-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
DETERMINATION OF FACTORS ASSOCIATED WITH LONG-TERM ENDOTHELIAL LOSS AND REFRACTIVE RESULT IN PATIENTS WITH ARTISAN PHAKIC LENS
DETERMINATION OF FACTORS ASSOCIATED WITH LONG-TERM ENDOTHELIAL LOSS AND REFRACTIVE RESULT IN PATIENTS WITH ARTISAN PHAKIC LENS
Purpose: To determine the changes in endothelial cell density, refractive results, and risk factors associated with endothelial loss in patients with irisclaw phakic intraocular lenses for myopia/myopic astigmatism (Artisan).
Methodology: Data collection was obtained from an existing database with information on patients with a phakic Artisan lens implant between 1998 and 2011 at the Virgilio Galvis Ophthalmology Centre, with at least 5 years of follow-up. As a second stage, an analysis was carried out to identify the change in endothelial cell density and its potential associated factors.
Results: A total of 80 eyes with myopic errors were included with a follow-up of 11.9 + 3.48 years. The percentage of total loss of endothelial cells was greater than 25% of the preoperative density in 43.8% of the eyes. A postoperative annual loss > 1.6% was found in 47.0% of the eyes with that information available. 41 eyes (51%) had final endothelial density < 2000 cells/mm2, and 7 (8.8%) eyes had endothelial cell density < 1000 cells/mm2. Among the variables studied, no associated factors for long-term endothelial loss were found. During the course of the study, 8 (10%) phakic intraocular lenses were explanted, including 3 with accelerated endothelial loss, and another 2 with cataract associated and a significantly low endothelial density. The last mean spherical equivalent was -0.81 (±1.01 D), and the final uncorrected distance visual acuity was 0.45 logMar (Snellen 20/56).
Conclusion: Artisan-type phakic lenses are a good alternative for the correction of high myopic defects, with predictable refractive results in the long term. However, there is an increased loss of endothelial cells in the long term in a high percentage of patients. Strict postoperative follow-up, including endothelial evaluation, is required, and further studies are warranted.
Klíčová slova:
Refractive surgery – intraocular phakic lens – loss of endothelial cells – corneal oedema – corneal endothelium
Authors: LC. Martinez 1,3; A. Tello 2,3,4,6; V. Galvis 2,3,4,6; SJ. Villamizar 4,5,6; DV. Nova 3
Authors place of work: Department of Ophthalmology, Universidad Industrial de, Santander Bucaramanga, Santander, Colombia 1; Department of Anterior Segment, Fundación Oftalmológica, Santander FOSCAL, Floridablanca, Santander, Colombia 2; Department of Ophthalmology, Fundación Oftalmológica, Santander FOSCAL, Floridablanca, Santander, Colombia 3; Centro Oftamológico Virgilio Galvis, Floridablanca, Santander, Colombia 4; Department of Epidemiology. Centro Oftamológico Virgilio Galvis, Floridablanca, Santander, Colombia 5; Department of Ophthalmology, Universidad Autónoma de, Bucaramanga, Bucaramanga, Colombia 6
Published in the journal: Čes. a slov. Oftal., 78, 2022, No. 4, p. 188-195
Category: Původní práce
doi: https://doi.org/10.31348/2022/21Summary
Purpose: To determine the changes in endothelial cell density, refractive results, and risk factors associated with endothelial loss in patients with irisclaw phakic intraocular lenses for myopia/myopic astigmatism (Artisan).
Methodology: Data collection was obtained from an existing database with information on patients with a phakic Artisan lens implant between 1998 and 2011 at the Virgilio Galvis Ophthalmology Centre, with at least 5 years of follow-up. As a second stage, an analysis was carried out to identify the change in endothelial cell density and its potential associated factors.
Results: A total of 80 eyes with myopic errors were included with a follow-up of 11.9 + 3.48 years. The percentage of total loss of endothelial cells was greater than 25% of the preoperative density in 43.8% of the eyes. A postoperative annual loss > 1.6% was found in 47.0% of the eyes with that information available. 41 eyes (51%) had final endothelial density < 2000 cells/mm2, and 7 (8.8%) eyes had endothelial cell density < 1000 cells/mm2. Among the variables studied, no associated factors for long-term endothelial loss were found. During the course of the study, 8 (10%) phakic intraocular lenses were explanted, including 3 with accelerated endothelial loss, and another 2 with cataract associated and a significantly low endothelial density. The last mean spherical equivalent was -0.81 (±1.01 D), and the final uncorrected distance visual acuity was 0.45 logMar (Snellen 20/56).
Conclusion: Artisan-type phakic lenses are a good alternative for the correction of high myopic defects, with predictable refractive results in the long term. However, there is an increased loss of endothelial cells in the long term in a high percentage of patients. Strict postoperative follow-up, including endothelial evaluation, is required, and further studies are warranted.
Keywords:
refractive surgery – intraocular phakic lens – loss of endothelial cells – corneal oedema – corneal endothelium
INTRODUCTION
Patients with high refractive errors (myopia, hyperopia and high astigmatism) or with corneal pathologies, such as advanced keratoconus, among others, are not suitable for refractive correction with Excimer laser or glasses, a fact that has led to the search for alternatives in their treatment. In the last two decades, the placement of phakic intraocular lenses fixed in the iris (such as the iris-claw Artisan lens) has been indicated as a surgical alternative for refractive correction in these patients.
The number of patients in whom the Artisan lens has been implanted has increased progressively in recent decades, leading to the need for studies of refractive results and possible complications secondary to its use. Good visual results and safety have been found in short - and mid-term follow-up studies. However, on the other hand, few studies have been done on the long-term outcomes (10 years or more), in terms of possible late postoperative complications (including corneal endothelial loss). Endothelial cells are responsible for maintaining the cornea in a stable state of hydration; the density of these endothelial cells is thus critical for that function. Any type of surgical procedure that is performed in the anterior chamber involves some type of trauma to these cells and leads to a decrease in their population. For this reason, it is important to estimate the percentage of endothelial cell loss after implantation of phakic iris-claw intraocular lenses. Considering that this procedure is done in young adults, long-term studies are critical to determine the continuous loss of endothelial cells related to the surgery and the phakic intraocular lens presence, which is added to the normal loss secondary to aging.
For this reason, in this study we aim to evaluate the refractive results after the implantation of phakic iris-claw intraocular lenses, and to investigate the main factors associated with the loss of endothelial cells in the long term.
MATERIALS AND METHODS
Study design and patient population
This was a descriptive, longitudinal, retrospective, observational study. The study group included patients who had undergone implantation of phakic iris-claw intraocular lenses (Artisan) at Virgilio Galvis Ophthalmological Centre from 1998 to 2012 in Floridablanca (Colombia). Inclusion criteria were age older than 18 years; preoperative transparent cornea; preoperative measurement of the anterior chamber (from the endothelium) > 2.9 mm; presurgical endothelial count greater than 2000 cells/mm2 and postoperative follow-up for at least 5 years.
Exclusion criteria included patients with previous intraocular surgery; patients with ocular past history of ocular conditions, such as retinopathies, glaucoma, uveitis, and Fuchs endothelial dystrophy.
Variables studied
The collection of information on the variables was obtained from an existing database with information on patients who had an iris-claw phakic intraocular lens implanted between 1998 and 2012 at the Virgilio Galvis Ramírez Ophthalmological Centre. The information was handled with codes, in order to be anonymous. Variables analysed included: follow-up time in years, age, gender, eye, visual acuity, subjective refraction, endothelial cell density (Tomey EM-1000 or Topcon SP-3000P devices), power of the implanted lens, model of the implanted lens, and surgeon. In addition, the following variables were analysed, if available: preoperative depth of the anterior chamber (measured with Visante® or Orbscan IIZ® devices), postoperative distance in microns from the centre of the lens to the endothelium, and distance in microns from the most nasal and temporal border of both haptics to the endothelium (MS-39 device); preoperative (measured with Orbscan or Visante devices) and postoperative pachymetry (measured with Orbscan, Visante or MS-39 devices).
Data were collected with the R version 4.1.1 program to perform the statistical analysis.
Analysis of the endothelial cell density was performed as follows:
Total corneal endothelial cell loss was determined by comparing the last corneal endothelial density with respect to the preoperative one, thus including the endothelial cell loss related to the surgical trauma, age, and that related to the presence of the iris-claw phakic intraocular lens in the anterior chamber.
Endothelial cell loss directly related to the surgical procedure was determined by comparing the presurgical density versus the postoperative one, obtained at 6 months or earlier, after surgery.
Finally, progressive endothelial cell loss after surgery, excluding surgical trauma, was determined by comparing endothelial cell density in an examination at least 6 months after surgery with the last examination available. Both examinations should have been undertaken with the same specular microscope.
The physiological annual loss of cell density was considered abnormal if it was above 1.6% of annual loss, calculated as 2 standard deviations higher than the mean in the longitudinal study by Bourne et al. [1].
The corrected distance visual acuity and refractive result (performed by an optometrist) of each patient in the preoperative period was used, to compare it with the visual acuities and refractions in the postoperative period at 6 months after the procedure, and every year thereafter. In the database, they were reported in Snellen notation (which is how they are measured in the clinical examination) and converted to LogMar notation for statistical calculation, and the refraction data reported by optometry.
The measurement of distances in microns from the optics and haptics of the phakic iris-claw intraocular lens to the endothelium was performed, using the MS-39 Tomograph and Topographer. An analysis was performed to identify the presence of associated factors with endothelial cell loss.
Statistical analysis
In the descriptive analysis, the measures of central tendency and dispersion of the quantitative variables were estimated according to the frequency distribution. Regarding the univariate analysis, the nominal qualitative variables were presented in proportions, the ordinal ones were presented in medians, the numerical ones were presented in averages or medians, and standard deviation or interquartile range according to their normality. The possible relationship between them was evaluated, using the Chi Square test according to the frequency distribution. Subsequently, a correlation analysis was done between the number of endothelial cells/years, which made it possible to identify potential losses associated with the procedure, independent of endothelial loss due to age.
In addition, with the variables of total loss, loss due to surgical trauma, and percentage of annual loss, a multiple regression was performed that included the quantitative variables of the different distances from the lens to the endothelium and pachymetry. For the statistical analysis, an alpha of 0.05 was used and the R version 4.1.1 program was used.
RESULTS
Regarding the demographic data of the population, data were obtained from a total of 80 eyes of 52 patients, with 77% of patients being female. Mean follow-up time was 11.73 years, ranging from 5.3 to 18.5 years. 68.7% of the eyes had at least 10 years of postoperative follow-up. All the patients had a pre-surgical myopic defect. 10 toric lenses and 70 spherical lenses were included in the study (Table 1).
Tab. 1. Baseline characteristics of patients and eyes 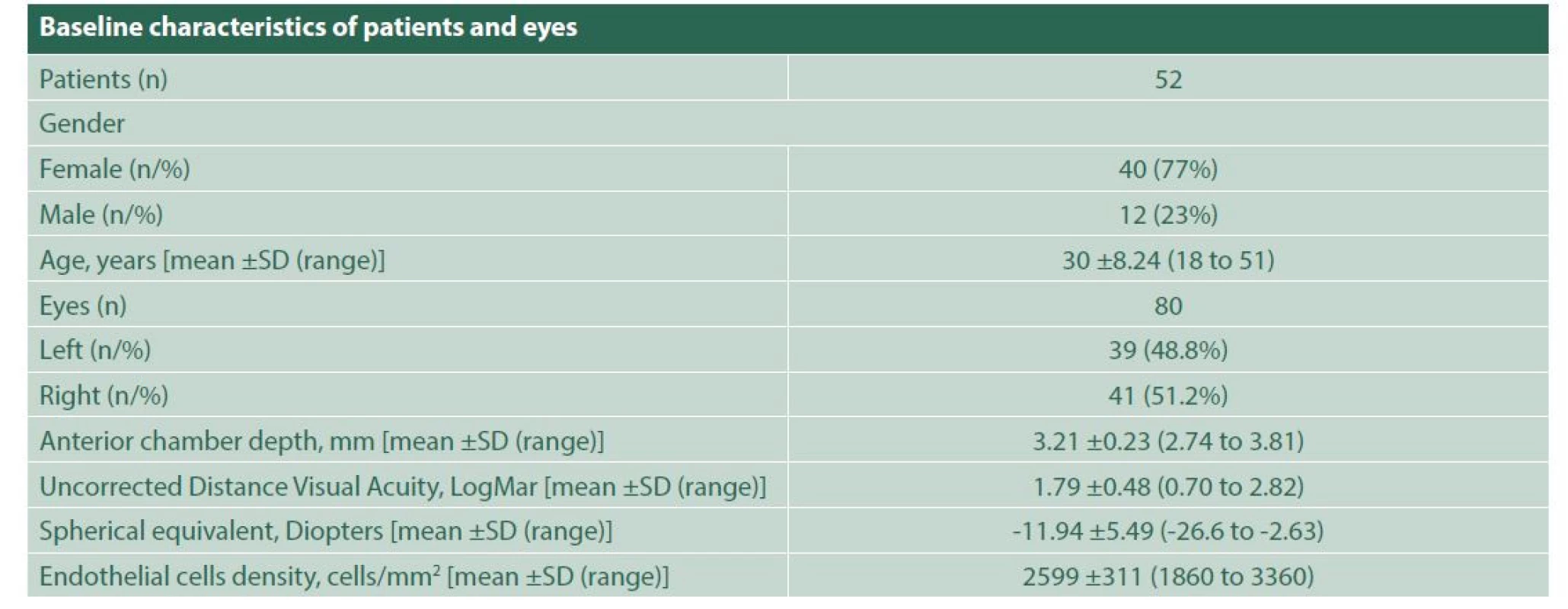
SD – Standard deviation At the last follow-up, total endothelial cell loss was greater than 25% in 43.8% of eyes. An annual percentage of loss > 1.6% was found in 31 eyes at the last follow-up (47.0% of the eyes with that information available), with a maximum value of annual endothelial loss of 13.9%. As final endothelial count, 41 eyes (51%) had endothelial counts < 2000 cells/mm2; of these, 7 eyes had endothelial cell counts < 1000 cells/mm2 (Table 2).
Tab. 2. Corneal endothelial cell loss and density at the last follow up examination 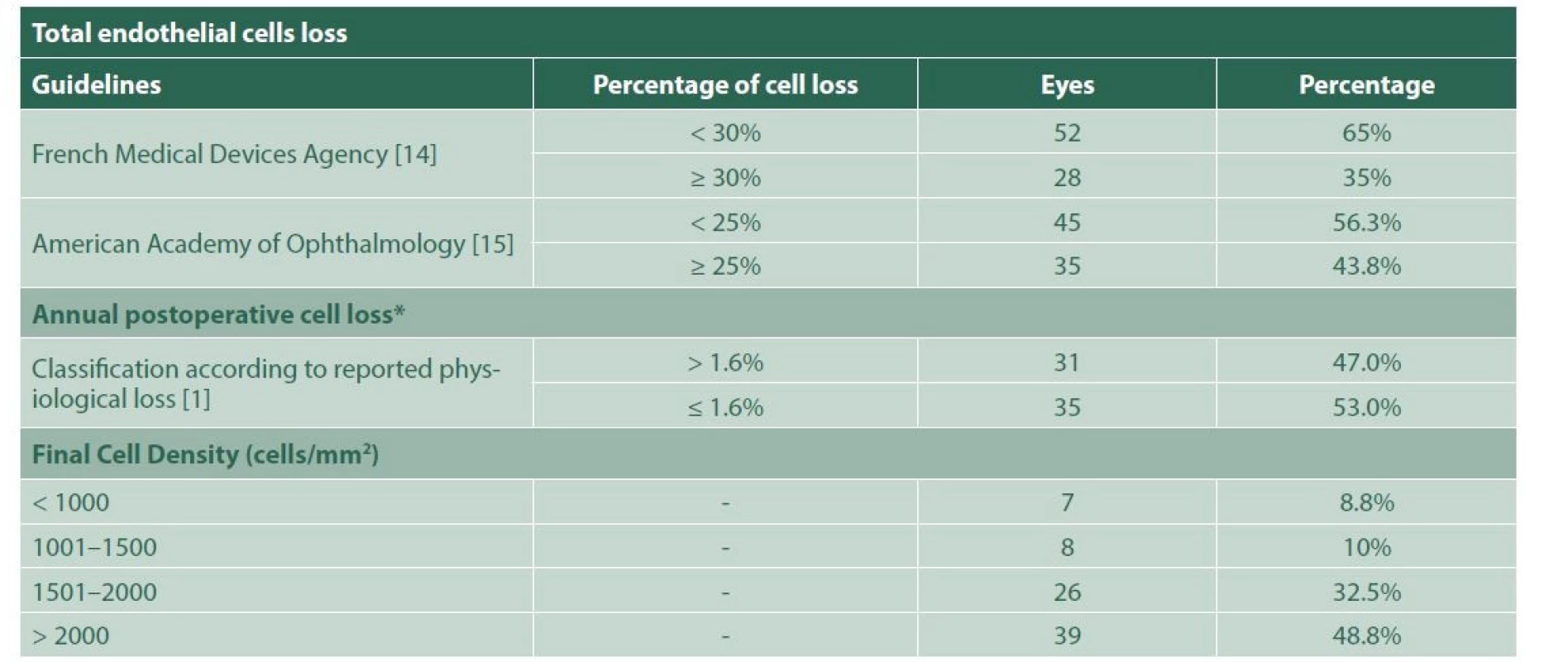
* Calculated excluding cell loss related to surgical trauma The measurements of the distances of different parts of the phakic intraocular lenses to the corneal endothelium (Figure 1) yielded an average distance of 2.23 ±0.24 mm from the centre of the lens optic; 1.79 ±0.30 mm from the nasal edge of the optic to the endothelium; 1.94 ±0.29 mm from the temporal edge of the optic to the endothelium; 1.26 ±0.29 mm from the nasal edge of the haptic of the intraocular lens to the endothelium; and 1.41 ±0.29 mm from the nasal edge of the haptic of the intraocular lens to the endothelium.
Figure 1. In A) Optic Coherence Tomography of the anterior segment (MS-39, CSO) showing the distances from the optic, from the nasal and temporal edges of the optic, and from the haptics of the phakic iris-claw intraocular lens (ARTISAN) to the endothelium. B) and C) Slit lamp photographs of the anterior segment of a patient with the phakic iris-claw intraocular lens (ARTISAN) 
Mean preoperative sphere was -11.00 ±5.68 Dioptres (D); mean preoperative cylinder was -1.86 ±1.29 D; and mean preoperative Spherical Equivalent was -11.94 ±5.49 D. The mean preoperative uncorrected distance visual acuity was 1.79 LogMAR (Snellen 20/1230). In the last postoperative visit, the mean sphere was -0.73 ±2.01 D; mean postoperative cylinder was -1.12 ±0.84 D; mean postoperative spherical equivalent was -0.81 ±1.01 D. Postoperative data in 5 eyes were not considered, due to the presence of cataract at the last follow-up. Defocus equivalent was obtained (calculated as the numerical value of the absolute value of the spherical equivalent, plus half the absolute value of the refractive cylinder). Mean postoperative Defocus Equivalent was 1.40 ±1.1 D (range from 0 to 1.75 D).
Mean Distance Uncorrected Visual Acuity was 0.45 LogMar (Snellen 20/56) at the last follow-up visit. The cumulative percentages of eyes within a range of spherical equivalent, refractive cylinder, and postoperative defocus are shown in Table 3.
Tab. 3. Final postoperative refraction according to spherical equivalent, cylinder and defocus equivalent 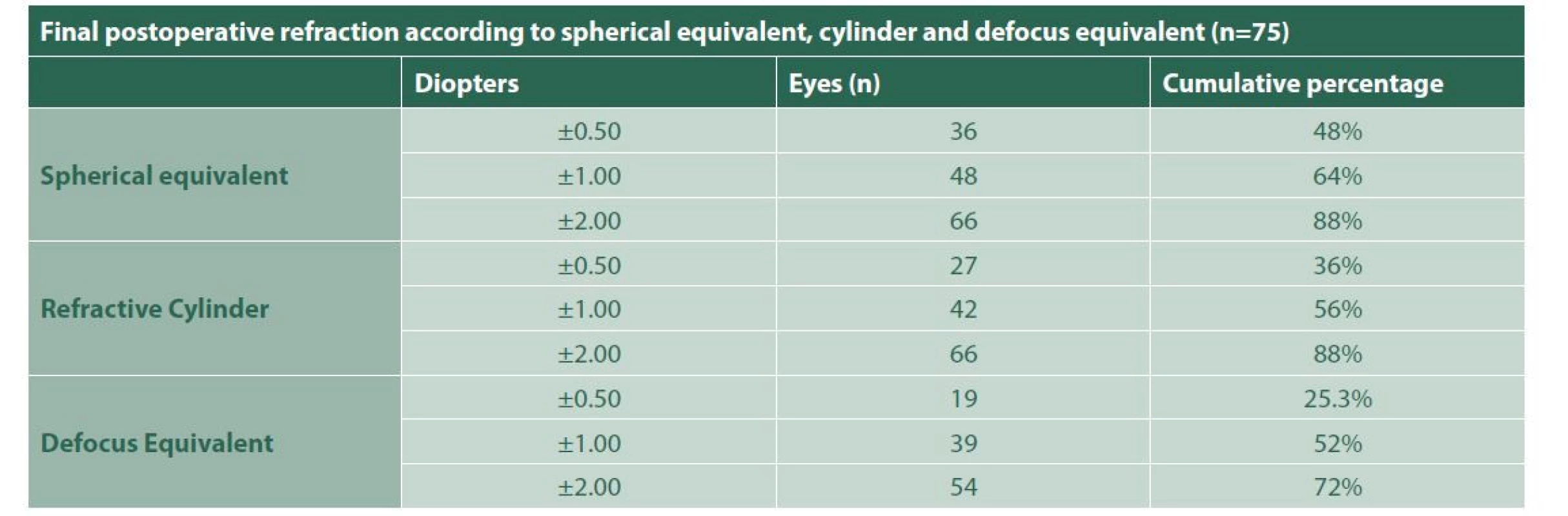
The correlation between the variables (sex, age, presurgical anterior chamber measurement, presurgical endothelial count, optic and haptic distances from the endothelium) and annual endothelial loss, total endothelial cell loss and loss due to surgical trauma, in search of possible associations was not statistically significant in all variables (Tables 4–6).
Tab. 4. Correlation: Total Endothelial cells loss at the last follow up examination 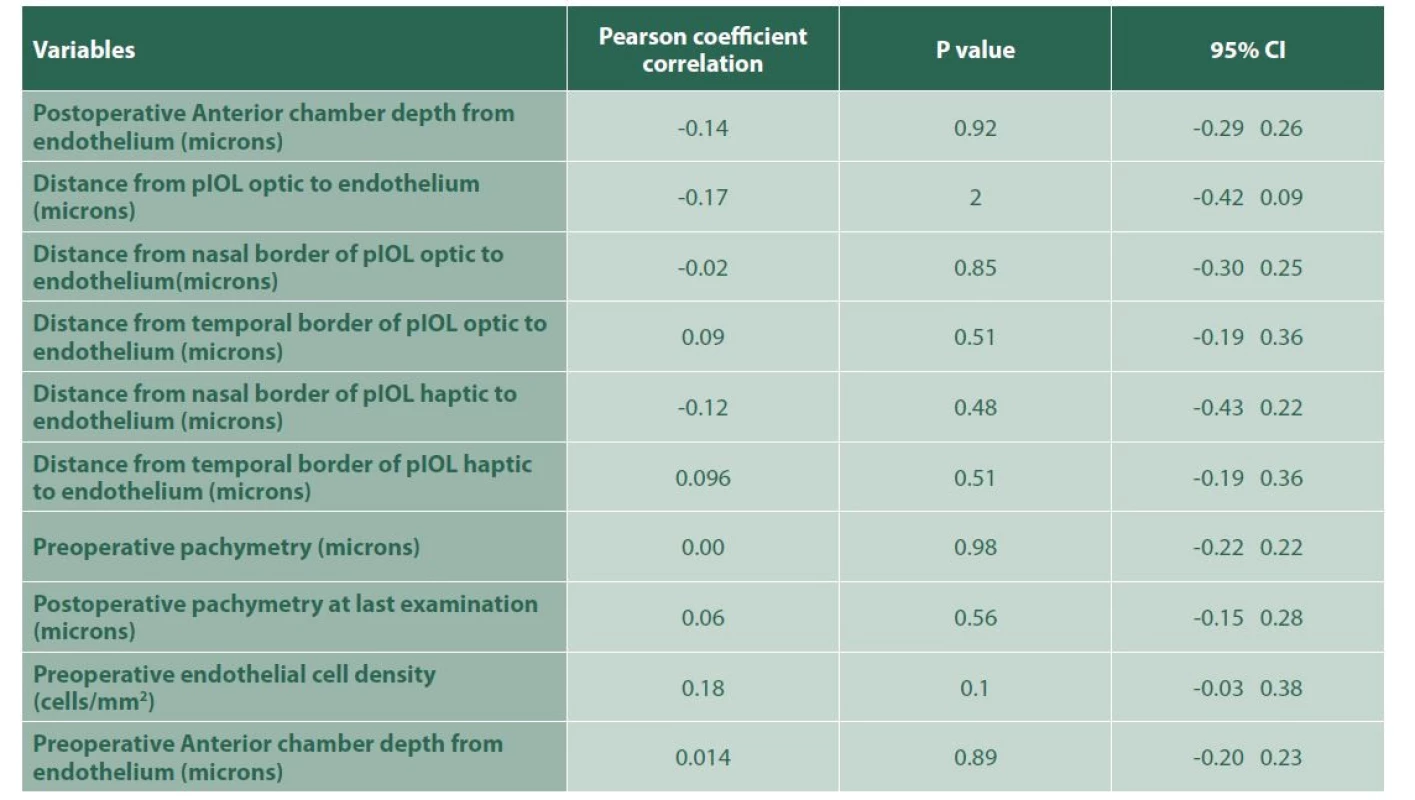
pIOL – Phakic intraocular lens, 95% CI – 95% confidence interval Tab. 5. Correlation: Annual Loss of Endothelial cells after surgery excluding surgical trauma 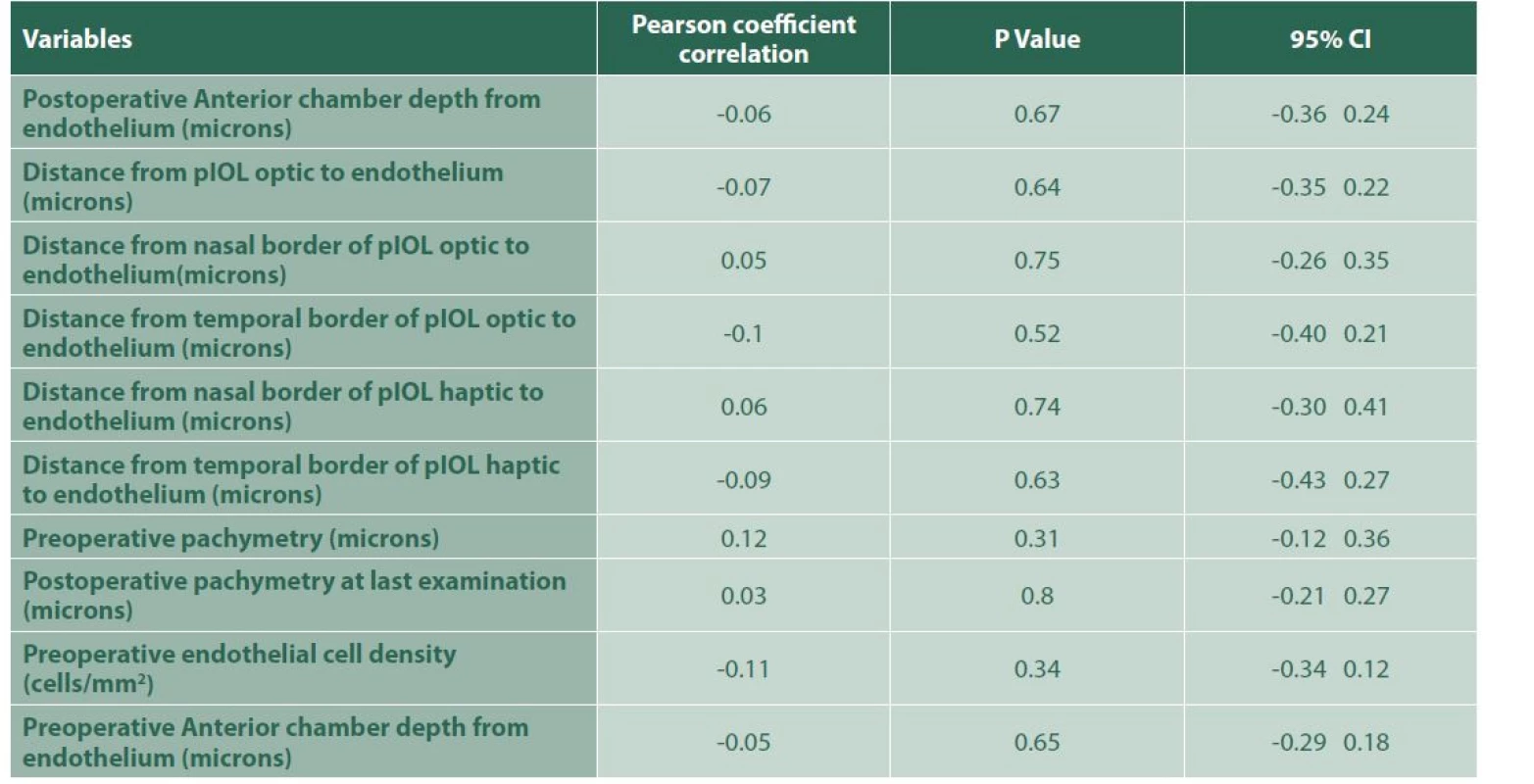
pIOL – Phakic intraocular lens, 95% CI – 95% confidence Tab. 6. Correlation: Endothelial cell loss related to surgical trauma 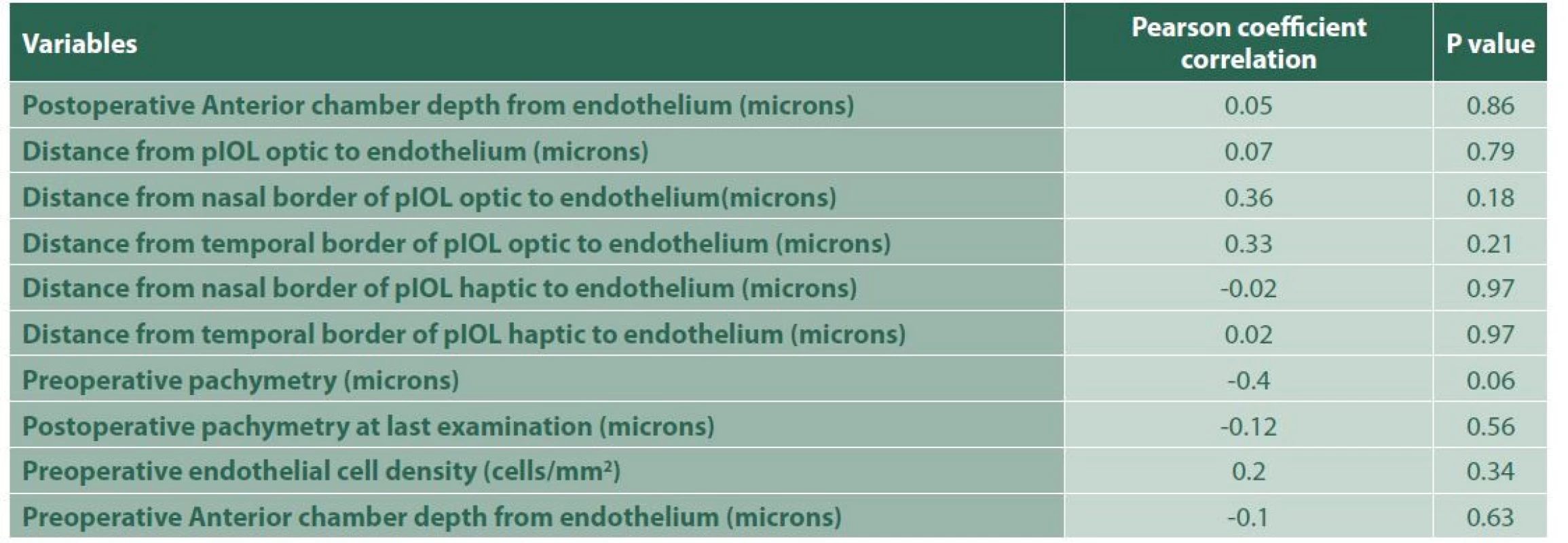
pIOL – Phakic intraocular lens Finally, with the variables total endothelial loss and percentage of annual postoperative loss, a multiple regression was carried out that included the quantitative variables of distance between the lens and the endothelium, presurgical endothelial count, age and pachymetry, in order to identify associated risk factors of postoperative endothelial cell loss. However, no significant results were found in the regression model. Regarding endothelial loss due to surgical trauma, it was found that, as pre-surgical pachymetry increased, endothelial loss decreased by 2.3% (95% CI -4.22. -0.49) (p=0.02) (Table 7). No linear relationship was found between the distances from the intraocular lens to the endothelium and the total loss of endothelial cells or the percentage of postoperative annual loss.
Tab. 7. Multiple Regression Model: Loss of endothelial cells due to surgical trauma and pre-surgical pachymetry 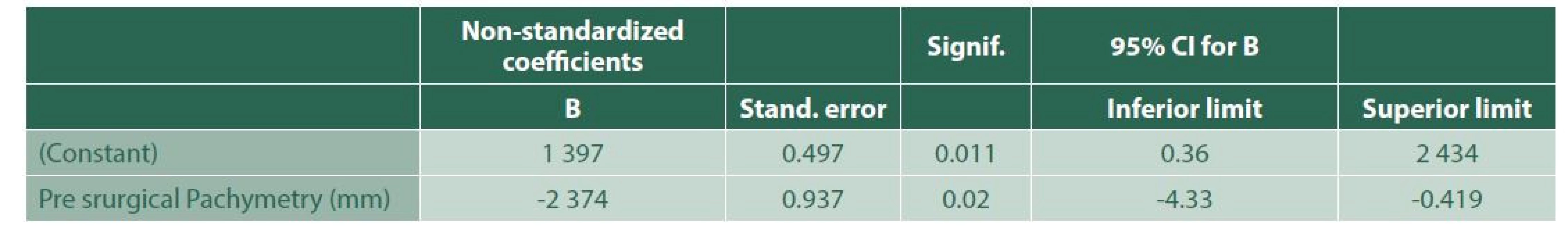
Stand. error – Standard error, Signif. – Significance, 95% CI – 95% confidence interval By the end of the follow-up period, a total of 8 iris-fixed phakic lenses were explanted, 5 of these having cataract as the first indication. However, of these, 2 had low endothelial cell count as the second indication, and 3 lenses were explanted due to very low endothelial cell count, with a central cellular density between 791 and 887 cells/mm2. One patient’s eye required phakic lens repositioning after 6 years of implantation, due to subluxation.
DISCUSSION
The treatment of high refractive errors (myopia or hyperopia) has been a challenge in modern ophthalmology. Various studies have shown that the correction of high myopic errors with anterior chamber iris-claw phakic intraocular lenses (such as the Artisan and Verisyse) is predictable and has good stability in the short and medium term [2-6]; having similar results compared to posterior chamber phakic intraocular lenses (ICL) [7]. In our study, we obtained refractive results that remained stable in the majority of patients throughout the follow-up time, with a mean preoperative distance uncorrected visual acuity LogMar of 1.79 (Snellen 20/1230) vs. a postoperative distance uncorrected visual acuity with a mean of 0.45 Log - MAR (Snellen 20/56). Mean preoperative SE of -11.0 ±5.68 D improved to a final SE of -0.81 ±1.0 D.
However, there is concern due to the presence of long-term adverse effects, such as the accelerated loss of corneal endothelial cells that exceeds the annual physiological loss of 0.6% [1,8]. There are case reports in the literature of iris-claw phakic IOL explantation due to corneal decompensation or severe loss of endothelial cells [9,10]. In our group of 80 eyes, 8 lenses (10%) had to be explanted. In 5 cases, a cataract with impact on vision was found as the first indication for explant, in 2 of which there was, in addition, a significant decrease in endothelial cell density. In 3 other cases without cataract, a very significant decrease in endothelial cell density was found (with cell densities below 1000 cells/mm2), with an average follow-up of 12.6 years in these patients. Jonker et al., in their published longitudinal study with long-term follow-up, reported an iris-claw anterior chamber phakic lens explant rate of 6.1% due to low endothelial counts, a percentage which correlates with our study, where we obtained a 6.25% percentage of lenses explanted due to low endothelial count.
Most longitudinal studies available in the literature have shown medium-term follow-up results [11,12]. Few studies have reported long-term results > 5 years. In the predecessor study to this one, Galvis et al. found an endothelial cell loss percentage of 11.9% and 15.8% at 6 and 10 years, respectively. Jonker et al. reported results of endothelial loss in a group of 127 eyes, with a follow-up of up to 10 years, finding chronic postoperative endothelial loss, excluding that caused by surgical trauma of the lens implant, with an annual loss percentage of 1.75%. and 2.27% per year in patients with spherical and toric Artisan implants, respectively [13]. In the present study, we obtained a postoperative average annual loss of 2%, excluding the percentage of endothelial cell loss due to surgical trauma, with 47.0% of the eyes, with such information available, having a percentage of annual loss >1.6% – data that also correlate with those of Galvis et al., where 2.14% endothelial loss per year was obtained, with a mean postoperative follow-up of 9.6 years.
In 2006, the French Medical Devices Agency recommended that, regarding endothelial evaluation in phakic lens cases, specular microscopy density should be performed every six months, and if greater than 30% endothelial loss was observed compared to preoperative cell density and/or a density of less than 1500 cells/mm2, intraocular lens explantation should be considered [14]. In 2017, the American Academy of Ophthalmology formulated guidelines regarding the follow-up of patients with phakic intraocular lenses, indicating that a total loss of endothelial cells > 25% compared to the presurgical count should be an evaluation criterion to consider intraocular lens explant and replacement. [15]. In the present study, we found that 28% of the eyes had a total loss of endothelial cells > 30% of the preoperative value, and 35% of the eyes had a loss > 25% of the preoperative value at the end of the follow-up. In addition, 18.8% of eyes presented endothelial cell density < 1500 cells/mm2. All these data allowed us to indicate that there was a significant loss of endothelial cells in patients after iris-claw phakic intraocular lens implantation, which exceeded the normal physiological limits.
In search of factors related to this accelerated loss of endothelial cells, various studies have sought associations and correlations with other anatomical factors as risk factors. Saxena et al. identified a significant negative correlation between the anterior chamber depth and postoperative endothelial cell loss [12]. However, some researchers have not detected such association, e.g. Bouheraroua et al. and Galvis et al. [8,16].
With the advent of new technologies in the last decade, for the present study we decided to perform measurements with a new Optical Coherence Tomographer for the anterior segment (the MS-39 tomograph/topographer), which allows good visualisation of different parts of the phakic intraocular lens. We therefore performed several measurements of the distance of different portions of the phakic intraocular lens to the endothelium. The distances from the haptics to the endothelium were found to be lower than the distances from other portions of the intraocular lens. A multiple regression was performed without detecting a relationship between these measurements and postoperative endothelial cell loss. Therefore, we could not identify any of these distances as a risk factor for endothelial cell loss in patients with iris-claw phakic intraocular lenses. In contrast, Doors et al. performed a measurement of the distance between the edge of the optic and the endothelium, obtaining an average of 1.43 mm, using the Visante OCT device. They found an association between the annual postoperative cell loss and this distance [17].
Recently, another variable has been included as a possible factor related to endothelial loss, i.e. preoperative pachymetry, based on the idea that a thinner cornea may have higher capacity to deform under mechanical pressure, compared to a thicker cornea, promoting increased phakic intraocular lens to endothelium contact. This factor would be important in the context mentioned in a previous study by Galvis et al., where they mentioned a possible extrinsic mechanical factor, such as ocular rubbing or ocular compression when sleeping, as a possible cause of chronic endothelial loss in these patients.[8] Nemcova et al., in their recently published study, found an inverse correlation between baseline pachymetry and endothelial cell loss with a 12-year follow-up [18]. In the present study, an association between central corneal thickness and postoperative endothelial cell loss was not detected. On the other hand, a multiple regression found that, for each millimetre that increased in presurgical pachymetry, the loss due to surgical trauma during lens implantation decreased by 2.37% on average. However, the plausibility of this association is not clear.
Finally, despite the presence of dozens of studies in the literature, there is still doubt concerning the long-term safety results regarding the effects that the presence of the iris-claw phakic intraocular lens in the anterior chamber may have. In the present study, as in a previous one by Galvis et al. in our institution [8], a fairly significant total and annual postoperative endothelial cell loss was found in a significant percentage of patients. One year ago, seeing this trend, we decided to abandon the implantation of iris-claw phakic intraocular lenses.
Finally, as no risk factor clearly associated with chronic endothelial loss was found in these patients, additional studies with larger samples and longer postoperative follow - up times are warranted.
CONCLUSION
After long-term follow-up, it was found that iris-claw phakic intraocular lenses are a good alternative for the correction of high myopic defects, with stable and predictable long-term refractive results. However, an unacceptable endothelial cell loss and postoperative annual percentage of significant loss were found. 18.8% of eyes had an endothelial count < 1500 cells/mm2 at the end of the follow-up period, 35% had a total loss > 25% and 47.0% had a postoperative annual loss > 1.6% – values that are found outside the limits proposed as safe in the available literature. In the present study, no evidence was found of risk factors related to long-term endothelial loss in patients with an iris-claw phakic Artisan intraocular lens.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceutical company. The study has not been submitted to any other journal or printed elsewhere.
Received: 15 February 2022
Accepted: 28 March 2022
Dr. Luz Cátherine Martínez Malo, MD
Avenida El Bosque No 23-60
Fundación Oftalmológica de Santander - FOSCAL Floridablanca
Santander, Colombia
E-mail: luzkmalo@gmail.com
Zdroje
1. Bourne WM, Nelson LIL, Hodge DO. Central corneal endothelial cell changes over a ten-year period. Investig Ophthalmol Vis Sci. 1997;38(3):779-782.
2. Fechner PU, Haigis W, Wichmann W. Posterior chamber myopia lenses in phakic eyes. J Cataract Refract Surg [Internet]. 1996 Mar [cited 2018 Apr 15];22(2):178-182. Available from: http://www. ncbi.nlm.nih.gov/pubmed/8656381
3. Lifshitz T, Levy J, Aizenman I, Klemperer I, Levinger S. Artisan phakic intraocular lens for correcting high myopia. Int Ophthalmol. 2005;25(4):233-238.
4. Landesz M, Worst JG, Siertsema J V, van Rij G. Correction of high myopia with the Worst myopia claw intraocular lens. J Refract Surg [Internet]. [cited 2018 Apr 15];11(1):16-25. Available from: http:// www.ncbi.nlm.nih.gov/pubmed/7641044
5. Benedetti S, Casamenti V, Benedetti M. Long-term endothelial changes in phakic eyes after Artisan intraocular lens implantation to correct myopia. Five-year study. J Cataract Refract Surg. 2007;33(5):784-790.
6. Stulting RD, John ME, Maloney RK, Assil KK, Arrowsmith PN, Thompson VM. Three-Year Results of Artisan/Verisyse Phakic Intraocular Lens Implantation. Ophthalmology [Internet]. 2008 Mar [cited 2018 Apr 15];115(3):464-472.e1. Available from: http://linkinghub. elsevier.com/retrieve/pii/S0161642007009578
7. Hassaballa MA, Macky TA. Phakic intraocular lenses outcomes and complications: Artisan vs Visian ICL. Eye. 2011;25(10):1365-1370.
8. Galvis V, Villamil JF, Acuña MF, et al. Long-term endothelial cell loss with the iris-claw intraocular phakic lenses (Artisan®). Graefe’s Arch Clin Exp Ophthalmol. 2019;257(12):2775-2787.
9. Güell JL, Morral M, Gris O, Gaytan J, Sisquella M, Manero F. Five - Year Follow-up of 399 Phakic Artisan-Verisyse Implantation for Myopia, Hyperopia, and/or Astigmatism. Ophthalmology. 2008;115(6):1002-1012.
10. Van Eijden R, de Vries NE, Cruysberg LPJ, Webers CA, Berenschot T, Nuijts RMMA. Case of late-onset corneal decompensation after iris-fixated phakic intraocular lens implantation. J Cataract Refract Surg [Internet]. 2009;35(4):774-777. Available from: http://dx.doi. org/10.1016/j.jcrs.2008.09.032
11. Shajari M, Scheffel M, Koss MJ, Kohnen T. Dependency of endothelial cell loss on anterior chamber depth within first 4 years after implantation of iris-supported phakic intraocular lenses to treat high myopia. J Cataract Refract Surg [Internet]. 2016;42(11):1562-1569.Available from: http://dx.doi. org/10.1016/j.jcrs.2016.08.027
12. Saxena R, Boekhoorn SS, Mulder PGH, Noordzij B, van Rij G, Luyten GPM. Long-term Follow-up of Endothelial Cell Change after Artisan Phakic Intraocular Lens Implantation. Ophthalmology. 2008;115(4):7-9.
13. Jonker SMR, Berendschot TTJM, Ronden AE, Saelens IEY, Bauer NJC, Nuijts RMMA. Long-Term Endothelial Cell Loss in Patients with Artisan Myopia and Artisan Toric Phakic Intraocular Lenses. 5 - and 10-Year Results. Ophthalmology [Internet]. 2017;(June 2016):1-9. Available from: http://dx.doi.org/10.1016/j.ophtha. 2017.08.011
14. Bernard P FM. Definitive stop of marketing, product recall and follow - up of implanted patients. Presbyopia intraocular lenses NEWLIFE/ VIVARTE PRESBYOPIC. Agence Française Sécurité Sanit des Prod Santé. 2006;8.
15. MacRae S, Holladay JT, Hilmantel G, et al. Special Report: American Academy of Ophthalmology Task Force Recommendations for Specular Microscopy for Phakic Intraocular Lenses. Ophthalmology [Internet]. 2017;124(1):141-142. Available from: http://dx.doi. org/10.1016/j.ophtha.2016.09.034
16. Bouheraoua N, Bonnet C, Labbé A, et al. Iris-fixated phakic intraocular lens implantation to correct myopia and a predictive model of endothelial cell loss. J Cataract Refract Surg. 2015 Nov;41(11):2450 - 2457. doi: 10.1016/j.jcrs.2015.05.030. PMID: 26703496.
17. Doors M, Cals DWJK, Berendschot TTJM, et al. Influence of anterior chamber morphometrics on endothelial cell changes after phakic intraocular lens implantation. J Cataract Refract Surg. 2008;34(12):2110-2118.
18. Nemcova I, Pasta J, Hladikova K, et al. Myopic Correction with Iris-Fixated Phakic Intraocular Lenses: Twelve-Year Results. J Ophthalmol. 2021;2021 Available from: https://doi. org/10.1155/2021/7027793
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2022 Číslo 4- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- VITAMIN D AND OPHTHALMOPATHIAS. A REVIEW
- ENDOPHTHALMITIS IN OPHTHALMOLOGICAL REFERRAL CENTRE IN COLOMBIA: AETIOLOGY AND MICROBIAL RESISTANCE
- EFFECT OF RANIBIZUMAB AND AFLIBERCEPT ON RETINAL PIGMENT EPITHELIAL DETACHEMENT, SUBRETINAL AND INTRARETINAL FLUID IN AGE-RELATED MACULAR DEGENERATION
- DETERMINATION OF FACTORS ASSOCIATED WITH LONG-TERM ENDOTHELIAL LOSS AND REFRACTIVE RESULT IN PATIENTS WITH ARTISAN PHAKIC LENS
- COINCIDENCE OF IDIOPATHIC INTRACRANIAL HYPERTENSION AND LEBER HEREDITARY OPTIC NEUROPATHY. A CASE REPORT
- EN BLOC RESECTION OF RETINAL VASOPROLIFERATIVE TUMOR USING 23G VITRECTOMY. A CASE REPORT
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- EN BLOC RESECTION OF RETINAL VASOPROLIFERATIVE TUMOR USING 23G VITRECTOMY. A CASE REPORT
- VITAMIN D AND OPHTHALMOPATHIAS. A REVIEW
- COINCIDENCE OF IDIOPATHIC INTRACRANIAL HYPERTENSION AND LEBER HEREDITARY OPTIC NEUROPATHY. A CASE REPORT
- EFFECT OF RANIBIZUMAB AND AFLIBERCEPT ON RETINAL PIGMENT EPITHELIAL DETACHEMENT, SUBRETINAL AND INTRARETINAL FLUID IN AGE-RELATED MACULAR DEGENERATION
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




