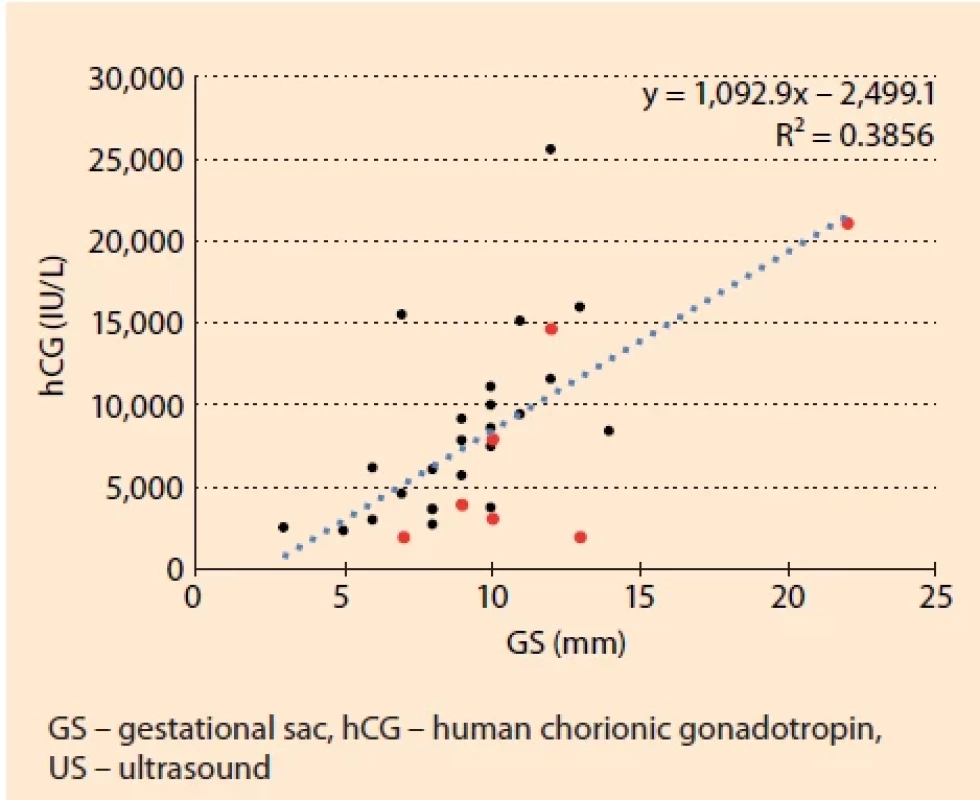
Obr. 1. Diagnostika těhotenství – závislost hCG v séru a ultrazvukového nálezu v dutině děložní. Nitroděložní jednočetné těhotenství, ještě ale nebyl přítomen zárodek s pulzací krevního oběhu (n = 32). U 21,9 žen % (7/32) bylo následně diagnostikováno „neprosperující těhotenství“ (červená). Korelace mezi hCG a GS byla ověřena pomocí Spearmanova korelačního koefi cientu. Korelace je pozitivní a středně silná: r = 0,600; p = 0,0003. Směr závislosti je naznačen regresní přímkou, u které je uvedena regresní rovnice a hodnota koeficientu determinace R2. Fig. 2. Pregnancy diagnosis – correlation between serum hCG and US fi nding in the uterine cavity. Intrauterine singleton pregnancy, the embryo with blood circulation pulsation was still not present, only subsequently prosperous (N = 25). The strength of association between hCG and GS was measured using Spearman correlation coeffi cient. There was a medium strong positive correlation: R = 0.711; P < 0.0001. The slope of regression line showed the trend, there is a regression equation and coeffi cient of determination, denoted R2. 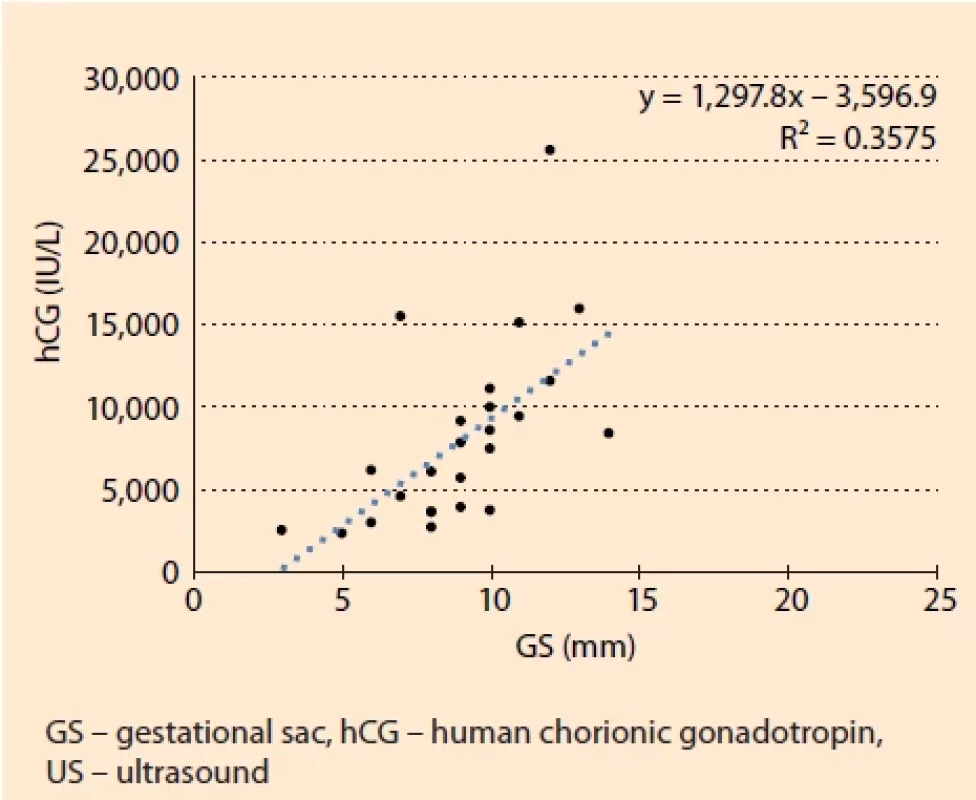
Obr. 2. Diagnostika těhotenství – závislost hCG v séru a ultrazvukového nálezu v dutině děložní. Nitroděložní jednočetné těhotenství, ještě ale nebyl přítomen zárodek s pulzací krevního oběhu, jen následně prosperující (n = 25). Korelace mezi hCG a GS byla ověřena pomocí Spearmanova korelačního koefi cientu. Korelace je pozitivní a středně silná: r = 0,711; p < 0,0001. Směr závislosti je naznačen regresní přímkou, u které je uvedena regresní rovnice a hodnota koefi - cientu determinace R2. Fig. 3. Pregnancy diagnosis – correlation between serum hCG and US fi nding in the uterine cavity. Intrauterine singleton pregnancy, the embryo with blood circulation pulsation was present, CRL ≥ 2 mm (N = 130). In 7.7% of women (10/130), CRL > 9 mm was present and MToP was not carried out (grey). In 9.2% of remaining women( 11/120), MToP follow-up was missed. The strength of association between hCG and CRL was measured using Spearman correlation coeffi cient. There was a medium strong positive correlation: R = 0.605; P < 0.0001. The slope of regression line showed the trend, there is a regression equation and coeffi cient of determination, denoted R2. 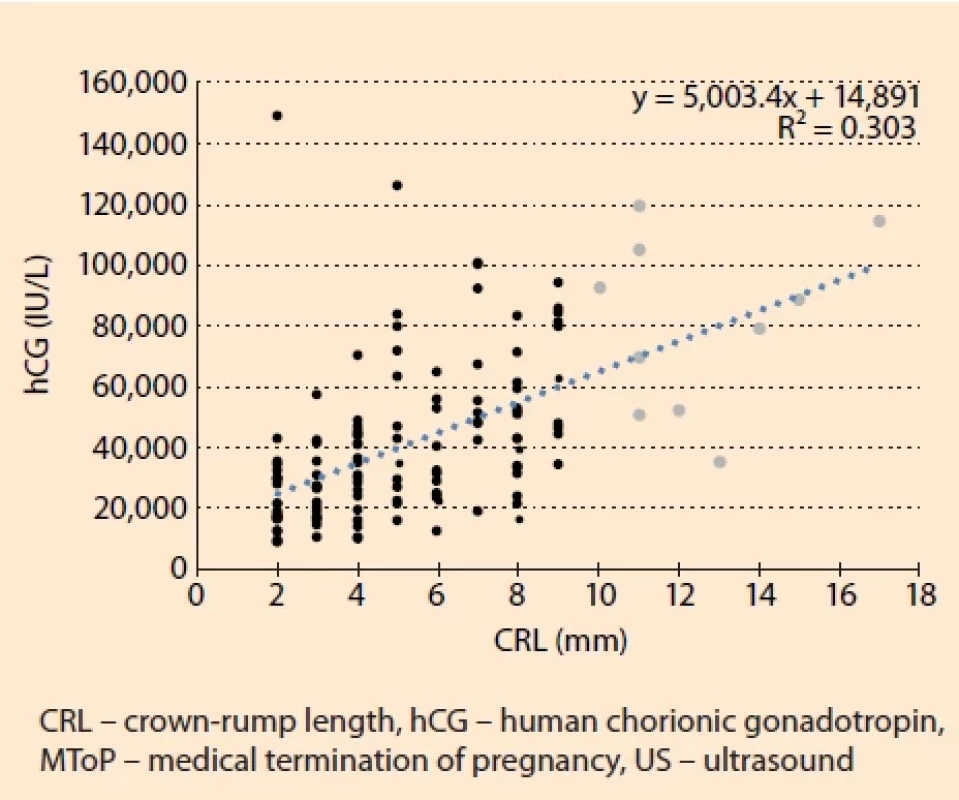
Obr. 3. Diagnostika těhotenství – závislost hCG v séru a ultrazvukového nálezu v dutině děložní. Nitroděložní jednočetné prosperující těhotenství, přítomen zárodek s pulzací krevního oběhu, CRL ≥ 2 mm (n = 130). U 7,7 % žen (10/130) bylo CRL > 9 mm (šedá) a MToP nebylo neprovedeno. U 9,2 % ze zbývajících žen (11/120) nebylo provedeno kontrolní vyšetření po MToP (černá) – chybí follow-up. Korelace mezi hCG a CRL byla ověřena pomocí Spearmanova korelačního koeficientu. Korelace je pozitivní a středně silná: r = 0,605; p < 0,0001. Směr závislosti je naznačen regresní přímkou, u které je uvedena regresní rovnice a hodnota koefi - cientu determinace R2. Fig. 4. Pregnancy diagnosis – correlation between serum hCG and US fi nding in the uterine cavity. Intrauterine singleton pregnancy, the embryo with blood circulation pulsation was present, only CRL 2–9 mm, the MToP and follow-up was carried out (N = 109). In 4.6% of women (5/109), a subsequent “Ongoing pregnancy“ was diagnosed (red). The strength of association between hCG and CRL was measured using Spearman correlation coeffi cient. There was a medium strong positive correlation: R = 0.526; P < 0.0001. The slope of regression line showed the trend, there is a regression equation and coeffi cient of determination, denoted R2. 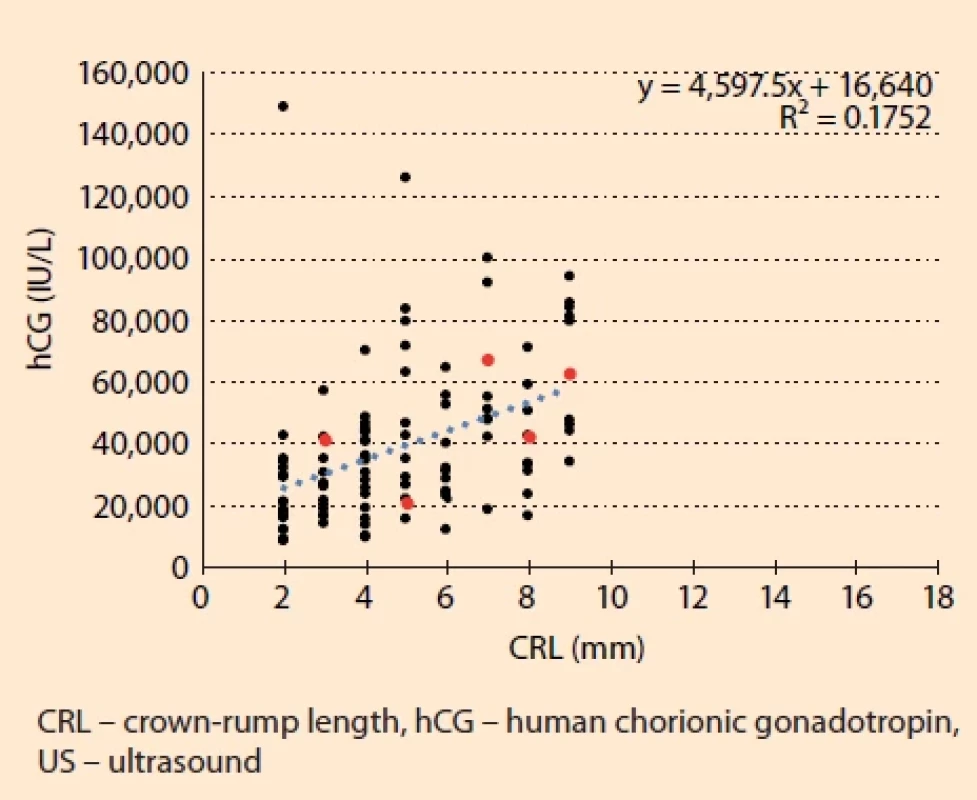
Obr. 4. Diagnostika těhotenství – závislost hCG v séru a ultrazvukového nálezu v dutině děložní. Nitroděložní jednočetné prosperující těhotenství, přítomen zárodek s pulzací krevního oběhu, jen CRL 2–9 mm, provedeno MToP a následně se dostavily i na kontrolní vyšetření (n = 109). U 4,6 % žen (5/109) bylo následně diagnostikováno „Pokračující těhotenství“ (červená). Korelace mezi hCG a CRL byla ověřena pomocí Spearmanova korelačního koefi cientu. Korelace je pozitivní a středně silná: r = 0,526; p < 0,0001. Směr závislosti je naznačen regresní přímkou, u které je uvedena regresní rovnice a hodnota koefi cientu determinace R2. Fig. 5. MToP follow-up – serum hCG decrease of previous level. MToP follow-up visit to rule out “Ongoing pregnancy“ (N = 104). In one woman (hCG decrease to 2.6%), an “Incomplete abortion“ was diagnosed and treated by Surgery (red). In one woman (hCG decrease to 34%), a missed abortion was diagnosed and treated by additional misoprostol (green). In one woman (hCG decrease to 74.9%), an “Incomplete abortion“ 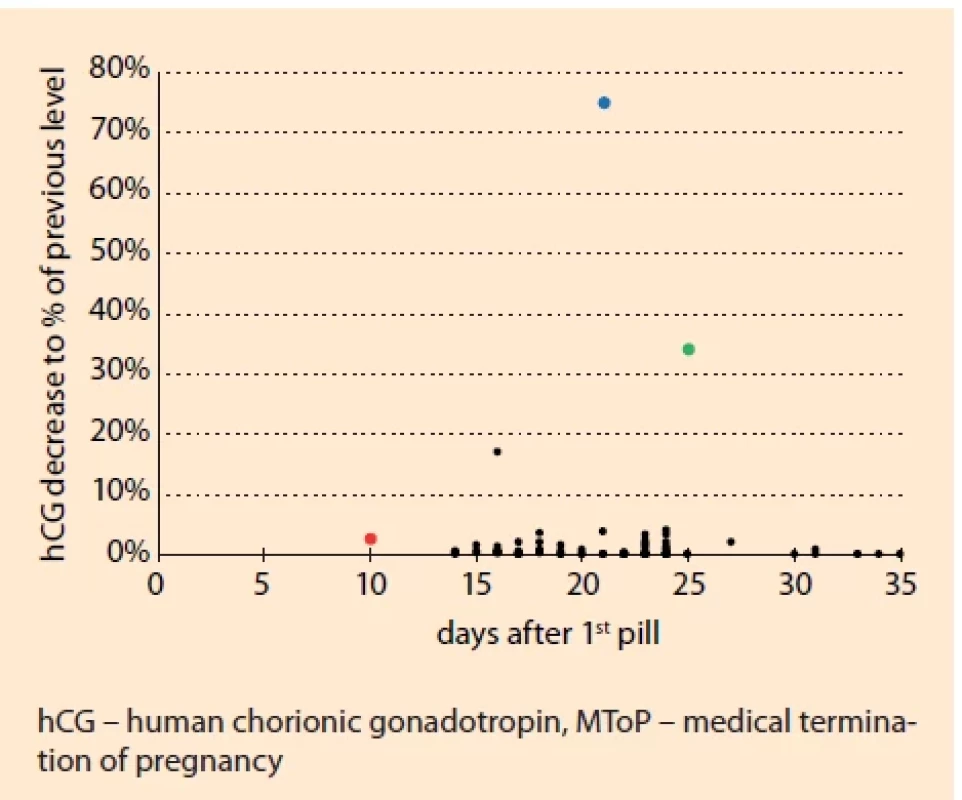
Obr. 5. MToP follow-up – pokles hCG v séru (% původní hodnoty). Kontrolní vyšetření po MToP, vyloučeny „Pokračující těhotenství“ (n = 104). U jedné ženy (pokles hCG v séru na 2,6 % původní hodnoty) byl diagnostikován nekompletní potrat a byla provedena chirurgická intervence (červená). U jedné ženy (pokles hCG v séru na 34,0 % původní hodnoty) bylo diagnostikováno zamlklé těhotenství, byl podán další misoprostol a chirurgickou intervenci nebylo nutné provést (zelená). U jedné ženy (pokles hCG v séru na 74,9 % původní hodnoty) byl diagnostikován nekompletní potrat s expektačním managementem (modrá). Fig. 6. MToP follow-up – serum hCG. MToP follow-up check; excluding “Ongoing pregnancy“ and missed abortion, but serum hCG was always > 1,000 IU/L (N = 103). In 8.7% of women (9/103), serum hCG > 1,000 IU/L was present (red). In 13.8% of women (15/109), serum hCG > 1,000 IU/L was present including “Ongoing pregnancy“ (N = 5) and missed abortion (N = 1). 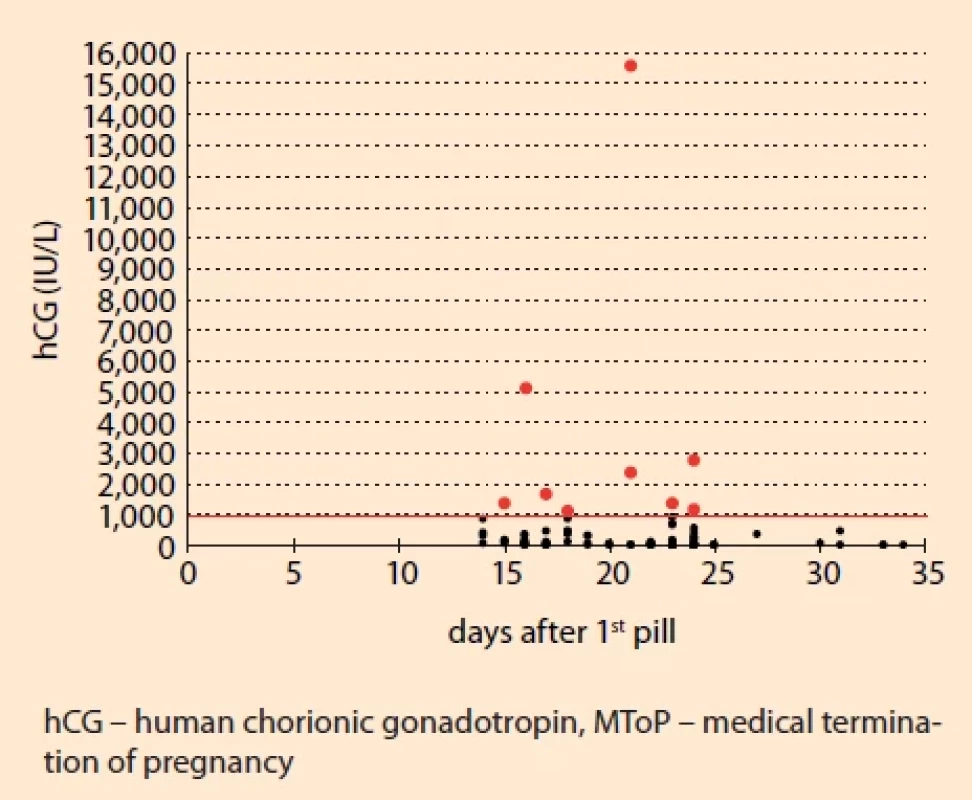
Obr. 6. MToP follow-up – hCG v séru. Kontrolní vyšetření po MToP, vyloučeny „Pokračující těhotenství“a zamlklé těhotenství, u kterých ale bylo hCG v séru vždy > 1 000 IU/l (n = 103). U 8,7 % žen (9/103) byla hodnota hCG v séru > 1 000 IU/l (červená). U 13,8 % žen (15/109) byla hodnota hCG v séru > 1 000 IU/l vč. „Pokračujícího těhotenství“ (n = 5) a zamlklého těhotenství (n = 1). Fig. 7. MToP follow-up – serum hCG / LSUP test. MToP follow-up check; excluding “Ongoing pregnancy“ and missed abortion, but serum hCG was always > 1,000 IU/L and LSUP test always positive (N = 103). In one woman, a false negative LSUP test was present (green). In six women, a false positive LSUP test was present (red). In 17.4% of women (20/109), a positive LSUP test was present including “Ongoing pregnancy“ (N = 5) and missed abortion (N = 1). 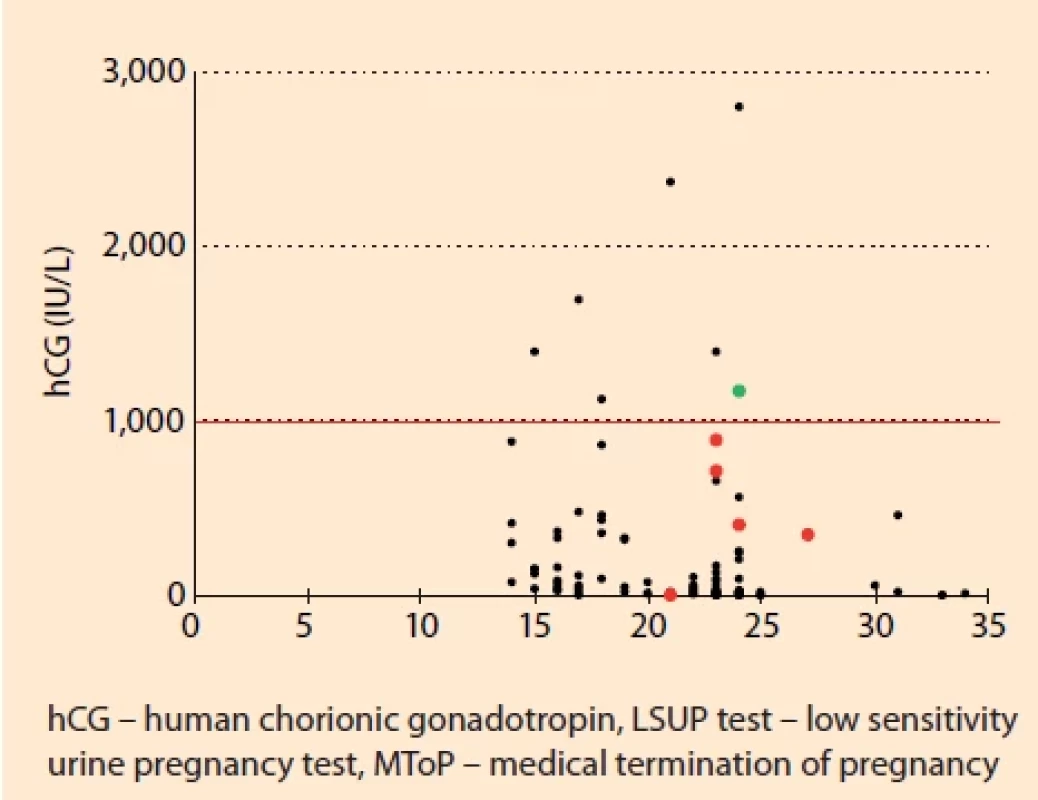
Obr. 7. MToP follow-up – hCG v séru / LSUP test. Kontrolní vyšetření po MToP, vyloučeny „Pokračující těhotenství“a zamlklé těhotenství, u kterých ale bylo hCG v séru vždy > 1 000 IU/l a LSUP test byl vždy pozitivní (n = 103). U jedné ženy byl LSUP test falešně negativní (zelená). U šesti žen byl LSUP test falešně pozitivní (červená). U 17,4 % žen (20/109) byl LSUP test pozitivní vč. „Pokračujícího těhotenství“ (n = 5) a zamlklého těhotenství (n = 1). Fig. 8. MToP follow-up – US uterine cavity dilatation. MToP follow-up check; excluding “Ongoing pregnancy“ and missed abortion (N = 103). In 1% of women (1/103), a subsequent surgical intervetion was carried out (red). In 5.5% of women (6/109), a subsequent surgical intervention was carried out including “Ongoing pregnancy” (N = 5); missed abortion (N = 1) was treated by additional misoprostol, not by surgery. 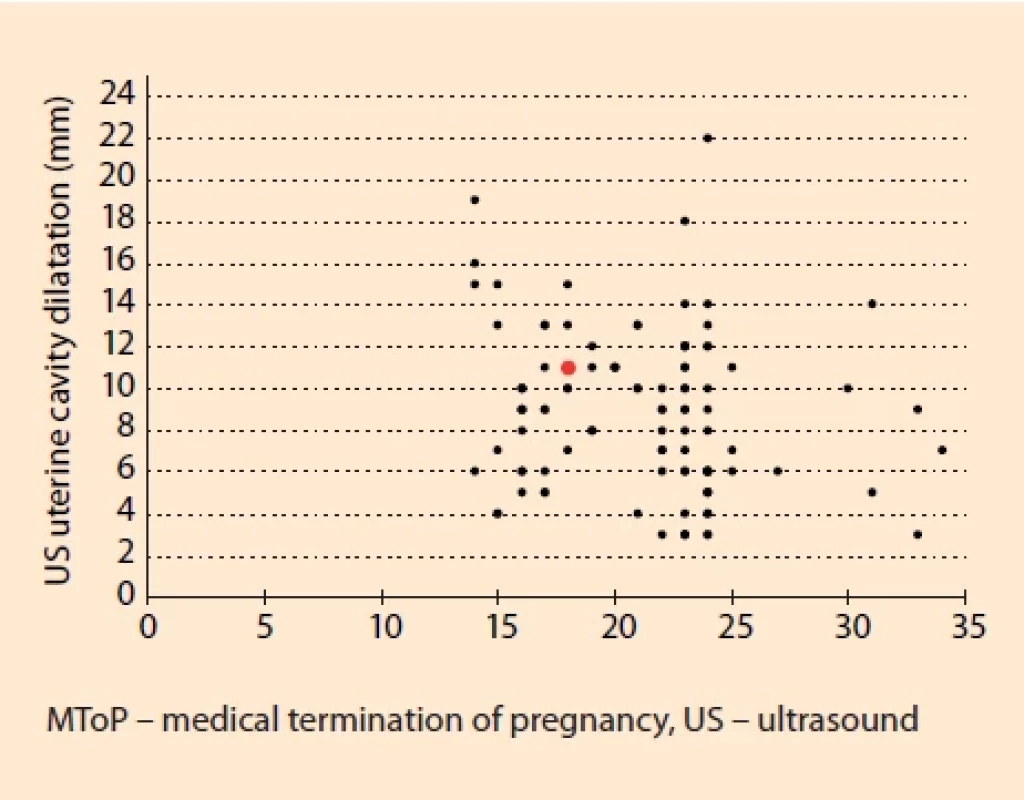
Obr. 8. MToP follow-up – šířka dutiny děložní při ultrazvukovém vyšetření. Kontrolní vyšetření po MToP, vyloučeny „Pokračující těhotenství“a zamlklé těhotenství (n = 103). U 1,0 % žen (1/103) byla provedena následná chirurgická intervence (červená). U 5,5 % žen (6/109) byla provedena následná chirurgická intervence vč. „Pokračujícího těhotenství“ (n = 5), u zamlklého těhotenství (n = 1) byl podán další misoprostol a chirurgickou intervenci nebylo nutné provést. Discussion
Pregnancy diagnosis
The objective of the work was to confirm a correlation between hCG levels and ultrasound findings at pregnancy dia g nosis. During the course of pregnancy, hCG levels change significantly. The hCG value is zero in non-pregnant women. In the early phases of pregnancy, hCG values double every 48–72 h and reach a peak at 8–11 weeks of pregnancy and will then gradually decline during the remainder of the pregnancy [18]. In the early stage of pregnancy, hCG increases daily by approximately 50% [19]. There is great individual variability in hCG values. Therefore, it is practically impossible to date a pregnancy based solely on hCG levels and hCG is used primarily to diagnose (confirm) a pregnancy [20]. The value of hCG from which US examination would always be able to identify an intrauterine gestational sac is unknown [21]. Ultrasound examination is used to date a pregnancy [22]. Nonetheless, the results of this work reveal that during pregnancy diagnosis, there is a positive and medium strong correlation between serum hCG levels and US findings (GS and CRL). However, a single value of hCG cannot predict if the pregnancy will be prosperous or unprosperous. Similarly, the value of hCG or CRL at the diagnosis of pregnancy cannot predict the success of MToP.
Medical termination of pregnancy may also be used in the very early stages of pregnancy (< 6 weeks of amenorrhea), where US cannot yet demonstrate a prosperous pregnancy (embryo with a present pulsation of the circulatory system) and we are guided by serum hCG values. In these cases, MToP is just as effective and safe as in the later weeks [23,24]. The method can also be used in cases of missed abortion. However, the inclusion criteria of this study were stricter (evidence of a prosperous intrauterine pregnancy), while women with unprosperous pregnancies in the early stages were excluded. Our data reliably reflect the effectiveness of MToP in cases of prosperous pregnancies and our results are therefore more accurate.
The study consisted of oral sequential administration of mifepristone and misoprostol up to 49 days of amenorrhea. It is the only legislatively approved form of administration in the Czech Republic [9]. Misoprostol may be used on its own [25–27], but appears to be more effective when used in combination with mifepristone [17,28,29].
MTOP follow-up
This study confirmed that MToP is a safe and effective method of terminating pregnancy. Failure of this method (ongoing pregnancy) was seen in 4.6% of women. Usually, the failure rate of this method is reported between 1–3% [30].
At MToP follow-up, the relation between US examination and serum/urine hCG levels was analysed. There is a significant decrease in hCG levels in the first few days following MtoP [31–33]. This study also reported a significant decrease in hCG levels after successful MToP. However, low levels of hCG may persist 4–6 weeks after complete abortion. Therefore, a routine, high sensitivity urine pregnancy test with a positive result is not suitable for determining the effectiveness of MToP [1].
Establishing the serum hCG level is a very reliable method [15,34], which was also confirmed in this study. All ongoing pregnancies and missed abortions were diagnosed using a cut-off value of 1,000. Establishing the serum hCG level is not influenced by experience of the examiner, as is the case during US examination. A disadvantage is the necessity of a blood draw from the woman. Both the US examination and blood draw require the woman to visit the medical facility. This may lead to a loss in follow-up of some women and possibly non-recognition of an ongoing pregnancy, such as in women with no pregnancy symptoms [35].
In the hands of an experienced physician, US examination is a fast and effective method. If the US examination is performed by an inexperienced examiner, who does not have sufficient experience with the MToP method, it can lead to excessive indications for instrumental revision of the uterine cavity. Enlargement of the uterine cavity and the presence of blood coagula may be misinterpreted to be residual tissue. Surgical intervention should be performed on the basis of clinical symptoms, such as heavy or prolonged bleeding, not solely based on ultrasound examination (with the exception of a continuing pregnancy) [14,16]. Only one woman from our set had to undergo surgical intervention after successful MToP due to clinical symptoms, even though the enlargement of the uterine cavity was not significantly greater than in the other women.
The LSUP test is an alternative for follow-up after MToP. The test is comparably successful to ultrasound examination [36]. In our patient set, the LSUP test diagnosed all ongoing pregnancies as well as missed abortions. The client can perform the test by herself in a home setting and report the result over the phone. In combination with a series of questions regarding bleeding and pregnancy symptoms, it is also a very effective method [37]. For most women this would be the method of choice to monitor the success of MtoP [38,39].
Conclusion
At pregnancy diagnosis, there is a medium strong positive correlation between serum hCG and CRL. In MToP follow-up, a negative LSUP test enables reliable exclusion of ongoing pregnancy and missed abortion; in case of a positive LSUP test, US examination should be performed; however, surgical intervention should not be indicated solely on the basis of uterine cavity dilatation.
Declarations
Ethics approval and consent to participate
All women in our study had to submit a written request for termination of pregnancy and meet the conditions for the provision of this health service established by the legislation of the Czech Republic. Before the provision of the health service, they signed a detailed informed consent to the provision of the health service, its description and subsequent data collection. During the study, all women at the University Hospital Olomouc, requesting a pharmacological termination of pregnancy, underwent the same procedure, which was completely in accordance with the latest world knowledge. Our study was not an experiment; it was the provision of an implemented health service and the collection of data from this service. At that time, it was the standard protocol at the Olomouc University Hospital.
The study (research) protocol was approved by the Ethics committee of the Olomouc University Hospital and Faculty of Medicine Palacky University Olomouc.
All methods were carried out in accordance with relevant guidelines and regulations.
Informed consent was obtained from all subjects.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available, as they are clinical data from the Olomouc University Hospital, but are available from the corresponding author upon reasonable request.
Author contributions
VD: manuscript writing, literature search, data analysis, data collection
PS: data collection, data analysis
MMT: data collection
KL: bio chemical analysis
VK: data collection
ML: expert opinion and supervision of the study, data analysis, data interpretation, critical reading and review of the manuscript
All authors read and approved the final manuscript.
ORCID authors
V. Dvorak 0000-0001-5029-4674
P. Slunska 0000-0003-0952-1745
M. Maderkova Tozzi 0000-0001-5857-9738
K. Langova 0000-0003-2387-0183
R. Pilka 0000-0001-8797-1894
M. Lubusky 0000-0003-0551-0942
Submitted/Doručené: 19. 9. 2023
Accepted/Přijaté: 20. 9. 2023Prof. Marek Lubusky, MD, PhD, MHA
Fetal Medicine Centre
Department of Obstetrics and Gynecology
Faculty of Medicine
Palacky University Olomouc
Olomouc University Hospital
Zdravotníků 248/7
779 00 Olomouc
marek@lubusky.com
Zdroje
1. Fiala C, Bombas T, Gemzell-Danielson K et al. Early medical abortion – a practical guide for healthcare. 2nd edition. Paris: Editions de Santé 2018.
2. Moreau C, Trussell J, Desfreres J et al. Medical vs. surgical abortion: the importance of women’s choice. Contraception 2011; 84 (3): 224–229. doi: 10.1016/j.contraception.2011.01.011.
3. WHO. Safe abortion: technical and policy guidance for health systems. WHO guidelines approved by the guidelines review committee. 2nd edition. Geneva: WHO 2012.
4. Ho PC. Women‘s perceptions on medical abortion. Contraception 2006; 74 (1): 11–15. doi: 10.1016/j.contraception.2006.02.012.
5. Robson SC, Kelly T, Howel D et al. Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS). Health Technol Assess 2009; 13 (53): 1–124, iii–iv. doi: 10.3310/ht13530.
6. Winikoff B, Ellertson C, Elul B et al. Acceptability and feasibility of early pregnancy termination by mifepristone-misoprostol. Results of a large multicenter trial in the United States. Mifepristone Clinical Trials Group. Arch Fam Med 1998; 7 (4): 360–366. doi: 10.1001/archfami.7.4.360.
7. Lubusky M. Umělé přerušení těhotenství: hledisko medicínské, organizační, legislativní a ekonomické. Gyn Por 2016; 1 (1): 12–29.
8. Lubusky M. Umělé přerušení těhotenství na žádost pacientky farmakologickou metodou, nepřesahuje-li těhotenství sedm týdnů. Gyn Por 2018; 2 (5): 314–316.
9. CGPS. Medical termination of pregnancy until the 49th day of secondary amenorrhea (gestational age). Ceska Gynekol 2014; 79 (2): 240–241.
10. Fiala C, Bombas T, Parachini M et al. Management of very early medical abortion – an international survey among providers. Eur J Obstet Gynecol Reprod Biol 2020; 246 : 169–176. doi: 10.1016/j.ejogrb.2020.01.022.
11. Ghosh J, Papadopoulou A, Devall AJ et al. Methods for managing miscarriage: a network meta-analysis. Cochrane Database Syst Rev 2021; 6 (6): CD012602. doi: 10.1002/14651858.CD02602.pub2.
12. Chu JJ, Devall AJ, Beeson LE et al. Mifepristone and misoprostol versus misoprostol alone for the management of missed miscarriage (MifeMiso): a randomised, double-blind, placebo-controlled trial. Lancet 2020; 396 (10253): 770–778. doi: 10.1016/S0140-6736 (02) 31788-8.
13. Fiala C, Cameron S, Bombas T et al. Outcome of first trimester medical termination of pregnancy: definitions and management. Eur J Contracept Reprod Health Care 2018; 23 (6): 451–457. doi: 10.1080/13625187.2018.1535 058.
14. Fiala C, Gemzel-Danielsson K. Review of medical abortion using mifepristone in combination with a prostaglandin analogue. Contraception 2006; 74 (1): 66–86. doi: 10.1016/ j.contraception.2006.03.018.
15. Fiala C, Safar P, Bygdeman M et al. Verifying the effectiveness of medical abortion; ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol 2003; 109 (2): 190–195. doi: 10.1016/s0301-2115 (03) 00012-5.
16. Reeves MF, Fox MC, Lohr PA et al. Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol 2009; 34 (1): 104–109. doi: 10.1002/uog.6404.
17. Kulier R, Kapp N, Gülmezoglu AM et al. Medical methods for first trimester abortion. Cochrane Database Syst Rev 2011; 9 (11): CD002855. doi: 10.1002/14651858.CD002855.pub4.
18. Blum J, Shochet T, Lynd K et al. Can at-home semi-quantitative pregnancy tests serve as a replacement for clinical follow-up of medical abortion? A US study. Contraception 2012; 86 (6): 757–762. doi: 10.1016/j.contraception.2012.06. 005.
19. Gnoth C, Johnson S. Strips of hope: accuracy of home pregnancy tests and new developments. Geburtshilfe Frauenheilkd 2014; 74 (7): 661–669. doi: 10.1055/s-0034-1368589.
20. Montagnana M, Trenti T, Aloe R et al. Human chorionic gonadotropin in pregnancy dia g – nostics. Clin Chim Acta 2011; 412 (17–18): 1515–1520. doi: 10.1016/j.cca.2011.05.025.
21. Lipscomb GH, Stovall TG, Ling FW. Nonsurgical treatment of ectopic pregnancy. N Engl J Med 2000; 343 (18): 1325–1329. doi: 10.1056/NEJM20 0011023431807.
22. Doubilet PM. Ultrasound evaluation of the first trimester. Radiol Clin North Am 2014; 52 (6): 1191–1199. doi: 10.106/j.rcl.2014.07.004.
23. Bizjak I, Fiala C, Berggren L et al. Efficacy and safety of very early medical termination of pregnancy: a cohort study. BJOG 2017; 124 (13): 1993–1999. doi: 10.1111/1471-0528.14904.
24. Faucher P. The first comparative study on very early medical termination of pregnancy, with and without ultrasound confirmation of an intrauterine pregnancy. BJOG 2017; 124 (13): 2000. doi: 10.1111/1471-0528.14951.
25. Dvořák V jr, Ľubušký M. Využití misoprostolu (prostaglandinu E1) při chirurgickém ukončení těhotenství v I. trimestru a v gynekologii. Gyn Por 2019; 3 (5): 300–302.
26. Abubeker FA, Lavelanet A, Rodriguez MI et al. Medical termination for pregnancy in early first trimester (≤ 63 days) using combination of mifepristone and misoprostol or misoprostol alone: a systematic review. BMC Womens Health 2020; 20 (1): 142. doi: 10.1186/s12905-020-01003-8.
27. Morris JL, Winikoff B, Dabash R et al. FIGO‘s updated recommendations for misoprostol used alone in gynecology and obstetrics. Int J Gynaecol Obstet 2017; 138 (3): 363–366. doi: 10.1002/ijgo.12181.
28. Blum J, Raghavan S, Dabash R et al. Comparison of misoprostol-only and combined mifepristone-misoprostol regimens for home-based early medical abortion in Tunisia and Vietnam. Int J Gynaecol Obstet 2012; 118 (2): 166–171. doi: 10.1016/j.ijgo.2012.03.039.
29. Ngoc NT, Blum J, Raghavan S et al. Comparing two early medical abortion regimens: mifepristone + misoprostol vs. misoprostol alone. Contraception 2011; 83 (5): 410–417. doi: 10.1016/j.contraception.2010.09.002.
30. Slunska P, Hanacek J, Fanta M et al. Management of Medical Termination of Pregnancy (MToP) up until the 7th week of gestation in the Czech Republic. Ceska Gynekol 2017; 82 (5): 336–344.
31. Barnhart K, Sammel MD, Chung K et al. Decline of serum human chorionic gonadotropin and spontaneous complete abortion: defining the normal curve. Obstet Gynecol 2004; 104 (5 Pt 1): 975–981. doi: 10.1097/01.AOG.0000142712.80407.fd.
32. Honkanen H, Ranta S, Ylikorkala O et al. The kinetics of serum hCG and progesterone in response to oral and vaginal administration of misoprostol during medical termination of early pregnancy. Hum Reprod 2002; 17 (9): 2315–2319. doi: 10.1093/humrep/17.9.2315.
33. Pocius KD, Bartz D, Maurer R et al. Serum human chorionic gonadotropin (hCG) trend within the first few days after medical abortion: a prospective study. Contraception 2017; 95 (3): 263–268. doi: 10.1016/j.contraception. 2016.09.007.
34. Behnamfar F, Mahdian M, Rahimi F et al. Misoprostol abortion: ultrasonography versus beta-hCG testing for verification of effectiveness. Pak J Med Sci 2013; 29 (6): 1367–1370. doi: 10.12669/pjms.296.3361.
35. Grossman D, Grindlay K. Alternatives to ultrasound for follow-up after medication abortion: a systematic review. Contraception 2011; 83 (6): 504–510. doi: 10.1016/j.contraception. 2010.08.023.
36. Clark W, Bracken H, Tanenhaus J et al. Alternatives to a routine follow-up visit for early medical abortion. Obstet Gynecol 2010; 115 (2 Pt 1): 264–272. doi: 10.1097/AOG.0b013e3181c99 6f3.
37. Fiala C, Bombas T, Parachini M et al. hCG testing to determine outcome after medical abortion: A Review. J Preg Child Health 2019; 6 (2): 409. doi: 10.4172/2376-127X.1000409.
38. Cameron ST, Glasier A, Dewart H et al. Telephone follow-up and self-performed urine pregnancy testing after early medical abortion: a service evaluation. Contraception 2012; 86 (1): 67–73. doi: 10.1016/j.contraception. 2011.11. 010.
39. Cameron ST, Glasier A, Johnstone A et al. Can women determine the success of early medical termination of pregnancy themselves? Contraception 2015; 91 (1): 6–11. doi: 10.1016/ j.contra ception.2014.09.009.
Štítky
Dětská gynekologie Gynekologie a porodnictví Reprodukční medicína
Článek vyšel v časopiseČeská gynekologie
Nejčtenější tento týden
2023 Číslo 6- Alergie na antibiotika u žen s infekcemi močových cest − poznatky z průřezové studie z USA
- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Isoprinosin je bezpečný a účinný v léčbě pacientů s akutní respirační virovou infekcí
-
Všechny články tohoto čísla
- Is there a difference between acute appendicitis in pregnant and non-pregnant women?
- Are the serum delta neutrophil index and systemic inflammatory index useful as predictive parameters for preeclampsia and HELLP syndrome?
- Medical Termination of Pregnancy (MToP) in the 1st trimester – the role of human chorionic gonadotropin and ultrasound in pregnancy diagnosis and MToP follow-up
- Pregnancy termination indications and outcomes before 24 weeks of gestation – a case series
- An updated perspective on diagnostics and treatment of idiopathic granulomatous mastitis
- A rare case of a live abdominal pregnancy in a woman with subsequent gestation in utero
- DNA analysis of partial hydatidiform mole revealing triandric monogynic tetraploidy
- Outcome of a patient with Herlyn-Werner-Wunderlich syndrome treated with Balloon septostomy – pre- and postsurgical ultrasound findings
- Methods and techniques of fertility preservation in patients with endometriosis
- Assisted oocyte activation
- Effect of pelvic floor status on the outcome of pelvic organ prolapse surgery
- Preeclampsia and diabetes mellitus
- Diagnosis of complicated gynaecological inflammations by computed tomography – one center experience
- Emergent hysterectomy for placenta accreta spectrum – some additional techniques
- Diagnostika a léčba endometriózy: Doporučený postup Sekce pro léčbu endometriózy ČGPS ČLS JEP
- Česká gynekologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Diagnostika a léčba endometriózy: Doporučený postup Sekce pro léčbu endometriózy ČGPS ČLS JEP
- Preeclampsia and diabetes mellitus
- Assisted oocyte activation
- Is there a difference between acute appendicitis in pregnant and non-pregnant women?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



