-
Medical journals
- Career
ENHANCED RECOVERY PROTOCOL FOLLOWING AUTOLOGOUS FREE TISSUE BREAST RECONSTRUCTION
Authors: GH. Yim 1; C. Lewis 2; C. Oates 2; WJM. Holmes 3; E. Proussakaia 2; SM. Wilson 2
Authors‘ workplace: Department of Plastic Surgery, Royal Devon & Exeter Hospital, Wonford, Exeter, UK 1; Department of Plastic Surgery, Southmead Hospital, Bristol, UK 2; Department of Plastic Surgery, Pinderfields Hospital, Wakefield, UK 3
Published in: ACTA CHIRURGIAE PLASTICAE, 62, 1-2, 2020, pp. 10-16
INTRODUCTION
Enhanced Recovery after Surgery (ERAS) is also known as fast-track surgery. It is based around the concept of taking a multidisciplinary approach towards pre-operative optimisation, with standardised protocols to minimise peri-operative variation and achieve the highest quality of post-operative rehabilitation 1–3. ERAS was first pioneered in Denmark in the 1990s to optimize recovery after colorectal surgery 4–6. This has since rapidly developed into a world-wide concept that is used across a number of surgical specialties from colorectal, orthopaedics, urology, vascular surgery to gynaecology 7–10. Within the specialty of plastic surgery, free tissue breast reconstruction has emerged as an area where ERAS can be used to enhance the care and recovery of patients. The common objective endpoints used to demonstrate a successful ERAS pathway relate to: inpatient post-operative opioid use, morbidity and hospital length of stay (LOS) 1,11–13.
After an audit of LOS following free deep inferior epigastric perforator (DIEP) breast reconstruction at North Bristol National Health Service (NHS) trust in 2014, it was quantified that the mean LOS for patients following surgery was 7 days; LOS was determined as the number of days from hospital admission to discharge home. Whilst this was similar to the literature14, there were reports that ERAS principles were being implemented for breast reconstruction15. The senior author (SMV) felt that further improvements could be made and the local ERAS protocol for breast reconstruction was formally introduced in February 2015.
The aims of this study are to: 1) evaluate our ERAS experience in comparison to that of contemporary literature, 2) evaluate the LOS, number and proportion of patients discharged without prescription of opioids, major and minor complication rates, and readmission rates, 3) evaluate the feedback of patients who were rehabilitated on the ERAS protocol.
MATERIALS AND METHODS
Study design
A retrospective review of the, prospectively maintained, Bristol free breast reconstruction database for patients treated between January 2016 and December 2016 was undertaken. All consecutive patients were included for the analysis with no exclusions. All patients underwent immediate or delayed free DIEP reconstruction that was either unilateral or bilateral. Patients that had concurrent therapeutic or risk reducing mastectomies were also included in the analysis.
Enhanced Recovery Protocol
The North Bristol NHS Trust ERAS protocol was developed by a multidisciplinary team of anaesthetists, nursing staff, surgeons, physiotherapists and pharmacists. The protocol was implemented at Southmead Hospital in February 2015 to bring together the care provided across the different disciplines. Pre-operatively, patients were counselled of what to expect during their ERAS journey and they also met with post reconstruction free DIEP patients. The patients were expected to have a body mass index of 30kg/m2 or less but they also had preoperative abdominal exercise classes with the aim to strengthen their core musculature in an effort to reduce the post-operative abdominal weakness. Computed tomography angiography (CTA) was undertaken to characterize patients’ abdominal perforators; this also determined whether recurrent disease was present prior to surgery. The ERAS protocol standardised the care across multiple domains of nursing, surgical, physiotherapy, analgesia and nutritional care. Immediate post-operative analgesia was oxycodone administered through a patient-controlled analgesic device (PCA). This was stepped down to oral analgesia within the first 24 hours following surgery. Regular flap monitoring was undertaken half hourly and then reduced in frequency to every four hours as the risk of flap failure subsided. Intravenous fluids were used intraoperatively and continued overnight but stopped on day 1 post operatively to encourage resumption of normal oral intake. The urine output was monitored to ensure normovolaemia; aiming for 0.5–1ml/kg/hr. Anti-emetics were prescribed, according to the anaesthetist’s choice, to reduce opioid induced nausea and vomiting. Normal intake of food and fluids was commenced within 18 hours of surgery but also supplemented through the use of high energy and protein drinks. Sports bras were worn from the first post-operative day to support the reconstructed breasts. Mobilisation was actively encouraged day 2 post-operatively. Bowel movements and blood testing were also managed according to the ERAS protocol. When patients were ready, they were discharged to their own home. The protocol is attached in Table 1.
1. The Enhanced recovery after surgery (ERAS) protocol for breast reconstruction implemented in February 2015. ASAP – As soon as possible, Hb – Haemoglobin, hr – hour, IV – Intravenous, kg – kilogram, ml – millilitres, PCA – Patient controlled analgesia, TDS – Three times daily, TWOC – Trial without urinary catheter, U&E – Urea & electrolytes 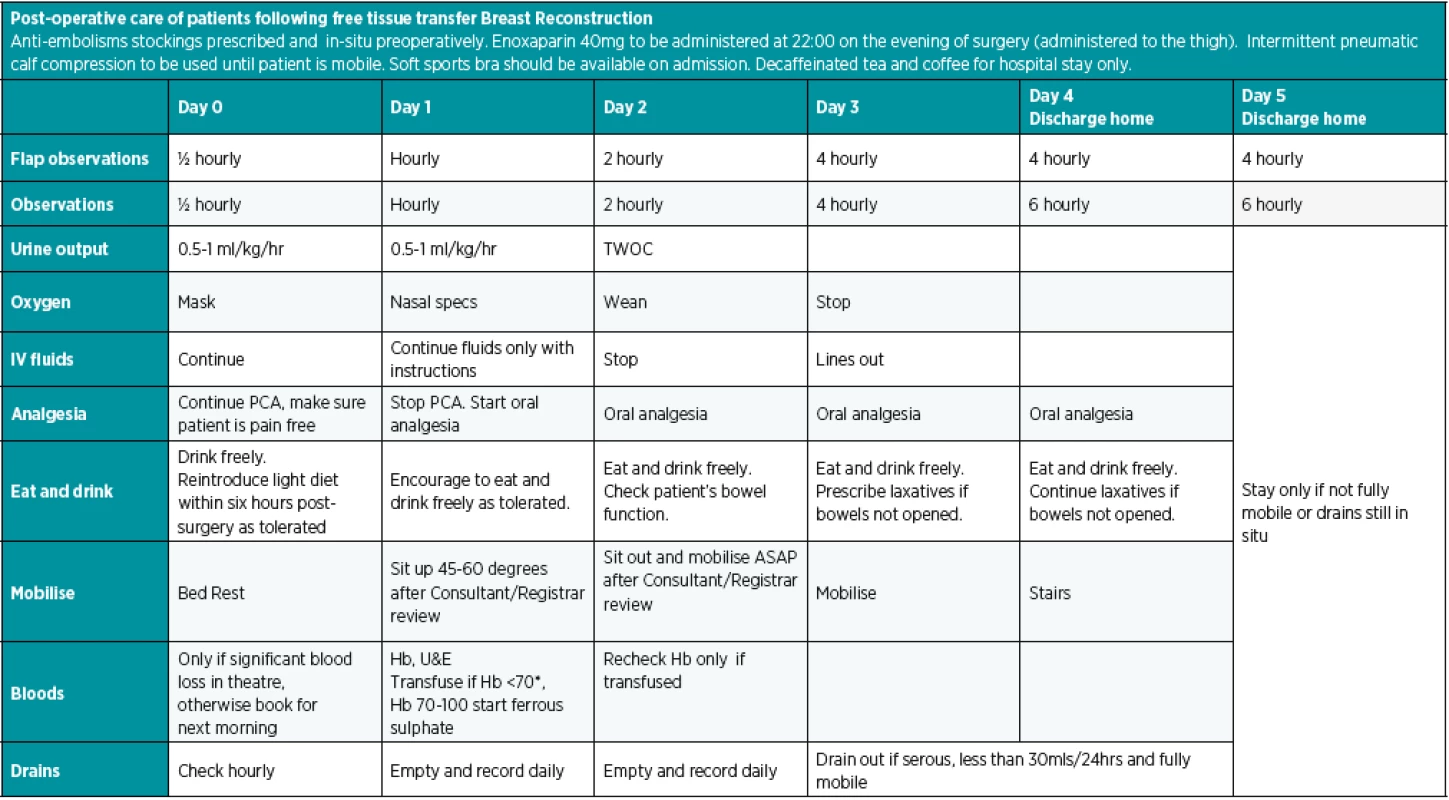
If Hb 70-100mg/dl, start ferrous sulphate 200mg three times daily for one month.
If Hb less than 70mg/dl, patient will need blood transfusion after discussion with consultant.The surgical technique
Surgery was undertaken at a single centre by two reconstructive breast surgeons (EP and SMW). All patients underwent preoperative assessment with a full blood count, renal and liver function tests. On the day of surgery, the breast, chest wall and the locations of DIEP perforators were marked pre-operatively using a hand-held Doppler with reference to the pre-operative CTA. At induction, intravenous flucloxacillin or teicoplanin and gentamicin (for patients who were penicillin allergic) were administered. The non-operative areas of the patient were kept warm with forced air warming to maintain their core body temperature above 36°C. Breast reconstruction was undertaken using tissue harvested from a free DIEP flap. The superficial epigastric venous system was also routinely prepared for emergency use in the event of venous congestion16. The recipient vessels were the internal mammary artery and vein, after resection of a portion of cartilage from the third rib 17. Both the artery and vein anastomoses were hand sewn end to end; no venous couplers were used. After DIEP inset, the remaining abdominal skin, fat, and fascia superficial to the external oblique were dissected to facilitate closure. A single-shot transverse abdominus plane (TAP) block was undertaken unguided for immediate post-operative analgesia. Sublay mesh (BARD Medical, Crawley United Kingdom) was inserted to reinforce the abdominal wall prior to closure of the abdomen in layers. Closed suction drains were placed, prior to completion of closure with one in the breast and two in the abdominal wall. The post-operative ERAS recovery protocol was then implemented on release from theatre until discharge home.
Post discharge questionnaire
A patient satisfaction questionnaire was developed for patients to assess the quality and their satisfaction with the ERAS service. Prior to ‘roll-out’ the questions were analysed by the North Bristol NHS trust research team to ensure that there was no bias in wording. Patients were all aware preoperatively that a questionnaire of their experience would be sent to them between 30 to 60 days following discharge. This was to ensure capture of any post-operative complications. Patients were then given between 90 to 120 days following discharge to return completed questionnaires. The questions were scored on the Likert scale of 0 – 10 with 0 representing the worst possible care and 10 representing the best possible care. The questions were:
1. At your pre-assessment appointment did the information given by the nurse practitioner prepare you for your stay in hospital?
2. What was your experience of the care you receive on the ward?
3. On the day of your discharge did you feel ready to go home?
Non-return of questionnaires was deemed as not wishing to participate in the survey. All data from the database and returned questionnaires were collated and analysed using Microsoft Excel (Microsoft Corporation, Redland, United States 2010).
RESULTS
A total of 70 patients underwent free DIEP reconstruction between January 2016 and December 2016. 28 patients underwent immediate reconstruction (40%) and 42 underwent delayed reconstruction (60%). Of these patients, three patients in the immediate group had bilateral risk reducing mastectomies with immediate reconstruction. Two patients in the delayed reconstruction group had previously undergone bilateral risk reducing mastectomies before deciding to have free DIEP reconstruction. 60 patients underwent unilateral free DIEP reconstruction (86%) and 10 patients underwent bilateral free DIEP reconstruction (14%); five of the bilateral reconstruction patients had risk reducing mastectomies. The mean and median ages at surgery were both 51 years (range of 23 to 71). No patients underwent any concurrent oophorectomies.
The mean LOS was 4.89 days with a median of 5 days (range 3–10 days). 61 patients (87%) were discharged within five days; 26 patients (37%) were discharged within 4 days. Nine patients (13%) were discharged after five days, with only two patients staying longer than seven days (3%). When the patients were stratified, the immediate group had a mean and median LOS of 5.21 and 5 days respectively; prolonged stays were due to abdominal haematoma, return to theatre and nausea/vomiting. The delayed group had a mean and median LOS of 4.67 and 4 days respectively; four patients had a prolonged stay due to nausea/vomiting, high drain output, pneumonia and postural hypotension. The unilateral group had a mean and median LOS of 4.93 and 5 days respectively. The bilateral group had a mean and median LOS of 5 days for both.
Sixty-five patients (93%) were discharged home on either: no medication, ‘over the counter’ analgesia or the patient’s own regular analgesia that they were taking preoperatively. Only six patients (8.5%) were discharged home on short a one-week course of paracetamol and the prescription opioid tramadol; three in the immediate group (11%) and three in the delayed group (7%). Of the patients that had a prolonged stay, none required prescription opioid on discharge.
Major complications were encountered in three patients (4%); two of the patients were from the immediate group and one was from the delayed group. Two patients returned to theatre for re-exploration of the DIEP flap; one each from the immediate and delayed groups. Of these two patients, one required a cephalic turndown for venous congestion and the other required the successful salvage of the arterial anastomosis. The third patient developed an abdominal haematoma requiring evacuation. There were no cases of complete or partial flap failure during the study period. One death occurred four months following discharge, due to acute progression of metastatic disease that was not detected at the time of the CT scan; this was not a complication of surgery or ERAS protocol.
Minor complications were encountered in five cases (7%); two within the immediate group (7%) and three within the delayed group (7%). Two patients (one each from the immediate and delayed groups) required blood transfusions. One patient, in the delayed group, developed a post-operative chest infection requiring a course of antibiotics. Two patients, one each from the immediate and delayed groups, had wound infections requiring treatment with antibiotics.
There were 69 questionnaires sent out; 1 questionnaire was not sent out due to death from disease progression. There were 34 returns, giving a 49% response rate. The results in Table 2 indicated that the responding patients were very satisfied with their care with mean and median scores greater than 9 out of 10 for all three domains.
2. The scores awarded by patients following their ERAS breast reconstruction. Q1 - At your pre-assessment appointment did the information given by the nurse practitioner prepare you for your stay in hospital? Q2 - What was your experience with the care you receive on the ward? Q3 - On the day of your discharge did you feel ready to go home? 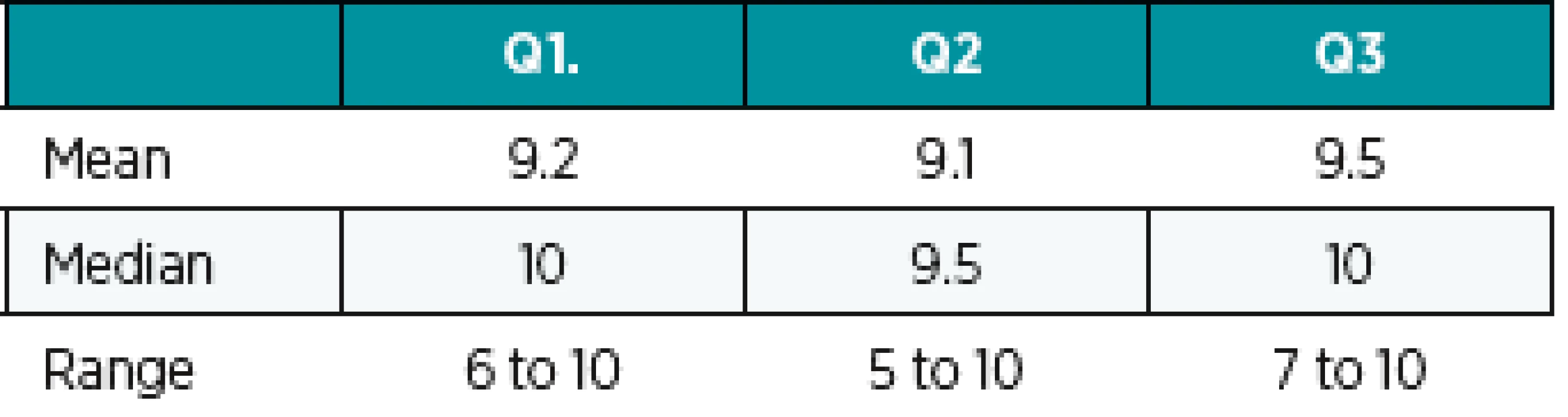
The patients were very satisfied with the preoperative counselling particularly the opportunities to meet other patients who underwent ERAS and also to undertake abdominal exercise classes. Patients were very satisfied with the quality of inpatient care but nausea, vomiting, and constipation were common problems. Comments relating to discharge included many positive comments of patients feeling ready to go home and discharge running like clockwork. However, one patient mentioned feeling inadequate when they did not reach ERAS milestones.
DISCUSSION
At the turn of the last decade, the LOS following free breast reconstruction for the majority of patients was reported to range around 7 days 14,18,19 and uptake of ERAS principles within the field of Plastic Surgery was previously felt to be slow1. Since then, there has been a rapid boom in the adoption of ERAS for breast reconstruction across a range of techniques including: implant based 20, pedicled flaps 12,15, and free autologous flaps 1,11,13,21–23. In 2014 we felt that our previously LOS was prolonged at seven days, this led to the implementation of our local ERAS protocol to successfully reduce the mean LOS to 4.89 days. This is broadly similar to other studies with a mean LOS ranging between 3.9–6.2 days 11,13,21,23 and our median LOS of 5 days is consistent with that of current UK practice24. Whilst we encountered two cases of unplanned return to theatre, for venous and arterial failure, there were no cases of partial or total flap failure. This is credit to the monitoring protocol and staff diligence in detecting and facilitating salvage of the free DIEP reconstructions. Our 2.8% rate of unplanned return to theatre were lower than other studies that had rates of between 5–10% 1,13,25. Flap failure was lower than other studies which had combined total and partial flap failure rates of between 2–5.8% 1,11,13,25. We had one case (1.4%) of haematoma at the abdominal donor site which was similar to the 1.4–2.2 % reported by others 11,25. Pneumonia was seen in one of our patients (1.4%) and this was also similar to Bonde et al 11. We had a low readmission rate with only one patient (1.4%) returning to their local hospital for treatment, this is at the lower end of the range compared to other studies that had a 2–14% readmission rate 1,13. The low rates of complications confirm the safety of our surgical and ERAS protocol.
As pain is a predictor of the quality of post-operative recovery and patient satisfaction 26, the low rates of our patients requiring prescription opioid analgesia on discharge (7%) reinforce the benefits of successful ERAS implementation. Analgesia on discharge is possibly a good marker of whether patients are ready for discharge. The effects of successful ERAS implementation have been reported to continue into the outpatient setting with lower median total opioid use and potentially reducing opioid misuse30. Particularly as evidence indicates that patients discharged with prescription opioids were more likely to become long term users compared to those with no opioid prescriptions 27–29
Our mailed questionnaire response rates of 49% was considered adequate 31 and the responses communicated very good overall satisfaction of care. Whilst the questionnaires raised many positive comments, they also highlighted improvements that could be made to our ERAS protocol. The common theme raised was the issue of early postoperative opioid induced nausea and vomiting. On comparison of our protocol to those with shorter lengths of stay, the key contributing factor is likely our ongoing use of PCA compared the omission of PCA usage in other studies11,23,32. Some have felt that opioid use delays recovery and is a major obstacle to early discharge32, this is an aspect that we will seek to address in future refinements of our protocol; though we are mindful that PCA usage is established in the UK with 63% of anaesthetists prescribing PCA for free autologous breast reconstruction24. The Transversus Abdominis Plane (TAP) block has been used to augment the multi-modal analgesia of patients with reports of lower morphine usage, less nausea & vomiting and thus a shorter LOS18,23,32. Some authors have used liposomal bupivacaine1,32, due to the reported prolonged release over 96 hours and benefits up to 72 hours post-operatively32. Though the clinical effects of non-liposomal bupivacaine have been felt to be equivalent to liposomal bupivacaine 23; particularly if administered with dexamethasone22. Despite numerous reports, a Cochrane library systematic review indicated that there was limited evidence that use of perioperative TAP block reduces opioid consumption and pain scores after abdominal surgery compared with no intervention or placebo33. Within the setting of nausea, vomiting and sedation there was insufficient evidence that TAP blocks led to a difference34; we also did not observe such effects following our TAP blocks.
The rapid uptake of ERAS principles has led to a wealth of studies that are highly variable in their parameters leading many to question whether the parameters are based on evidence or expert opinion 23,24. Whilst the co-authors of Astanehe were involved in drafting the evidence based ERAS society recommendations, it is worth noting that even they were not able to fully apply all aspects of the ERAS society recommendations; meeting 11 out of the 18 criteria 23,35; we managed to meet 10 of the criteria. A recent survey of UK breast reconstruction practice has also demonstrated wide variability in clinical practice across hospitals and even within hospitals24. Part of the reason behind the clinical variability may arise from conflicting evidence within the literature. For general anaesthesia, total intravenous anaesthesia has been recommended but others have recommended sevoflurane as it may have protective effects on the endothelium and vasculature24,35,36. Another aspect, that has been exemplified earlier by TAP blocks, is the absence of high-quality evidence24. The majority of the ERAS society recommendations were based on moderate evidence with only three aspects (body mass index <30, multi-modal analgesia and direct closure using sutures) being based on high quality evidence35. Another aspect of the variance is related to the compliance and whether outcomes are actually attributable to ERAS9, from the literature only three studies quantified compliance rates25,30,37. Redwood et al saw overall compliance rates of 57%37. Sharif-Askey et al saw the highest compliance with the pre - and intra-operative aspects: at 94% for pre-operative counselling, 90% for operative carbohydrate drink, 100% and 99% for pre-and intra-operative pain management respectively. Post-operatively this fell dramatically down to 44% for cessation of intravenous fluids and 68% for starting early oral fluid intake; though post-operative compliance of less than 50% is not uncommon 38–40. Rendon et al also reported high compliance rates of 93% pre-op, 91% intra-op, 96% post-op but it was unclear if partial fulfilment of the parameters counted as ‘compliance’30.
The barriers to ERAS implementation are multi-faceted, as ERAS is multi-disciplinary it requires engagement from all team members to fulfil all aspects from pre-admission through to post-discharge care38. Whilst deviation by patient or surgeon preference only contributed to 2% of non-compliance for Redwood et al, 10% of the non-compliance were from errors in ordering or executing the pathway. Resistance or dis-engagement with ERAS parameters needs to be settled before implementation, with all members of the team educated in its application to ensure a positive culture exists to facilitate ERAS implementation 38,41. Recent work by Pearsall et al distilled common enablers such as open communication, changing nursing culture, maintaining the ERAS protocol through continuing education of patients, new staff and existing staff 41. As ERAS protocols become embedded within the culture of the hospital, we can better asses their true effects once an acceptable level compliance becomes the norm.
As we all strive to further optimise our ERAS protocols and achieve ever shorter LOS, is there a limit to what can be achieved? Once the analgesic, mobilisation, dietary and drain factors are accounted for, the remaining critical aspect is monitoring of the free flap. We monitor flaps with decreasing frequency until discharge, but some authors argue that the monitoring can be much shortened. For Astanehe et al and Carruthers et al, all cases of microvascular problems were encountered within the first 24hrs23,42 and Bonde et al stopped flap monitoring after 48hrs11. A limited cohort of free autologous reconstructions have been discharged within 23 hours of admission by Martinez et al 43. Whilst Martinez et al previously encountered late vascular compromise after three days, they instituted changes such as anticoagulation and elective anastomosis of the superficial epigastric venous system to ensure robust reconstructions43. We recognise our study limitations such as the retrospective nature and absence of a pre-ERAs group to compare outcomes and the uncertainty of compliance rates. Despite this, we feel that the best comparison is against current literature. Our study has highlighted multiple areas to critically self-appraise and optimise particularly in the area of multi-modal analgesia and nausea. These themes are relevant to all clinicians involved in free autologous breast reconstruction and we are optimistic that future research can address the issues of underpowered studies to unify the variation that exists across ERAS protocols.
CONCLUSION
Our ERAS protocol for autologous free tissue breast reconstruction has seen lower complication rates, shorter lengths of stay and low rates of opioid analgesics prescribed at discharge. ERAS is being embraced globally and there are many who continue to push the possibilities of what can be achieved. However, we have seen that there is still a need to develop a stronger evidence base to support our practices. This is in parallel with ongoing education and audit cycles to foster a culture of ERAS that can safely optimise patient outcomes.
Conflicts of interest: The authors report no conflicts of interest.
Funding source: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval: Ethical approval was not required following the use of the Health Research Authority decision tool. The procedures used, comply with the principles of the Helsinki Declaration.
Corresponding author:
Guang Hua Yim, MD
Department of Plastic Surgery, Royal Devon & Exeter Hospital, Barrack Road, Wonford, Exeter EX2 5DW, UK
E-mail: gyim@doctors.net.uk
Sources
1. Afonso A., Oskar S., Tan KS, et al. Is Enhanced Recovery the New Standard of Care in Microsurgical Breast Reconstruction? Plastic and Reconstructive Surgery. 2017, 139 : 1053–61.
2. Ljungqvist O., Scott M., Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surgery. 2017, 152 : 292–8.
3. Gnaneswaran N., Perera M., Perera N., Peters M. Enhanced recovery after surgery (ERAS) pathways in autologous breast reconstruction: a systematic review. European Journal of Plastic Surgery. 2016, 39 : 165–72.
4. Fawcett WJ., Mythen MG., Scott MJP. I. Enhanced recovery: more than just reducing length of stay? British Journal of Anaesthesia. 2012, 109 : 671–4.
5. Carlson RH. ERAS Protocol Now Shown Helpful in Breast Reconstructive Surgery: Oncology Times. 2015, 37 : 14.
6. Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997, 78 : 606–17.
7. Paton F., Chambers D., Wilson P. et al. Effectiveness and implementation of enhanced recovery after surgery programmes: a rapid evidence synthesis. BMJ Open. 2014, 4 : 5015.
8. Kalogera E., Bakkum-Gamez JN., Jankowski CJ. et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013, 122 : 319–28.
9. Spanjersberg WR., Reurings J., Keus F., van Laarhoven CJ. Fast track surgery versus conventional recovery strategies for colorectal surgery. In: The Cochrane Collaboration, ed. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2011.
10. Tatsuishi W., Kohri T., Kodera K. et al. Usefulness of an enhanced recovery after surgery protocol for perioperative management following open repair of an abdominal aortic aneurysm. Surgery Today. 2012, 42 : 1195–1200.
11. Bonde C., Khorasani H., Eriksen K., Wolthers M., Kehlet H., Elberg J. Introducing the fast track surgery principles can reduce length of stay after autologous breast reconstruction using free flaps: A case control study. Journal of Plastic Surgery and Hand Surgery. 2015, 49 : 367–71.
12. Davidge K., Armstrong KA., Brown M. et al. Shifting Autologous Breast Reconstruction into an Ambulatory Setting: Patient-Reported Quality of Recovery. Plastic and Reconstructive Surgery. 2015, 136 : 657–65.
13. Batdorf NJ., Lemaine V., Lovely JK. et al. Enhanced recovery after surgery in microvascular breast reconstruction. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2015, 68 : 395–402.
14. Drazan L., Vesely J., Hyza P. et al. Bilateral breast reconstruction with DIEP flaps: 4 years’ experience. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2008, 61 : 1309–15.
15. Davidge KM., Brown M., Morgan P., Semple JL. Processes of Care in Autogenous Breast Reconstruction with Pedicled TRAM Flaps: Expediting Postoperative Discharge in an Ambulatory Setting. Plastic and Reconstructive Surgery. 2013, 132 : 339–44.
16. Davies AJ., O’Neill JK., Wilson SM. The superficial outside-flap shunt (SOS) technique for free deep inferior epigastric perforator flap salvage. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2014, 67 : 1094–7.
17. Dickson JK., Varey AHR., Wilson S. Preparation of the internal mammary vessels as recipients for free flap breast reconstruction. Ann R Coll Surg Engl. 2015, 97 : 318.
18. Wheble GAC., Tan EKH., Turner M., Durrant CAT., Heppell S. Surgeon-administered, intra-operative transversus abdominis plane block in autologous breast reconstruction: a UK hospital experience. J Plast Reconstr Aesthet Surg. 2013, 66 : 1665–70.
19. Spear SL., Newman MK., Bedford MS., Schwartz KA., Cohen M., Schwartz JS. A retrospective analysis of outcomes using three common methods for immediate breast reconstruction. Plast Reconstr Surg. 2008, 122 : 340–7.
20. Dumestre DO., Webb CE., Temple-Oberle C. Improved Recovery Experience Achieved for Women Undergoing Implant-Based Breast Reconstruction Using an Enhanced Recovery after Surgery Model: Plastic and Reconstructive Surgery. 2017, 139 : 550–9.
21. Rochlin DH, Leon DS, Yu C, Long C, Nazerali R, Lee GK. The Power of Patient Norms: Postoperative Pathway Associated With Shorter Hospital Stay After Free Autologous Breast Reconstruction. Annals of Plastic Surgery. 2019;82:S320–4.
22. Kaoutzanis C, Ganesh Kumar N, O’Neill D, et al. Enhanced Recovery Pathway in Microvascular Autologous Tissue-Based Breast Reconstruction: Should It Become the Standard of Care? Plastic and Reconstructive Surgery. 2018, 141(4):841–851.
23. Astanehe A., Temple-Oberle C., Nielsen M. et al. An Enhanced Recovery after Surgery Pathway for Microvascular Breast Reconstruction Is Safe and Effective: Plastic and Reconstructive Surgery – Global Open. 2018, 6 : 1634.
24. Gardiner MD., Giblin V., Highton D. et al. Variation in the perioperative care of women undergoing abdominal-based microvascular breast reconstruction in the United Kingdom (The optiFLAPP Study). Journal of Plastic, Reconstructive & Aesthetic Surgery. 2019, 72 : 35–42.
25. Sharif-Askary B., Hompe E., Broadwater G., Anolik R., Hollenbeck ST. The Effect of Enhanced Recovery after Surgery Pathway Implementation on Abdominal-Based Microvascular Breast Reconstruction. Journal of Surgical Research. 2019, 242 : 276–85.
26. Joshi GP., Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North America. 2005, 23 : 21–36.
27. Alam A., Long-term Analgesic Use After Low-Risk Surgery: A Retrospective Cohort Study. Archives of Internal Medicine.2012, 172 : 425–30.
28. Calcaterra SL., Yamashita TE., Min SJ., Keniston A., Frank JW., Binswanger IA. Opioid Prescribing at Hospital Discharge Contributes to Chronic Opioid Use. Journal of General Internal Medicine. 2016, 31 : 478–85.
29. Clarke H., Soneji N., Ko DT., Yun L., Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014, 348 : 1251.
30. Rendon JL., Hodson T., Skoracki RJ., Humeidan M., Chao AH. Enhanced Recovery After Surgery Protocols Decrease Outpatient Opioid Use in Patients Undergoing Abdominally Based Microsurgical Breast Reconstruction. Plastic and Reconstructive Surgery. December 2019; doi: 10.1097/PRS.0000000000006546.
31. Fincham JE. Response rates and responsiveness for surveys, standards, and the Journal. Am J Pharm Educ. 2008, 72 : 43.
32. Jablonka EM., Lamelas AM., Kim JN., et al. Transversus Abdominis Plane Blocks with Single-Dose Liposomal Bupivacaine in Conjunction with a Nonnarcotic Pain Regimen Help Reduce Length of Stay following Abdominally Based Microsurgical Breast Reconstruction: Plastic and Reconstructive Surgery. 2017, 140 : 240–51.
33. Charlton S., Cyna AM., Middleton P., Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Pain, Palliative and Supportive Care Group, ed. Cochrane Database of Systematic Reviews. 2010 Dec 8;(12):CD007705. doi: 10.1002/14651858.CD007705.pub2.
34. Bhat S. In patients requiring analgesia after abdominal surgery, how does adding perioperative transversus abdominis plane (TAP) blocks to standard postoperative analgesia affect outcomes? Cochrane Clinical Answers. September 2016.
35. Temple-Oberle C., Shea-Budgell MA., Tan M. et al. Consensus Review of Optimal Perioperative Care in Breast Reconstruction: Enhanced Recovery after Surgery (ERAS) Society Recommendations. Plastic and Reconstructive Surgery. 2017, 139 : 1056–71.
36. Motakef S., Mountziaris PM., Ismail IK., Agag RL., Patel A. Emerging Paradigms in Perioperative Management for Microsurgical Free Tissue Transfer: Review of the Literature and Evidence-Based Guidelines. Plastic and Reconstructive Surgery. 2015, 135 : 290–9.
37. Redwood JN., Matkin AE., Temple-Oberle CF. Adoption of Enhanced Recovery after Surgery Protocols in Breast Reconstruction in Alberta Is High before a Formal Program Implementation: Plastic and Reconstructive Surgery – Global Open. 2019, 7 : 2249.
38. Kahokehr A., Sammour T., Zargar-Shoshtari K., Thompson L., Hill AG. Implementation of ERAS and how to overcome the barriers. International Journal of Surgery. 2009, 7 : 16–9.
39. Polle SW., Wind J., Fuhring JW., Hofland J., Gouma DJ., Bemelman WA. Implementation of a fast-track perioperative care program: what are the difficulties? Dig Surg. 2007, 24 : 441–9.
40. Maessen J., Dejong CH., Hausel J. et al. A protocol is not enough to implement an enhanced recovery programme for colorectal resection. Br J Surg. 2007, 94 : 224–31.
41. Pearsall EA., Meghji Z., Pitzul KB. et al. A Qualitative Study to Understand the Barriers and Enablers in Implementing an Enhanced Recovery After Surgery Program: Annals of Surgery. 2015, 261 : 92–6.
42. Carruthers KH., Tiwari P., Yoshida S., Kocak E. Inpatient Flap Monitoring after Deep Inferior Epigastric Artery Perforator Flap Breast Reconstruction: How Long Is Long Enough? Journal of Reconstructive Microsurgery. 2019, 35 : 682–7.
43. Martinez CA., Reis SM., Rednam R., Boutros SG. The Outpatient DIEP: Safety and Viability following a Modified Recovery Protocol. Plastic and Reconstructive Surgery – Global Open. 2018, 6 : 1898.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2020 Issue 1-2-
All articles in this issue
- AN OVERVIEW AND OUR APPROACH IN THE TREATMENT OF MALIGNANT CUTANEOUS TUMOURS OF THE HAND
- ENHANCED RECOVERY PROTOCOL FOLLOWING AUTOLOGOUS FREE TISSUE BREAST RECONSTRUCTION
- SKIN SUBSTITUTES IN RECONSTRUCTION SURGERY: THE PRESENT AND FUTURE PERSPECTIVES
- GUNSHOT INJURIES OF THE OROFACIAL REGION
- INDICATION AND IMPORTANCE OF RECONSTRUCTIVE SURGERIES OF FACIAL SKELETON IN MAXILLOFACIAL SURGERY: REVIEW
- Editorial
- CURRENT OPTIONS IN PHARMACOLOGICAL INTERVENTIONS FOR MICROVASCULAR ANASTOMOSIS PATENCY: REVIEW
- ACCIDENTAL FINDING OF SYNCHRONOUS BILATERAL DUCTAL CARCINOMA IN SITU IN A YOUNG MAN REFERRED TO MASTECTOMY DUE TO GYNECOMASTIA – AND WHAT IF LIPOSUCTION HAVE BEEN USED? CASE REPORT
- RED BREAST SYNDROME (RBS) ASSOCIATED TO THE USE OF POLYGLYCOLIC MESH IN BREAST RECONSTRUCTION: A CASE REPORT
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- RED BREAST SYNDROME (RBS) ASSOCIATED TO THE USE OF POLYGLYCOLIC MESH IN BREAST RECONSTRUCTION: A CASE REPORT
- AN OVERVIEW AND OUR APPROACH IN THE TREATMENT OF MALIGNANT CUTANEOUS TUMOURS OF THE HAND
- GUNSHOT INJURIES OF THE OROFACIAL REGION
- SKIN SUBSTITUTES IN RECONSTRUCTION SURGERY: THE PRESENT AND FUTURE PERSPECTIVES
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

