-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaFROM WHITE BOARD TO PATIENT TRACKING SYSTEM IN ANESTHESIA AND BEYOND
Authors: Jan Bruthans 1,2
Authors place of work: Department of Biomedical Technology, Faculty of Biomedical Engineering, Czech Technical University in Prague, Czech Republic 1; Department of Anesthesiology and Intensive Care, First Faculty of Medicine, Charles University in Prague, Czech Republic 2
Published in the journal: Lékař a technika - Clinician and Technology No. 3, 2018, 48, 91-95
Category: Original research
Summary
Every acute-care hospital in the Czech Republic is equipped with a Hospital information system, still there is no Anesthesia information management system (AIMS) deployed in any of these hospitals. Relaying the information obtained in anesthesia consultation and managing an anesthesia sub-department proved to be challenging when using a shared Word document and classic white board to keep track of the changing situation. We designed an in-house web-based system that stores the data obtained in anesthesia consultation, shares these data via email with relevant parties and then serves as a patient tracking system in the post-operative care unit. This system also provides statistical data associated with anesthesia required by our hospital. Although AIMS would be an ultimate solution for our needs, we were able to cover our most pressing needs by much more simple arrangement which we plan to develop further.
Keywords:
Anesthesia management information system, Patient tracking system, Hospital information system
Introduction
Computer technologies are being introduced in the Czech hospitals for more than twenty-five years. Every acute-care hospital in the Czech Republic is currently equipped with Hospital information system (HIS) [1]. However, the present HIS have only basic function-alities, as tracking patients from the point of arrival at hospital until leaving the hospital (admission-discharge-transfer systems, ADT [2]), keeping unstructured clini-cal data (clinical information systems), billing health-care payers, etc. Up to my knowledge, there is no deployment of wide-scale advanced HIS covering intensive-care or anesthesia care in the Czech Republic at present.
Specifics of anesthesia consultation
An integral part of anesthesia is the anesthesia consultation (also known as pre-anesthesia checkup). The anesthesiologist is expected to personally visit the patient, check his health status (with specific attention to previous anesthesia history and complications) and agree on preferred type of anesthesia. The anesthesio-logist not only decides on necessary provisions in the operating room (types of monitoring and invasive measures used, warming of the patient, units of blood reserved), but also plans type of post-operative treatment (standard ward via post-operative care unit, intensive-care unit, resuscitation-care unit, etc.). A rec-ommended course of anesthesia consultation is in effect in the Czech Republic [3].
Ideally the anesthesiologist administering anesthesia would be the one conducting the anesthesia consultation the day before the operation. However, this provider is usually committed elsewhere when the consultation is conducted, so another anesthesiologist must execute the consultation and then relay the information to the rele-vant person.
Specifics of surgery department
First Surgery Department of General Teaching Hospi-tal and First Faculty of Medicine provides abdominal, thoracic and trauma surgery. Four operation groups cover five operating rooms (OR) on daily basis. About fifteen to twenty operations are daily performed, up to twenty percent of them are unscheduled (inserting these unscheduled cases into the operating plan (OP) might take place the day before, in the morning of the opera-tion or even on a short notice, as in case of admission with severe bleeding).
Anesthesia sub-department (part of a Department of Anesthesiology and Intensive Care, author of this study is a deputy head of this sub-department) provides the daily service of four anesthesiology teams (physician and nurse), post-operative care unit team (PACU, two nurses), consultant anesthesiologist (present on OR or PACU) and acting head anesthesiologist (AHA, respon-sible for organization and providing of cardiopulmonary resuscitation). AHA also conducts the most of anesthe-sia consultations, the other anesthesiologists take part if their OP terminates earlier.
Changes in OP (inserting a case in OP, shifting a case from one OR to another, reordering cases, dropping a case) are prompted not only by an unscheduled case but also because of other reasons (longer operation than anticipated, unavailability of surgical tools or person-nel). The decision to change OP might come from different sources (head of surgery, head of OR nurses, surgery consultants, etc.), so AHA should be able to retain a clear picture of actual state in every working OR and should be able to assist the decision how the OP is changed to minimize the impact on the OP as whole.
Traditional way of coping with requirements
To retain and share the information gathered in anesthesia consultations AHA created every day a Word document which he sent by an email before the end of working hours to a predefined set of addresses (other anesthesiologists, nurses, OR nurses, etc.). If another anesthesiologist took part in the anesthesia consulta-tions, he usually took notes on a paper and provided these to the AHA to enter them in the document.
Based on this document, the PACU nurse created in the morning an OP depiction on a white board in the PACU. On this board changes in OP were shown, either by arrows or rewrites. Finished cases were erased, so a blank board meant a finished OP (a welcome sign for an anesthesiologist taking over a night shift!).
Each anesthesia case was recorded into an anesthesia book, entries about patient data, type of anesthesia, drugs used, etc. were created manually. Only severe complications of anesthesia were reported via standard hospital reporting system, whereas “mild” complica-tions (prolonged awakening, difficult airway, etc.) were usually not reported at all.
Required statistical data (number of patients under-going anesthesia, types of anesthesia, etc.) were gathered form the anesthesia book monthly either by an author of this study or by someone he had chosen (usually as a form of punishment). There was no second-ary control of these obtained data, so their value was – to say the least – questionable.
IT equipment present
The General Teaching Hospital is equipped with an outdated Stapro Medea HIS. Data are stored in non-structured way (as text entries). The surgeon must create an operation protocol, there is no required entry from the anesthesiologist (although he might enter a short notice – typically mentioning the difficult airway information for future use). A scheduling system exists in Stapro Medea, but OP is created by the head of surgery using an Excel file (which is sent at the end of previous week to all relevant parties).
No data can be inserted in our HIS originating in another system, also it is quite difficult to extract data from our HIS. At least an adjacent ADT can provide basic patient information (name, surname, health insur-ance company), if birth certificate number (a basic Czech patient identifier) is provided.
Our hospital is equipped with LDAP server and with MS Outlook with remote access (with short message service authentication). Also, Wi-Fi access is nowadays available virtually in every place in the hospital.
OR and PACU throughout the hospital are equipped with touch-screen personal computers (introduced when a simple surgery tracking system was bought few years ago, but this system is not used much at present).
Introducing own proprietary system
Anesthesia information management system (AIMS) would be a logical and fulfilling solution to our needs, but as Stapro Medea does not contain any such functions and because of the budget constrains we decided to opt for much more modest solution.
Head of anesthesia sub-department with author of this article provided an overview of most needed functions, a resident anesthesiologist with experience in web-application design provided the actual programming work, partly during his working hours, partly in his free time.
IT department of our hospital approved server/com-puting time usage, as well as LDAP server usage and assisted with ADT usage.
During the development process, other anesthesio-logists and anesthesia nurses were consulted and their relevant remarks were taken into consideration. The whole development process took about half a year, after a monthly trial the system was pronounced as usable.
Functions of the system
The resulting system works as a web-based applica-tion, available from any web-browser from any computer (or tablet / mobile phone) connected via the hospital ethernet (also via the Wi-Fi, the tablet / mobile phone must be registered to be able to connect).
Every anesthesiologist or anesthesia nurse can log in the system using his / her hospital password (via the LDAP server that also decides whether the person belongs to the anesthesia branch).
The system depicts each day of the OP and is structured into each OR. The primary data (name and diagnosis of the patient, sequence of the patients, name of the anesthesiologist) must be entered manually by the AHA using the above-mentioned Excel file from the surgeons.
At the anesthesia consultation, the birth certificate number is entered and the verified name from the ADT is filled in. Also, at this moment, previously stored data (from previous anesthesia, as quite a lot of our patients undergo more procedures in due time) are depicted. Then adjacent diseases, allergies, ASA-score, planned type of anesthesia (including catheters, transfusions, etc.) is entered – either using predefined texts or by entering unstructured data. Also, the placement informa-tion should be entered at this stage. (See Fig. 1 for better understanding).
Fig. 1. Anesthesia consultation entry 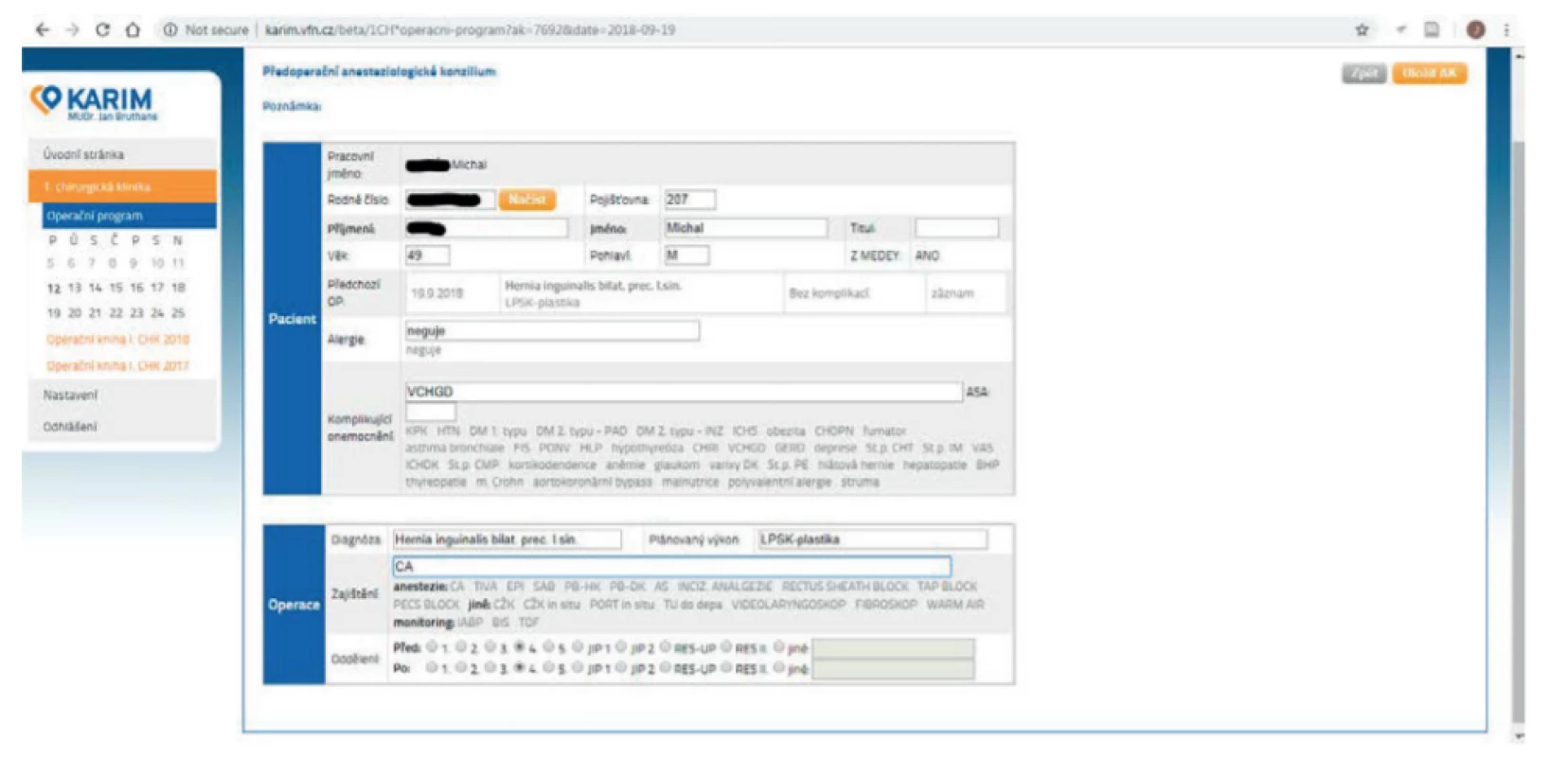
The whole OP for the next day with all anesthesia-relevant information is sent the previous day precisely at 7 : 00 PM to a predefined set of addresses – to all consultant anesthesiologists and head anesthesia nurse of the sub-department, to the OR head nurse of the surgery and then to all other anesthesiologists which are entered as caregivers on any OR for the next day. So, the information is limited for those needing it. Also, birth certificate numbers are omitted for privacy reasons.
The OP of the actual day exists in two variations – a full version with all the data (to be opened in a computer or a tablet by an anesthesiologist if needed) and a limited version that is shown on the touch-screen PC in PACU unit (some data are omitted again for privacy reasons). This touch-screen is then used instead the white board – by tapping next to the patient name, a position status is assigned (icons show - on the PACU before the operation / on the OR / on the PACU after the operation and the grayed entry means the patient has left the anesthesia care – see Fig. 2). Another patient can be inserted in the system using similar approach, also patients can be reorganized in any necessary way (also shifted to another day or left unassigned).
Fig. 2. Patient tracking system. 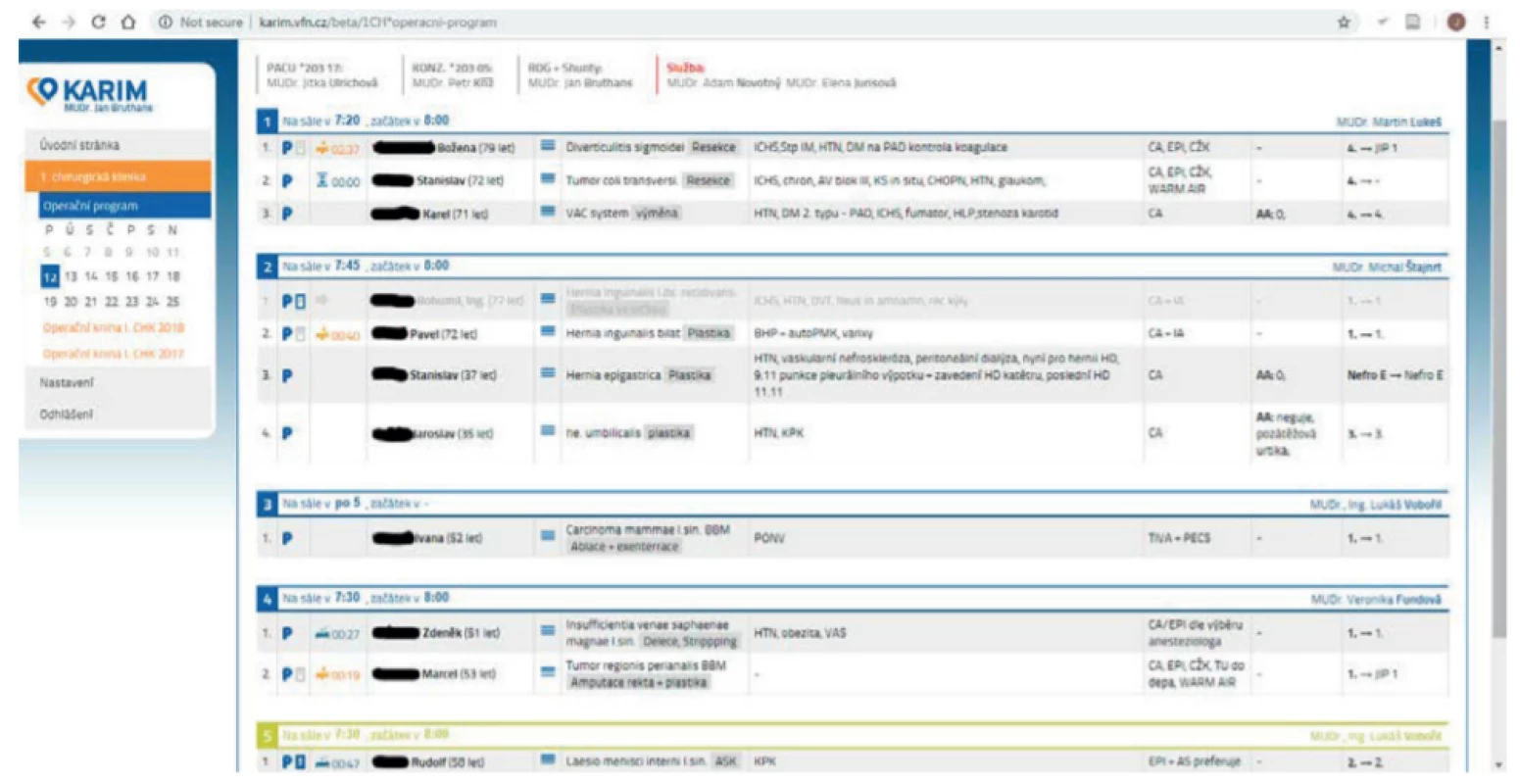
After the case closure the attending anesthesiologist fills a case data to the system (drugs used, types of anesthesia, potential complications, and nurse present), data from anesthesia consultation are used to pre-fill the form – see Fig. 3). From these data, the required statistical data are computed and depicted in the system.
Fig. 3. Anesthesia data entry. 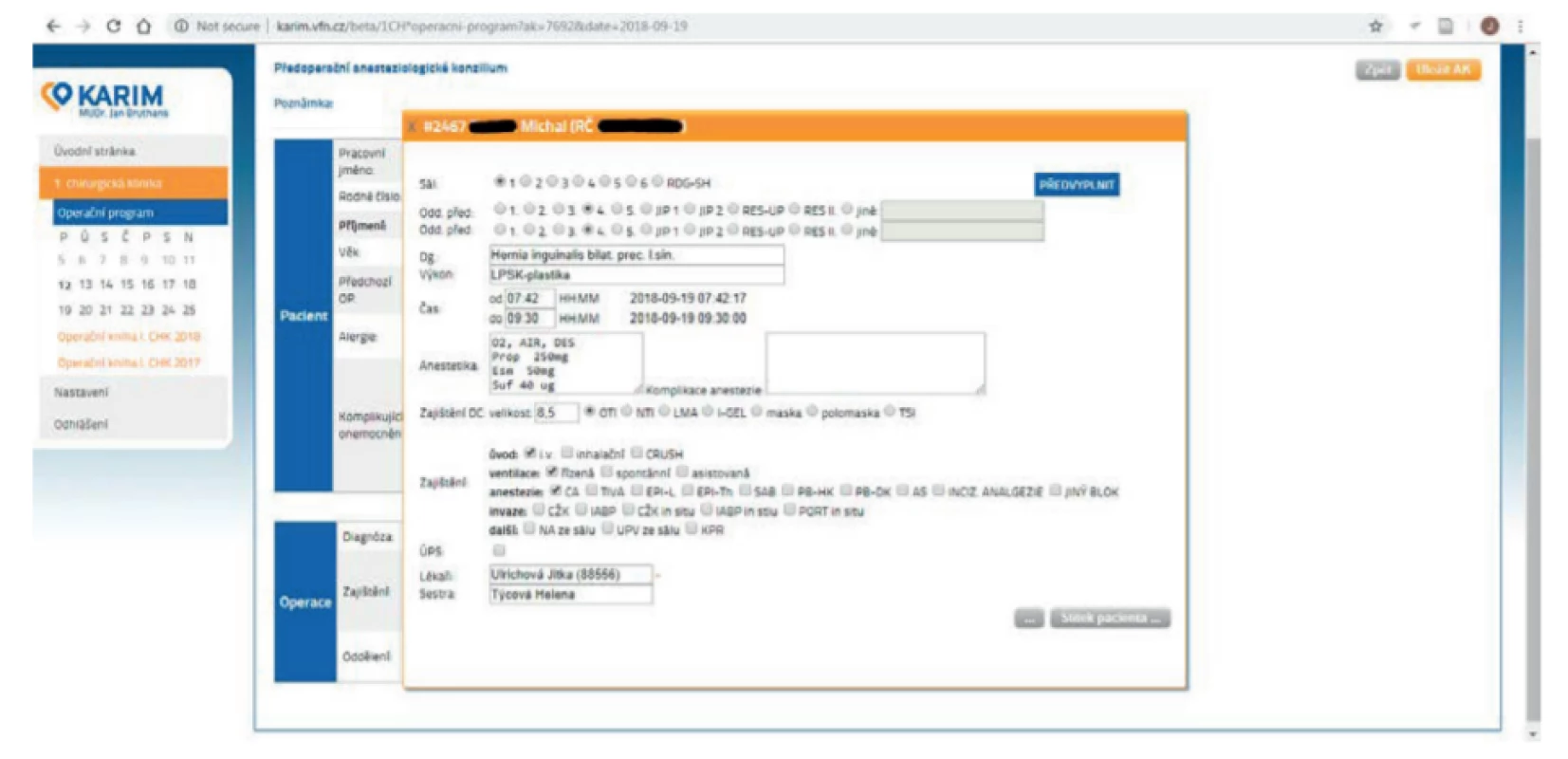
Discussion
As already stated above, AIMS would cover not only functions provided by our system, but much other functionalities are available - automated entry from the anesthesia and monitoring devices, creating of elec-tronic record, billing of the care provided, even clinical decision systems [4, 5]. Studies also show that AIMS increases accuracy over manually handwritten records [6]. Still AIMS are not always part of HIS and such an integration might be a challenging task [7], also atten-tion should be given to the user interface design of AIMS [8].
However, up to my knowledge there is no functional AIMS in the Czech Republic, despite growing usage worldwide [9]. Our HIS (Stapro Medea) does not have such functionality and acquiring and integration of AIMS is not a priority for our hospital. Facing this situation, we decided for an in-house proprietary system that covers at least our most pressing needs. Other authors have felt the same way and designed a proprietary tracking system [10].
Although we have not monitored time needed for creating our system, we can certainly claim that we ended with an inexpensive solution. Still, our approach has its limits and is dependent on its creators. The documentation of the system is virtually non-existent, and departure of our colleague programmer would mean a serious hurdle in the system usage.
The system is still regarded as “beta”, so smaller errors happen from time to time. We still plan to add other functions, as documenting of the stay at PACU and we would like to expand its usage from our sub-department to all five anesthesiology sub-departments.
Conclusions
Although AIMS is an ideal and ultimate solution for anesthesia management and for work flow management in OR, much simpler interim solutions are obtainable. Such a house-developed system might be inexpensive and well-tailored to specific needs and can provide an improvement in the daily anesthesia and surgery care.
Jan Bruthans, M.D., Ph.D.
Department of Biomedical Technology
Faculty of Biomedical Engineering
Czech Technical University in Prague
nám. Sítná 3105, CZ-272 01 Kladno
E-mail: bruthjan@fbmi.cvut.cz
Phone: +420 723 426 288
Zdroje
-
Behrová, J.: Porovnání komerčních NIS (nemocničních infor-mačních systémů) používaných v jednotlivých zdravotnických zařízeních v ČR (Comparison of Commercial EMTs Used in Health-Care Facilities in the CR) [Diploma thesis]. [Kladno]: Czech Technical University; 2016.
-
Spahni, S., Lovis, C., Mercille, R., Verdel, H., Cotton, M., Geiss-bühler, A.: Implementing a new ADT based on the HL7 version 3 RIM. Int J Med Inf 2007;76 : 190–4.
-
Černý, V., Cvachovec, K., Ševčík, P., Šturma, J.: Recommended examinations before diagnostic or therapeutic procedures when anesthesia care is required [Internet]. Czech Society of Anaes-thesiology and Intensive Care Medicine; 2009 [cited 2018 Sep 29]. Available from: http://www.csarim.cz/storage/app/media/
Doporucene%20postupy%20a%20stanoviska%20CSARIM/MP_CSARIM_Predanest_vysetreni_verze_2_final_190509.pdf -
Kadry, B., Feaster, W. W., Macario, A., Ehrenfeld, J. M.: Anes-thesia Information Management Systems: Past, Present, and Future of Anesthesia Records. Mt Sinai J Med J Transl Pers Med. 2012 Jan;79(1):154–65.
-
Shah, N. J., Tremper, K. K., Kheterpal, S.: Anatomy of an Anes-thesia Information Management System. Anesthesiol Clin. 2011 Sep;29(3):355–65.
-
Reich, D. L., Wood, R. K., Mattar, R., Krol, M., Adams, D. C., Hossain, S., et al.: Arterial Blood Pressure and Heart Rate Discrepancies Between Handwritten and Computerized Anes-thesia Records. Anesth Analg. 2000 Sep;91(3):612–6.
-
Springman, S. R.: Integration of the enterprise electronic health record and anesthesia information management systems. Anesthesiol Clin. 2011 Sep;29(3):455–83.
-
Wanderer, J. P., Rao, A. V., Rothwell, S. H., Ehrenfeld, J. M.: Comparing two anesthesia information management system user interfaces: a usability evaluation. Can J Anesth Can Anesth. 2012 Nov;59(11):1023–31.
-
Ehrenfeld, J. M., Rehman, M. A.: Anesthesia information mana-gement systems: a review of functionality and installation considerations. J Clin Monit Comput. 2011 Feb;25(1):71–9.
-
Wiemuth, M., Fink, E., Burgert, O.: A workflow management system for the perioperative area supporting all actors. In: 2015 17th International Conference on E-health Networking, Application & Services (HealthCom) [Internet]. Boston, MA, USA: IEEE; 2015 [cited 2018 Sep 29]. p. 28–31. Available from: http://ieeexplore.ieee.org/document/7454468/
Štítky
Biomedicína
Článek vyšel v časopiseLékař a technika

2018 Číslo 3-
Všechny články tohoto čísla
- EFFECT OF SAMPLING RATE ON THE ACCURACY OF MEASUREMENT OF NEONATAL OXYGEN SATURATION EXPOSURE
- BIPHASIC CALCIUM PHOSPHATE SCAFFOLDS DERIVED FROM HYDROTHERMALLY SYNTHESIZED POWDERS
- FLEXIBLE TEG ON THE ANKLE FOR MEASURING THE POWER GENERATED WHILE PERFORMING ACTIVITIES OF DAILY LIVING
- FROM WHITE BOARD TO PATIENT TRACKING SYSTEM IN ANESTHESIA AND BEYOND
- EEG MICROSTATES ANALYSIS IN PATIENTS WITH EPILEPSY
- Lékař a technika
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- EEG MICROSTATES ANALYSIS IN PATIENTS WITH EPILEPSY
- EFFECT OF SAMPLING RATE ON THE ACCURACY OF MEASUREMENT OF NEONATAL OXYGEN SATURATION EXPOSURE
- BIPHASIC CALCIUM PHOSPHATE SCAFFOLDS DERIVED FROM HYDROTHERMALLY SYNTHESIZED POWDERS
- FLEXIBLE TEG ON THE ANKLE FOR MEASURING THE POWER GENERATED WHILE PERFORMING ACTIVITIES OF DAILY LIVING
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



