-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Fetal MRI – a brief update on current imaging and indications
Fetální magnetická rezonance – stručný přehled současného zobrazení a indikací
Cíl: Autoři se v článku zabývají možnostmi vhodného zobrazení a nejčastějšími indikacemi k magnetické rezonanci u plodu.
Metody: Na příkladech klinických indikací k diagnostice pomocí magnetické rezonance jsou dokumentována orgánová specifika metody. Popsány jsou nejtypičtější systémově zaměřené indikace včetně nejběžnějších zobrazovacích technik. Nálezy jsou doplněny obrazovou dokumentací.
Výsledky: Magnetická rezonance má dnes důležité místo v prenatální diagnostice centrálního nervového systému i orgánů plodu, má úlohu v plánování postnatálního managementu.
Závěry: Fetální magnetická rezonance hraje klíčovou úlohu zejména při diagnostice složitějších onemocnění a anomálií plodu.
Klíčová slova:
indikace – fetální magnetická rezonance – zobrazování
Authors: Jayapal Praveen 1; Kyncl Martin 2; Rubesova Erika 1
Authors place of work: Department of Radiology, Lucile Packard Children‘s Hospital, Stanford University School of Medicine, Stanford, California, USA ; Department of Radiology, Second Faculty of Medicine, Charles University and Motol University Hospital, Prague, Czech Republic 2
Published in the journal: Čes-slov Pediat 2023; 78 (2): 91-95.
Category: Přehledový článek
doi: https://doi.org/10.55095/CSPediatrie2023/013Summary
Objective: In this article, the authors describe the most common indications of fetal MRI and the appropriate imaging technique.
Methods: Fetal MRI image acquisition is explained for the most common indications. The technique is illustrated by various cases.
Results: MRI has become an indispensable imaging tool for prenatal diagnosis, characterization, and postnatal management planning of fetal neurological or body anomalies.
Conclusions: Fetal MRI is an essential diagnostic tool for the diagnosis of challenging and complex fetal anomalies.
Keywords:
imaging – indications – fetal magnetic resonance
Introduction
Ultrasound is the first-line imaging modality for diagnosing fetal anomalies, however some anatomical structures are difficult to image due to fetal position or bone shadowing. Although ultrasound has a great spatial resolution it has a relatively low tissue contrast, and some abnormalities may be difficult to characterize on ultrasound alone. The first MRI was performed in 1983 in a pregnant patient for placental abnormality but it is only with the development of rapid single shot acquisition in early nineties, that MRI started to be used more broadly as an additional diagnostic tool.(1) Although MRI compared with US, is less readily available, and more expensive,(2) MRI has become an indispensable imaging tool for prenatal diagnosis, characterization, and postnatal management planning of fetal neurological or body anomalies. Fetal MRI performed before 18 weeks provides very limited information since spatial resolution of MRI is lower than of ultrasound but can be occasionally performed in severe anomalies. In some cases, additional information can be obtained before 22 weeks however MRI becomes increasingly helpful thereafter.(3) The use of 3-T magnets in fetal MRI has improved the availability and quality of advanced imaging sequences and provides diagnostic images.(4)
In this article, we discuss the availability of appropriate imaging and common indications for fetal MRI.
Common clinical indications
Common clinical indications are summarized in the table 1.
Tab. 1. Common indications for fetal MRI 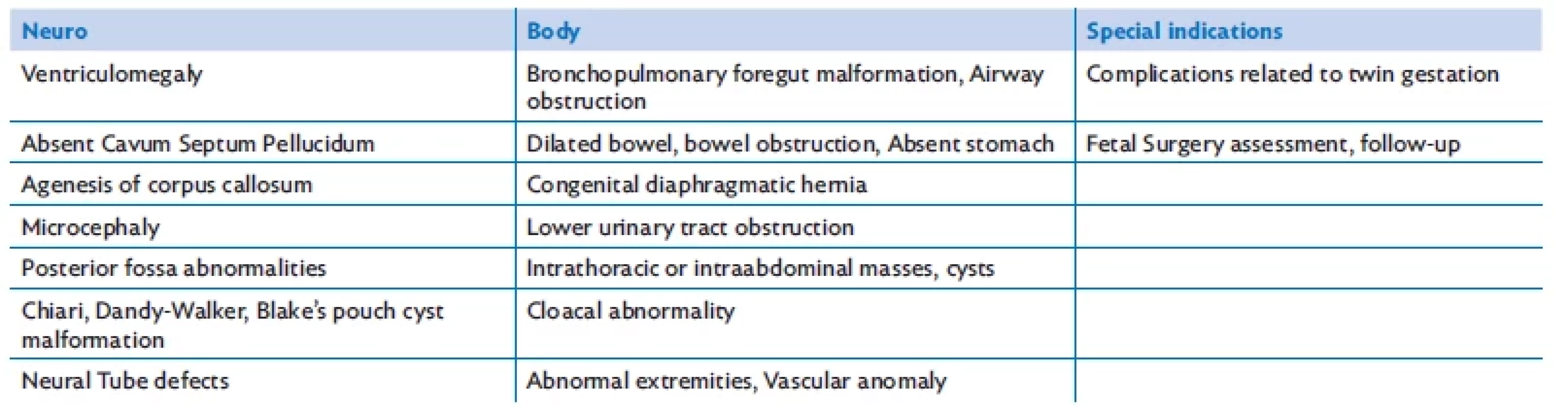
Neurological indications
The first fetal MRI’s were performed for brain anomalies and neurological indications remain the main indication for fetal MRI. Neurological indications are by far predominant and up to 30% of the fetal MRI scans are performed on a 3-T unit.(5) The major advantage of 3-T MRI is its increased signal-to-noise ratio, which is linearly proportional to the imaging field strength. For fetal MRI neurological indications, especially for assessment of the posterior fossa, parenchymal lesions and small midline structures, imaging at 3 T when available is preferable (Fig. 1). When compared to ultrasound, MR images are not impacted by the shadowing of the skull which is a limitation of ultrasound. Additionally, images can be obtained in any plane and are not limited by fetal position.(6) Often the abnormalities detected by fetal US represent the tip of an iceberg, and further evaluation with MRI reveals additional underlying abnormalities.
Fig. 1. A 30-week-old fetus with Dandy-Walker malformation. A sagittal T2-weighted Single-Shot Turbo Spin Echo (SSTSE) sequence at 3-T. MRI shows hypoplastic vermis (arrow) and posterior fossa cyst (asterisk). 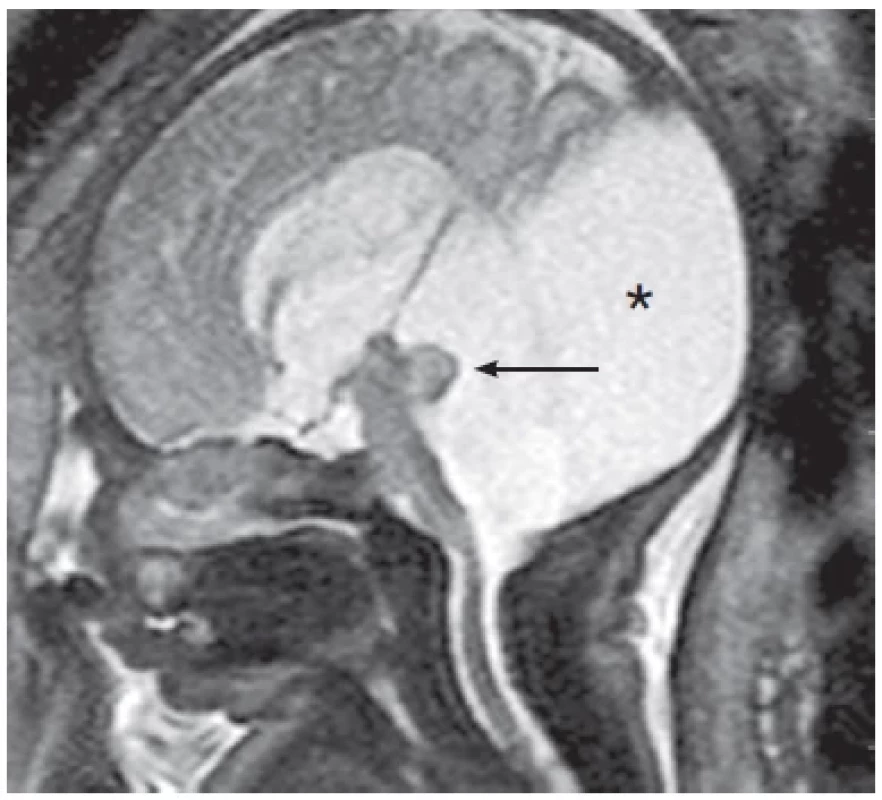
One of the most common fetal neurological indications is ventriculomegaly, which is defined as ventricles measuring more than 10mm in axial plane on US. MRI allows an accurate measurement of the lateral ventricles which is challenging by ultrasound, especially in the third trimester due to bone shadowing from the skull. It allows a better evaluation of the brain parenchyma and may reveal additional serious abnormalities such as migrational abnormalities, parenchymal or intraventricular hemorrhage, lissencephaly, Chiari malformations, agenesis of the corpus callosum.(7) Fetal MRI enables to evaluate the process of neuronal migration, to assess the lamination of brain structure (accurate visualization of the ventricular zone, subcortical plate, and cortex) and gyrification at different gestational stages.
Various MRI sequences are being developed to further evaluate the structures of the fetal brain. Among others, magnetic resonance spectroscopy (MRS), diffusion tensor imaging (DTI), perfusion imaging, functional magnetic resonance imaging (fMRI) and susceptibility weighted imaging (SWI), combined with higher clinically applicable static magnetic field strengths have provided new insights into brain development.(8)
Fetal MRI plays a crucial role in the evaluation of neural tube defects and is required for planning of corrective surgery in utero.
Fetal body indications
MRI plays an increasingly important role in the prenatal diagnosis of fetal body pathology and provides detailed information about fetal respiratory, gastrointestinal, and genitourinary systems. Fetal MRI should be offered when US cannot provide certain information crucial for pregnancy course, delivery plan and postnatal management. The most common fetal body indications are diaphragmatic hernia, and bronchopulmonary malformations in the chest, fetal bowel obstruction, esophageal atresia, omphalocele, bladder exstrophy, lower urinary tract obstruction, various abdominal masses, and vascular malformations (Fig. 2, Fig. 3).(9) The choice of the magnet intensity (1.5 versus 3 Tesla magnet) for body indications is based on several factors. Although 3 T offers a better signal to noise ratio, it is also associated with worsening of the number of artifacts and therefore, in patients with advanced gestational age or with polyhydramnios, 1.5 T magnet may be more suitable for fetal imaging.
Fig. 2. A 40-week-old fetus with no prenatal care presents with a large left hemidiaphragmatic hernia. A – Coronal Fast Image Employing Steady State Acquision (FIESTA ) image demonstrating the absence of the left hemidiaphragm with partial herniation of the liver, colon, and small bowel loops in to the left hemithoracic cavity (arrow) causing mediastinal shift towards the left. B – Coronal Liver Acceleration Volume Acquisition (LAVA, T1-weighted) image demonstrating herniated meconium-filled colon within the left hemithoracic cavity (meconium has high T1 signal) (arrow). C – Axial FIESTA image demonstrating fluid-filled small bowel loops in the left hemithoracic cavity and displaced mediastinal structures towards the right; a portion of the right lung can be partially seen in this image (arrow). 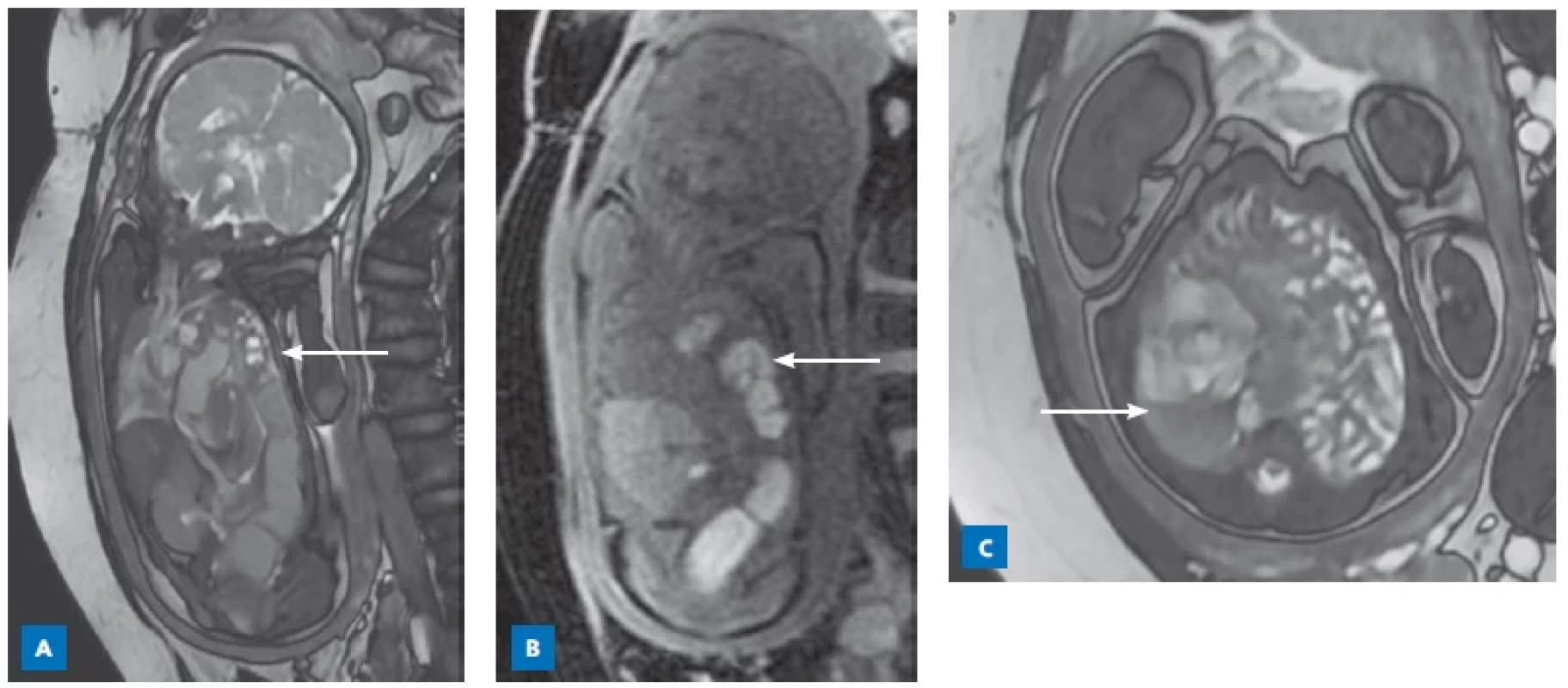
Fig. 3. A 22-week-old fetus with a giant omphalocele. The sagittal Single Shot Fast Spin Echo (SSFSE) image at the midline demonstrates herniation of the liver (arrow) through the anterior abdominal wall. A thin membrane can be clearly seen covering the herniated liver, which is characteristic of an omphalocele. 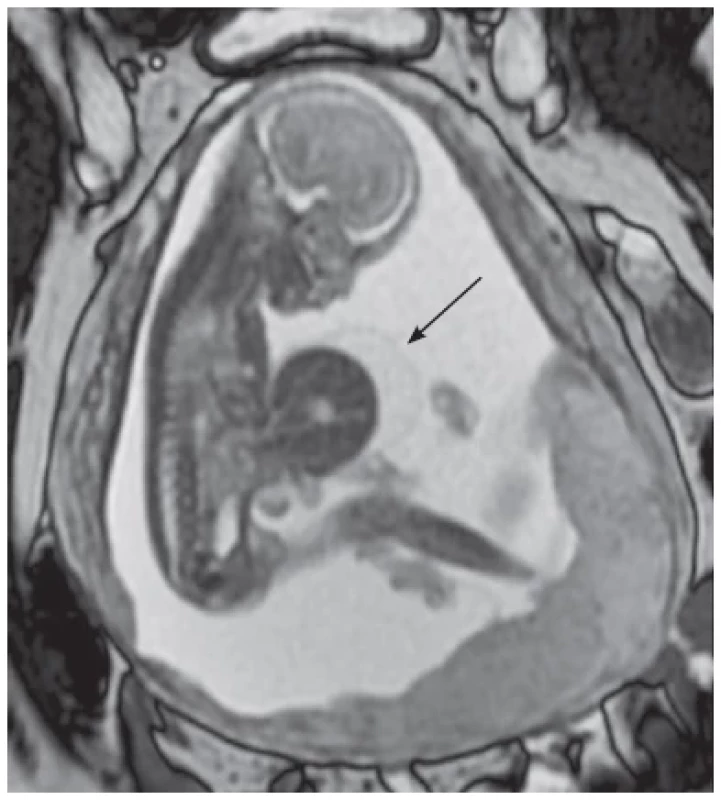
Fetal chest anomalies
Thanks to its tissue contrast superior to ultrasound, fetal MRI can delineate and characterize various chest masses. In diaphragmatic hernia, it allows the calculation of the volumes of herniated organs and of the lung volumes, which helps to establish the prognosis of neonatal outcome.(10)
Bronchopulmonary malformations (BPM) refer to a spectrum of pulmonary developmental anomalies that include congenital pulmonary airway malformation (CPA M), bronchopulmonary sequestration (BPS), congenital lung overinflation (CLO) and hybrid lesions (Fig. 4).(11) With advanced gestational age, the BPM are more difficult to visualize by ultrasound because of the increase in lungs echogenicity. Fetal MRI allows to visualize the BPM throughout pregnancy and helps to characterize the type of BPM. Characterizing the BPM lesions may impact the postnatal management process, such as surgical removal or imaging follow up, as well as parental counseling.
Fig. 4. A 25-week-old fetus with bronchopulmonary sequestration of the left lung. A coronal T2-weighted Single-Shot Turbo Spin Echo (SSTSE) sequence at 1.5-T MRI demonstrate bronchopulmonary sequestration with anomalous arterial supply (arrow). 
Finally fetal MRI is very useful to establish patency of airways in the setting of neck masses or airway obstruction and for the planning of fetal surgeries and EXIT procedures. Fetal abdominal anomalies Meconium is characterized by a high signal on T1-weighted images, which is due to its high content in fat and bile salts and accumulates within the colon. The rectum acts as a reservoir and can be visualized on MRI already in the early second trimester. The distribution pattern of meconium helps with the diagnosis and location of bowel obstruction (Fig. 5). The presence of a microcolon indicates a distal obstruction such as distal ileal atresia or meconium ileus in the setting of cystic fibrosis.
Fig. 5. A 35-week-old fetus with colonic atresia. A coronal T1-weighted Spin Echo (SE) sequence at 1.5T MRI shows subhepatic bowel dilatation, hyperintense meconium signal in the intestinal lumen (arrow). 
Fetal MRI provides better visualization of renal structural and positional abnormalities and may provide additional information in cases of hydronephrosis and subsequent renal changes such as subcortical cysts in the setting of obstructive dysplasia.
Fetal MRI is a complementary imaging method for the evaluation of urogenital and anorectal malformations (ARMs), which represent a complex group of anomalies.(12) Fetal MRI better than ultrasound determines the localization of the distal rectum and a fluid filled rectum with calcified meconium pellets is an indication of anal atresia with urorectal fistula in male or a cloaca in female fetuses. Fluid filled rectum is always abnormal and may reflect an ARM or an abnormality of meconium formation such as fetal diarrhea.
Other indications for fetal MRI are congenital abdominal cysts such as ovarian, mesenteric, renal or duplication cysts. MRI is helpful to evaluate the origin of the cyst, as well as its relationship to the surrounding organs.
Musculoskeletal malformation
Although the indications for fetal MRI have been somewhat limited for musculoskeletal abnormalities, MRI has been shown to be useful in the setting of arthrogryposis, or to establish lung volumes in the setting of severe skeletal dysplasia. Further applications of fetal MRI for the imaging of extremities are still under investigation.
Fetal MRI in practice
Fetal MRI is performed as soon as possible after sonographic diagnosis of an abnormality to give the parents early counseling and the opportunity to terminate a pregnancy where the fetus may be severely affected. Some MRI’s may be performed or repeated mid-third trimester in order to plan the delivery and postnatal management. In many cases, third trimester fetal MRI may replace or delay postnatal imaging that requires neonatal anesthesia or radiation exposure.
Fetal MRI can be performed safely on both 1.5 and 3 tesla MR magnets.(13) Various practices exist in different institutions. Accurate assessment of fetal anomalies requires a good knowledge of the imaged problem. Good communication between the referring physician and the radiologist is therefore key. At most institutions, the patient has a same day ultrasound performed by the same radiologist interpreting the fetal MRI to reassess the findings and to prioritize the imaging of the fetal body region and choose the sequences that are relevant to the underlying diagnosis. In order to decrease fetal motion, patients may be instructed to avoid eating and consuming beverages with high sugar or caffeine content two hours before the MRI. The patients are routinely screened for MRI-unsafe materials in their bodies, such as metals, non-MRI compatible pacemakers, etc. The patient is placed in the supine position. A surface coil is then placed on the abdomen. The average total time for the procedure is variable based on the fetal motion but is usually performed within 30 minutes.
Conclusion
Fetal MRI plays a pivotal role in diagnosis of some of the most challenging and complex fetal abnormalities. Several of the severe fetal anomalies are occult on ultrasound, and the ability to diagnose them on the MRI has paved the way for novel treatment options such as fetal surgery in select diagnoses.
The corresponding author:
MUDr. Martin Kynčl, Ph.D.
Klinika zobrazovacích metod 2. LF UK a FN v Motole
V Úvalu 84
150 06 Praha 5
martin.kyncl@fnmotol.czCes-slov Pediat 2023; 78(2): 91–95
Zdroje
1. Campbell S. A short history of sonography in obstetrics and gynaecology. Facts Views Vis Obgyn 2013; 5(3): 213–229.
2. Rubesova E, Barth R. Advances in fetal imaging. Am J Perinatol 2014; 31(07): 567–76.
3. Prayer D, Malinger G, Brugger PC, et al. ISUOG Practice Guidelines: performance of fetal magnetic resonance imaging. Ultrasound Obstet Gynecol 2017; 49(5): 671–80.
4. Colleran GC, Kyncl M, Garel C, Cassart M. Fetal magnetic resonance imaging at 3 Tesla — the European experience. Pediatr Radiol 2022; 52(5): 959–70.
5. Cassart M, Garel C. European overview of current practice of fetal imaging by pediatric radiologists: a new task force is launched. Pediatr Radiol [Internet]. 2020 Jun 18 [cited 2020 Oct 17]. Available from: http://link.springer. com/10.1007/s00247-020-04710-4
6. Coakley FV, Glenn OA, Qayyum A, et al. Fetal MRI: A developing technique for the developing patient. Am J Roentgenol 2004; 182(1): 243–52.
7. Barzilay E, Bar-Yosef O, Dorembus S, et al. Fetal brain anomalies associated with ventriculomegaly or asymmetry: An MRI-based study. AJNR Am J Neuroradiol 2017; 38(2): 371–5.
8. Tocchio S, Kline-Fath B, Kanal E, et al. MRI evaluation and safety in the developing brain. Seminar Perinatol 2015; 39(2): 73–104.
9. Saleem SN. Fetal MRI: An approach to practice: A review. J Adv Res 2014; 5(5): 507–23.
10. Niemiec SM, Louiselle AE, Phillips R, et al. Third-trimester percentage predicted lung volume and percentage liver herniation as prognostic indicators in congenital diaphragmatic hernia. Pediatr Radiol [Internet]. 2022 Oct 27 [cited 2022 Nov 13]. Available from: https://link.springer.com/10.1007/ s00247-022-05538-w
11. Barth RA. Imaging of fetal chest masses. Pediatr Radiol 2012; 42(S1): 62 – 73.
12. Alamo L, Meyrat BJ, Meuwly JY, et al. Anorectal malformations: finding the pathway out of the labyrinth. RadioGraphics 2013; 33(2): 491–512.
13. Victoria T, Jaramillo D, Roberts TPL, et al. Fetal magnetic resonance imaging: jumping from 1.5 to 3 tesla (preliminary experience). Pediatr Radiol 2014; 44(4): 376–86.
Štítky
Neonatologie Pediatrie Praktické lékařství pro děti a dorost
Článek vyšel v časopiseČesko-slovenská pediatrie
Nejčtenější tento týden
2023 Číslo 2- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Isoprinosin je bezpečný a účinný v léčbě pacientů s akutní respirační virovou infekcí
- Syndrom Noonanové: etiologie, diagnostika a terapie
-
Všechny články tohoto čísla
- Severe combined immunodeficiencies
- Myocarditis and cardiomyopathy
- Current pharmacotherapy options in pediatric obesity
- Pediatrička Lenka Ťoukálková: Jsem týmová hráčka
- doc. MUDr. Michal Hladík, PhD., slávi 70 rokov
- Spomienka na veľkého pediatra – profesora Birčáka
- Pediatrická poezie
- Josef Čapek: Česající se
- Co jsme psali
- Wilhelm Conrad Röntgen (1845–1923): Sto let poté
- Hybrid imaging PET/MRI in pediatric patients
- Modern anatomical imaging in pediatric cardiology using CT angiocardiography and 3D virtual heart models
- Preparation of the child for the magnetic resonance examination
- Fetal MRI – a brief update on current imaging and indications
- Prenatal diagnosis of ovarian cysts, management and pregnancy outcomes
- Česko-slovenská pediatrie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Myocarditis and cardiomyopathy
- Prenatal diagnosis of ovarian cysts, management and pregnancy outcomes
- Preparation of the child for the magnetic resonance examination
- Current pharmacotherapy options in pediatric obesity
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



