-
Medical journals
- Career
Per-oral endoscopic pyloromyotomy (g-poem) for the treatment of gastroparesis – a pilot single-centre study with mid-term follow-up
Authors: R. Husťak 1,2; Z. Vacková 1; J. Krajciova 1; M. Janicko 3; M. Buncová 4; E. Kieslichová 5; J. Spicak 1; J. Martínek 1,6,7
Authors‘ workplace: Department of Hepatogastroenterology, Institute for Clinical and Experimental Medicine (IKEM), Prague 1; Department of Laboratory Testing Methods in Health Care, Faculty of Health Sciences and Social Work, University of Trnava 2; Department of Nuclear Medicine, IKEM, Prague 4; Department of Anesthesiology and Intensive Care, IKEM, Prague 5; Institute of Physiology, Charles University in Prague, Prague 6; Faculty of Medicine, Ostrava University, Ostrava 7; st Department of Internal Medicine, University Hospital and Faculty of Medicine, Pavol Jozef Safarik University in Kosice, Kosice 31
Published in: Rozhl. Chir., 2020, roč. 99, č. 3, s. 116-123.
Category: Original articles
doi: https://doi.org/10.33699/PIS.2020.99.3.116–123Overview
Introduction: Endoscopic pyloromyotomy (G-POEM) is an emerging therapeutic method for the treatment of gastroparesis (GP). So far, only limited case-series suggesting its effectivity have been published. The aim of our study was to assess the effectivity of G-POEM in patients with refractory GP.
Methods: Consecutive patients with severe and refractory GP were offered the procedure. An abnormal gastric emptying study (GES) was necessary for inclusion. The main outcome was treatment success defined as a decrease of the total GSCI symptom score by at least 40% from baseline at 3, 6, 12 and 24 months.
Results: G-POEM was performed in 9 patients (5 women, mean age 56.3): 5 post-surgical, 2 diabetic, 1 idiopathic and 1 combined post-surgical and diabetic. The median follow-up was 23M (range 12–31). All procedures were successfully completed. One patient experienced delayed bleeding from gastric ulceration, which was successfully treated endoscopically; all remaining patients recovered uneventfully. Treatment success was achieved in 8/9 patients (88.9%) at 3, 6 and 12M and in 3/4 (75%) at 24M. The mean GSCI decreased from 3.16 to 0.86 (p=0.008), 0.74 (p=0.008), 1.07 (p=0.008) and 1.31 (p=0.11) at 3, 6, 12 and 24M after the procedure. The Quality of Life Index improved from the baseline value of 77 (range 48−102) to 113 (86–138, p=0.03) and 96 (50–124, p=0.4) at 12 and 24M. In patients with treatment success, no recurrences have occurred so far. GES improved/normalized in all the patients.
Conclusion: G-POEM was effective in 88.9% of patients with refractory GP and the effect seems to be long-lasting.
Keywords:
endoscopic pyloromyotomy – gastroparesis − gastric emptying scan − gastric emptying
INTRODUCTION
Gastroparesis (GP) is a gastric motility disorder, defined as symptomatic delayed gastric emptying (GE) in the absence of any mechanical obstruction. In clinical practice, idiopathic and diabetic gastroparesis are the most common aetiologies, each accounting for about one third of the patients [1]. Gastroparesis may also develop as a consequence of oesophageal or gastric surgery; other causes comprise neurological, infectious, and infiltrative disorders [2] vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain. Management of gastroparesis should include assessment and correction of nutritional state, relief of symptoms, improvement of gastric emptying and, in diabetics, glycemic control. Patient nutritional state should be managed by oral dietary modifications. If oral intake is not adequate, then enteral nutrition via jejunostomy tube needs to be considered. Parenteral nutrition is rarely required when hydration and nutritional state cannot be maintained. Medical treatment entails use of prokinetic and antiemetic therapies. Current approved treatment options, including metoclopramide and gastric electrical stimulation (GES, approved on a humanitarian device exemption. Patients with gastroparesis suffer from dyspepsia, nausea, vomiting, regurgitation, weight loss and poor nutritional status. Traditionally, gastroparesis has been considered as a disorder caused by gastric hypomotility and the role of pyloric muscle might have been underestimated. Recent studies have shown that pyloric sphincter pressure is elevated in a not negligible number of patients with gastroparesis and, therefore, “pylorospasm”, initially described as abnormally prolonged, high-amplitude pyloric contractions in diabetic patients with nausea and vomiting [3], may be an underlying cause (or an additional pathophysiological factor) responsible for gastroparesis. Treatment methods targeting the pyloric muscle leading to its decreased tone may therefore provide a therapeutic effect.
Effective treatment for gastroparesis has been a true clinical challenge especially in patients with severe symptoms. Dietary measures and pharmacologic therapy have limited or no efficacy [4]. Endoscopic or surgical therapies may be considered in patients with refractory gastroparesis, in whom conservative measures were not effective. A majority of endoscopic or surgical approaches target the pyloric sphincter. Endoscopic methods include an intrapyloric botulinum toxin injection and trans-pyloric stent placement. The injection of botulinum toxin is only partially effective [5−6], and a systematic review did not confirm its clinical effectiveness [5]. Stenting seems to be effective but provides only a short-term relief with a considerable risk of stent migration [6]. Laparoscopic pyloroplasty according to Heineke-Mikulicz is the surgical method [7]. Two studies reported clinical improvement in approx. 80% of patients who underwent laparoscopic pyloroplasty [8].
To assess the severity of gastroparesis-related symptoms, the Gastroparesis Cardinal Symptom Index (GCSI) has been developed for this item. The GCSI consists of 9 symptoms with three subscales that are graded by the patient with a symptom recall of 2 weeks. The GCSI is part of a larger questionnaire PAGI-SYM (Patient Assessment of Upper Gastrointestinal Symptom severity index) established to assess patient-reported symptoms in gastroparesis (dyspepsia and gastroesophageal reflux). PAGI-SYM as well as GCSI subscale scores varied significantly by global disease severity, with higher (worse) scores observed in those subjects who rated their gastroparesis as moderate to severe (mean GCSI >2.3 means severe gastroparesis).
G-POEM (gastric per-oral endoscopic pyloromyotomy) is a novel endoscopic method based on a principle of submucosal tunnelling. Khashab et al. performed the first human G-POEM in a patient with severe refractory gastroparesis with an excellent symptomatic improvement after the procedure [9]. Since then, several groups reported promising results of G-POEM reaching a clinical effect in 73−86% of patients [10]. So far, approximately 200 cases of G-POEM have been recorded in literature worldwide with no or rare adverse events [10]. Patients with idiopathic or post-surgical gastroparesis may respond better compared to patients with diabetic gastroparesis [11]. Thus, G-POEM seems to be a promising mini-invasive method for the treatment of selected patients with refractory gastroparesis, although its role in the management of gastroparesis still needs to be elucidated. In our centre, we performed the first G-POEM in November 2015. The main aim of our study was to analyse outcomes of 9 consecutive patients who underwent G-POEM in our centre and were followed up for at least 12 months.
METHODS
This is a retrospective analysis of prospectively collected data of 9 consecutive patients who underwent G-POEM for refractory gastroparesis at our centre between November 2015 and November 2017. All patients signed an informed consent form and the protocol was approved by the local Ethics Committee and by the Ministry of Health of the Czech Republic as G-POEM is still considered an experimental procedure.
Patients
Patients over 18 years old suffering from severe refractory gastroparesis (symptom duration >6 months, GSCI (Gastroparesis Cardinal Symptom Index) >2.3, ineffective conservative measures such as diet modification, prokinetic drug(s), nutritional support) were eligible for enrolment. The patients were eligible for inclusion only when delayed gastric emptying scintigraphy (GES, retention of Tc-99m >60% at 2 h and/or ≥10% of residual activity at 4 h on a standardized sulphur colloid solid-phase) objectively proved their condition. Exclusion criteria were: prior endoscopic pyloromyotomy, severe coagulopathy, regular administration of opioids, oesophageal varices, liver cirrhosis, activereflux oesophagitis, active peptic ulcer, pregnancy, active gastric malignancy, mental eating disorders, organic pyloric stricture, intestinal obstruction and eosinophilic gastroenteritis. Patients with functional dyspepsia were also excluded.
Pre-procedural evaluation
Prior to G-POEM, GSCI and the quality of life score (Gastrointestinal Quality of Life Index; GIQLI by Eypasch, Wood-Dauphinee and Troidl) were assessed and upper GI endoscopy and gastric emptying study were performed. In patients tested positive for H. pylori, the treatment of this infection was discussed with the patient individually. Treatment of H. pylori infection was not necessary before enrolment unless there was an absolute indication for its treatment. Patients had fasted for at least 24 hours and were admitted to the hospital one day before the procedure and upper GI endoscopy was performed to remove potential food residues. Blood was drawn to assess WBC, RBC, CRP, to test liver and renal functions, and to assess potassium and sodium levels.
G-POEM procedure
All procedures were performed by one experienced endoscopist (JM) under general anaesthesia in an endoscopic unit using a high-definition endoscope (Olympus H180J; Olympus, Center Valley, PA, US), fitted with a transparent plastic distal attachment piece (Olympus MH-588, Olympus Medical System, Tokyo, Japan or Fuji ST Hood DH-28GR, Tokyo, Japan). CO2 was used for insufflation (CO2 regulation unit, Olympus Medical System). We used a triangle-tipped (TT) knife (Olympus Corporation, Tokyo, Japan) without and later with a jet function for the whole procedure. For mucosal entry, we used VIO-300D (ERBE, Tübingen, Germany) endocut Q – mode (effect 2, 40−60 W), for tunnelling and myotomy we used spray coagulation (effect 2, 40−60 W). Coag-Grasper (Olympus Corporation, Tokyo, Japan) or TT knife were used for hemostasis. A single dose of omeprazole 40 mg i.v. was given to patients at 6 : 00–7 : 00am, and sixty to fifteen minutes before the procedure ceftriaxone 2 g and metronidazole 500 mg were administrated intravenously by a nurse or by the anaesthesiologist at the endoscopic unit. The procedure started with submucosal injection followed by longitudinal mucosal incision done approximately 5 cm proximally from the pylorus on the great curvature. Submucosal tunnel was then created towards the pyloric muscle. After finding the pyloric arc, the muscle was myotomised at the 6 o´clock position up to the serosa (Fig. 1). At the end of the procedure, the mucosal incision was closed using hemoclips (high resolution clips, Boston Scientific, Marlborough, MA, USA or EZ Clip™ HX-1100QR, Olympus), and if necessary, we used the endoscopic suturing system (The OverStitch™, Austin, Texas) as a rescue closure technique.
1. A) Endoscopic view of the longitudinal mucosal incision; B) Endoscopic suturing system used for mucosotomy closure; C) Successful closure. 
Post-procedural management
After the procedure, patients were administered omeprazole i.v. and on POD 1, a second dose of ceftriaxone (2 g) was administered. On POD 1, a control fluoroscopy study with water-soluble contrast was performed to exclude leakage. If no leak was present, patients were allowed to drink and to eat liquid diet and were discharged on POD 1 or 2. Patients were given a PPI (esomeprazole 2x40 mg) orally for 1 month. In case a leak was revealed, upper GI endoscopy with an additional intervention (clipping) was carried out to secure the mucosal closure.
Follow-up
Patients were followed up at 3, 6, 12 and 24 months after G-POEM. The Gastroparesis Cardinal Symptom Index and a QoL questionnaire were obtained at each follow-up visit at the clinic. A gastric emptying study and upper gastrointestinal endoscopy were performed 3 months after the G-POEM procedure.
Outcomes
The main outcome was the treatment success rate at 3, 6, 12 and 24 months after the procedure. Treatment success was defined as a decrease of the total GSCI score of at least 40% from its baseline value. Secondary outcomes included evolution of GSCI and gastric emptying study throughout the follow-up period, quality of life and the safety and technical feasibility of the procedure.
Statistical analysis
The data is presented as means with standard deviation, medians with percentiles or as proportions of subjects with a given characteristic. Paired t-test was used to compare pre - and post-treatment results (GSCI, GSCI sub-scores, GES) and a p-value less than 0.05 was considered as statistically significant. The p-values were calculated using the two-sided paired t-test and were corrected for FWER (Family Wise Error Rate) using the Holm-Bonferroni method (as the total GSCI is an aggregation of 9 symptom scores, normality of the data can be assumed).
RESULTS
Patients
A total of 9 (5 women) patients underwent G-POEM at our institution for refractory gastroparesis till November 2017 and were analysed in the present study. The aetiologies were as follows: post-surgical (pGP) in 5 patients (55.6%), diabetic (dGP) in 2 (22.2%), idiopathic (iGP) in 1 (11.1%) and combined (post-surgical + diabetic) in 1 (11.1%) patient. Table 1 shows baseline characteristics of the patients. One patient from the cohort underwent G-POEM combined with POEM as a single procedure for coexisting idiopathic gastroparesis and achalasia and one female patient underwent G-POEM for gastroparesis after multivisceral transplantation despite previous (ineffective) surgical pyloroplasty. All nine patients completed the 12-month follow-up period; 4 patients completed the 24-month follow-up period. The mean length of hospital stay was 2.9 days (range: 1−6).
1. Baseline demographic data of the patients undergoing G-POEM 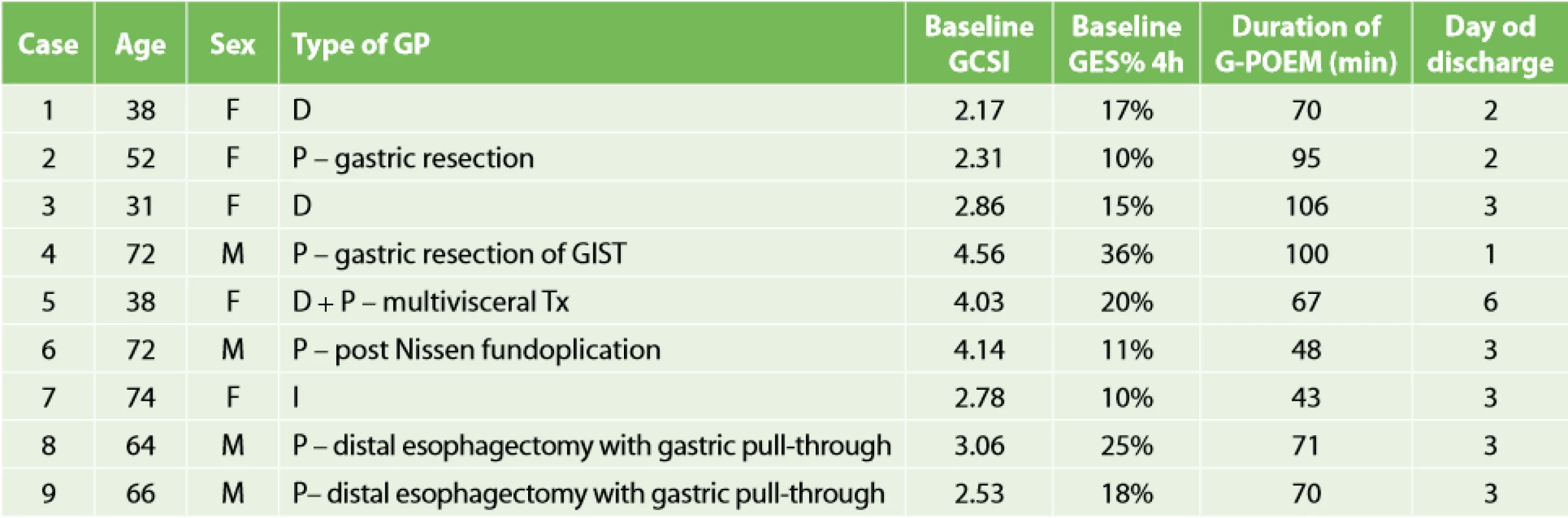
GP – gastroparesis. GCSI – Gastroparesis Cardinal Symptoms Index. D – diabetic. P – post-surgery. I – idiophatic. GES – Gastric Emptying Study. GIST – gastrointestinal stromal tumor. Tx – transplantation Procedure
G-POEM was completed successfully in all patients. The mean procedure time was 75±23 minutes and the pyloromyotomy length was 2.3±0.4 cm. Endoscopic clips were used to close the incision in 7 patients (median number of hemoclips was 8, range 5–19), while an endoscopic suturing system was used in two patients, in one case with excessive laceration of mucosotomy toward the pylorus (Fig. 1A, B, C). One closure with endoscopic clips was not completely successful as one clip had to be added on POD 1 because of a leak on X-ray.
Treatment efficacy
Treatment success was achieved in 8/9 (88.9%) at 3, 6 and 12M, and 3/4 (75%) at 24M. The mean GSCI score decreased from 3.16±0.82 to 0.86±0.63, 0.74±0.56, 1.07±0.62 and 1.31±0.82 (3/4 pts) at 3, 6, 12 and 24M after the procedure (baseline vs all other visits, Tab. 2). Detailed evolution of mean GCSI per case is summarized in Graph 1. No relapse or recurrence occurred in 8 patients with an initial treatment success. Median of the Gastrointestinal Quality of Life Index improved from 77 (range 48–1) before G-POEM to 108 (range 90–133, p=0.01), 114 (range 84–138, p=0.03), 113 (86–138, p=0.03) and 96 (50–124, p=0.4) at 3M, 6M, 12M and 24M. GES normalized or at least improved in all patients (Graph 2).
2. Effects of G-POEM on symptom severity for all 9 categories of GSCI + the total symptom score 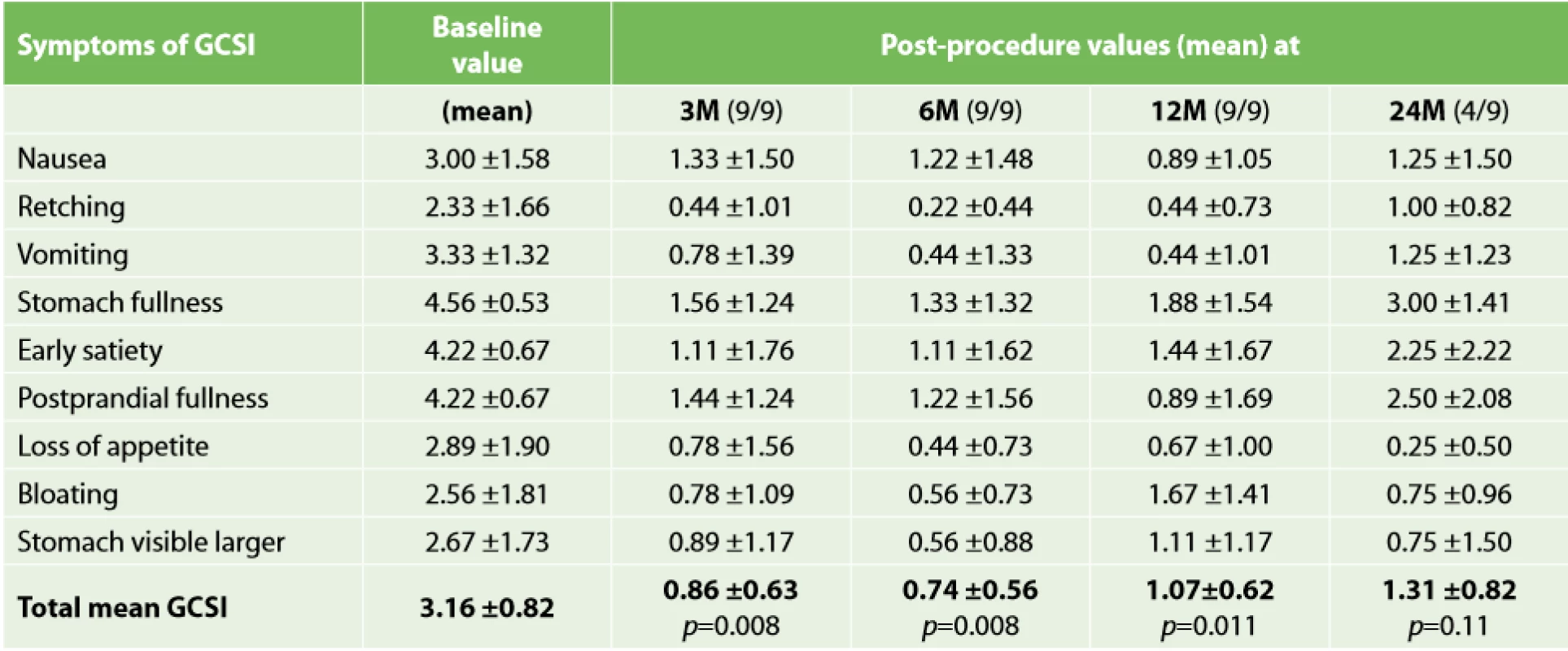
1. Mean GCSI evolution per patient during follow-up visits. All patients except one (1 dGP) reached treatment success 
2. Effects of G-POEM on evolution of 4h scintigraphic gastric % retention per case 
Adverse events
Periprocedural adverse events (AEs) were noted in 2 patients: one patient had an insufficient mucosotomy closure and had a leak on X-ray study (Clavien-Dindo complication classification type II) and one female with the history of multivisceral transplantation presented with delayed (8 days after G-POEM) gastrointestinal bleeding from a large ulceration at the site of the submucosal tunnel (Clavien-Dindo type IIIa) without peritonitis. Bleeding was successfully treated endoscopically and with intravenous proton pump inhibitor administration and nasojejunal tube placement for short-term feeding, and the patient was hospitalized for another 6 days to restart her oral immunosuppressant drugs treatment. A detailed medical history revealed that the patient accidentally stopped using PPI one week after G-POEM. In one patient, capnoperitoneum had to be decompressed using a venous cannula.
DISCUSSION
In our study, we have shown promising results of endoscopic pyloromyotomy (G-POEM) for the treatment of gastroparesis. The treatment was successful in all but one patient (8/9, 89%) and no significant recurrences occurred in those patients with an initial treatment success during a follow-up period of 1 (all patients) and 2 (4 patients) years. One female patient with dGP failed to experience an improvement of her symptoms although the GES completely normalized. Gastric emptying study normalized or improved in all patients. The procedure was relatively safe and we experienced one severe adverse event (delayed bleeding from ulceration at the site of submucous tunnelling), which was probably caused by erroneous withdrawal of a proton pump inhibitor shortly after the procedure.
Even though we analysed a rather small group of patients, there is a need to gather world-wide experience with regard to both efficacy and safety as G-POEM is still considered as an experimental procedure. The majority of so far published studies has been rather limited with respect to both the number of included patients and the length of the follow-up [12]. We believe that our (although limited) experience will provide additional evidence for efficacy and safety of G-POEM.
We performed the first G-POEM in November 2015, and only 9 procedures were done by November 2017, which was less than we had expected as we are a tertiary centre for submucosal endoscopy (more than 50 POEMs per year) and also a referral centre for specialised diabetology care. However, we are rather conservative with regard to patient selection for G-POEM; the patients have to suffer from severe and refractory gastroparesis. At present, performing G-POEM in patients with mild or moderate gastroparesis is not appropriate as there is more evidence needed to prove the efficacy of G-POEM in the treatment of gastroparesis. Our treatment efficacy was similar to that reported in other studies. A French group reported the short-term treatment success of 80% (10 out of 12 patients) and of 69% at 6 months [11,13] debilitating condition. We report an experience conducting gastric per-oral endoscopic pyloromyotomy (G-POEM. The authors found diabetic aetiology and female gender as possible predictors of treatment failure.
In a pooled analysis of 7 studies including 189 patients, the technical success was 100% and short-term clinical success (3M) was 81.5% [10]. In a recent large multicentre case series of gastric pyloromyotomy for the treatment of gastroparesis, G-POEM resulted in an excellent response rate, with 85 % of patients having both symptomatic and GES improvement. The mean follow-up was 11 months and this study is among only a few having reported relatively longer follow-up. Despite including only 9 patients in our study, all of them completed 12 months, and 4 of them 24 months of follow-up. Thus, our study reports mid - or long-term results, which are lacking in the majority of the other studies. Interestingly, among 8 patients with a treatment success, nobody recurred and the patients continue to have a long-standing improvement of their quality of live. Of note, the difference between a high baseline GSCI and lower GSCI at 24 months was not statistically significant due to the low number of patients who reached 24 months of the follow-up.
Thus, it seems that G-POEM may be effective in about 60−80% of patients with gastroparesis. There are several questions which need to be answered before G-POEM may be considered as a standard clinical procedure. These questions especially concern 1) indications, 2) efficacy, 3) safety, 4) technical performance and 5) comparison with other treatments.
At present, there are no clear indications for G-POEM and all patients suffering from refractory gastroparesis may be suitable candidates for G-POEM, especially those patients with a visible pyloric spasm on endoscopy and/or patients with an effect of botulinum toxin (BT) injection/dilatation/temporary transpyloric stent placement. However, the etiopathogenesis of gastroparesis is very complex and a pylorospasm may play an important role in some (but probably not in all) patients suffering from the disease. The principal problem is that we do not have a reliable tool for assessing the pyloric function (a measurement of pyloric compliance – Endoflip – may be a promising method in the future). It should be noted that the efficacy of BT remains controversial – according to a randomized study, BT is not an effective treatment of gastroparesis [14]. Moreover, all physicians who are experienced in managing patients with this disease know that psychological factors play an important role and a “placebo” response could not be ruled out in cases where a dilatation or BT injection provide a short-term relieve. Thus, appropriate indications for G-POEM should be defined in the near future. Moreover, approaching G-POEM in patients suffering from mild to moderate gastroparesis (GCSI >2.0) is dubious.
As already described, short-term efficacy seems promising and long-term data is missing. G-POEM is undoubtedly a new method, attracting an interest. In interventional medical research, a new interesting topic leads often to a large number of small, usually retrospective studies, which are frequently mashed up in the so-called meta - or pooled - analyses. The follow-up is very short and there is usually no control group. Not surprisingly, these studies usually conclude that “the new method is excellent”. No doubt, this seems the case with G-POEM, as well. Nevertheless, management with either G-POEM or laparoscopic pyloroplasty does not preclude a future intervention with the other technique for patients with treatment failure. Both methods could be considered first-line interventions that preserve all other surgical options, in case any one of them fails. Since placebo responses could complicate the assessment of treatment success, G-POEM could be performed after a follow-up period of at least 6-month from the failure of pyloroplasty (and vice versa). Larger, prospective and controlled studies will probably show the results of G-POEM in a more realistic light.
G-POEM seems relatively safe, adverse events are rare and severe adverse events seem extremely rare. However, as we described in our study, severe AEs may occur and centres performing G-POEM should not underestimate this issue. The lesson learnt from our experience is that patients should have a prolonged (1−2 months) treatment with a proton pump inhibitor twice daily, otherwise a gastric ulceration at the site of the submucosal tunnel may occur. Other delayed non-fatal bleeding events have also been reported [12].
With regard to technical aspects, as more G-POEMs are being performed world-wide, more subtle technical differences are noted. For example, the initial incision can be longitudinal or transversal. G-POEM can be performed on the anterior or posterior gastric wall. Or, several different methods can be used to close the mucosal incision. Obtaining an adequate mucosal closure is one of the most important steps of the procedure and is essential to avoid major morbidity. At present, simple closure with endoscopic clips has been the most frequently described method for mucosal closure in patients undergoing G-POEM. However, as gastric mucosa is thicker compared to the oesophagus and may lack elasticity, thus, endoscopic clips may not be an ideal closure method in the stomach, and therefore an endoscopic suturing system (OverStitch; Apollo) should be used as a rescue technique. In our opinion, the endoscopic clips may not work well in all circumstances as two of our patients needed either the addition of one clip on POD 1 (because of a leak) or a completely different closure method (endoscopic suturing system) because of excessive laceration of mucosotomy toward the pylorus. As in the case of POEM, these technical aspects need further assessment in prospective studies.
As G-POEM is a new procedure and its indications seem not as frequent compared to POEM, there are no studies comparing G-POEM to other treatments including laparoscopic pyloroplasty. This is currently the most common surgical treatment for patients with refractory gastroparesis and with the history of failed medical therapy. The technique has been evaluated in multiple studies with a similar rate of symptom improvement (70−80%) as reported for G-POEM [7]. In our study, one patient had undergone previous pyloroplasty, which was not effective and G-POEM resulted in a very good effect. Thus, previous pyloroplasty does not preclude subsequent endoscopic pyloromyotomy.
Our study has several limitations; the main is the small number of patients included and the retrospective nature of our analysis. Thus, our results should be interpreted with care. On the other hand, the long-term follow-up (at least 12 months) can be considered as a strong point of the study.
In conclusion, our study suggests that G-POEM may be an effective treatment modality for selected patients with refractory gastroparesis. We report a treatment success in 86% (8/9) of patients, with an improvement/normalisation of GES in all treated patients. Our study adds to the accumulating evidence supporting G-POEM as a technically feasible, relatively safe, and efficacious treatment option for patients with gastroparesis. However, larger prospective and controlled studies are necessary to confirm the preliminary promising data. While G-POEM is relatively safe, severe adverse events may occur.
Abbreviations:
CRP – C Reactive Protein
GCSI – Gastroparesis Cardinal Symptom Index
GE – Gastric Emptying
GP – Gastroparesis
GES – Gastric Emptying Scan
GIQLI – Gastrointestinal Quality of Life Index
G-POEM – Gastric Per-Oral Endoscopic Myotomy
TT – Triangle Tip knife
POD – Post-Operative Day
RBC – Red Blood Cells
WBC – White Blood Cells
Grant 17-28797A from the Czech Ministry of Health
Conflict of interests
The authors declare that they have no conflict of interest in connection with the article and that the article was not published in any other journal except congress abstracts and clinical guidelines.
MUDr. Rastislav Husťak
Department of Hepatogastroenterology
Institute for Clinical and Experimental Medicine
Videnska 1921
140 21 Prague 4
e-mail: rhustak@gmail.com
Sources
- Jung HK, Choung RS, Locke 3rd GR, et al. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology 2009;136 : 1225–1233. doi: 10.1053/j.gastro.2008.12.047.
- Camiller M, Parkman HP, Shafi MA, et al. Clinical guideline: Management of gastroparesis. Am J Gastroenterol. 2013;108 : 18–38. doi: 10.1038/ajg.2012.373.Clinical.
- Mearin F, Camilleri M, Malagelada JR. Pyloric dysfunction in diabetics with recurrent nausea and vomiting. Gastroenterology 1986. doi: 10.1016/0016-5085(86)90262-3.
- Quigley EM. Prokinetics in the management of functional gastrointestinal disorders. J Neurogastroenterol Motil. 2015;21 : 330–336. doi: 10.5056/jnm15094.
- Ukleja A, Tandon K, Shah K, et al. Endoscopic botox injections in therapy of refractory gastroparesis. World J Gastrointest Endosc. 2015;7 : 790–798. doi: 10.4253/wjge.v7.i8.790.
- Khashab MA, Besharati S, Ngamruengphong S, et al. Refractory gastroparesis can be successfully managed with endoscopic transpyloric stent placement and fixation (with video). Gastrointest Endosc. 2015;82 : 1106–1109. doi: 10.1016/j.gie.2015.06.051.
- Hibbard ML, Dunst CM, Swanstrom LL. Laparoscopic and endoscopic pyloroplasty for gastroparesis results in sustained symptom improvement. J Gastrointest Surg. 2011;15 : 1513–1519. doi: 10.1007/s11605-011-1607-6.
- Clarke JO, Snape Jr. WJ. Pyloric sphincter therapy: botulinum toxin, stents, and pyloromyotomy. Gastroenterol Clin North Am. 2015;44 : 127–136. doi: 10.1016/j.gtc.2014.11.010.
- Khashab MA, Ngamruengphong S, Carr-Locke D, et al. Gastric per-oral endoscopic myotomy for refractory gastroparesis: results from the first multicenter study on endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2016. doi: 10.1016/j.gie.2016.06.048.
- Khoury T, Mizrahi M, Mahamid M, et al. State of the art review with literature summary on gastric peroral endoscopic pyloromyotomy for gastroparesis. J Gastroenterol Hepatol. 2018;33(11):1829-1833. doi: 10.1111/jgh.14293.
- Gonzalez JM, Benezech A, Vitton V, et al. G-POEM with antro-pyloromyotomy for the treatment of refractory gastroparesis: mid-term follow-up and factors predicting outcome. Aliment Pharmacol Ther. 2017;46 : 364–370. doi: 10.1111/apt.14132.
- Li L, Spandorfer R, Qu C, et al. Gastric per-oral endoscopic myotomy for refractory gastroparesis: a detailed description of the procedure, our experience, and review of the literature. Surgical Endoscopy 2018;32(8):3421-3431. doi: 10.1007/s00464-018-6112-5.
- Gonzalez JM, Lestelle V, Benezech A, et al. Gastric per-oral endoscopic myotomy with antropyloromyotomy in the treatment of refractory gastroparesis: clinical experience with follow-up and scintigraphic evaluation (with video). Gastrointest Endosc. 2017;85 : 132–139. doi: 10.1016/j.gie.2016.07.050.
- Arts J, Holvoet L, Caenepeel P, et al. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26 : 1251–1258. doi: 10.1111/j.1365-2036.2007.03467.x.
Labels
Surgery Orthopaedics Trauma surgery
Article was published inPerspectives in Surgery

2020 Issue 3-
All articles in this issue
- Laparoscopic liver resections – state of art
- Right hemicolectomy – from laparoscopic facilitated technique to robotic intracorporeal anastomosis
- Our experience with transanal total mesorectal excision (TaTME) procedures in middle and distal rectal tumors
- Acute abdomen in pregnancy: a retrospective study of pregnant patients hospitalised for abdominal pain
- Perioperative acute internal carotid thrombosis after general surgery
- Lumbar hernia – case report
- „Quo vadis“ laparoskopická chirurgie… chirurgie 3.0?
- Diskuze k editorialu „Můžeme vyřešit současné problémy regionálních chirurgických pracovišť?“ prof. MUDr. M. Rysky v Rozhledech chirurgie 2/2020.
- Profesor Eduard Albert: není Impakt jako „impact“.
- Per-oral endoscopic pyloromyotomy (g-poem) for the treatment of gastroparesis – a pilot single-centre study with mid-term follow-up
- Perspectives in Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Right hemicolectomy – from laparoscopic facilitated technique to robotic intracorporeal anastomosis
- Acute abdomen in pregnancy: a retrospective study of pregnant patients hospitalised for abdominal pain
- Our experience with transanal total mesorectal excision (TaTME) procedures in middle and distal rectal tumors
- Lumbar hernia – case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

