-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Influence of cornea on intraocular pressure measurement by ICARE PRO and ORA
Authors: F. Pluháček 1; A. Unzeitigová 1; K. Marešová 2; J. Rybář 3
Authors place of work: Katedra optiky, Přírodovědecká fakulta, Univerzita Palackého v Olomouci, vedoucí katedry: prof. Mgr. Jaromír Fiurášek, Ph. D. 1; Oční klinika, Fakultní nemocnice a Lékařská fakulta, Univerzita Palackého v Olomouci, přednosta kliniky: prof. MUDr. Jiří Řehák, CSc., FEBO 2; Ústav automatizace, měření a aplikované informatiky, Strojnická fakulta, Slovenská technická univerzita v Bratislavě, vedoucí ústavu: prof. Ing. Cyril Belavý, CSc. 3
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 3, p. 111-118
Category: Původní práce
doi: https://doi.org/10.31348/2019/3/1Summary
Aim: To compare intraocular pressure readings (IOP) measured by ICARE PRO and ORA G3 and analyse the influence of the corneal hysteresis (CH), central corneal thickness (CCT), average central corneal radius, corneal astigmatism and age on the readings. In addition, to compare the repeatability of measurement by both tonometers.
Methods: The data was collected by IOP measurements in both eyes in 40 individuals between ages of 41 and 86 years. The number of 74 eyes (70 eyes in the case of ORA repeatability) were included to the study, remaining eyes were excluded due to incomplete data, abnormal cornea or low quality of measurement. The subjects were all diagnosed for glaucoma or were suspected of having glaucoma. In the case of ORA tonometer, the Goldmann-correlated IOP (IOPG) and corneal compensated IOP (IOPCC) were monitored. The CH was measured by ORA, CCT by ultrasound pachymeter and corneal curvature and astigmatism by autokeratometer. The effect of corneal parameters and age on IOP or on differences between tonometers were analysed by multiple linear regression. The comparison of readings from both tonometers and repeatability analysis (based on test-retest) were realised using a paired t-test and a Bland-Altman method. The level of statistical significance was set to 0.05.
Results: The IOP readings from both tonometers were positively correlated with CCT and negatively with CH. The effects of other monitored parameters were insignificant. The mean ICARE PRO reading did not differ significantly from IOPG but were significantly lower than IOPCC. The variability of differences was, however, high in both cases and differences were influenced by IOP and CH (ICARE PRO shown higher readings with decreasing IOP and increasing hysteresis). The lowest repeatability coefficient shown ICARE PRO, the worst IOPCC (3.0 mmHg for ICARE PRO, 3.8 mmHg for IOPG and 4.8 mmHg for IOPCC).
Conclusion: The IOP values measured by both considered tonometers are significantly influenced by corneal hysteresis and central thickness. The effect of CCT can arise from an effect of a corneal stiffness. Regarding the high variability of mutual differences, the data from ICARE PRO and ORA are not interchangeable. The repeatability of ICARE PRO was comparable with Goldmann applanation tonometer measurement under given conditions, and better than ORA.
Keywords:
intraocular pressure – ICARE – ORA – corneal hysteresis – central corneal thickness
INTRODUCTION
Measurement of intraocular pressure (IOP) plays a significant role in the diagnosis and screening of glaucoma. The gold standard in the measurement of intraocular pressure is considered to be the Goldmann applanation tonometer, the use of which however requires the application of anaesthetics, fluorescein and sufficient experience on the part of the examiner. In the case of non-standard conditions, such as measurement of recumbent or uncooperative patients or children, examination outside of the clinic etc., small and easily portable “rebound tonometers” of the ICARE type from the Icare Finland company can be a useful tool. These tonometers determine intraocular pressure from the change of kinetic properties of a small single-use probe upon its rebound from the cornea (17, 18). They do not require anaesthesia of the cornea or application of other pharmaceuticals, and at the same time, within the framework of the studies conducted to date, demonstrate good accordance of the measurements with the results of Goldmann applanation tonometry (2, 8, 9, 12, 22, 24, 28, 29).
Another group of tonometers that do not require the application of pharmaceuticals, and furthermore with regard to the possibility of an automatic mode minimise the influence of the operating staff, are non-contact tonometers. These are based on the observation of corneal deformation by means of a jet of air. The progressively strengthening, very short air pulse causes flattening (applanation) of the cornea, in which IOP is determined from the time necessary for applanation and from the current pressure of the air pulse at the moment of applanation (17). In general the effect of the pressure of the air pulse may cause two applanations – the first upon increase of the pressure of the stream of air and the second upon its decrease, upon which the cornea returns to its original shape. Standard tonometers usually use only one applanation for determining pressure. The ORA (Ocular Response Analyser) device from Reichert Technologies enables the observation of both applanations, and on the basis of the determined differences also evaluates the biomechanical properties of the cornea, which reflect its viscoelasticity, see e.g. (16, 17, 35), specifically corneal hysteresis (CH) and rigidity. Hysteresis is manifested by different pressure values, corresponding to the first and second applanation, and is numerically defined as the difference between both applanation pressures. Two output values are determined on the basis of these parameters, namely IOPG, which should correlate with the measurement by a Goldmann tonometer, and intraocular pressure with calculated corneal compensation of the influence of hysteresis (IOPCC). In this, IOPG is stipulated as the mean of both applanation pressures.
In comparison with ORA, the ICARE tonometer does not usually record a marked difference as against IOPG, nevertheless it is distinct in comparison with IOPCC (10, 14, 35), in which a number of studies, e.g. (35), record this difference only in the case of glaucoma patients. It is known that the parameters of the cornea are significantly influenced by data from both types of tonometers, in which a significant role is played especially by biomechanical properties (3, 35), as well as e.g. thickness (2, 13, 14, 19, 21, 28). As a result, it is possible to expect that a mutual comparison of both instruments will show a dependency on these parameters, as shown in the case of corneal hysteresis by the study by J. Shin et al. (35). Because hysteresis simultaneously manifests a significant correlation with the incidence of glaucoma (for an overview of the issue see e.g. (6)), it is of fundamental importance to know its influence on the measurement of IOP using various instruments.
The aim of this study was to mutually compare the results of measurement of intraocular pressure obtained by the tonometers ICARE PRO (IOPIC) and ORA G3 (IOPG and IOPCC), and to determine the influence of corneal hysteresis (CH), central corneal thickness (CCT), mean central radius of corneal curvature (R), size of corneal astigmatism (Ast) and age. The comparison was supplemented by an analysis of the repeatability of measurement.
METHOD
Cohort of probands
The study took place at the Department of Ophthalmology at the University Hospital of Palacký University in Olomouc. The study included 40 probands, of whom 24 were women and 16 men, within an age range of 41 to 86 years with an average age of 66 years and standard deviation of 11 years. All the probands had been either diagnosed with glaucoma or were being observed for suspected glaucoma. Both eyes of each proband were examined, in which only eyes with a normal, healthy cornea, in which all the observed parameters had been successfully measured, were included in the study. In the case of measurement of corneal hysteresis, observed quality of measurement by the instrument equal to or greater than 3 was required. In total 74 eyes were included in the study, in which all the stipulated requirements were met, with the exception of determination of repeatability of the ORA tonometer, in which only 70 eyes were included due to the low quality of measurement in the retest. The study was conducted in accordance with the provisions of the Helsinki declaration.
Procedure of examination
All the examinations took place within the framework of a single complex ophthalmological examination. First of all R and Ast were determined with the aid of an autokeratorefractometer. Subsequently the anaesthetic Benoxi 0.4% (manufacturer Unimed Pharma) was applied to the conjunctival sac of each eye for the purposes of ultrasonic measurement of corneal thickness, and fluorescein was also applied for colouring the lachrymal film for the purposes of other ophthalmological examinations. After measurement of central corneal thickness using the ultrasonic pachymeter Accupach V (manufacturer Accutome), measurement of intraocular pressure IOPIC with an ICARE PRO tonometer was conducted at the same work station (without the need to move the proband) at an interval of approximately three minutes. Each eye was measured twice consecutively (test and retest). The resulting measurement on the given eye was the mean of a series of six rapidly conducted consecutive partial measurements. If the measurement was evaluated by the instrument software as erroneous, or if there was a large dispersion within the partial values, the measurement was not accepted and the entire series was repeated. Subsequently within the framework of the same examination room the probands were moved to the ORA instrument, on which IOP was again measured twice. On the basis of the first measurement (test) using the ORA tonometer, CH, IOPG and IOPCC were determined. In the case of the second measurement (retest), only both intraocular pressure values were recorded. The coefficient of measurement quality was always observed in the test and retest. Measurement on both tonometers was always conducted by the same sufficiently experienced operator.
Data analysis
First of all the dependency of intraocular pressure on CCT, CH, R, Ast and age of the proband was evaluated in a combined effect of these factors, with the aid of multiple linear regression. For the purposes of regression only the values IOPIC, IOPG and IOPCC from the first measurement (test) were always used from each proband.
The accordance of the data obtained by both instruments (specifically IOPIC x IOPG and IOPIC x IOPCC) and the analysis of the repeatability of measurement by the test-retest method were evaluated by a paired t-test and with the aid of Bland-Altman graphs (1, 31), which identify the dependency of the differences of the observed quantities on their average. For a mutual comparison of the instruments, again only the values from the first measurement (test) were used. Within the framework of the analysis, partial differences of the compared values were stipulated for each eye, i.e. IOPIC - IOPG and IOPIC – IOPCC, or more precisely the differences of measurement from the test and retest, the mean values and standard deviations (SD) of these differences in the observed cohort of the eyes, and the corresponding 95% confidence intervals. The upper and lower limit of the confidence interval was set as the mean difference ± 1.96·SD. In the case of repeatability the value of 1.96·SD is also indicated as the coefficient of repeatability (CoR). In addition for each eye the arithmetical averages of the compared values from both instruments were calculated (IOPIC + IOPG)/2 and (IOPIC + IOPCC)/2, or more precisely the averages of the values from the test and retest. The influence of the observed corneal parameters and age on the differences between the individual instruments was analysed by multiple linear regression.
For data processing the MS Excel program was used, multiple linear regression and applicable tests of data normality (Shapiro-Wilk test) were conducted in the STATISTICA 13.0 program (StatSoft, Tulsa, OK, USA). All the statistical hypotheses were tested on a level of significance of 0.05. The results are presented in the text in the form of mean ± relevant standard deviation.
RESULTS
The mean values of intraocular pressure determined in the test were 16.7 mmHg ± 3.5 mmHg for IOPIC, 16.1 mmHg ± 5.5mmHg for IOPG and 17.8 mmHg ± 5.3 mmHg for IOPCC. The quality of measurement coefficient on the ORA instrument was within the range of 3.2 to 9.0, with a mean value of 5.3 and standard deviation of 1.5. The mean values of measured corneal parameters including the relevant standard deviations are presented in table 1. Multiple regression demonstrated a significant influence of CH and CCT both in the case of IOPIC (p = 0.0077 and p = 0.00018) and of both values of intraocular pressure from ORA (in all cases p = < 0.0001). The other observed quantities did not correlate significantly with IOPIC, IOPG or IOPCC. The partial correlation coefficients (i.e. correlations determined upon removal of the influence of other observed variables) of all the evaluated parameters with measured values of intraocular pressure are summarised in table 2. From here it ensues that in the case of both instruments, higher CCT corresponds to higher measured values of intraocular pressure, whereas by contrast the measured intraocular pressure decreases with increasing CH. The pressure values measured by the ORA tonometer record a stronger dependency on CH and CCT than in the case of the data from ICARE PRO.
Tab. 1. Mean values and standard deviations (SD) of the corneal hysteresis (CH), central corneal thickness (CCT), mean central radius of corneal curvature (R) and size of corneal astigmatism (Ast) 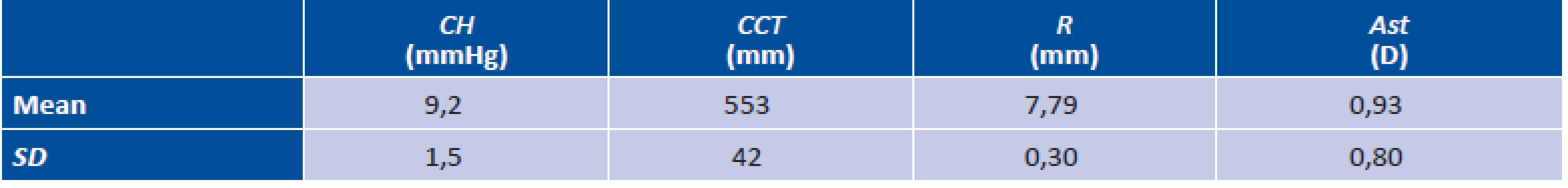
Tab. 2. Values of partial correlation coefficients of all observed variables (corneal hysteresis CH, central corneal thickness CCT, mean central radius of corneal curvature R, size of corneal astigmatism Ast and age) with all measured values of intraocular pressure (values from the first measurement are always used; IOPIC represents data from ICARE PRO and IOPG and IOPCC data from ORA. Significant correlations are indicated with a star 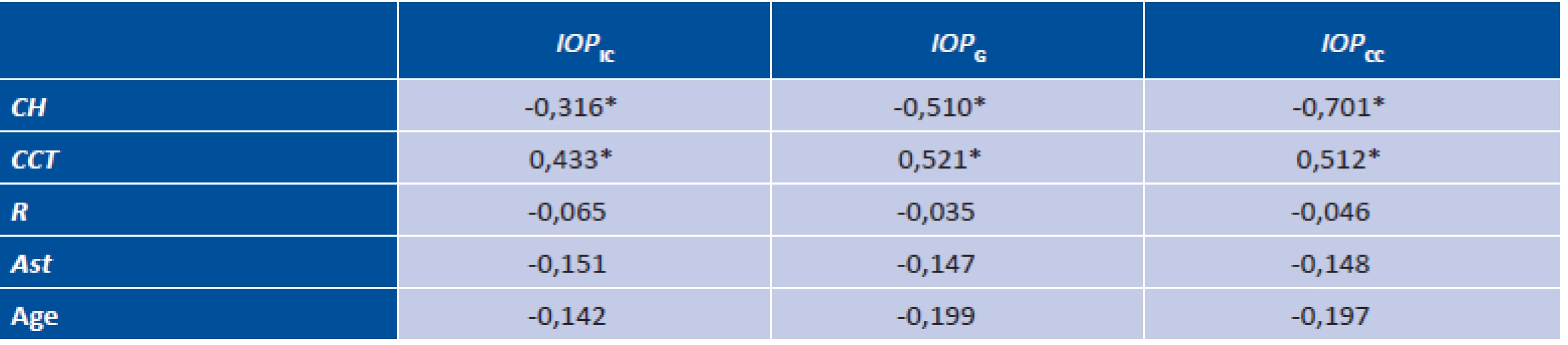
A graphic comparison of the values from both instruments with the aid of Bland-Altman graphs is illustrated in fig. 1. The upper graph compares IOPIC and IOPG, the lower graph IOPIC and IOPCC. The mean difference (represented by a full line in the graphs) between IOPIC and IOPG (0.6 mmHg ± 3.5 mmHg) was statistically insignificant (paired t-test, p = 0.13), whereas IOPCC was significantly higher as against IOPIC by 1.1 mmHg ± 3.6 mmHg (p = 0.013). The corresponding scope of the 95% of the confidence interval (indicated in the graphs by dashed lines) was from -6.2 mmHg to 7.4 mmHg for IOPIC and IOPG and from -8.2 mmHg to 6.0 mmHg for IOPIC and IOPCC. From the graphs it can be seen that the difference has a decreasing tendency upon an increase of intraocular pressure, indicated by the regression line (dotted). Here ICARE PRO overmeasures for low pressure values as against ORA, whereas the reverse applies for high values. In accordance with the graphs, multiple regression confirmed a significant correlation of the difference of measured pressures with an average size of intraocular pressure (p < 0.0001 and p = 0.023) and furthermore demonstrated a correlation with corneal hysteresis (p < 0.027 and p < 0.0001). The other parameters did not have a significant influence. The partial correlation coefficients of the differences between the instruments and all the included parameters of cornea and age are summarised in table 3. In patients with higher hysteresis, ICARE PRO records higher values than ORA. The difference between the values is more influenced by pressure in the case of comparison with IOPG, in the case of IOPCC by hysteresis. The influence of hysteresis on the difference in values between ICARE PRO and ORA is demonstrated by the graphs in fig. 2.
Tab. 3. Values of partial correlation coefficient of all observed variables (corneal hysteresis CH, central corneal thickness CCT, mean central radius of corneal curvature R, size of corneal astigmatism Ast and age) and average of compared pairs of measurements of intraocular pressure with values of mutual difference of intraocular pressure of compared pairs (values from the first measurement are always used; IOPIC x IOPG and IOPIC x IOPCC are compared; IOPIC represents data from ICARE PRO and IOPG and IOPCC data from ORA). Significant correlations are indicated with a star 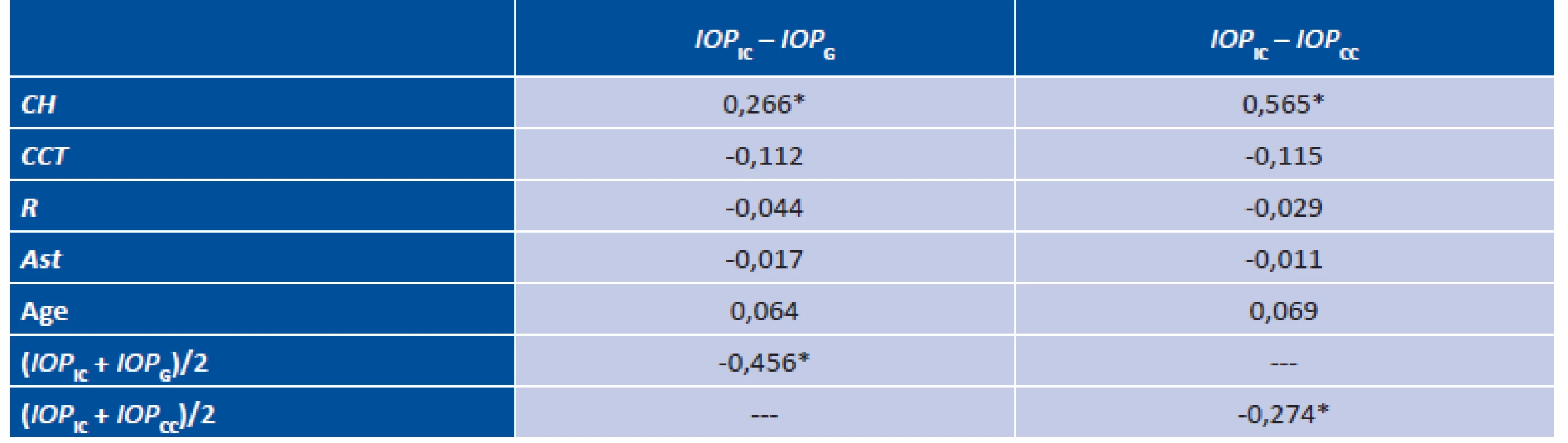
Fig. 1. Bland-Altman graphs identifying the dependency of the differences in values of intraocular pressure measured by the ICARE PRO (IOPIC) and ORA instruments in the case of pressure correlated with a Goldmann tonometer (IOPG; upper graph) and corrected with respect to the biomechanical properties of the cornea (IOPCC; lower graph) on the mean value of compared pressures. The rings represent values for the individual eyes, the dashed lines delineate the 95% confidence interval, the full line represents the mean difference. The dotted line is a regression line interspersed with data. 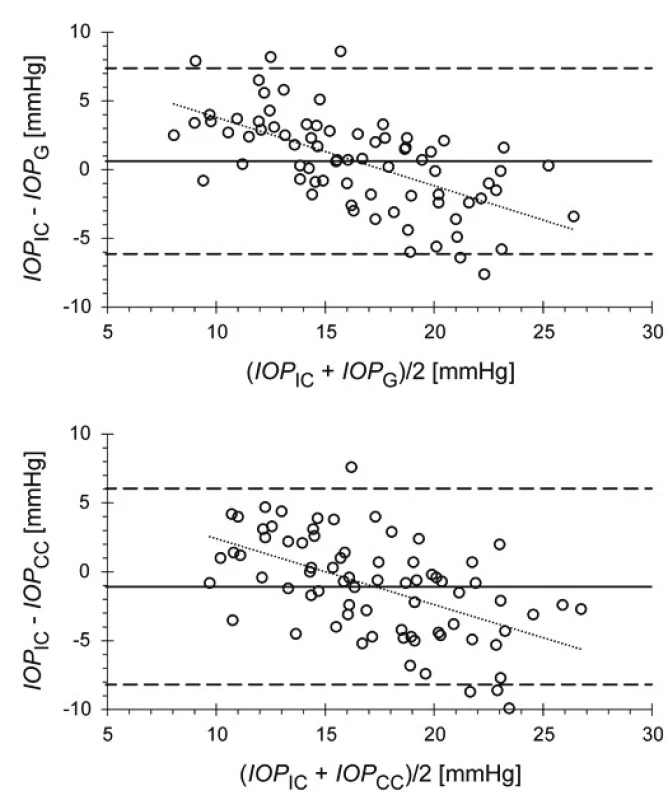
Fig. 2. Graphs identifying the dependency of the differences in values of intraocular pressure measured by the ICARE PRO (IOPIC) and ORA instruments in the case of pressure correlated with a Goldmann tonometer (IOPG; upper graph) and corrected with respect to the biomechanical properties of the cornea (IOPCC; lower graph) on corneal hysteresis (CH). The rings represent difference values for the individual eyes, the dashed lines delineate the 95% confidence interval, the full line represents the mean difference. The dotted line is a regression line interspersed with data. 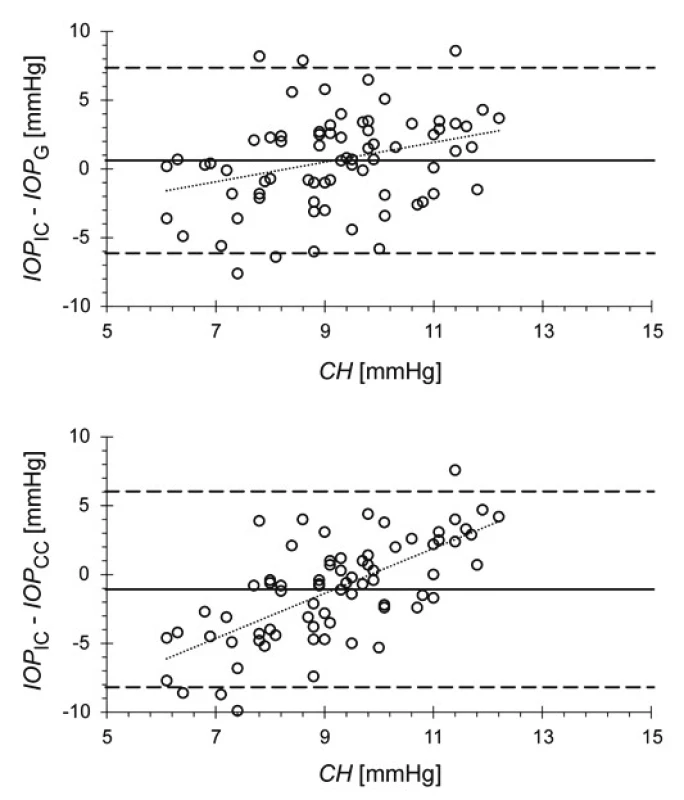
The results of the measurements of repeatability are presented in table 4, which summarises the mean values from the test and retest, their mean difference and corresponding standard deviations. In the case of the values from ICARE PRO, no significant difference was found between the test and retest (paired t-test, p = 0.68), although the values of the test and retest for outputs from ORA differed significantly (p = 0.0043 for IOPG and p = 0.014 for IOPCC). Table 4 shows that repeated measurement in the case of ORA records slightly lower values, however on average it is possible to consider the difference insignificant from a clinical perspective. The results are recorded in graphs in fig. 3. From the graphs and from table 4 it ensues that the best repeatability is provided by IOPIC (ICARE PRO), whereas by contrast the worst was recorded in the case of IOPCC.
Tab. 4. Mean values and standard deviations (SD) of all observed values of intraocular pressure in the case of the first measurement (test) and repeated measurement (retest), their difference and corresponding coefficient of repeatability (CoR); IOPIC are data from ICARE pro, IOPG and IOPCC data from ORA. Significant differences are indicated with a star. 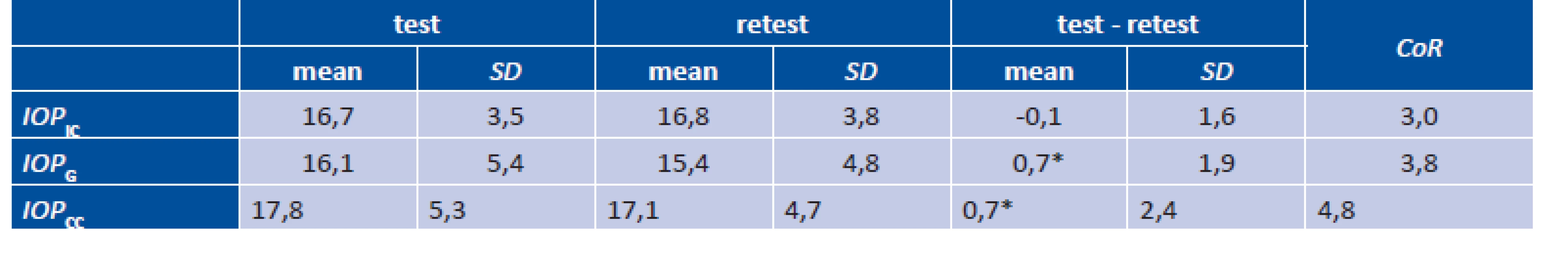
Fig. 3. Bland-Altman graphs identifying the dependency of the differences of the test and retest on the mean value from both measurements for data from the ICARE PRO (IOPIC; upper graph) and ORA instruments in the case of pressure correlated with a Goldmann tonometer (IOPG; middle graph) and corrected with respect to the biomechanical properties of the cornea (IOPCC; lower graph). The rings represent values of the differences for the individual eyes, the dashed lines delineate the 95% confidence interval, the full line represents the mean difference. 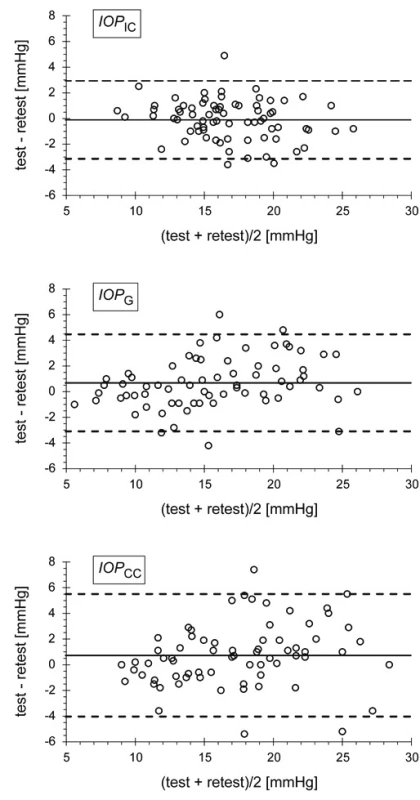
DISCUSSION
The result of the measurement of intraocular pressure may be influenced by a range of factors. On one hand these may be undesirable changes of IOP directly before measurement, on another these are factors distorting the actual measurement. For example, factors with a direct influence on IOP include physical exertion before measurement (25, 26, 38), hypoxia (4, 7, 15, 27, 30), intake of fluids (33, 34, 37), change of body or head position (for an overview see e.g. (32)). The actual measurement of IOP is then influenced primarily by the measuring method and the properties of the cornea. The results obtained by the different methods may therefore differ among themselves. The study presented in this article performed a comparison of the ocular tonometers ICARE PRO and ORA on a cohort of eyes of glaucoma patients or persons with suspected glaucoma. The comparison also included an analysis of the influence of selected corneal parameters. It was determined that the data on IOP from both the observed instruments is significantly correlated with corneal hysteresis (the measured values of IOP decrease with increasing CH) and central corneal thickness (higher CCT leads to higher measured values of IOP). A stronger dependency was observed in the case of the outputs from ORA. The determined influence of corneal hysteresis on measurement by both tonometers is confirmed also by other studies (3, 35). In the case of central corneal thickness, however, there is no consensus among the existing publications. The majority of studies which evaluated the influence of CCT without regard to other (especially biomechanical) parameters determined a positive correlation, i.e. an increasing value of pressure with increasing CCT in the case of tonometers of the ICARE (2, 13, 14, 19, 21, 28, 35) and ORA types (14, 20, 35). By contrast, upon consideration of the concurrent effect of CCT and biomechanical parameters by the method of multiple regression (3, 35, 3), no relationship with IOP was confirmed. Because CCT is positively correlated with corneal rigidity (thicker corneas are more rigid, see e.g. (5, 35, 5)), on the basis of their mutual relationship it is possible to consider the influence of CCT observed in our and other studies to be a reflection of the influence of corneal rigidity. However, measurement of CH was not included in this study. On the other parameters (R, Ast, age), no dependency was determined by the method of multiple regression in accordance with (11, 20, 35). Furthermore, study (35) determined that the outputs from ICARE and ORA are also not influenced (upon summary evaluation by multiple regression) by axial length of the eye or by spherical equivalent.
From a mutual comparison of the instruments it ensued that IOPIC and IOPG do not differ significantly, whereas the mean value of IOPIC was statistically significantly lower in comparison with the mean of IOPCC by approximately 1.1 mmHg ± 3.6 mmHg. However, in both cases a relatively high variability of the differences between the instruments was found in individual eyes, represented by wide confidence intervals in the Bland-Altman graphs (see fig. 2). Due to this variability, mutual interchangeability of the results from ICARE PRO and ORA is not possible. The existing comparative studies show a similar (10) or slightly smaller (35) width of confidence intervals. The mean differences we determined are influenced by the size of intraocular pressure and CH, whereas the parameters CCT, R, Ast and age did not record any fundamental influence. Upon higher mean pressure, ICARE PRO recorded lower values as against the ORA tonometer, and vice versa. By contrast, higher corneal hysteresis led to an increase in the data from ICARE PRO as against both values from ORA. A similar dependency of differences between both the tested instruments on CH is stated by publication (35), though without the influence of IOP. Previously conducted studies, in accordance with our results, unanimously confirm that the IOPIC and IOPG values do not differ on average, both in the case of normal healthy individuals (10, 14, 35) and in the case of glaucoma patients (35). As against this, the difference between IOPIC and IOPCC is evaluated differently. Shin et al. (35) determined that glaucoma patients record an approximately 0.89 mmHg lower value of IOPIC as against IOPCC, whereas in normal healthy individuals they did not find any significant difference. By contrast, studies (10,14) state a difference between IOPIC and IOPCC also in normal healthy probands, in which according to (10) ICARE PRO records lower and according to (14) higher values than ORA. The cause of the differences may be in the dependency we found on the size of IOP and CH, in which it is known that CH reaches different mean values in glaucoma patients as opposed to normal healthy individuals (6).
The test-retest demonstrated better repeatability in the case of ICARE, which is comparable with published data for the Goldmann applanation tonometer (e.g. (36, 39)). Repeatability in the case of ORA was slightly worse, in which the worst result was recorded for IOPCC. This may be due to the fact that IOPCC is determined by a calculation in which CH enters (a measured quantity with its own variability), which may have a worsening effect on the resulting repeatability. A difference in repeatability between IOPCC in comparison with IOPG is recorded also by a number of other studies, e.g. (23, 36, 39), in which (23) however states slightly better IOPCC as against IOPG. In the case of both values, a small but from a clinical perspective statistically significant change between the test and retest was determined in the case of ORA – upon repeated measurement on ORA there was a slight mean decrease of the measured values. The reason may be the practical familiarity of the proband with the measurement and therefore the lesser stress upon repeated measurement. All the measurements were conducted by a single operator. With regard to the fact that measurement on an ORA tonometer is automatic to a substantial degree, it is possible to expect a lesser influence of the operating person (this assumption is documented e.g. by the results of (23)) in contrast with measurement on ICARE PRO. In the case that each measurement is performed by a different operator, it is therefore possible to expect worse repeatability in the case of ICARE PRO and only minimal changes in the case of ORA.
CONCLUSION
The results of this study have demonstrated that upon measurement of intraocular pressure using ICARE PRO and ORA tonometers, the results are influenced above all by corneal hysteresis and central corneal thickness. Upon markedly deviating values of these parameters from the average, a distortion of the measurement result may therefore occur. In this the observed influence of corneal thickness may indirectly reflect the influence of corneal rigidity, which is directly proportionate to corneal thickness. From the presented results it also ensues that the values from both observed instruments cannot be mutually interchanged, and therefore e.g. upon observation of changes of IOP over time it is necessary always to use the same type of instrument. In this, upon use by the same operator, ICARE PRO recorded comparable repeatability with a Goldmann applanation tonometer, in the case of IOPG repeatability is slightly worse, and conspicuously worse in the case of IOPCC.
Acknowledgement
This study was supported by the project 16RPT03 inTENSE within the European Metrology Programme for Innovation and Research (EMPIR). EMPIR is co-financed by the Horizon 2020 programme of the European Union for research and innovations and states participating in the EMPIR programme. It also obtained support from the VEGA project (1/0556/18), entitled “Ensuring Metrological Control of Intraocular Pressure Gauges”.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Zdroje
1. Bland, JM., Altman, DG.: Statistical methods for assessing agreement between two methods of clinical measurement. Lancet, 327(8476); 1986 : 307-10.
2. Brusini, P., Salvetat, ML., Zeppieri M. et al: Comparison of ICare tonometer with Goldmann applanation tonometer in glaucoma patients. J Glaucoma, 15(3); 2006 : 213-7.
3. Chui, WS., Lam, A., Chen, D. et al.: The influence of corneal properties on rebound tonometry. Ophthalmology, 115(1); 2008 : 80-4.
4. Cymerman, A., Rock, PB., Muza, R. et al.: Intraocular pressure and acclimatization to 4300 m altitude. Aviat Space Envir Med, 71(10); 2000 : 1045-50.
5. Çevik, SG., Kıvanç, SA., Akova-Budak, B. et al.: Relationship among Corneal Biomechanics, Anterior Segment Parameters, and Geometric Corneal Parameters. J Ophthalmol; 2016 : 8418613.
6. Deol, M., Taylor, DA., Radcliffe, NM.: Corneal hysteresis and its relevance to glaucoma. Curr Opin Ophthalmol, 26(2); 2015 : 96-102.
7. Ersanli, D, Yildiz, S., Sonmez et al.: Intraocular pressure at a simulated altitude of 9000 m with and without 100% oxygen. Aviat Space Environ Med, 77(7); 2006 : 704-6.
8. Fernandes, P., Díaz-Rey, JA., Queirós A. et al.: Comparison of the ICare rebound tonometer with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt, 25(5); 2005 : 436-40.
9. Gandhi, NG, Prakalapakorn, SG, El-Dairi, MA et al.: Icare ONE rebound versus Goldmann applanation tonometry in children with known or suspected glaucoma. Am J Ophthalmol, 154(5); 2012 : 843-849.
10. Gillan, WDH: Intra-ocular pressure measurements using the Ocular Response Analyser and ICare tonometer: A comparison. Afr Vision Eye Health, 74(1); 2015 : 29.
11. Hagishima, M., Kamiya, K., Fujimura, F. et al.: Effect of corneal astigmatism on intraocular pressure measurement using ocular response analyzer and Goldmann applanation tonometer. Greafes Arch Clin Exp Ophthalmol, 248(2); 2010 : 257-62.
12. Hladíková, E., Pluháček, F., Marešová, K.: Porovnání měření nitroočního tlaku ICARE PRO® tonometrem a Goldmanovým aplanačním tonometrem. Cesk Slov Oftalmol, 70(3); 2014 : 90-3.
13. Iliev, ME., Goldblum, D., Katsoulis, K. et al.: Comparison of rebound tonometry with Goldmann applanation tonometry and correlation with central corneal thickness. Br J Ophthalmol, 90(7); 2006 : 833-5.
14. Jorge, JM., González-Méijome, JM., Queirós, A. et al.: Correlations between corneal biomechanical properies measured with the ocular response analyzer and ICare rebound tonometry. J Glaucoma, 17(6); 2008 : 442-8.
15. Karadag, R., Sen, A., Golemez, H. et al.: The effect of short-term hypobaric hypoxic exposure on intraocular pressure. Curr Eye Res, 33(10); 2008 : 864-7.
16. Kaushik, S., Pandav, SS.: Ocular Response Analyzer. J Curr Glaucoma Pract, 6(1); 2012 : 17-9.
17. Kirstein, EM., Elsheikh, A., Gunvant, P.: Tonometry – past, present and future. In Gunvant, P. (Ed), Glaucoma - current clinical and research aspects. InTech, 2011, p. 85-108.
18. Kontiola, A.: A new electromechanical method for measuring intraocular pressure. Doc Ophthalmol, 93(3); 1997 : 265-76.
19. Malini, B., Rajendra, R, Anita, G. et al.: A study of correlation between central corneal thickness and intra ocular pressure measurement using Goldmann applanation tonometer and rebound tonometer. IOSR-JDMS, 13(2); 2014 : 70-80.
20. Martinez-de-la-Casa, JM., Gracia-Feijoo, J., Fernandez-Vidal, A. et al.: Ocular response analyzer versus Goldmann applanation tonometry for intraocular pressure measurements. Invest Ophthalmol Vis Sci, 47(10); 2006 : 4410-4.
21. Martinez-de-la-Casa, JM., Gracia-Feijoo, J., Castillo, A. et al.: Reproducibility and clinical evaluation of rebound tonometry. Invest Ophthalmol Vis Sci, 45(12); 2005 : 4578-80.
22. Moreno-Montañés, J, García, N., Fernández-Hortelano, A. et al.: Rebound tonometer compared with Goldmann tonometer in normal and pathologic corneas. Cornea, 26(4); 2007 : 427-30.
23. Moreno-Montañés, J., Maldonado, MJ., Gracía, N. et al.: Reproducibility and clinical relevance of the ocular response analyzer in nonoperated eyes: corneal biomechanical and tonometric implications. Invest Ophthalmol Vis Sci, 439(3); 2008 : 968-74.
24. Munkwitz, S, Elkarmouty, A, Hoffman, EM et al.: Comparison of the ICare rebound tonometer and the Goldmann applanation tonometer over a wide IOP range. Graefes Arch Clin Exp Ophthalmol, 246(6); 2008 : 875-9.
25. Najmanová, E., Pluháček, F., Botek, M.: Intraocular pressure response to maximal exercise test during recovery. Optom Vis Sci, 95(2); 2018 : 136-42.
26. Najmanová, E., Pluháček, F., Botek, M.: Intraocular pressure response to moderate exercise during 30-min recovery. Optom Vis Sci, 93(3); 2016 : 281-5.
27. Najmanová, E., Pluháček, F., Botek, M. et al.: Intraocular pressure response to short-term extreme normobaric hypoxia exposure. Front Endocrinol, 9; 2018 : 785
28. Nakamura, M., Darhad, U., Tatsumi, Y. et al.: Agreement of rebound tonometer in measuring intraocular pressure with three types of applanation tonometers. Am J Ophthalmol, 142(2); 2006 : 332-4.
29. Pakrou, N., Gray, T, Mills, R. et al.: Clinical comparison of Icare tonometer and Goldmann applanation tonometry. J Glaucoma, 17(1); 2008 : 43-7.
30. Pavlidis, M., Stupp, T., Georgalas, I. et al.: Intraocular pressure changes during high-altitude acclimatization. Greafes Arch Clin Exp Ophthalmol, 244(3); 2006 : 298-304.
31. Pluháček, F., Siderov, J.: Mesopic visual acuity is less crowded. Greafes Arch Clin Exp Ophthalmol, 256(9); 2018 : 1739-46.
32. Prata, TS., De Moraes, CG., Kanadani, FN. et al: Posture-induced intraocular pressure changes: considerations regarding body position in glaucoma patients. Surv Ophthalmol, 55(5); 2010 : 445-53.
33. Read, SA., Collins, MJ.: Water drinking influences eye length and IOP in young healthy subjects. Exp Eye Res, 91(2); 2010 : 180-5.
34. Salcedo, H., Arciniega, D., Mayorga, M. et al.: Role of the water-drinking test in medically treated primary open angle glaucoma patients. J Fr Ophthalmol, 41(5); 2018 : 421-4.
35. Shin, J., Lee, JW., Kim, EA. et al: The effect of corneal biomechanical properties on rebound tonometer in patients with normal-tension glaucoma. Am J Ophthalmol, 159(1); 2015 : 144-54.
36. Sullivan-Mee, M., Gerhardt, G., Halverson, KD. et al.: Repeatability and reproducibility for intraocular pressure measurement by dynamic contour, ocular response analyzer, and Goldmann applanation tonometry. J Glaucoma, 18(9); 2009 : 666-73.
37. Susanna, CN., Susanna, R. Jr, Hatanaka, M. et al.: Comparison of intraocular pressure changes during the water drinking test between different fluid volumes in patients with primary open-angle glaucoma. J Glaucoma, 27(11); 2018 : 950-6.
38. Vera, J., Jiménez, R., Redondo, B. et al.: Fitness level modulates intraocular pressure response to strength exercises. Curr Eye Res, 43(6); 2018 : 740-6.
39. Wang AS., Alencar, LM., Weinreb, RN. et al.: Repeatability and reproducibility of Goldmann applanation, dynamic contour and ocular response analyzer tonometry. J Glaucoma, 22(2); 2013 : 127-32.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 3- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
-
Všechny články tohoto čísla
- Vliv rohovky na měření nitroočního tlaku tonometry ICARE PRO a ORA
- Využití optické koherenční tomografie u pacientů s útlakem optického chiasmatu
- Možnosti zlepšení zrakových funkcí u pacientů se stabilní makulopatií-pilotní výsledky nové studie
- Ranibizumab v léčbě choroidální neovaskularní membrány z jiné příčiny než věkěm podmíněná makulární degenerace
- Anomálie funkcie zrenice u detských pacientov – 2 kazuistiky
- Selektivní angiografie s možností trombolýzy u nemocných s okluzí arteria centralis retinae
- Doc. MUDr. Karel Kuběna, CSc. - zemřel
- 23. Zimný kongres ESCRS
- Kongres SOE
- Očná klinika Lekárskej fakulty Univerzity Komenského v Bratislave oslavuje 100-té výročie činnosti – 2. časť
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Anomálie funkcie zrenice u detských pacientov – 2 kazuistiky
- Vliv rohovky na měření nitroočního tlaku tonometry ICARE PRO a ORA
- Možnosti zlepšení zrakových funkcí u pacientů se stabilní makulopatií-pilotní výsledky nové studie
- Ranibizumab v léčbě choroidální neovaskularní membrány z jiné příčiny než věkěm podmíněná makulární degenerace
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



