-
Medical journals
- Career
Features of adherence to drug therapy elderly:the impact of the diseaseand form of the drug
(the results of research in the urban population of Ecuador)
Authors: K. Prashchayeu; Pobeda Padilla Ag; A. Ilnitski; Pobeda Padilla Va; E. Fesenko; T. Khadieva
Published in: Geriatrie a Gerontologie 2015, 4, č. 4: 203-208
Category: Original Article/Study
Overview
The problem of commitment to ongoing drug therapy is complex, multidimensional, it affects both patient and doctor, and also influenced by the form of the medication. The research was focused on revealing the peculiarities of commitment to the ongoing drug therapy in elderly patients depending on the nature of the disease and the form of the medicine. The research is based on a sample of the urban population of the Republic of Ecuador. 111 elderly patients were examined, the age of the respondents ranged from 65 to 74 years of age (the average age of 69.2+2.2 years and there were 49 men and 62 women). The elderly patients were interviewed using a purpose-made questionnaire. It was found out that among the elderly, the degree of commitment to drug therapy is 53.2 % and it is significantly lower than in middle aged patients, for whom the number stands at 78.4 %. The reasons for which the patient does not follow the prescribed treatment regimen can be grouped as follows: causes associated with the patient; social reasons; reasons related to the drugs; reasons related to issues of communication and interaction between the doctor and the patient. The commitment to drug therapy decreases in the elderly often based on the form in which the drug is administered, with eye drops, injectable forms of medicines, drugs directly contained in vials and large tablet forms of drugs being affected the worst.
Keywords:
elderly people – adherence to therapy – commitment – medicinal forms – forgetfulness – polypragmasy – polymorbidityIntroduction
Specifics of treatment of older people are an acute issue in theoretical and practical medicine. This is largely due to the peculiarities of the elderly organism with its reduced adaptive capacity and high level of morbidity(1).
Pharmacological methods are in the basic method of treatment in elderly people, despite the fact that they should be supplemented by non-drug (non-pharmacological) methods of rehabilitation to prevent excessive use of drugs(2).
The achievements of modern society in the field of pharmacology allowed to develop effective, strong medicines, thanks to which it became possible to treat serious diseases, thereby increasing the life expectancy of patients. However, the achieved the positive effects may be offset due to the fact that patients do not always scrupulously follow the doctor’s instructions.
According to scientific analyses, commitment to drug therapy in patients with chronic diseases rarely not exceeds 50 % even in developed countries.
In the poorly developed and developing countries, there is a lack of resources and poor access to medical care, and one can assume that in these populations the specific weight of the patients, are committed to the pharmaceutical therapy, even.
Adherence to drug therapy is a complex psychological and clinical phenomenon. Adherence to the therapy is the level of adherence of the patient’s behaviour the the recommendations, necessary for the preservation of his health: attendance at the planned appointments at clinics/hospitals, reception of drugs in accordance with the doctor’s prescriptions, a belief in the need to change the way of life in accordance with the advice of a doctor, a thorough documentation, necessary medical attention (for example, the diary of measurement of blood pressure)(3).
Older patients’ adherence to therapy decreases in connection with memory loss, loneliness, reduced intellectual ability and sensory deficit. All this makes the doctor-patient contact more difficult and reduces the degree of fulfilment of relatively simple prescriptions.
Age in itself is not a factor that reduces the commitment. Adherence to therapy depends primarily on the personal characteristics of the individual person regardless of his age.
Adherence to treatment is essential for the well-being of elderly patients and is an important component of their health. In elderly people, non-observance of the prescriptions of the doctor increases the likelihood of treatment failure, and may also lead to the occurrence of complications, which increases the costs of treatment(4).
Low adherence to treatment leading to poor compliance with treatment regimen, may have different forms: the patient has difficulties starting the treatment, the volatility of the admission of drugs or premature failure from them, incomplete understanding of the patient’s treatment schemes, namely, the lack of emphasis on the dose of the drug, the time of his admission and objectives, the need to change their traditional way of life for the improvement of the effects from the treatment, the lack of periodic consultations and etc.
In terms of adherence to therapy, age is not a factor of adherence to treatment, but the complex schemes of treatment often administered to the elderly, a large number of different drugs, as well as frequent depression and cognitive disorders in this group of patients may lead to a sharp reduction in commitment and adherence.
Low adherence to therapy is defined as the voluntary or involuntary non-adherence. Reasons for the lack of adherence varied. Basic causes of low adherence to therapy are distrust of the designated drug, inadequate assessment of the severity of the disease, low prestige of the specialist who has prescribed the therapy(5).
Thus, the problem of commitment to ongoing drug therapy is a complex, multidimensional, it affects both patient and doctor, and also administration of the medication. This question is of considerable specificity in relation to the people of elderly and senile age. Adherence to the drug therapy of people of senior age groups is an important and insufficiently studied problem especially in developing countries. The topical issue is studying of how the commitment is affected by age-sensitive: reduction of memory, geriatric features of the digestive system, especially the communication of a doctor with an elderly man, his economic status, etc. Knowledge of the specified range of issues will not only identify the state of adherence to the drug therapy, but also prove scientifically the ways of its increase, which will ultimately help improve the condition of persons of elderly and senile age, improving their quality of life(6).
The goal of this research is to reveal the peculiarities of commitment to the ongoing drug therapy in elderly patients depending on the nature of the disease and the form of the medicine.
Material and methods of research
Following dissertation research is based on the example of the urban population of the Republic of Ecuador. In this country demographic processes are fully consistent with global trends of demographic transition, when in connection with the socio-cultural and industrial factors there is reduction in mortality rates and increase in life expectancy at birth, while there is a decrease in the birth rate. This is naturally reflected in the proportion of persons of elderly and senile age in the population, which has a stable tendency to growth. Moreover, the problems of geriatric segment of the population are in need to search for new forms of prevention and treatment of such common diseases as osteoarthritis, osteoporosis, Alzheimer’s disease and other. The above allows to state that the laws of demographic changes and features of the population of persons of elderly and senile age in Ecuador are all-civilization character.
The data obtained in the survey, examination, and clinical observation of older persons in the Republic of Ecuador in 2009–2012, in the cities of La Libertad, Salinas, Santa Elena (province of Santa Elena), the city of Quito, the capital of the Republic of Ecuador (Pichincha) were analysed. Bases of the study were: non-profit centres of social support in the clinic «baste» (province of Santa Elena); state gerontology centre (province of Santa Elena); the state house for the elderly (Quito, Pichincha). All was examined 111 elderly patients, the age of the respondents ranged from 65 to 74 years of age (the average age of 69.2+2.2 years), and men – 49 pers., women – 62 people. These patients were the main group. The control group consisted of patients of middle age, who received treatment in outpatient centres clinic «baste» (province of Santa Elena). All were examined by the 88 patients of middle age, the age of the respondents varied from 40 to 49 years of age (the average age of a 47.1+2.8 years), and men – 46 persons, women – 42 people. In the study did not include patients requiring a stranger care, as well as with mental diseases, accompanied by intellectual reduction, cancer and severe haematological diseases.
Distribution of patients according to the nosological forms. From the last survey and the survey of 111 patients of advanced age of 50 patients (45.0 %) suffered from arterial hypertension, 26 (23.4 %) patients had osteoarthritis of various localization, 18 older people suffered from diabetes mellitus I and type II (16.2 %) and the same number (18 pers., or 16.2 %) were registered forms of coronary heart disease, osteoporosis was detected in 12 cases (10.8 %), chronic obstructive pulmonary disease – in 8 cases (7.2 %), 8 patients had Alzheimer’s disease (7.2 %), 7 - rheumatoid arthritis (6.3 %)and 7 patients had sensorineural hearing loss (6.3 %), registered hypercholesterolemia as an independent disease was in 6 patients (5.4 percent), non–alcoholic steatohepatitis registered in 6 cases (of 5.4 %), benign hyperplasia of the prostate gland – in 4 cases (of 3.6 %), iron-deficiency anaemia is also in 4 cases (10.8 %), myopia was noted in 12 cases (10.8 %), chronic gastritis in 3 cases (2.7 %), chronic otitis – in 3 cases (2.7 percent), and other nosological forms were registered in 37 patients (33.3 per cent). Thus, in 111 patients of elderly age, included in the study were registered 229 diseases, the index of polymorbidity amounted to 2.06.
From the last survey and the survey of 88 patients of middle age, 26 patients (29.5 %) suffered from arterial hypertension, 13 (14.7 %) of patients had osteoarthritis of various localization, 7 people suffered from diabetes mellitus I and type II (7.9 %), and 12 pers., or 13.6 %) had registered forms of coronary heart disease, osteoporosis was detected in 3 cases (3.4 %), chronic obstructive pulmonary disease in 6 cases (6.8 %),and 4 patients had rheumatoid arthritis (4.5 %), 3 patient – neurosensory baryecoia (3.4 %), registered hypercholesterolemia as an independent disease was in 4 patients (4.5 per cent), non-alcoholic steatohepatitis registered in 5 cases (5.7 %), benign hyperplasia of the prostate gland in 3 cases (3.4 %), iron deficiency anemia in 4 cases (4.5 %), myopia was observed in 9 cases (10.2 %), chronic gastritis in 6 cases (6.8 %), and chronic otitis – in 3 cases (3.4 %), the other nosological forms were registered in 12 patients (13.6 percent). Thus, in 88 patients of middle age, included in the study, there were 107 registered diseases, the index of polymorbidity amounted to 1.22.
This situation corresponded to the average levels of morbidity in the relevant age groups.
The diagnostics of diseases. Diagnostics of the diseases was carried out in accordance with the current recommendations of the world health organization and National guidelines of the Ministry of health of the Republic of Ecuador.
The method of interviewing. Interviewing elderly patients on the subject of commitment to the receiving therapy was carried out according to the original questionnaire and included open questions (asking for extended and long answers), which allowed to older patients to exactly express some of the problems, arising at the reception of the certain medicinal forms.
Questions were addressed to elderly people taking prescription drugs, with the aim of identifying problems in the treatment of different forms of drug, with the special way highlighted the difficulties encountered in the application of one or another form of the drug.
The questionnaire included detailed questions about different forms of production of drugs, taken by elderly patients (tablets in blisters, tablets in bottles, effervescent tablets, drops for internal reception, eye drops, injections, inhalers, gels and creams, adhesives for the skin) with a view to identifying the most inconvenient for the application of medicinal forms.
Statistical processing of the data. Statistical processing of the results of research carried out with the help of computer program Statistica 6.0. The significance of differences between the groups were determined with the help of the t-test student, Chi-square. Statistically considering the differences, with the appropriate error value the reliability of p<0,05.
The main results
In the course of the study it was found that when the main nosological forms with one and the same diseases of the degree of adherence to the prescribed doctor of treatment was significantly higher in people of middle age (table 1). Overall degree of adherence to therapy in older people was 53.2 % and was significantly lower, than in the middle aged patients (78.4 percent), p<0,05.
1. Adherence to therapy for people of different ages at the leading nosological forms 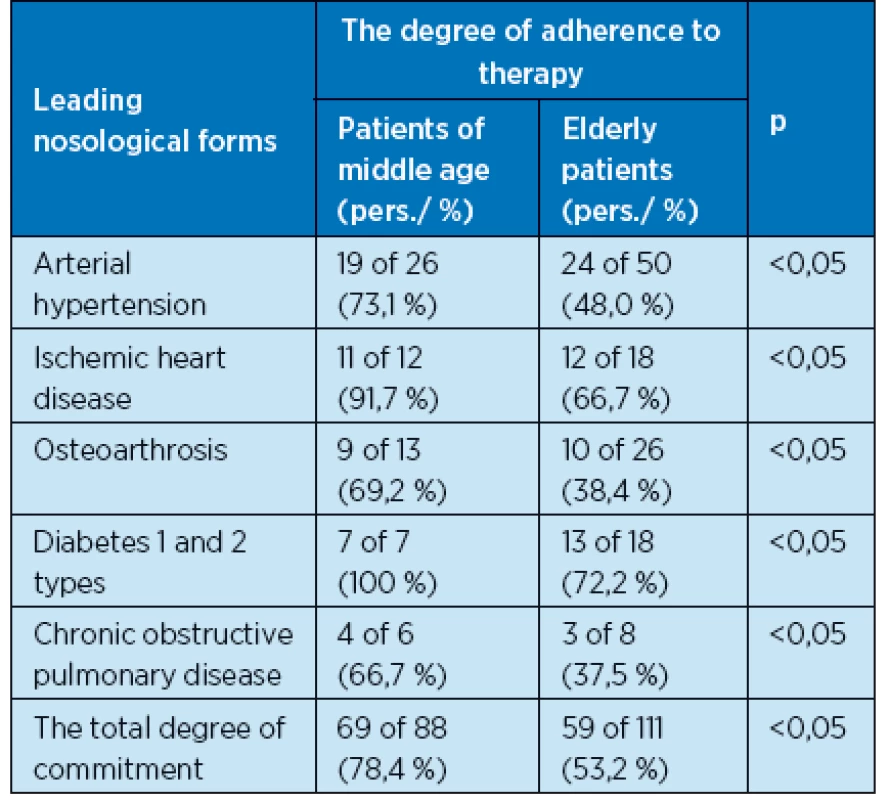
In the course of interviewing elderly patients found that the conduct of their drug therapy was accompanied by a considerable number of problems, different from the problems encountered in patients of middle age (Fig. 1).
Fig. 1 The main associated with the age of the problem of drug therapy (the share of persons with which these problems have arisen, in %). 
So, old age fairly often led to the reduction of adherence to therapy compared to patients of middle age (p<0.05) with factors such as fear of side-effects of therapy, forgetfulness when receiving the drugs, the presence of the articular syndrome and other physical difficulties that hinder the taking of medicines, an inconvenient size tablet forms, economic failure patients, the need to receive a large amount of drugs (полипрагмазия), health literacy of the patient.
In connection with the identified age peculiarities in the formation of adherence to therapy and the degree of its severity, we decided to detail the number of characteristics inherent in elderly patients.
It is revealed, that not only the age and age-associated features of physical and mental status were independent factors of decrease adherence to the prescribed drug therapy. An independent factor influencing the degree of adherence to therapy, may be the form of medicines, appointed by the doctor. In Figure 2 it is shown that the most often in the elderly commitment to the decline in the appointment of such medicinal forms as eye drops, injectable forms of medicines, drugs, contained in vials directly and tablet forms of drugs.
Fig. 2 The frequency of occurrence of problems in elderly patients with reception of medicinal forms, which contribute to the reduction of commitment to drug therapy 
It is revealed, that these problems are in the basis of the reduction of the commitment of elderly patients to the ongoing drug therapy. Reasons for the decline in commitment to vary depending on the nosological forms.
So, it is revealed, that in case of arterial hypertension in the elderly is important «forgetfulness» when receiving the drugs, χ2 = 7,9; the existence of a concomitant of osteoarthritis with pain syndrome, which violated the ton motility of fingers of hands and led to difficulties when removing the product from a factory of packaging, χ2 = 7,6; the large size pills of medicinal forms, which created the objective difficulties in swallowing, χ2 = 7,5; fear of side effects of drugs due for polypragmasia, χ2 = 7,4; inability to purchase drugs because of economic difficulties, χ2 = 7,3, p<0,05 (table. 2).
2. The main reasons for the decline in commitment of elderly patients to receiving drug therapy in arterial hypertension 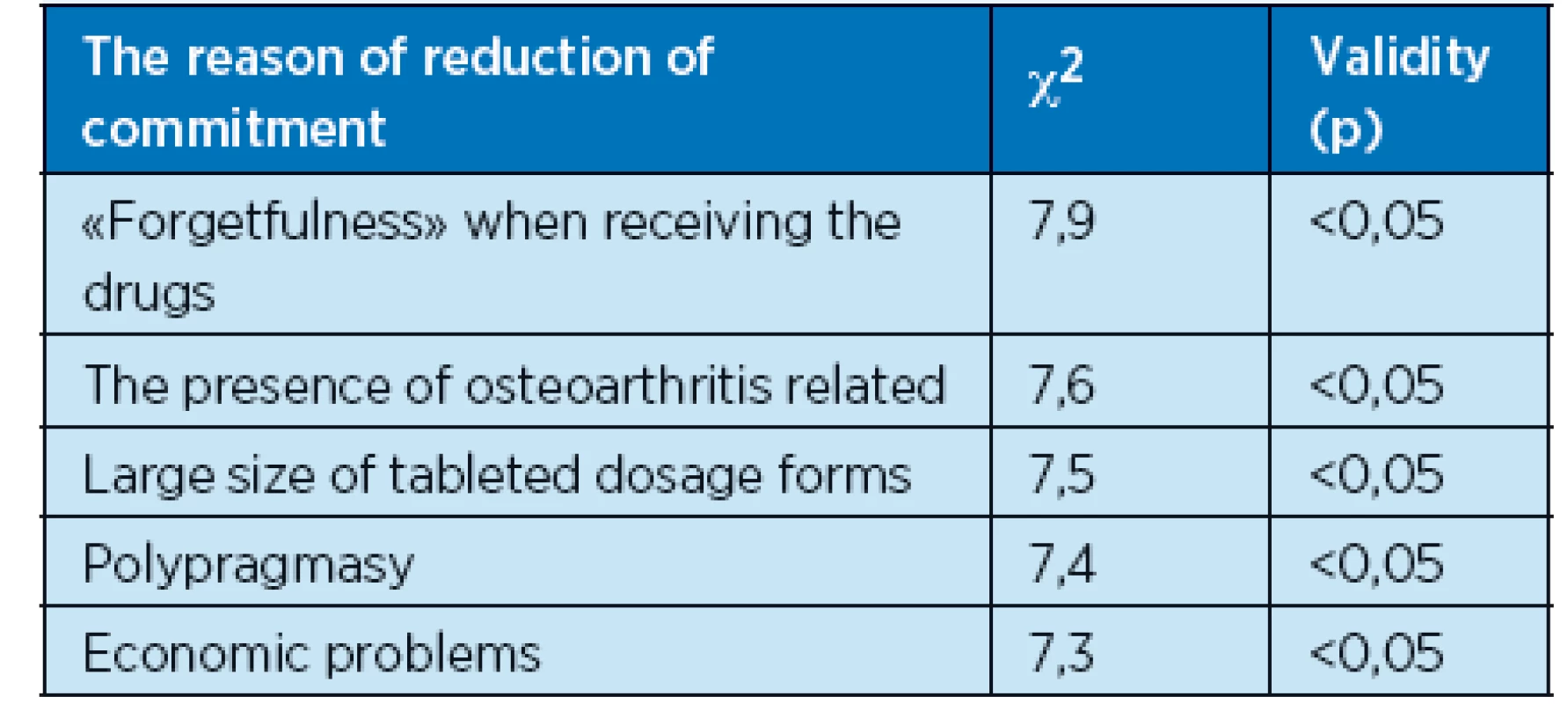
In rheumatoid arthritis is joint pain syndrome, χ2 = 8,2; «forgetfulness» by taking medicines, χ2= 8,0; violation of the functions of the musculoskeletal system and low, in this regard, the availability of pharmacies, χ2 = 7,9; fear for polypragmasia, χ2 = 7,7; the large size pills of medicinal forms, χ2 = 7,6, p<0,05. On the background of osteoarthritis fairly important were the factors such as joint pain syndrome and concomitant violation of thin motility of fingers brush, χ2 = 7,9; «forgetfulness» when receiving the drugs, χ2 = 7,8; fear of side effects, χ2 = 7,7; the causes of the economic plan, χ2 = 7,6; fear of the consequences for polypragmasia, χ2 = 7,4, p<0,05 (table. 3).
3. The main reasons for the decline in commitment of elderly patients to receiving drug therapy in osteoarthritis 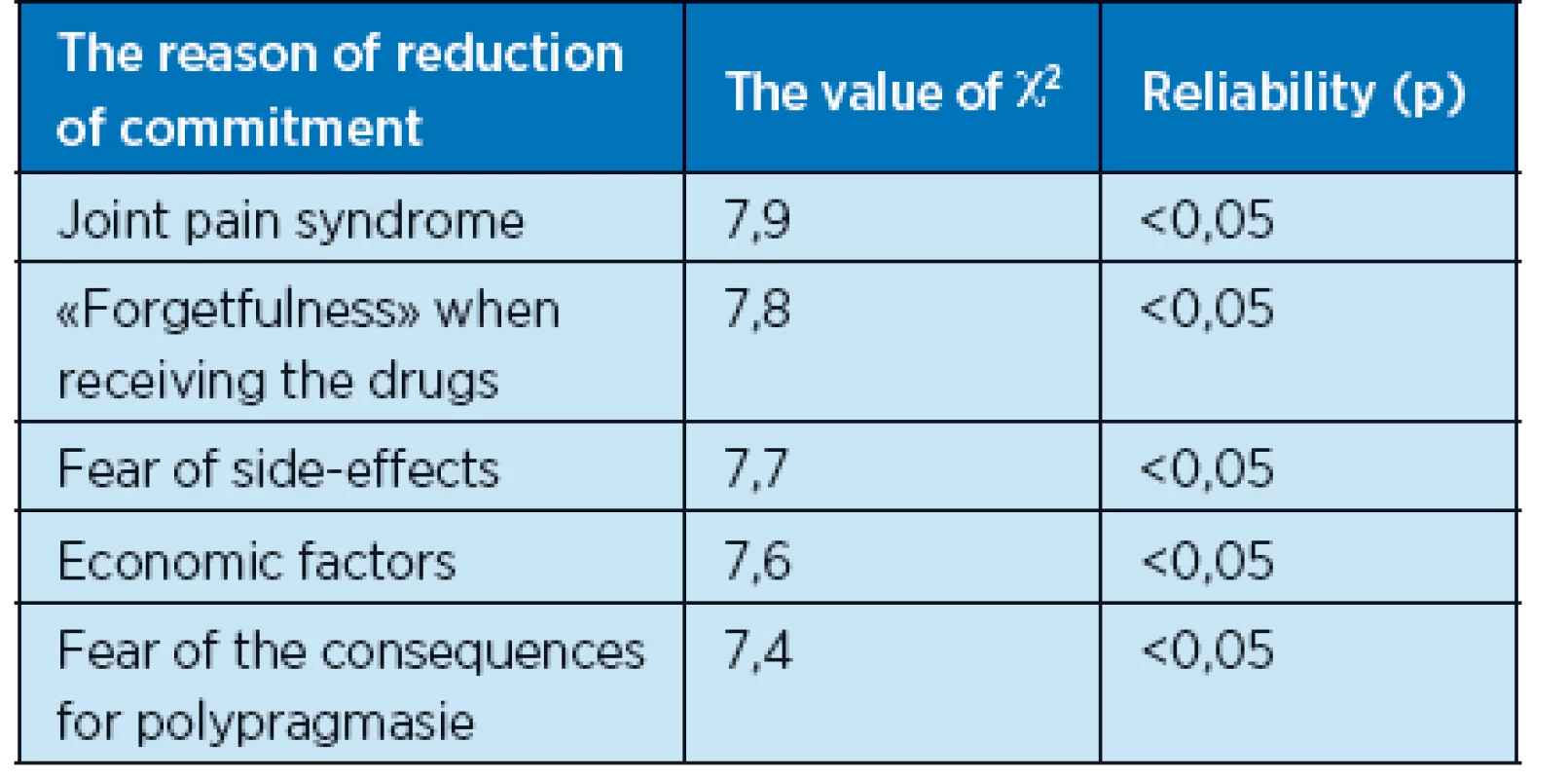
In diabetes causes of reduction commitment were «forgetfulness» by taking medicines on the background of different degrees of diabetic encephalopathy, χ2 = 8,1; large size of medications in the form of tablets, χ2 = 7,9; availability for polypragmasia, χ2 = 7,7; fear of side-effects-appointed medical treatment, χ2 = 7,5, p<0,05. In osteoporosis - «forgetfulness» by taking medicines, χ2 = 7,9; the fear of the side effects of medicines, χ2 = 7,7; painful articular syndrome, χ2 = 7,7; limitation of physical mobility and low, in this regard, the availability of pharmacies, χ2 = 7,6, p<0,05. In Alzheimer’s disease – «forgetfulness» by taking medicines, χ2 = 8,2; the difficulty of information about drug therapy, χ2 = 8,2; joint pain syndrome on the background of the accompanying osteoarthrosis, χ2 = 8,1; low availability of pharmacies and medicines, χ2 = 7,9, p<0,05. In other nosological forms of adherence to therapy was reduced to the following reasons: sensorineural hearing loss – forgetfulness» by taking medicines, χ2 = 8,1; joint pain syndrome, χ2 = 7,9; the large size and the volume of tableted dosage forms, χ2 = 7,7, p<0.05; chronic gastritis and non-alcoholic стеатогепатоз – «forgetfulness» by taking medicines, χ2 = 8,0; fear of side-effects of medication, χ2 = 7,9; the existence of economic problems in acquiring medicines, χ2 = 7,7, p<0.05; and benign hyperplasia of the prostate gland - «forgetfulness» by taking medicines, χ2 = 8,0; low availability of medicines in connection with a violation of the functions of the urinary system and musculoskeletal system, χ2 = 7,8, p<0.05; and miopia high degree of the «forgetfulness» by taking medicines, χ2 = 7,8; the fear of side effects, χ2 = 7,6; difficulties in establishing contacts with the patient, χ2 = 7,5, p<0,05.
Discussion
Reasons for the decline in commitment of older people to the therapy may be considered in groups, although, as has been shown in our study, one patient may have the position of the complex of diverse reasons.
Summing up their own data and literature data, the reasons for which the patient does not follow the prescribed treatment regimens, can be grouped as follows:
- Causes, associated with the patient. The presence at the patient of sensory – decrease in vision and/or hearing impairment can lead to the fact, that the patient does not receive the necessary information, when the doctor gives him oral or written instructions; cognitive disorders in the patient - information received by the patient of a doctor may be distorted, for example, if the patient’s dementia, depression, etc.; peculiarities of the course of disease.One of the psychological reasons for the low adherence to therapy may be the formation of adaptation to the existing symptoms or conditions, when the patient prefers to live with minor manifestations of the disease, than follow the appointed treatment. Reduction in the degree of adherence to treatment is especially pronounced in patients with asymptomatic course of the disease, as well as in situations where the effect of the medication does not occur at once (7).
- Social reasons. Patients living alone (often women), have less of a commitment to therapy.
- Reasons related to drugs. Commitment to increases in that case, if the course of treatment is short. Also the reduction of adherence to therapy is observed in the following cases: the patient has a chronic disease that forced him to take medicines constantly; polypragmasia; the complexity of schemes of treatment and the calculation of the dosage; cases, if the introduction of a product requires the presence of qualified staff; if the side effects of the drug (e.g., impotence) is causing the patient considerable inconvenience.
- Reasons that caused by the peculiarities of communication and interaction between the doctor and the patient. It is very important for the physician to be clearly explained to the elderly patient terms and stages of treatment. Prescriptions may not be fulfilled in full, if the patient does not have the opportunity to ask your doctor all questions of interest to him. Insufficient duration of the consultation can also lead to poor patient adherence to treatment. It should be remembered, that the complicated treatment regimens require more time to explain their patient, and don’t underestimate the importance of repeated consultations. Often issues in the administration of the drug to occur in patients only in the process of treatment.
Thus, the problem of commitment to ongoing drug therapy is a complex, multidimensional, it touches on the elderly patient, and the doctor, and also administration of the medication (8).
Practically all older people are characterized by some problems with health. The majority of older people (about 80 %) suffer from chronic diseases. Due to this, there is a high frequency of consumption of drugs among older people.
It is important to consider that these drugs are available in a different form, in the majority of cases, an elderly person or by reason of his illness, or because of absent assistance forget to take them, or does it not according to the schedule, confuses the pills, because sometimes he knows them only by their colour.
This describes a situation where older patients don’t know the name of tableted drugs, which they take, as well as in the moment of reception of various drugs elderly people with chronic diseases such as rheumatoid arthritis because of pain in the joints of the wrist can’t get the medicine out of the packaging. All this leads to the fact that older people or do not take drugs, because they forget, or are not able to get them out of the packaging, or are not able to follow a schedule.
Forms of products/problems
Upon reception of various forms of medicinal products may encounter the following problems:
Eye drops. Eye drops are one of the commonly prescribed forms of medicinal products. Reduction of commitment to their application is due to the fact that often older people themselves are not able to drop his eyes because of the pain in the joints, lack of skills, tremor of the hands and should almost always resort to the assistance of another person.
Tableted preparations with a large samples of active substance. Some drugs, such as vitamins, are issued by the large size, which makes it difficult to older people, their reception and they refuse them.
Liquid medicines. Drugs produced in bottles with the various types of caps, also cause a lot of problem in older people, as they sometimes tightly closed, and the old people can’t open them, when they need to take this medicine. Also, often because of poor eyesight, shake the hands of older people find it difficult to comply with the accuracy of dosing, especially the number of drops.
The injectable form. Injections are very well accepted by older people, because they really believe in their rapid effect, but many of them complain, because they cause too much pain and stress, so often prefer to interrupt treatment. In addition to the use of injections requires a dedicated staff, and the elderly are often difficult to themselves reach health centres or find someone who would do them an injection at home.
Creams and gels. The use of creams and gels are sometimes physical difficulties in the application of the patients of elderly age, especially when the lesion is small joints of hand, violations of the fine motor skills of Central Genesis.
Taking all this into account, it is necessary to look for ways to help older people in the moment of reception of medicines, and also establish a special system of reminders that will allow to comply with the admission of drugs, thus increasing the effectiveness of therapy and adherence to it.
Conclusions
- The elderly degree of commitment to drug therapy is 53.2 % and is significantly lower, than in middle aged patients, for whom this number is at 78.4 %. This allows us to consider old age as an independent factor of reduction of the level of commitment to the prescribed drug therapy.
- The most significant reasons for the decrease in the level of commitment to drug therapy among the elderly are factors such as fear of side-effects of therapy (in 3.6 % of cases), forgetfulness (33.3 %), the presence of the articular syndrome and other physical difficulties that hinder the taking of medicines (18.9 %), inconvenient size tablet forms (8.1 %), economic failure of patients (7,5 %), the need to receive a large amount of drugs (polypragmasia) (5.6 %), poor health literacy of the patient (1.8 %). These factors are significantly more frequent among elderly patients than among middle-aged patients.
- In old age, in addition to the age and age-related peculiarities of physical and mental status, there are independent factors behind decreased adherence to the prescribed drug therapy, such as the form of the drugs, prescribed by the doctor. The most common forms leading to decreased adherence among the elderly are eye drops, injectable forms of medicines, drugs supplied in vials and tablet forms of drugs.
- Development of measures aimed at increasing the commitment to the ongoing drug therapy in elderly and senile age should be based on the effects of the leading causes of reduction of adherence to therapy, represented by three groups: 1) those associated with the age of the patient (e.g., age-related decline in memory); 2) those associated with the presence another disease (for example, articular syndrome or other physical constraint on the normal reception of the medicinal product); 3) those associated with psychological characteristics of the elderly patient (for example, fear of side effects, the fear of receiving large quantities of drugs); 4) the socio-economic causes (economic insolvency, poor health literacy in the elderly patient).
Prashchayeu K1,
Pobeda Padilla AG2,
Ilnitski A3,
Pobeda Padilla VA2,
Fesenko E1,
Khadieva T1
1Open Institute of Human and Nature, Vilnius, Lithuania
2University of Santa-Elena, Santa-Elena, Ecuador
3Belarusian Association of Gerontology and Geriatrics, Vitebsk, Belarus
Sources
1. Young JB, Robinson M, Chell S, Sanderson D, et al. A whole system study of intermediate care services for older people. Age and Ageing 2005; 34(6): 577–583.
2. Bryant SL. The information needs and information seeking behaviour of family doctors. Health Information & Libraries Journal 2004; 21(2): 84–93.
3. Lichtenberg P, Heresco-Levy U. Nitzan U. The ethics of the placebo in clinical practice. Journal of Medical Ethics 2004; 30 : 551–554
4. Shine KI. Health care quality and how to achieve it. Acad Med 2002; 77 : 91–99.
5. Jing Jin, Grant Edward Sklar,Vernon Min Sen Oh, Shu Chuen Li: Factors affecting therapeutic compliance: A review from the patient’s perspective Ther Clin Risk Manag 2008; 4(1): 269–286.
6. Russell CL, Conn VS, Jantarakupt P: Older adult medication compliance. Am J Health Behav 2006; 30 : 636–650.
7. Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases. JAMA 2005; 294 : 716–724
8. Conn VS, Hafdahl AR, Cooper PS, et al. Interventions to improve medication adherence among older adults. Gerontologist 2009; 49 : 447–462.
Labels
Geriatrics General practitioner for adults Orthopaedic prosthetics
Article was published inGeriatrics and Gerontology

2015 Issue 4-
All articles in this issue
- Horečka jako častý symptom
- Průjmová onemocnění v ordinaci praktického lékaře
- Vředová choroba žaludku a dvanácterníku a infekce Helicobacter pylori u starší populace
- Zánětlivá onemocnění močových cest v geriatrické populaci
- Léčba nehojících se ran u geriatrických pacientů
- Cestování seniorů – prevence infekcí při cestách do exotických krajin
- Geriatrická péče jako impulz k zavedení nového konceptu prevence a kontroly infekcí
- Streptokokové a pneumokokové infekce z pohledu geriatra
-
Features of adherence to drug therapy elderly:the impact of the diseaseand form of the drug
(the results of research in the urban population of Ecuador)
- Geriatrics and Gerontology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Horečka jako častý symptom
- Průjmová onemocnění v ordinaci praktického lékaře
- Streptokokové a pneumokokové infekce z pohledu geriatra
- Léčba nehojících se ran u geriatrických pacientů
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

