-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Lichen planus as a possible rare cause of an ocular disease
Authors: J. Nekolová 1; M. Středová 1; M. Podhola 2; N. Jirásková 1
Authors place of work: Oční klinika, Fakultní nemocnice v Hradci Králové, Sokolská 581, 50005 Hradec Králové, přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO 1; Fingerlandův ústav patologie, Fakultní nemocnice v Hradci Králové, Sokolská 581, 50005 Hradec Králové, přednosta prof. MUDr. Aleš Ryška, Ph. D. 2
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 4, p. 219-223
Category: Kazuistika
doi: https://doi.org/10.31348/2019/4/6Summary
Lichen planus is a relatively common mucocutaneous papulosquamous disorder of unknown etiology that is thought to be immunologically mediated. Ocular involvement of lichen planus (LP) is a rare event, which can lead to irreversible damage to the ocular surface and loss of vision from cicatrizing blepharoconjunctivitis and corneal scarring. Steroids are the first treatment choice. Treatment with topical ciclosporin A is also a possible treatment.
We report a case of 79-year-old woman who was treated for long lasting severe inflammatory disease of a ocular surface. It led to blindness of one eye and low vision of the second eye. The diagnosis was made thanks to correlation of biopsy results from oral and ocular surface. The patient was also diagnosed with middle-stage dementia. Negative impact of steroid therapy on mental condition of this patient was considered. On the other hand, dementia could cause worse compliance with recommended treatment regime.
Chronic inflammatory disease of ocular surface requires long lasting treatment very often and it is sometimes not as effective as expected. Discovering etiological causes of the disease is a priority for the right treatment. We emphasize also the key role of physical and mental condition in management of ocular surface disease.
Keywords:
lichen planus – cicatrizing blepharoconjunctivitis – Steroid therapy
INTRODUCTION
Lichen planus (LP) is an autoimmune inflammatory mucocutaneous papulosquamous pathology of unknown etiology. It is manifested in two forms, skin and mucosa. Ocular manifestations are rare and little known, but in differential diagnostics of severe and poorly managed blepharitis, this etiological unit is also necessary to consider. In addition to manifestations on the eyelids, it also causes severe, often cicatrising keratoconjunctivitis (2, 6, 7, 15). We present a case report of a 79-year-old woman treated over a number of years for a severe inflammatory disease of the ocular surface, which led to blindness in one eye and severe affliction of the other eye, in whom a diagnosis per exlusionem was determined, also thanks to the correspondence of the results of the biopsy from a lesion of the oral cavity and from a sample of the eyelid (Fig. 1 and 2). The patient was subsequently diagnosed with previously undetected medium-severe dementia, in which we consider also the negative effect of steroids on the deterioration of her mental condition, as well as the negative influence of the dementia itself on compliance with the recommended therapeutic regime.
Fig. 1. Histological sample from lesion in oral cavity in patient, sample taken in 2011. Spinocellular epithelium of mucosa of oral cavity with layer of parakeratosis, vacuolar degeneration, in subretinal conjunctiva streaked lymphocytic infiltrate typical of lichen planus 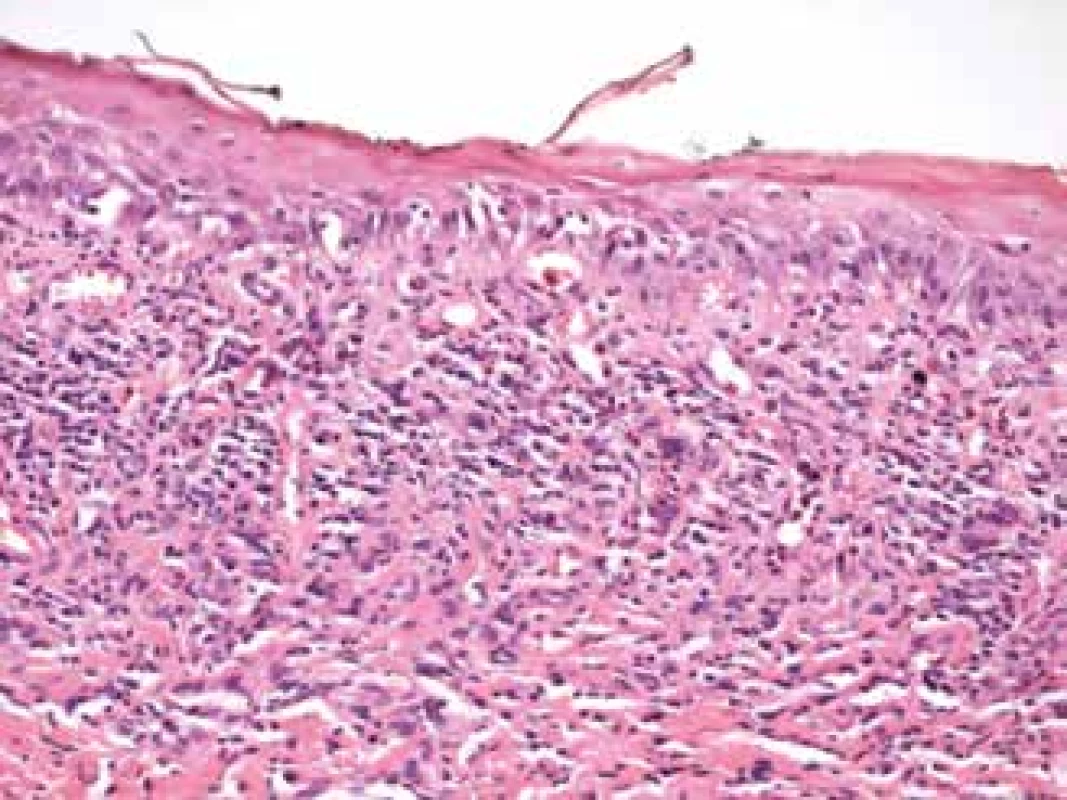
Fig. 2. Histological sample from edge of left eyelid, taken during partial tarsorrhaphy in 2017. Similar histological features attesting to lichenoid changes as in fig. 1, with lymphocytic infiltration of subepithelial conjunctiva 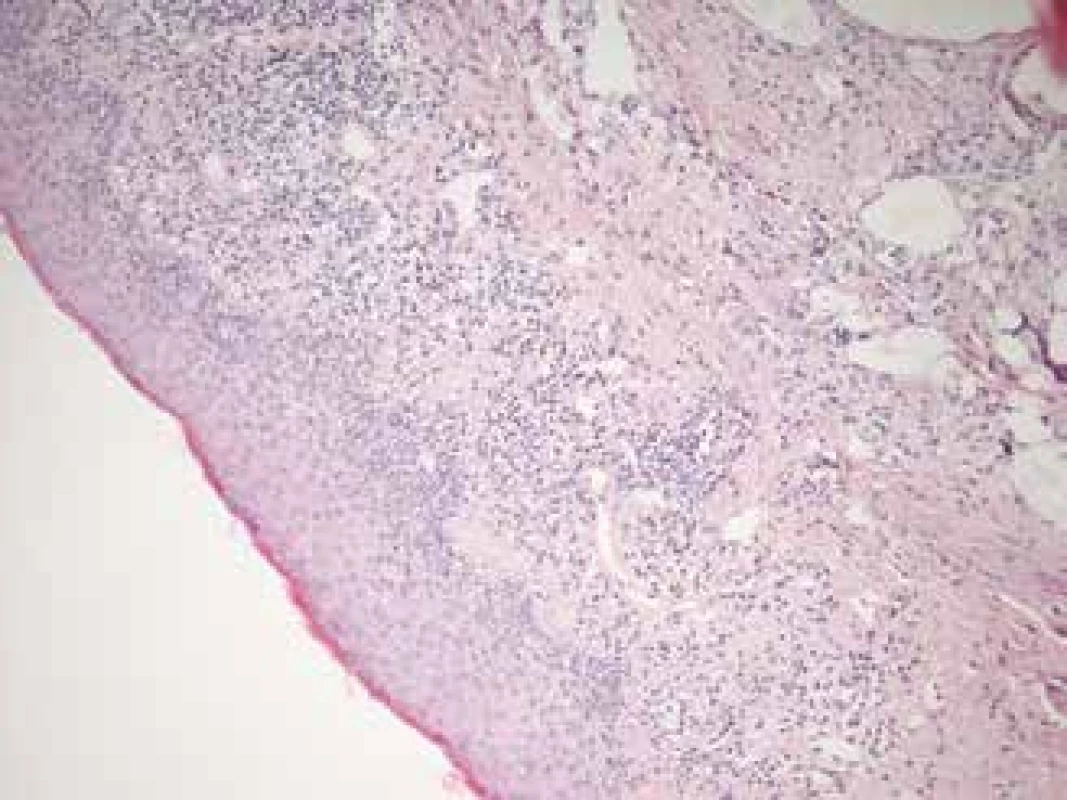
CASE REPORT
The patient, born in 1939, stated that she suffered the general pathologies of arterial hypertension, atrial fibrillation, aortic, mitral and tricuspid insufficiency and varices of the lower limbs. In her medical history she had two incidences of short-term loss of consciousness. Since 2011 the patient had been treated for lichen planus of the buccal mucosa. A biopsy was taken from a lesion on the mucosa of the oral cavity, with confirmation of the diagnosis (Fig. 1). Treatment with local preparations was conducted by stomatologists. No signs of systemic bullous pathology were present.
The patient’s ocular complaints began in April 2015, when she first reported to a local ophthalmologist with reddening of the eyes, she was treated as standard with antibiotics and steroids locally, adjusted therapy which slightly improved the condition. Her visual acuity (VA) at this time was within the range of 0.6-0.4 in the left eye, in the right eye within the norm.
A worsening of ocular complaints occurred at the beginning of June 2015, when the local ophthalmologist diagnosed herpetic keratitis in the left eye and applied antiherpetic treatment, VA deteriorated to 0.2. However, the clinical finding did not correspond to a herpetic etiology, and as a result this treatment was subsequently discontinued later at our centre. Due to irritation of the left eyeball, peripheral vascularisation and severe pain resulting from a non-healing epithelial defect with a size of 3x2 mm, we recommended application of eye drops from autologous serum to the left eye. Despite this, VA deteriorated to 3/50 at the beginning of July 2015, and irritation of the eye persisted, as a result of which we admitted the patient to our department. With intensive anti-infectious and mainly lubrication therapy, an improvement of her condition was achieved. During the course of subsequent hospitalisations, the patient’s complaints always improved temporarily, severe pain affecting her quality of life subsided, but her condition again deteriorated a few weeks later, with the result that the patient required further hospitalisations. A leucoma had already formed in the left eye at this time, and newly formed blood vessels had begun to grow into the opacified cornea, nonetheless the epithelial defect persisted, causing the patient severe pain (Fig. 3). Irritation improved after plastic surgery of a newly formed entropion of the lower left eyelid, we performed the procedure in November 2016. Further pain relief and stabilisation of the ocular finding was achieved by the application of ten drops of Cacicol. Nevertheless, this condition also was not permanent. After October 2017 a pronounced deterioration occurred, which required a further two hospitalisations. During the first of these, general therapy was applied with doxycycline for severe posterior blepharitis, in which we recommended long-term use. Again, not even this treatment was sufficiently effective. Before the last hospitalisation, cicatrising changes of the conjunctivas of the right eye (Fig. 4) began to appear in the patient, and the opacified cornea of the left eye began to dissolve in the place of the epithelial defect (Fig. 5). An attempt to apply local cyclosporine A in the preparation Ikervis gtt ophth failed, the patient was unable to tolerate the drug due to excessive stinging. General samples were taken in order to exclude the possibility of pathologies causing cicatrising conjunctivitis, mainly pustular diseases. All were negative. We also performed partial tarsorrhaphy of the left eye and sent the removed part of the eyelid for a histological examination. In the right eye the finding of severe keratoconjunctivitis worsened, with shallowing of the fornices and symblepharon, and visual acuity of the only seeing eye of 0.05. As a result we applied 3 infusions of solumedrol 1g to the patient, followed by oral steroid therapy in a dose of 80 mg of Prednisone with gradual reduction of 20 mg. It was this treatment that was finally effective, and improved the local condition of the eye as well as subjective severe complaints of the patient. Upon an attempt to reduce the dose, reactivation of the disease occurred.
Fig. 3. Left eye of patient with severe cicatrising blepharoconjunctivitis, vascularised leucoma, on surface persistent painful defect of corneal epithelium. Whitish plaques on edges of eyelid suggestive of lichenoid lesions 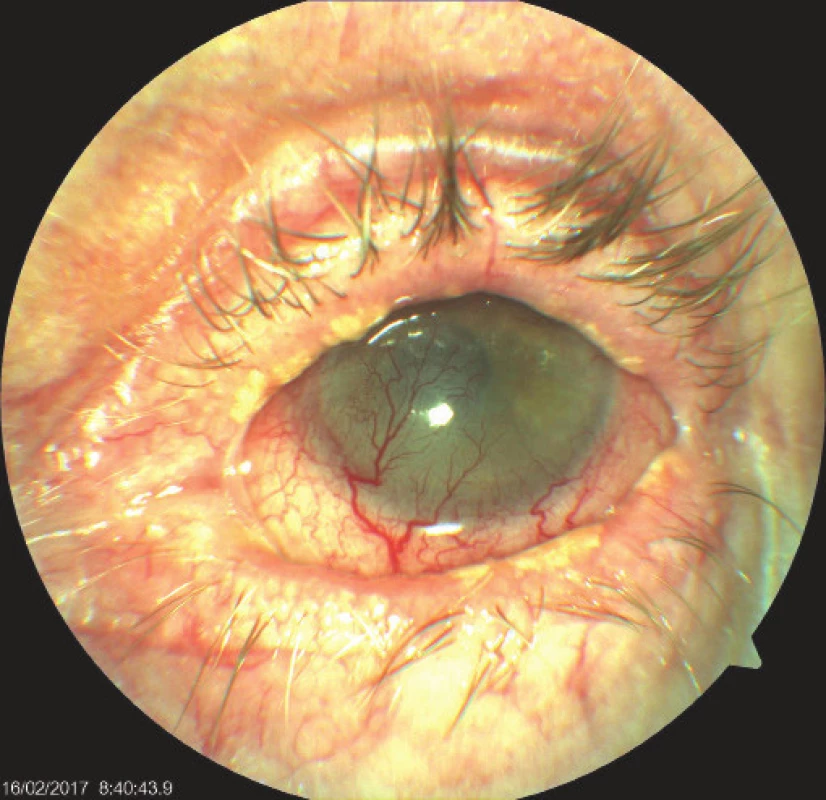
Fig. 4. Right eye of patient – cicatrising blepharoconjunctivitis, whitish plaques on edges of eyelids, symblepharon later appearing 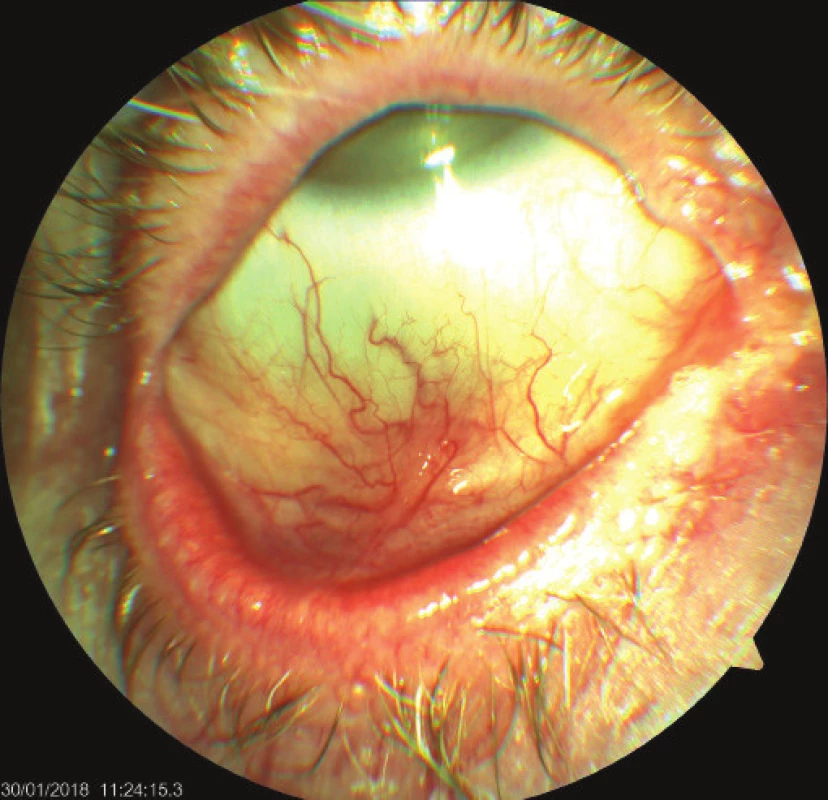
Fig. 5. Left eye of patient – incipient lysis of corneal leucoma, condition after partial tarsorrhaphy, eye irritated 
Unfortunately, at the end of January 2018 the patient’s general psychological condition worsened, she ceased to take all of her medications, was unable to remember virtually anything, and stated that she had fallen. Due to her disorientated condition she was hospitalised at a neurological clinic, where a detailed general examination was performed, including magnetic resonance of the brain with a negative result, and the patient was diagnosed with medium-severe dementia. The patient was no longer able to remain within her home environment, and was admitted to an inpatient department for subsequent care. Throughout the period of institutional treatment, the condition on the surface of both eyes improved markedly upon regular application of drops from autologous serum, ocular gel and Flucon 4x per day, and oral treatment with Prednisone in a dose of 20 mg per day. The patient’s vision at the last follow-up examination was 0.6 in right eye and light projection was correct in the left eye, the patient felt no pain and was relatively satisfied.
A number of diagnostic tests were conducted during the course of care for the patient with severe blepharoconjunctivitis and keratitis. A Schirmer’s test and break-up time (BUT) test, which demonstrated medium affliction, were performed as standard. Swabs from the conjunctival sac were repeatedly negative, in isolated cases with identification of staphylococcus epidermis and once Corynebacterium propinquum was detected in a swab from the right eye (6/2015). Samples to confirm primary Sjögren’s syndrome were negative (ENA SS A, ENA SS B, ANA, RF), as were samples for diagnosis of pustular diseases (immunoglobulins in serum: values of IgD, IgA1 and IgA2), all within the limits of the norm. An immunohistochemical blood test for anti-desmosomes, indirect immunofluorescence and anti-intercellular adhesion molecules were also negative.
A removed part from the margin of the lower left eyelid upon the performance of partial tarsorrhaphy at the end of 2017 (Fig. 2) was histologically examined. The excision was of a length of 7 mm, width 2 mm, the surface of the epidermis was maturing commensurately, beneath this was a finding of a streaked chronic inflammation, which minimally penetrated into the basal layers of the epidermis and was of a lichenoid character. The sample also contained a present histocytary reaction around the fine empty chambers (CD68), in which these changes suggested lipophagic granuloma. Some of the empty chambers were represented by dilated lymphatic blood vessels (CD31, D2-40). Staining for mycoses and BK was negative. The pathologist concluded the finding as chronic inflammation and histiocytic reaction with dilation of the lymphatic slits. No findings of changes which would be typical of Sjögren’s syndrome were present in the supplied material, no signs of a pustular pathology were found, including direct immunofluorescence. With regard to the lichenoid appearance and medical history of lichen planus in the patient’s oral cavity, we contacted a histologist, and a comparison was conducted of preparations from the conjunctiva and a preserved tissue sample from the left buccal mucosa, which was taken at the beginning of the patient’s acute complaints from her erosive lesion, with a whitish reticular lesion in the area of the oral cavity in 2011 (Fig. 1). Microscopically this concerned a fatty and fibrous particle with isolated fascicles of transversely streaked muscle tissue, which was covered on the surface by a regularly maturing spinocellular epithlium with a heightened regenerative exertion in the basal zone. Subepithelially there was evidence of layered lymphocytic inflammatory infiltrate, the elements of which penetrated as lesions into the basal sections of the epithelium. The microscopic finding was compatible with a clinical diagnosis of lichen planus. No convincing dysplastic changes or malignant tumour structures were identified within the scope of the examined material. The pathological changes in both preparations were identical, and as a result we concluded the condition as an ocular manifestation of lichen planus.
DISCUSSION
Differential diagnostics of cicatrising pathologies of the anterior segment of the eye is fairly complex. Correct diagnosis is often determined late, in the advanced stages of the pathology. At this time the clinical picture may be modified by previous, untargeted therapy. In first place we considered ocular cicatricial pemphigoid (OCP) in this patient. This is an autoimmune subepithelial pustular pathology on a background of type II hypersensitivity. It is characterised by linear deposits of immune reactants along the basal membrane of the epithelium. However, negative tests and the absence of typical signs of the pathology did not confirm this diagnosis. We are aware that in some studies (5, 12, 14) authors have determined a diagnosis of OCT even despite the negativity of these examinations. By contrast, some authors, for example Thorne et al., included in their study only patients who had direct positive immunofluorescence (14, 16). In the case of our patient, a sample of the margin was examined in tarsorrhaphy, we did not take another sample of the conjunctiva due to the risk of activating scarring, and we also did not take a new sample of the buccal mucosa for examination by direct immunofluorescence.
The patient did not have any further signs of pustular pathology on the skin, genitals or other mucous membranes beyond the aforementioned finding of LP in the oral cavity.
The majority of studies dealing with ocular manifestations of lichen planus are a set of case reports, and all mention the rare incidence of this disease. This is in contrast with non-ocular manifestations, which are a relatively common finding. Lichen planus occurs in approximately 0.9-1.2% of the population, most frequently between the third and sixth decade of life, both sexes are equally affected (4). It has diverse clinical manifestations, most often on the skin and mucous membranes of the mouth or genitalia (3, 13). Lichenoid lesions have a characteristic appearance and behaviour. They are recurring, mostly small, polygonal purplish papules with a flat surface, on which a superficial network of white lines (Wickham striae) is visible. They may appear practically anywhere on the entire body, but are often symmetrically located on the skin above the flexors on the limbs or on the chest, and frequently cause itching. Mucosa LP have the appearance of whitish reticular macules. Lesions are stationary, subacute or with a chronic course. Ocular lichen planus may lead to irreversible damage to the surface of the eye and loss of vision. It most frequently causes severe dry eye syndrome with a large imbalance of the lachrymal film, scarring of the conjunctivas and corneas and chronic inflammation of the eyelids. It typically reacts poorly to any local ocular therapy (9, 10). It is stated that lichen may be for example a causative agent of scleritis (13).The cause of this pathology is T-cell mediated autoimmune inflammation. Changes affecting the region of the basal membrane are explained by apoptosis of keratinocytes, which originates due to the action of CD8+ T-lymphocytes. These cells are activated by tumour necrosis factor alpha. Decayed keratinocytes impair the firmness of the basal membrane, which splits. Matrix metalloproteinase 9 also enters this process (3).
Similarly as in the aforementioned international case reports (6, 7, 9, 15), in our case we also reached a diagnosis only after arduous, long-term treatment of severe keratoconjunctivitis, which took place asymmetrically in both eyes, thanks to the consistency of the histological results of the pathological lesions of the buccal mucosa and eyelid conjunctiva and the negativity of indicators for OCP. Both clinical units, LP and OCP, are similar, manifesting pathology in the region of the BM and a similar clinical picture, and correspondingly subsequent therapy is also similar. In the histological image of LP, however, there is a predominant infiltration of the subepithelial connective tissue by lymphocytes, which for lichen is typical in a band. Some lymphocytes may infiltrate also into the basal layers of the spinocellular epithelium, the basal layers of which manifest vacuolar degeneration, which also ranks among the general signs of lichenoid changes. Irregular acanthosis of the epidermis appears on the surface, with hypergranulosis and compact hyperkeratosis (4). The histological image shows presence of eosinophils in the sample of tissue from the surface of the eye of our patient, potentially pointing to a “lichenoid reaction”, which may be induced by several pharmaceuticals including for example beta-blockers, thiazide diuretics, captopril, gold salts, antimalarial drugs, cinnarizine, lithium, penicillamine (17), although the patient had not used any of the above pharmaceuticals.
Therapy of cicatrising pathologies of the ocular surface is diverse. Local treatment is taken as supportive. With regard to the characteristics of the disease, long-term or even permanent lubrication therapy is required using preparations not containing preservative agents. Steroid therapy is also used, which in our patient however did not have a substantial effect. At present it is possible also to apply local cyclosporine A in drops, which our patient did not tolerate due to severe ocular discomfort. General immunosuppressant treatment is of fundamental importance. The method of choice is steroid therapy (2, 6, 9, 10), although in the case of insufficient monitoring of the pathology or the need for higher CS doses with the risk of occurrence of adverse effects it is possible also to proceed to the use of other immunomodulating agents such as cyclophosphamide, azathioprine, sulphapyridine and above all mycophenolate mofetil, more frequently in combination with CS treatment. Our patient was incorrectly treated for a long period of time only with local CS and anti-infectious drugs, she eventually responded favourably to pulses of steroids intravenously, followed by long-term treatment with prednisolone (Prednisone) orally in a dose of 20 mg. Upon attempts to reduce the dose, reactivation of the disease occurred. Unfortunately, it is not possible to commence treatment of this patient with other immunosuppressants due to her present very poor condition, which prevents regular and frequent follow-up examinations. During the course of the pathology the patient suffered from severe pains caused by defects on the ocular surface, which she tolerated relatively well. Paradoxically, her psychological condition deteriorated rapidly following relative stabilisation of her ocular condition and the subsidence of pain. She ceased to use eye drops and pharmaceuticals whatsoever, and was diagnosed with medium-severe dementia, which had not been manifested at all during her previous frequent visits. We are therefore considering the possibility of an adverse influence of aggressive steroid therapy in deteriorating the patient’s psychological condition. This phenomenon is mentioned in the literature (1, 8, 11). Nonetheless, it is also necessary to consider an alternative interpretation, in which the patient forgot to use eye drops and pharmaceuticals as recommended due to her as yet undetected dementia. We are led to this conclusion by the fact that following her hospitalisations, as well as during institutional treatment, when the correct therapy was ensured, the patient’s condition on the ocular surface of both eyes improved markedly, and she now remains stable with the set treatment.
CONCLUSION
Chronic inflammatory diseases of the anterior segment of the eye often lead to frustrations on the part of both the patient and the doctor. Treatment is long-term, and does not always bring the expected results. Detection of the etiology of the pathology represents a priority for the purpose of targeting subsequent therapeutic measures. In our study we have presented a lesser known cause of cases of cicatrising chronic blepharoconjunctivitis which is unresponsive to treatment. We also point to the fact that the patient’s general physical and psychological condition of health plays a key role in managing adverse ocular conditions.
Presented in the form of a lecture at the 26th congress of the Czech and Slovak Ophthalmology Society in Prague
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 17. 10. 2018
Accepted: 23. 8. 2019
Available on-line: 6.1.2020
MUDr. Jana Nekolová, Ph.D.
Oční klinika FN Hradec Králové
Sokolská 581,
500 05 Hradec Králové
Zdroje
1. Cipriani, G., Picchi, L., Vedovello, M., et al.: Reversible dementia from corticosteroid therapy. Case report. Clin Geriatrics, 20(7); 2012 : 2-5.
2. Dart, JK.: The 2016 Bowman lecture conjuntival curses: scarring conjunctivitis 30 years on. Eye, 31; 2017 : 301-332.
3. Dřízhal, I., Paulusová, V.: Orální lichen planus-současné poznatky. Cesk Stomatol, 108(2); 2008 : 35-38.
4. Duchková, H.: Lichen planus. Doporučené postupy pro praktické lékaře. Dostupný na: www.cls.cz/dp. Reg. č. a/004/238.
5. Elder, MJ., Bernauer, W., Leonard, J., et al.: Progression of disease in ocular pemphigoid. Br J Ophthalmol, 80; 1996 : 292-6.
6. Huang, S., Channa, P.: Cicatrical keratoconjunctivitis associated with lichen planus. A case report. GMS Ophthalmol Cases, 7(5); 2015 : 1-3.
7. Igra, E., Kennedy, S., MacDermott, EJ. et al.: Isolated ocular lichen planus in a child. J AAPOS, 19(4); 2015 : 381-3.
8. Keenan, PA., Jacobson, MW., Soleymani, RM., et al.: The effect on memory of chronic prednisone treatment in patients with systemic disease. Neurology, 47(6); 1996 : 1396-402.
9. Muňoz, ER., Martínez-Escala, ME., Juanpere, N. et al.: Isolated conjunctival lichen planus. A diagnostic Challenge. Arch Dermatol, 147(4); 2011 : 465-67.
10. Pakravan, M., Klesert, TR., Akpek, EK.: Isolated lichen planus of the conjunctiva. Br J Ophthalmol, 90(10); 2006 : 1325-6.
11. Sacks, O., Shulman, M.: Steroid dementia: an overlooked diagnosis?. Neurology, 64(4); 2005 : 707-9.
12. Saw, VP., Dart, JK.: Ocular musous membrane pemphigoid: diagnosis and management strategies. Ocul Surf, 6(3); 2008 : 128-42.
13. Shoughy, SS.: Unusal ocular presentation in a patient with lichen planus. Can J Ophthalmol, 53; 2018: e122-24.
14. Szabó, E., Palos, M., Skalická, P.: Oční jizevnatý pemfigoid - restrospektivní studie. Cesk Slov Oftalmol, 72 (1); 2016 : 283-91.
15. Thorne, JE., Jabs, DA., Nikolskaia, OV. et al.: Lichen planus and cicatrizing conjunctivitis: characterization of five cases. Am J Ophthalmol, 136(2); 2003 : 239-43.
16. Thorne, JE., Woreta, FA., Jabs, DA., et al.: Treatment of ocular mucous membrane pemphigoid with immunosuppressive drug therapy. Ophthalmology, 115(12); 2008 : 2146-52.
17. Viktorinová, M.: Nežádoucí účinky léků na kůži. Prakt. lékáren, 9(6); 2013 : 214–18.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 4- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- Slovo vedoucího redaktora
- Late postoperative opacification of a hydrophobic acrylic intraocular lens AcryNovaTMPC 610Y
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Ranibizumab in macular oedema secondary to branch retinal vein occlusion – 24 months of treatment
- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- SIMULTANEOUS BILATERAL ACUTE ANGLE-CLOSURE GLAUCOMA IN MILLER FISHER SYNDROME
- Lichen planus as a possible rare cause of an ocular disease
- Výročie narodenia prof. MUDr. Milana Izáka, PhD, FEBO
- Panu docentovi s láskou...
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Lichen planus as a possible rare cause of an ocular disease
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




