-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Prevalence study on carbapenemase-producing Escherichia coli and Klebsiella pneumoniae isolates in Czech hospitals – results from Czech Part of European Survey on Carbapenemase--Producing Enterobacteriaceae (EuSCAPE)
Prevalenční studie kmenů Escherichia coli a Klebsiella pneumoniae produkujících karbapenemázu v českých nemocnicích – výsledky české části studie EuSCAPE (European Survey on Carbapenemase-Producing Enterobacteriaceae)
Cíl:
Jedním z faktorů ohrožujících současnou medicínu je šíření multirezistentních gramnegativních bakterií. V článku jsou shrnuty výsledky 6měsíční prevalenční studie zaměřené na kmeny K. pneumoniae a E. coli provedené v českých nemocnicích v rámci projektu EuSCAPE (European Survey on Carbapenemase-Producing Bacteria).Metodika:
Do studie bylo zapojeno 10 nemocnic ze všech krajů České republiky. Během sledovaného období (1. listopad 2013 až 30. duben 2014) bylo shromažďováno deset prvozáchytů K. pneumoniae a E. coli necitlivých ke karba-penemům z klinických vzorků (krev, dolní cesty dýchací, moč, punktát, stěry z ran). Zároveň byl deponován první citlivý izolát zachycený od téhož pacienta a vybraného bakteriálního druhu. Byla stanovena citlivost k 15 různým antibiotikům podle metodiky EUCAST. Karbapenemázy byly identifikovány metodou MALDI-TOF MS hydrolýzy meropenemu. Kmeny produkující karbapenemázy byly podrobeny multilokusové sekvenační typizaci a byly identifikovány geny karpapenemáz.Výsledky:
Během sledovaného období bylo shromážděno 30 izolátů (K. pneumoniae n = 28, E. coli n = 2) necitlivých ke karbapenemům. U pacienta přeloženého z Ukrajiny po zranění během revoluce na Majdanu byl identifikován sekvenční typ (ST) 11 K. pneumoniae produkující karbapenemázu NDM-1. Druhý izolát produkující karbapenemázu produkoval enzym OXA-48. Jednalo se o kmen K. pneumoniae ST101 identifikovaný u pacienta přijatého z komunity.Závěr:
Tato prevalenční studie opět potvrdila nízkou prevalenci enterobakterií produkujících karbapenemázy (CPE) v České republice. Zároveň opět ukazuje na riziko spojené s importem CPE ze zemí s vysokou prevalencí nebo neznámou epidemiologickou situací..Klíčová slova:
karbapenemázy – CPE – MALDI-TOF – citlivost – rezistence – Enterobacteriaceae
Authors: J. Hrabák 1; V. Študentová 1; V. Jakubů 2; V. Adámková 3
; L. Dvořáková 4; M. Balejova 5; T. Bergerová 1; E. Chmelařová 6; P. Ježek 7; P. Kabelíková 8; M. Kolář 9
; P. Paterová 10; R. Tejkalová 11; C. Papagiannitsis 1; H. Žemličková 2
Authors place of work: Department of Microbiology, Faculty of Medicine and University Hospital in Plzen, Plzen, Czech Republic 1; National Reference Laboratory for Antibiotics, National Institute of Public Health, Prague, Czech Republic 2; Department of Clinical Microbiology, General University Hospital, Prague, Czech Republic 3; Department of Microbiology, Masaryk’s Hospital, Ústí nad Labem, Czech Republic 4; Laboratory of Bacteriology, České Budějovice Hospital, České Budějovice, Czech Republic 5; Department of Microbiology, Institute of Public Health, Ostrava, Czech Republic 6; Department of Microbiology, Regional Hospital in Příbram, Příbram, Czech Republic 7; Department of Medical Microbiology, Motol University Hospital, Charles University, Prague, Czech Republic 8; Department of Microbiology, Faculty of Medicine and Dentistry, Palacky University Olomouc and University Hospital Omouc Olomouc, Czech Republic 9; Department of Clinical Microbiology, Faculty of Medicine and University Hospital in Hradec Králové, Hradec Králové, Charles University, Czech Republic 10; Department of Microbiology, Faculty of Medicine, Masaryk University and St. Anne’s University Hospital, Brno, Czech Republic 11
Published in the journal: Epidemiol. Mikrobiol. Imunol. 64, 2015, č. 2, s. 87-91
Category: Původní práce
Summary
Objective:
One of the most important threats of current medicine is the spread of multiresistant Gram-negative bacteria. We report here data from a six-month prevalence study on carbapenemase-producing K. pneumoniae and E. coli performed in Czech hospitals participating on European Survey on Carbapenemase-Producing Enterobacteriaceae (EuSCAPE).Methods:
Ten hospitals covering all regions of the Czech Republic were selected. During the study period (1st November 2013 to 30th April 2014), first ten carbapenem non-susceptible isolates of K. pneumoniae or E. coli isolated from non-surveillance specimens (i.e., blood, lower respiratory tract secretions, urine, puncture fluids, and wound secretions) of single successive patients were collected. Successive carbapenem-susceptible isolates of the same species were also preserved as controls. Susceptibility to 15 antibiotics was determined using EUCAST recommendations. Carbapenemase activity was detected by MALDI-TOF MS meropenem hydrolysis assay. Positive isolates were subjected for molecular typing (multi-locus sequence typing, identification of carbapenemase gene).Results:
During the study period, thirty non-susceptible isolates (K. pneumoniae n = 28, E. coli n = 2) were identified in 5 hospitals. Only two of them were confirmed to be carbapenemase producers. A NDM-1-producing K. pneumoniae ST11 was recovered from a patient, transferred from Ukraine, being injured during a Maidan revolution. The second isolate, an OXA-48-producing K. pneumoniae, belonging to ST101, was recovered from a patient admitted to a hospital for an ischemic stroke.Conclusions:
This study again confirmed that the Czech Republic still belongs to the countries with low prevalence of carbapenemase-producing Enterobacteriaceae (CPE). Cases of CPE are usually restricted to an import from high-prevalence countries or countries with unknown epidemiological situation.Keywords:
carbapenemase – CPE – MALDI-TOF – susceptibility – resistance – EnterobacteriaceaeINTRODUCTION
One of the most important antibiotic resistance mechanisms in Enterobacteriaceae is production of carbapenemases. Those enzymes are mostly able to hydrolyse almost all b-lactams, including carbapenems. Their genes are usually encoded on mobile genetic elements, (e.g., plasmids) encoding other resistance determinants such as aminoglycoside-modifying enzymes, gyrase/topoisomerase-protecting proteins (Qnr) etc. Genes of metallo-b-lactamases, a diverse group of carbapenemases, are commonly found as gene cassettes of integrons resulting in multiresistant phenotype of the strain. Some carbapenemase genes are closely connected to epidemiologically successful clones (e.g., KPC-producing Klebsiella pneumoniae ST258/ST512) or epidemiologically successful plasmids with high conjugation potential (e.g., blaOXA-48-type connected with IncL/M plasmids) [1, 2, 3].
In the Czech Republic, occurrence of carbapenemase-producing Enterobacteriaceae (CPE) has been reported low, restricted on cases identified in patients repatriated from countries with high CPE prevalence (e.g., Greece, Italy, Sri Lanka) and sporadic outbreaks [4, 5, 6]. In some European countries, however, epidemiological situation seems to be alarming (e.g., Greece and Italy) with more than 30% carbapenem-resistant K. pneumoniae invasive isolates reported annually to the EARS-Net database [7]. In patients infected by a CPE, treatment options are usually limited to only few choices (e.g., colistin, combination therapy) with unpredicted outcome [8].
In April of 2010, the first meeting funded by European Centre for Disease Prevention and Control (ECDC) held in Netherlands’ National Institute for Public Health and the Environment (RIVM). As a result from that workshop, the first position article describing epidemiological situation in participated countries was published [9]. Followed that initiative, European Survey on Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) was established. The Czech Republic belongs to the members, that have participated on EuSCAPE activities since its establishment in 2010.
Based on national data, a surveillance article describing the progress in the spread of CPEs in Europe was published in collaboration with national EuSCAPE representatives in 2013 [7]. The data suggest that except few countries with high rate of KPC - and VIM-producing isolates and silent spread of OXA-48-type carbapenemases, the situation seems to be stabilized. As reported by most European countries (including the Czech Republic), national guidelines for detection, verification and for management of colonized/infected patient are available.
We report here data from a prevalence study on carbapenemase-producing K. pneumoniae and Escherichia coli performed in 10 Czech hospitals between 1st November 2013 and 30th April 2014. Similar study was performed in all European countries participating on EuSCAPE project (n = 39).
MATERIALS AND METHODS
Study Design
Ten hospitals (see Table 1, Figure 1) covering all regions were selected. During the study period (1st November 2013 to 30th April 2014), first ten carbapenem non-susceptible isolates of K. pneumoniae or E. coli recovered from single successive patients had been collected. Selected clinically-significant isolates were included in the study (i.e., blood, lower respiratory tract secretions, urine, puncture fluids, and wound secretions). No surveillance or screening isolates were included (e.g., stool, upper respiratory tract). Non-susceptibility was defined according to the epidemiological cut-off value (ECCOF) of K. pneumoniae of at least one carbapenem (i.e., ertapenem MIC > 0,064 mg/l, meropenem MIC > 0,125 mg/l, imipenem MIC >1 mg/l, or inhibition zone diameter [IZ] for ertapenem < 29 mm, meropenem < 25 mm, and imipenem < 24 mm respectively). Carbapenem-susceptible isolates (a wild-type) of the same species and the same patient identified were also preserved as carbapenem-susceptible control group.
Figure 1. Distributions of hospitals participated on EuSCAPE project in the Czech Republic Obr. 1. Distribuce nemocnic zúčastněných v projektu EuSCAPE v České republice 
Species Identification and Susceptibility Testing
Each isolate sent to the Department of Microbiology, Faculty of Medicine in Plzen, Charles University in Prague was re-identified using MALDI-TOF mass spectrometry (MS), MALDI Biotyper version 3.1 (Bruker Daltonik GmbH, Bremen, Germany). Susceptibility to ampicillin, amoxicillin/clavulanic acid, cefotaxime, ceftazidime, cefepime, aztreonam, ciprofloxacin, gentamicin, tobramycin, co-trimoxazole, piperacillin/tazobactam was determined by disk diffusion method and interpreted using EUCAST recommendations [10]. Minimal inhibitory concentrations (MICs) of ertapenem, meropenem, imipenem, colistin and fosfomycin, were examined using E-test (bioMérieux) and categorized according to the EUCAST criteria as well [10].
Detection of b-Lactamases
Carbapenemase activity was detected using MALDI-TOF MS meropenem hydrolysis assay [11, 12] with recently described modification [13]. In that modification, reaction buffer is supplemented by ammonium bicarbonate to enhance sensitivity against OXA-48-type carbapenemases [13]. Carbapenemases were preliminary identified using an inhibitor-based phenotypic method [14]. Precise identification was performed by PCR amplification followed by sequencing of respective carbapenemase gene [14].
Typing of the Isolates
Carbapenemase-producing isolates were subjected for multi-locus sequence typing (MLST) as previously described [15]. Sequence types (STs) were assigned at the K. pneumoniae MLST database (http://www.pasteur.fr/recherche/genopole/PF8/mlst/Kpneumoniae.html).
RESULTS
During the study period, thirty-nine isolates were collected (Klebsiella pneumoniae n = 37, Escherichia coli n = 2). Thirty, including both E. coli isolates, were non-susceptible to at least one carbapenem. Seven isolates were collected as negative controls. Carbapenem non-susceptible isolates were identified in 5 of 10 hospitals included in the study. All of those five hospitals were tertiary-care university settings providing a specialized care (including hematooncology wards). Description of the hospitals is summarized in Table 1.
Tab. 1. Number of isolates included in the study collected from each hospital and characteristics of the region/hospitalFigure 1. Distributions of hospitals participated on EuSCAPE project in the Czech Republic Tabulka 1. Počet izolátů zahrnutých ve studii identifikovaných v jednotlivých nemocnicích včetně charakteristiky spádové oblasti 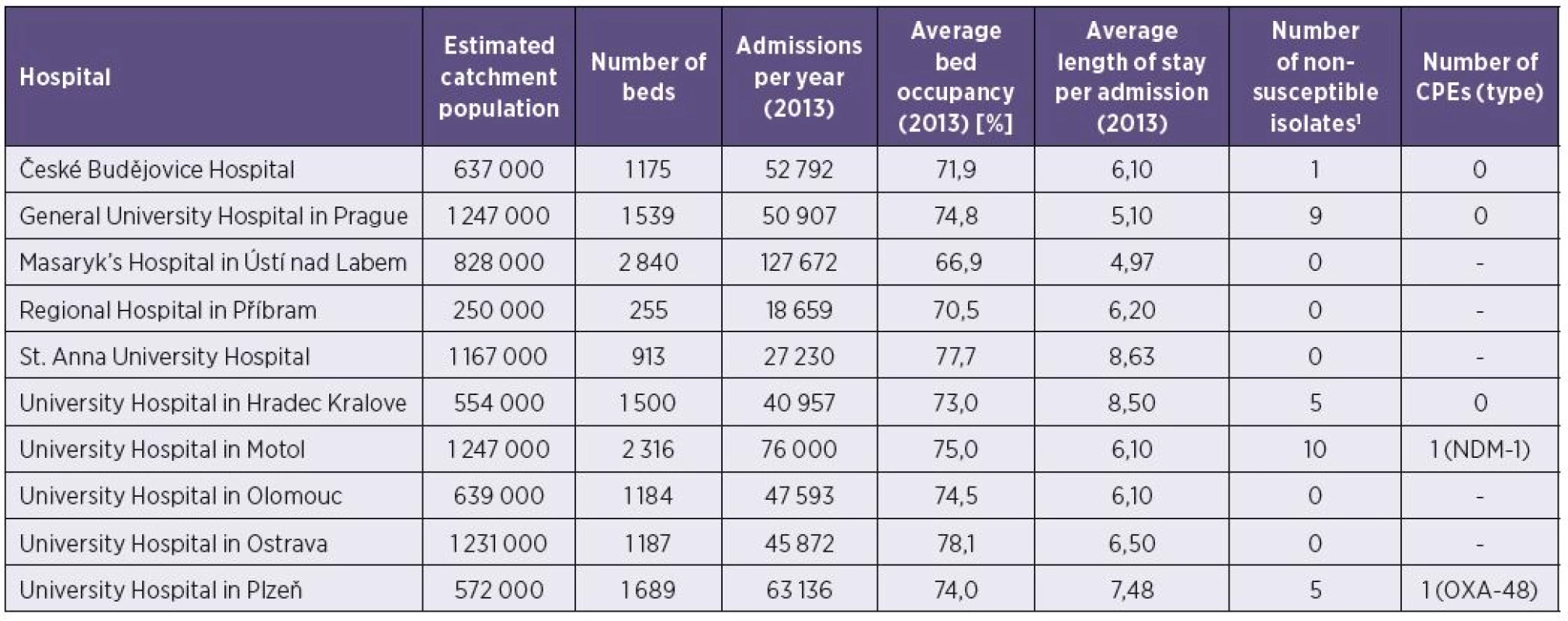
Among the non-susceptible isolates, only two K. pneumoniae isolates were confirmed as carbapenemase producers. In the University Hospital in Motol, K. pneumoniae ST11 producing NDM-1 metallo-b-lactamase was recovered from a wound of 51 years old man transferred from Ukraine being injured during Maidan revolution. Based on the Czech National Guideline [16], the patient was isolated immediately after the admission to the hospital and screened for the presence of CPE. Therefore, no transmission to other patients occurred.
The second isolate, a ST101 K. pneumoniae producing OXA-48 carbapenemase was recovered from a bronchoalveolar lavage of a 39 years old man hospitalized for an ischemic stroke. The isolate was identified immediately after patient’s admission (hospitalization in ICU). The patient died on the 5th day of hospitalization. Because of an isolation of that patient immediately after identification of carbapenem non-susceptible isolate and screening of the ICU patients for 4 weeks according to the Czech National Guideline [16], no spread of the OXA-48-producing isolate has been observed.
Resistance of the other carbapenem-non-susceptible isolates (n = 28) was caused by an alteration of a cell-wall permeability together with a production of b-lactamases with no activity against carbapenems (competitive inhibition).
DISCUSSION
Occurrence of CPEs in Europe varied from sporadic occurrence (e.g., Denmark, Latvia, Lithuania, Slovenia) to the countries with endemic situation (e.g., Greece, Italy) [7]. The majority of European countries, including the Czech Republic, are categorized as regions with single/sporadic hospital outbreaks [7]. Since 2010, when a complex European study on CPEs was performed [9], in almost all countries an increase of CPEs occurrence has been observed. Only in Israel, which was included in the study as well, the situation changed from an epidemiological stage “endemic” to “inter-regional spread” [7].
This study again confirmed that the Czech Republic still belongs to the countries with low CPE prevalence. During the study period, we identified only two carbapenemase-producing K. pneumoniae isolates. In 2011, only three hospital out-breaks (VIM-1-producing K. pneumoniae ST11, KPC-3-producing K. pneumoniae ST512, KPC-2-producing K. pneumoniae ST258) and two sporadic cases (VIM-4-producing K. pneumoniae, KPC-2-producing K. pneumoniae ST258) were observed [5]. In period that followed, occurrence of CPEs in the Czech Republic remains the same, restricted to few hospital outbreaks and sporadic imported cases [6, 17]. In Czech Republic, current epidemiological situation may be probably caused by strict surveillance (included a selective screening and isolation procedures) in patients repatriated from foreign countries or those in a risk with a contact with patient infected/colonized by CPE as it is recommended by Czech Ministry of Health [16].
Interestingly, the OXA-48-producing K. pneumoniae identified at the University Hospital in Plzen was recovered from a community patient. This finding suggests a potential unnoticed spread of this b-lactamase in community as described in other countries [2, 18]. Another remarkable finding was that the NDM-1-producing K. pneumoniae was recovered from an Ukrainian patient. To our knowledge, this is the first description of carbapenemase-producing Enterobacteriaceae in Ukraine. Unfortunately, there is no epidemiological data focusing on resistance in this European country. As many people from Ukraine works in EU countries, this may represent a potential risk for public health as it has also been described for other serious pathogens (HIV, Mycobacterium tuberculosis) [19, 20].
Those findings, however, have demonstrated the necessity of the detection of carbapenemase-producing bacteria in routine microbiological laboratories. Even if the epidemiological situation in the Czech Republic seems to be optimistic, unnoticed spread of CPEs may represent serious problem for public health. Based on EU level, surveillance recommendations have been introduced in many European countries as well as a Risk Assessment has been published by European Centre for Disease Prevention and Control based on EuSCAPE project results [21].
Acknowledgement
This study was supported by the research project grants from the Ministry of Health of the Czech Republic (grant Nr. NT11032-6/2010); and by the Charles University Research Fund (project Nr. P36). C. C. Papagiannitsis was supported by the project: „Support of establishment, development, and mobility of quality research teams at the Charles University“ financed by The Education for Competitiveness Operational Programme (ECOP) funded by the ESF and the government budget of the Czech Republic (project Nr.CZ.1.07/2.3.00/30.0022).
Do redakce došlo dne 20. 10. 2014.
Adresa pro korespondenci:
Doc. Ing. Jaroslav Hrabák, Ph.D.
Biomedicínské centrum
Alej Svobody 76
304 60 Plzeň
e-mail: Jaroslav.Hrabak@lfp.cuni.cz
Zdroje
1. Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, Cornaglia G, Garau J, Gniadkowski M, Hayden MK, Kumarasamy K, Livermore DM, Maya JJ, Nordmann P, Patel JB, Paterson DL, Pitout J, Villegas MV, Wang H, Woodford N, Quinn JP. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis, 2013;13 : 785-796.
2. Poirel L, Potron A, Nordmann P. OXA-48-like carbapenemases: the phantom menace. J Antimicrob Chemother, 2012;67 : 1597-1606.
3. Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL. Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev, 2012;25 : 682-707.
4. Hrabak J, Niemczyková J, Chudackova E, Fridrichova M, Studentova V, Cervena D, Urbaskova P, Zemlickova H. KPC-2-producing Klebsiella pneumoniae isolated from a Czech patient previously hospitalized in Greece and in vivo selection of colistin resistance. Folia Microbiol, 2011;56 : 361–365.
5. Hrabak J, Papagiannitsis CC, Studentova V, Jakubu V, Fridrichova M, Zemlickova H and Czech Participants of European Antimicrobial Resistance Surveillance Network. First outbreaks of carbapenemase-producing Klebsiella pneumoniae in the Czech Republic in 2011. Euro Surveill, 2013;18:pii=20626.
6. Papagiannitsis CC, Studentova V, Chudackova E, Bergerova T, Hrabák J, Raděj J, Novak I. Identification of a New Delhi Metallo-β-lactamase-4 (NDM-4)-producing Enterobacter cloacae from a Czech patient previously hospitalized in Sri Lanka. Folia Microbiologica, 2013;58 : 547–549.
7. Glasner C, Albiger B, Buist G, Tambić Andrašević A, Cantón R, Carmeli Y, Friedrich AW, Giske CG, Glupczynski Y, Gniadkowski M, Livermore DM, Nordmann P, Poirel L, Rossolini GM, Seifert H, Vatopoulos A, Walsh T, Woodford N, Donker T, Monnet DL, Grundmann H and the European Survey on Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) working group. Carbapenemase-producing Enterobacteriaceae in Europe: a survey among national experts from 39 countries, February 2013. Eurosurveillance, 2013;18:pii=20525.
8. Falagas ME, Karageorgopoulos DE, Nordmann P. Thera-peutic options for infections with Enterobacteriaceae producing carbapenem-hydrolyzing enzymes. Future Microbiol, 2011;6 : 653–666.
9. Grundmann H, Livermore DM, Giske CG, Canton R, Rossolini GM, Campos J, Vatopoulos A, Gniadkowski M, Toth A, Pfeifer Y, Jarlier V, Carmeli Y, CNSE Working Group. Carbapenem-non-susceptible Enterobacteriaceae in Europe: conclusions from a meeting of national experts. Euro Surveillance, 2010;15:pii=19711.
10. European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, version 4.0. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/Breakpoint_table_v_4.0.pdf, 2014;Accessed 1th February 2013
11. Hrabák J, Walková R, Študentová V, Chudáčková E, Bergerová T. Carbapenemase Activity Detection by Matrix-Assisted Laser Desorption/Ionisation Time-of-Flight Mass Spectrometry. J Clin Microbiol, 2011;49 : 3222–3227.
12. Hrabák J, Studentová V, Walková R, Zemlicková H, Jakubu V, Chudácková E, Gniadkowski M, Pfeifer Y, Perry JD, Wilkinson K, Bergerová T. Detection of NDM-1, VIM-1, KPC, OXA-48, and OXA-162 carbapenemases by MALDI-TOF mass spectrometry. J Clin Microbiol, 2012;50 : 2441–2443.
13. Studentova V, Papagiannitsis CC, Izdebski R, Pfeifer Y, Chudackova E, Bergerova T, Gniadkowski M, Hrabak J. Detection of OXA-48-type carbapenemase-producing Enterobacteriaceae in diagnostic laboratories can be enhanced by addition of bicarbonates to cultivation media or reaction buffers. Folia Microbiol, 2014;20 : 839-853. DOI: 10.1007/s12223-014-0349-8
14. Hrabák J, Papagiannitsis CC, Chudáčková E. Detection of carbapenemases in Enterobacteriaceae: a challenge for diagnostic microbiological laboratories. Clin Microbiol Infect, 2014: in press. DOI: 10.1111/1469-0691.12678
15. Diancourt L, Passet V, Verhoef J, Grimont PA, Brisse S. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol, 2005;43 : 178–182.
16. Ministry of Health of the Czech Republic. 2012. Control of cases of colonisation/infection by carbapenemase-producing enterobacteria (CPE – carbapenemase-producing enterobacteria). Věstník Ministerstva zdravotnictví ČR, 2012;8 : 10-19. Available on http://www.mzcr.cz/Legislativa/dokumenty/vestnik-c8/2012_6865_2510_11.html.
17. Hrabák J, Jakubů V, Španělová P, Študentová V, Papagiannitsis CC, Urbášková P, Žemličková H. Carbapenemase producing Enterobacteriaceae detected in the Czech Republic from June 2012 to April 2014. Zprávy CEM, 2014;23 : 137–140.
18. Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers in Enterobacteriaceae worldwide. Clin Microbiol Infect, 2014: in press.
19. Kelly JA, Amirkhanian YA. The newest epidemic: a review of HIV/AIDS in Central and Eastern Europe. Int J STD AIDS, 2003;14 : 361–371.
20. Atun R, Olynik I. Resistance to implementing policy change: the case of Ukraine. Bull World Health Organ, 2008;86 : 147–154.
21. Grundmann H, Glasner C, Magiorakos A-P, Högberg-Diaz L, Monnet DL, Albiger B. Carbapenemase-producing bacteria in Europé: results from the EuSCAPE project, 2013, Stocholm: European Centre for Disease Prevention and Control, 2013.
Štítky
Hygiena a epidemiologie Infekční lékařství Mikrobiologie
Článek MUDr. Gustav Walter
Článek vyšel v časopiseEpidemiologie, mikrobiologie, imunologie
Nejčtenější tento týden
2015 Číslo 2- Stillova choroba: vzácné a závažné systémové onemocnění
- Jak souvisí postcovidový syndrom s poškozením mozku?
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
-
Všechny články tohoto čísla
- Enterovirus sequencing as a new approach to the laboratory diagnosis for clinical and epidemiological purposes
- Profesor Zdeněk Hubálek, nový nositel Patočkovy medaile
- Významné životní výročí MUDr. Vladimíra Zikmunda, CSc.
- MUDr. Gustav Walter
- Toxoplasmosis in immunocompromised patients
- The possibilities of zoonotic transmission of rotaviruses
- Hepatitis E – overview of the latest knowledge
- West Nile virus transmission risk in the Czech Republic
- Prevalence study on carbapenemase-producing Escherichia coli and Klebsiella pneumoniae isolates in Czech hospitals – results from Czech Part of European Survey on Carbapenemase--Producing Enterobacteriaceae (EuSCAPE)
- Diagnosis of infections caused by Clostridium difficile in the Czech Republic: availability, possibilities, and interpretation of laboratory results
- The prevalence of nasal carriage of Staphylococcus aureus aureus and methicillin-resistant S. aureus (MRSA) among general medicine students of the Palacky University Olomouc
- Epidemiologie, mikrobiologie, imunologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- The possibilities of zoonotic transmission of rotaviruses
- Hepatitis E – overview of the latest knowledge
- The prevalence of nasal carriage of Staphylococcus aureus aureus and methicillin-resistant S. aureus (MRSA) among general medicine students of the Palacky University Olomouc
- Toxoplasmosis in immunocompromised patients
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



