-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Corticosteroid Induced Posterior Subcapsular Cataract
Authors: J. Kačmař; D. Cholevík
Authors place of work: Gemini oční klinika, a. s., přednosta: MUDr. Pavel Stodůlka, Ph. D., FEBOS-CR
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 6, p. 226-232
Category: Původní práce
doi: https://doi.org/10.31348/2018/6/2Summary
Objective:
A description of the development of a clinical ocular finding of 23 patients (35 eyes) with steroid-induced posterior subcapsular cataract of different source, focusing on its character and mechanism of origin.
Methods:
The medical records of 23 patients, 14 women, 9 men, median age 44.5 years (median 44 years, interval 29 - 52 years) were evaluated retrospectively and had undergone surgery from 5/2016 to 5/2018 at Gemini Eye Clinic Bělský les. All patients underwent a complex eye examination and cataract surgery with artificial intraocular lens implantation.
Results:
In all of these patients, the incidence of the various stages of the posterior subcapsular cataract was correlated with the use of steroid therapy locally, generally per os, inhaled or combined, mainly in pre-adolescent patients. Postoperatively, a significant improvement in CDVA (corrected distance visual acuity) was observed in all patients in the set.
Conclusion:
Steroid-induced cataract is a clinical diagnosis reserved for conditions of cataract formation in relation to the dose and duration of use of corticosteroid medication. The diagnostic diagram of this process seems to be unambiguous, requires a thorough examination of the ocular finding and carefuly obtain internal and pharmacological history of the patient. The basic treatment approach is cataract surgery, which should be performed by an experienced surgeon for a higher risk of possible complications.
Keywords:
posterior subcapsular cataract – corticoids – presenilic age – side effects
INTRODUCTION
Cataract is characterised as opacity of the lens, which subjectively causes a deterioration of visual acuity in the patient. We define visual acuity as the ability to distinguish details which we observe and which are displayed on the retina in a certain place and size. Cataract remains one of the main causes of damage to the sight of the patient, leading to a deterioration in the patient's quality of life, and in addition has a considerable economic impact on the entire society. In terms of the number of performed procedures, surgery leading to the removal of a cataract remains one of the most financially costly operations in Europe and Western countries [19].
Despite the fact that in the majority of cases this concerns a physiological process in connection with the ageing of the lens, its premature incidence and progression is often described in connection with the pathology diabetes mellitus, high blood pressure, obesity, smoking and excessive consumption of alcohol, as well as previous injuries or inflammations of the eye, undergone eye surgery, and also long-term use of a wide spectrum of pharmaceuticals. In ophthalmology this concerns medications on the basis of corticosteroids used systemically in tablet form, or in the form of subconjunctival, periocular, intraocular or intravitreal injections, in the form of inhalation sprays and topical medications. Use is also dependent upon the predominant mechanism of effect of the individual substances, in ophthalmology this acts in order to suppress inflammatory reactions of the anterior segment and post-traumatic changes. The occurrence of steroid-induced cataract is influenced to a certain degree by the amount, length and manner of administration of the medication. Susceptibility to the incidence of cataract, as well as several other pathologies, as a consequence of the use of corticoids is variable in different individuals [17, 15].
The link between cataract and use of corticoids was first described by Black et al. [3]. In their study they observed a link between the incidence of posterior subcapsular cataract (PSC) in patients with rheumatoid arthritis treated with corticoids. They described the following dependency: the higher the dose, the greater the prevalence of incidence of PSC. Furthermore, they presented the hypothesis that if the dose of medication does not exceed 10 mg of Prednisone per day, the risk of occurrence of cataract is essentially minimal.
Over the course of time, the opinion came to predominate that no safe minimum dose of corticoid exists, mainly due to variable patient sensitivity and potential genetic predisposition [21].
A number of theories exist concerning the mechanism of origin of steroid-induced cataract, primarily due to changes of osmotic balance and regulatory systems, the influence of oxidation stress caused by free radicals, direct modification of proteins or due to complex metabolic breakdown [16].
Recently the opinion has predominated that glucocorticoids are covalently bonded to proteins of the lens, which leads to a deeper destabilisation of the structure of the protein, enabling further modification (i.e. oxidation) leading to the onset of cataract [9].
In addition to the risk of cataract, the frequently occurring adverse effects of corticoids include the onset of iatrogenic, secondary open-angle glaucoma. In their study from 1950, Gordon and McLean [11] described the formation of secondary glaucoma in patients treated systemically with the aid of adrenocorticotropic hormone (ACTH), and subsequently Francois [10] demonstrated the same also following local therapy, which probably leads to changes of the structure of the trabecular meshwork. The induced changes are accompanied by an elevation of intraocular pressure, which typically increases after a number of weeks of continual dosage, and in the majority of cases returns to normal after the termination of treatment.
Following long-term unsupervised use, this may not infrequently result in an elevation of pressure leading to irreversible changes on the optic nerve and a deterioration of visual functions, leading to total blindness. Cantrill et al. [5] observed and described a difference in the level of steroid response, in this case an elevation of intraocular pressure, depending on the strength of the known and frequently used pharmaceuticals. (table 1)
Tab. 1. Increase in intraocular pressure depending on the type of medicinal product (source: Cantrill et al.) 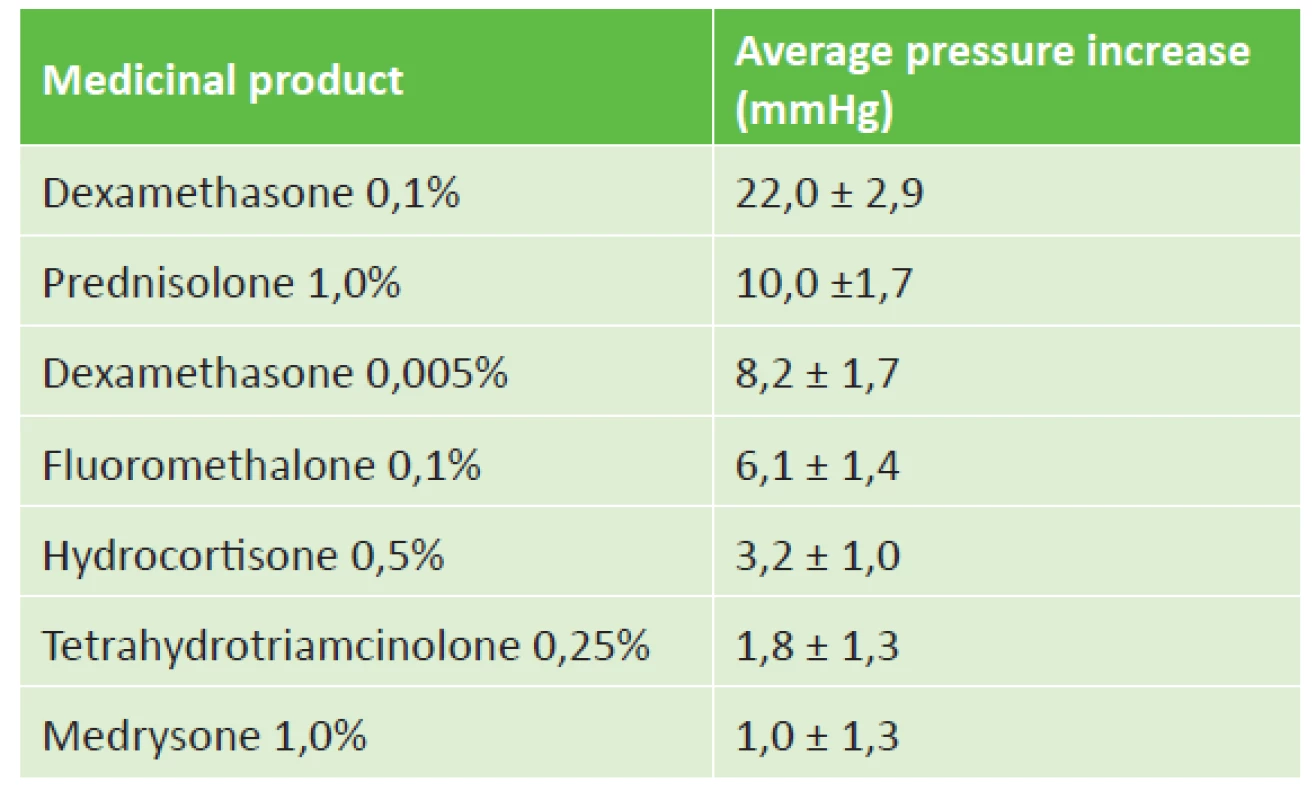
It is necessary to include in this consideration patients known as "steroid responders", in whom even a small dose of corticosteroids or brief duration of treatment may lead to an incommensurate increase of intraocular pressure. In clinical practice it is necessary to first of all identify these risk patients, above all by frequent measurement of intraocular pressure, and to apply anti-glaucomatous therapy in a timely manner. It is often essential also to adjust the treatment with corticosteroid preparations in such a manner as to ensure that the effect of increased intraocular pressure does not cause irreversible damage to the eye.
Corticosteroids suppress the defensive capabilities of tissues, and as a result it is necessary to approach their application in the treatment of ocular infections with caution. Their effect may frequently mask the development of bacterial, viral or fungal infections, prolong their duration and thus impede their treatment. Long-term use of local corticoid therapy demonstrably retards the healing of the corneal epithelium, leading to its thinning due to the inhibition of collagen synthesis, and in extreme cases to perforation of the cornea. As a result, in the initial stages corticoids are also on principle contraindicated for the treatment of corneal ulcers and viral infections.
New hope for minimising the risk of use of corticoids appears to be offered by directly influencing growth factors, which could to a certain extent also bring a broadening of the spectrum of safe use of corticoids and a reduction of the potential occurrence of accompanying adverse effects.
METHOD
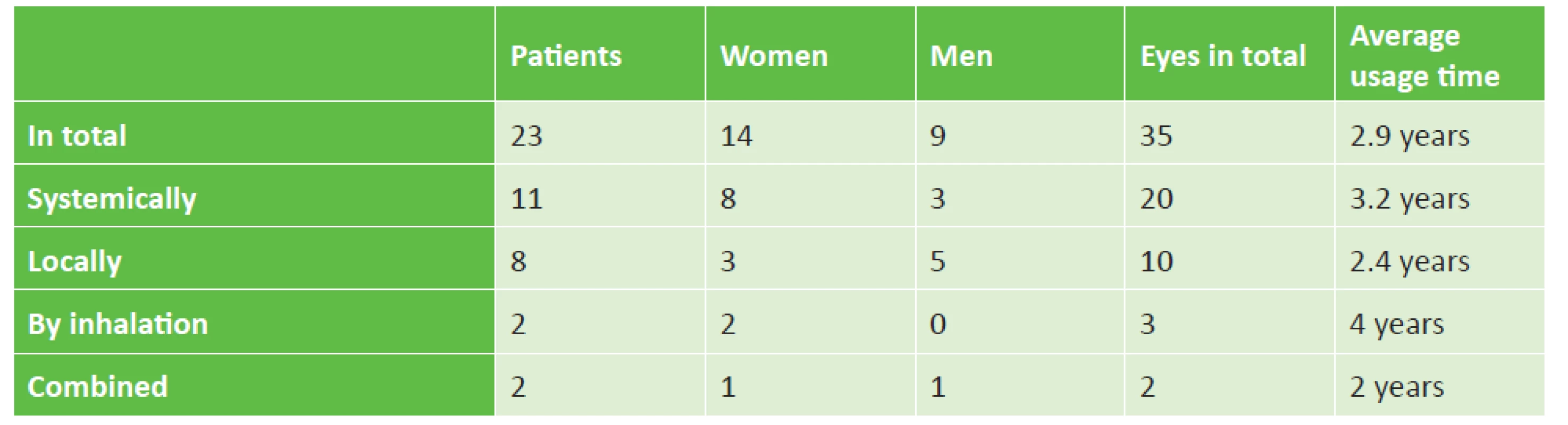
The cohort comprised 23 patients, of whom 14 were women and 9 men, with a finding of steroid-induced posterior subcapsular cataract, operated on at the Gemini Eye Clinic at Bělský les, Ostrava. The average age of the patients in the cohort was 44.5 years (median 44 years, interval 29-52 years). The average duration of use of corticoids differed depending on the method of application of the medication.
The cohort included only patients of a pre-senile age with posterior subcapsular cataract in various stages, with a demonstrable link of its origin to the use of corticosteroid therapy in various forms of application. It did not include patients with other types of opacities of the lens, in whom it was not possible to determine unequivocally whether the onset of the opacity was contributed to by other factors.
(table 2)
All the patients underwent an examination of uncorrected and corrected distance visual acuity on LCD optotypes, and near vision with the aid of Jaeger tables. Intraocular pressure was examined by a noncontact method using the instrument Tonoref II, Nidek. A comprehensive ocular examination of the anterior segment was conducted on a slit lamp YZ56, 66 Vision – Tech, and an examination of pupil reactions. In patient with recurring iridocyclitis we recorded only a minimally limited reaction to illumination in comparison with the other patients in the cohort.
There followed an examination of the posterior segment in artificial mydriasis induced by a combination of Unitropic 1% gtt. (tropicamide) + Neosynephrin-pos 10% gtt. (phenylephrine hydrochloride) applied at regular intervals, 1 drop every 10 minutes until mydriasis was induced. A biomicroscopic examination of the ocular fundus with the aid of an indirect lens (VOLK 60–90 D) did not detect any pathological change which could explain a decrease in visual acuity in our cohort.
In 6 eyes the condition of the cataract did not permit a detailed examination of the ocular fundus, and as a result this was supplemented by an ultrasound B-scan examination using the instrument US-4000, Nidek. In all cases the vitreous area was anechogenic, without signs of retinal detachment or any other pathological process.
An examination was conducted on a static automatic perimeter Cenerfield 2, Oculus. However, in 6 patients the results were not significant due to the pronounced degree of PSC, and could not be evaluated. In all the other patients the accompanying finding was recorded in the sense of a deterioration of contrast sensitivity to blind spots in the central part of the visual field.
A no less fundamental component of the ophthalmological examination was to carefully obtain an internal and pharmacological anamnesis, focusing on the dose, method of administration and duration of use of corticoids. The cohort of treated patients was then further divided into 4 groups according to the method of administration.
The first group included a total of 11 patients, 20 eyes with systemically, per os administered corticoids. The average period of use was 3.2 years, in which the shortest time was 2 years and the longest 7 years, in an average dose of 7 mg of methylprednisolone per day. The most common reason for treatment with corticoids was rheumatoid arthritis in 5 cases, followed by psoriasis vulgaris, polyneuropathy, antiphospholipid syndrome and condition following brain surgery.
The second group included 2 patients, 3 eyes, in whom a causal connection was demonstrated with inhalation administration of the corticoid beclomethasone dipropionate for the treatment of a severe form of asthma over a period of use of at least 5 years.
The third group comprised 2 patients, 2 eyes, with combined therapy of severe atopic eczema in the form of ointment and injection administration over a period shorter than 2 years.
The fourth group included 8 patients, 10 eyes, treated locally with ointment and drops. These were primarily patients with frequently recurring incidence of iridocyclitis and chronic inflammations of the conjunctivas. In one case this concerned unprompted use of combined medication in the form of the ointment Maxitrol (neomycin+polymyxin B+dexamethasone) for the treatment of chronic chalazion with a duration of 2 years. Another case concerned a female patient with atopic eczema treated for 3 years as chronic with intermittent application of the ointment Elocom (mometasone-furoate) into the area of upper and lower eyelids and periocular region. (graph 1)
Graph 1. Percentage representation of patients in the group according to the route of administration of corticosteroids 
In the period from 5/2016 to 5/2018, cataract surgery was performed on all 35 eyes, with the implantation of a hydrophilic artificial intraocular lens. The indication for surgery was posterior subcapsular cataract of various grades, evaluated and divided according to the Crews [6] classification of PSC from 1963, which to a certain extent reflects the ratio of the degree of opacity of the lens and the dose of corticoid. (table 3)
Tab. 3. Ratio of opacity of the lens to the corticosteroid dose (source: Crews et al.) 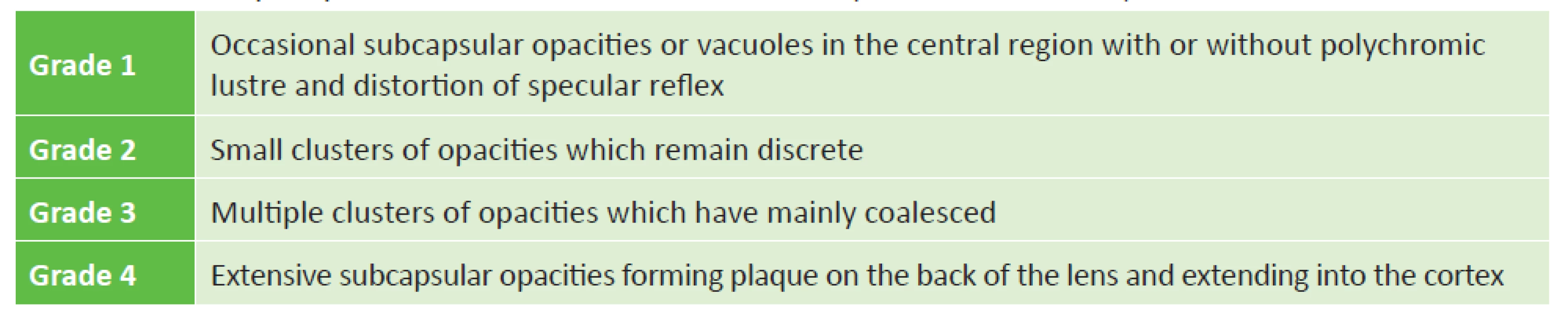
In our observed cohort there was a predominance of occurrence of posterior subcapsular cataract of 2nd - 3rd grade, in two patients we observed a 4th grade cataract. (fig. 1)
Fig. 1. Image of 3rd grade posterior subcapsular cataract according to Crews 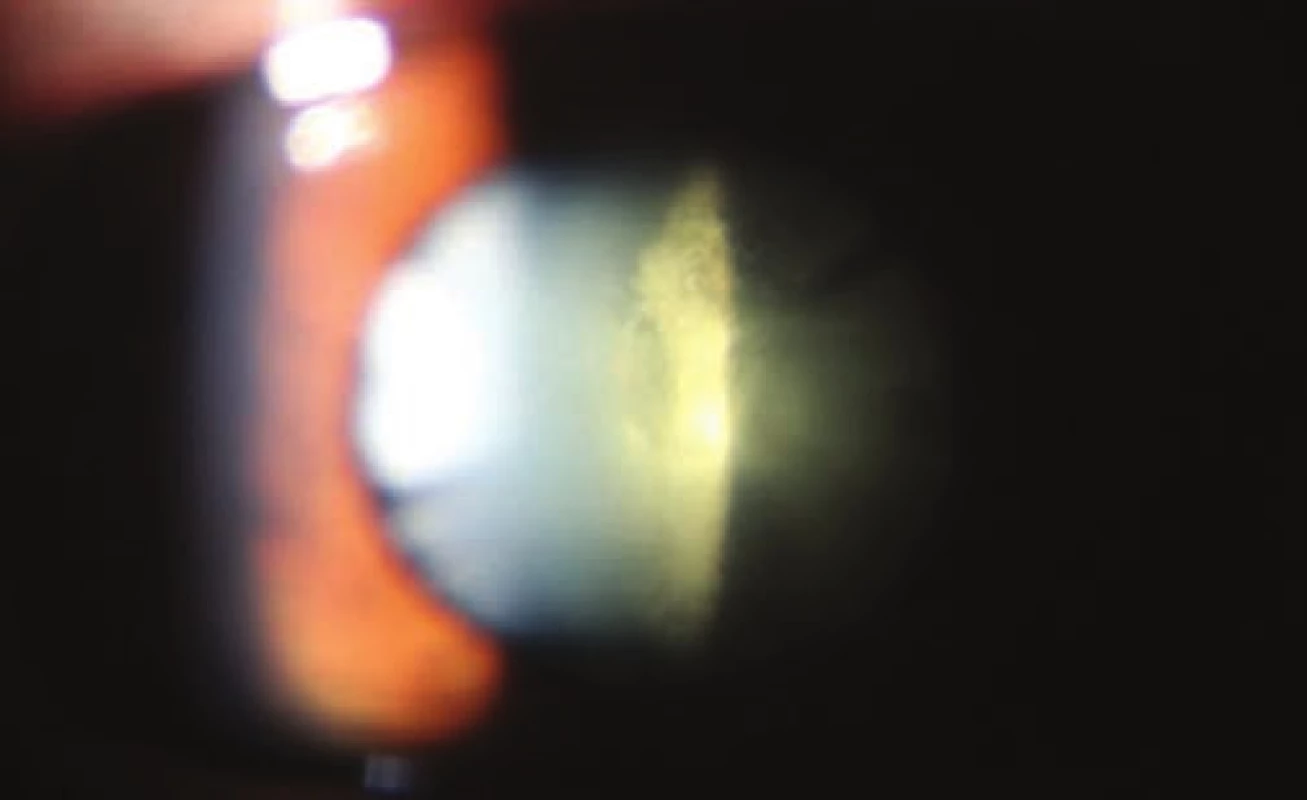
Cataract surgery was performed on all eyes by the standard method of phacoemulsifcation, and in 33 cases a monofocal hydrophilic lens was implanted. In 2 cases a trifocal hydrophilic intraocular lens FineVision, PhysIOL was implanted. The calculation of the intraocular lens was performed on the instrument IOL Master 5000, Zeiss, in combination with ultrasonic biometry on the instrument US-4000, Nidek, with keratometry on the instrument CEM-530, Nidek.
All the patients were operated on by a single surgeon using the instrument Stellaris, Bausch & Lomb. In all cases the surgical procedure took place without complications.
The postoperative treatment included application of the combined preparation Tobradex (tobramycin/dexamethasone), 1 drop 5 times a day for the first 3 days, then 3 times a day until the completion of treatment. In the case of patients with historically demonstrated incidence of iridocyclitis, application of the pharmaceutical Yellox (bromfenac sodium sesquihydrate), 1 drop twice a day until completion of treatment, was added to the therapy. During the course of regular follow-up examinations – 1 day, 1 week, 1 month and 3 months after the procedure, it was not necessary to adjust the given treatment.
In 4 eyes there was pronounced fibrosis of the posterior capsule. In these cases YAG capsulotomy was performed in the early postoperative period on the instrument YC 1800, Nidek.
RESULTS
The average value of corrected distance visual acuity (CDVA) of all patients before surgery in decimal values was 0.36, within the range of worst CDVA on the level of light perception with erroneous light projection and best CDVA of 0.8. The average value of CDVA after surgery was 0.94. There was a significant improvement of CDVA in all patients in the cohort. (graph 2)
Graph 2. Corrected distance visual acuity before and after posterior subcapsular cataract surgery 
The average value of intraocular pressure before cataract surgery was 14.28 mmHg. The resulting value of intraocular pressure one month after surgery was 14.22 mmHg. We did not record any elevation or instability of intraocular pressure either preoperatively or postoperatively. We did not register the occurrence of secondary glaucoma in dependency on the use of corticoids in any of the observed groups. (graph 3)
Graph 3. Development of intraocular pressure before and after cataract surgery 
In patients with historically demonstrated incidence of iridocyclitis there was no reactivation of the pathology in the postoperative period, and no postoperative occurrence of cystoid macular edema (CME). The further postoperative course in all the operated patients was without significant noteworthy features, as was the supplemented postoperative finding on the ocular fundus.
DISCUSSION
Corticosteroids are steroid hormones synthesised from cholesterol in the adrenal cortex. Their synthetic analogue, corticoids, became widely used in medicine from the 1850s due to their anti-inflammatory, anti-allergic, anti-edematous and immunosuppressant effect [23, 4].
The first record of systemic use of corticoids dates from 1948, on a female patient with severe form of rheumatoid arthritis admitted to the Mayo Clinic, Rochester, Minnesota, USA. This was a 29-year-old female patient with severe to destructive damage to the joints, as a result of which she was virtually incapable of movement and was thus referred for hospital care. Treatment was commenced on this patient with everyday application of 100 mg of “compound E” (17-hydroxy-11-dehydrocorticosterone). After one week there was a significant reduction of swelling, muscle and joint rigidity and pain. The condition of the muscular and joint apparatus improved to such an extent that in the following days the patient was able to go shopping by herself in the local shopping centre [13].
Over the course of time the spectrum of application of corticoids in medicine was dramatically extended, in some fields to such an extent that they became the drug of first choice for several pathologies. However, new observations on the effect of corticoids opened up a discussion concerning their potential adverse systemic and local effects on the organism. In fact, at present the prevailing opinion is that after diabetes, myopia and glaucoma, steroid-induced cataract is the fourth most common cause of occurrence of secondary cataract.
The first to describe these adverse effects of corticoids in the treatment of rheumatoid arthritis were Black et al. [3]. In their study on a cohort of 44 patients with rheumatoid arthritis treated with systemically with corticoids, they described a 39% incidence of various stages of PCS. These were very diverse cataracts, which were nevertheless so characteristic to a certain extent that Oglesby et al. [18] described them in their study as “cataract developing in the area of the posterior pole between the cortex and posterior capsule, with frequent forward propagation in an irregular manner. The edges are most frequently sharp, but occasionally surrounded by a fine, greyish haze. The fine structure was composed of small, whitish crystals separated by similarly small vacuoles, which in combination may form a grainy agglomeration, occasionally manifesting a linear composition or joining together in a number of larger vacuoles. Inside they often contained particles of light blue, green or red colour.”
Black furthermore expressed the hypothesis that if the duration of treatment did not exceed 1 year and the dose 10 mg of prednisone per day, the risk of occurrence was essentially minimal [3]. In our cohort of patients treated with corticoids administered generally, the average dose was 7mg of methylprednisolone per day over an average period of 3.2 years. Calculation to the dose of prednisone (9 mg) appears to confirm the assertion [17, 21] that there is essentially no safe minimum dose limit of a corticoid which could not lead to the onset of cataract, mainly due to variable sensitivity and potential genetic predisposition on the part of the patient. (table 4)
Tab. 4. Corticosteroid dose equivalents (source: Medscape) 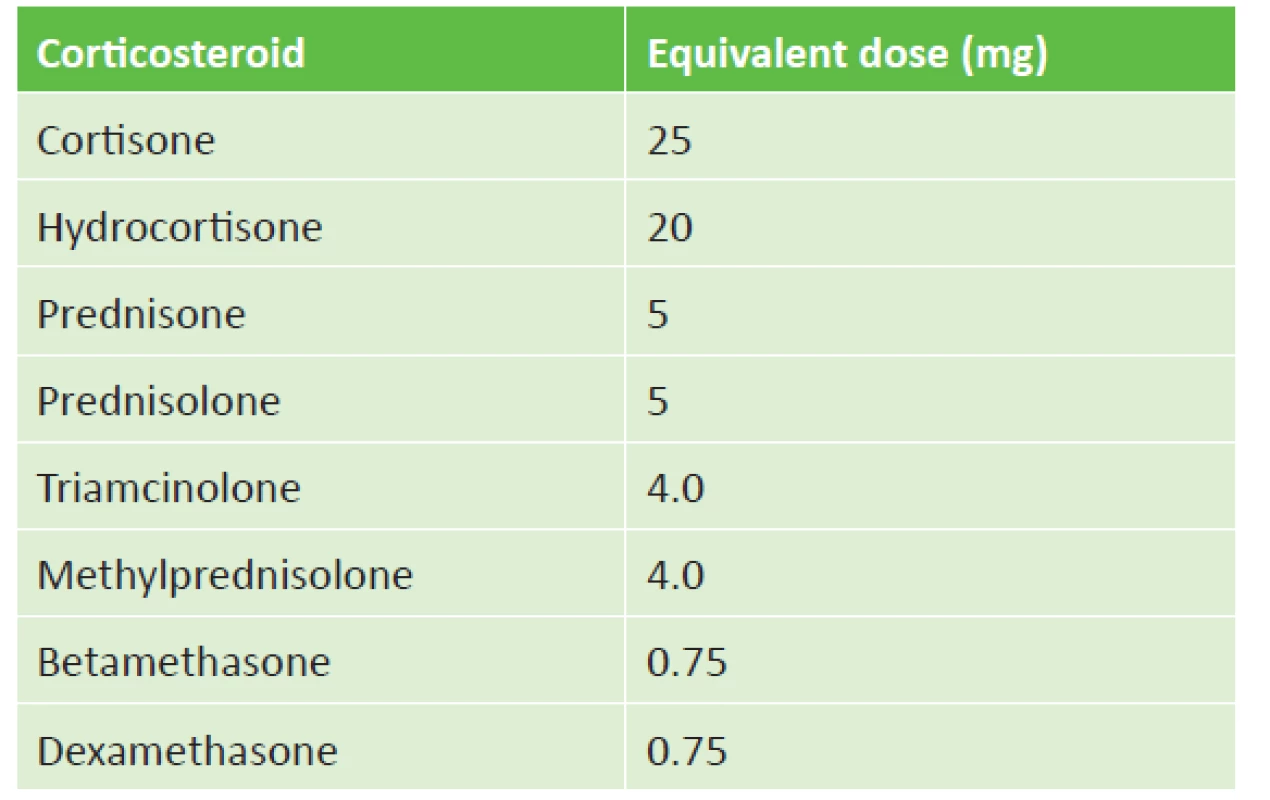
The use of corticoids was progressively extended not only within the framework of treating a broader spectrum of pathologies, but also in terms of the method of their administration. For example, more than sixty years have elapsed since the first successful use of the corticosteroid hydrocortisone for the external treatment of eczema, and this discovery represented the greatest revolution to date in the treatment of various inflammatory and proliferative dermatoses. Nowadays it is impossible to imagine the treatment of a number of skin complaints without corticosteroids, even though the risks of the adverse effects ensuing from their use are very well known [22].
A similar situation applied in ophthalmology, in which corticoids began to be widely used in order to suppress inflammatory reactions of the anterior segment, as well as post-traumatic changes. Similarly as with corticoids administered generally, in local treatment there applies a dependency on the amount and length of use. Intraocular inflammatory pathologies as such may contribute to the development and progression of cataract, and it is therefore often virtually impossible to separate the degree of effect. In these cases cataract surgery is demanding, connected with a higher percentage of possible and often unforeseeable complications. Historically these operations have been accompanied by severe postoperative inflammations, hypotonia, and in extreme cases phthisis of the eyeball. A contribution to minimising the perioperative and postoperative risks was undoubtedly made by a deeper understanding of the course of the pathology, optimisation of the therapeutic process, minimal invasiveness of the procedure, the design and material of the implanted lenses, and above all the experience of the operating surgeon in dealing with potential ensuing complications and the ability to respond to them appropriately by adjusting the surgical technique [2].
The essential basis of a good result is to identify the right time to perform the operation and thereby minimise not only the danger of potential postoperative complications, but also the risk of occurrence of CME. Our approach to our cohort of patients was in accordance with the rule of not operating within a period of at minimum 3 months from the last reactivation of the pathology. The basis was a pacific preoperative finding, which persisted in the observed cohort of patients up to the late postoperative period – an observation period of at least 3 and at longest 6 months from the operation.
Corticoids may have specific adverse effects, and may be administered to the eye by various methods. In the case of administration by inhalation, the introduction of therapy by inhaled corticosteroids into medical practice at the end of the 1980s was the most significant milestone in the history of the treatment of bronchial asthma. Inhaled corticoids are responsible for a significant reduction in morbidity and mortality in patients with this pathology. At present these corticoids are considered the most effective anti-inflammatory preventive anti-asthmatic agents, and are the drug of first choice for all age categories [14].
Despite substantial efforts on the part of the pharmaceutical industry, to date no new treatment has been discovered which could approximate the efficacy of inhaled corticoids. As a result, at present they are used far more frequently, in larger doses and at longer intervals than at any time previously. This trend is accompanied by increasing concerns with regard to the potential systemic as well as local adverse effects of inhaled corticoids. At present only a proportion of 10-40% of the dose is processed by the respiratory system, whereas the remainder passes through and is absorbed by the digestive tract [11].
The current trend is an endeavour to develop an “ideal inhaled corticoid” which could act only in the required locality with a minimal systemic effect, maximum efficacy and therefore the possibility of reducing the final dose [1].
In our group of patients treated with the inhaled corticoid beclomethasone dipropionate we recorded PSC in stage 2-3, despite the fact that the dose of the corticoid within the framework of the estimated daily dose for adults and children from the age of 12 was minimal, application of the course of several years probably produced a cumulative effect, which led to the onset of pre-senile cataract [20].
Saag et al. [20], according to a cross-sectional urban population study of 4433 patients in the region to the west of Sydney, expect the highest prevalence of incidence of posterior subcapsular cataract in the case when the total dose of beclomethasone is higher than 2000 mg.
Similarly, Cumming et al. [8] in their cross-sectional population study of 3654 patients from Austria confirm a dependency of the incidence of PSC in correlation with a cumulative effect of inhaled corticoid. Furthermore, they also come to the conclusion that the prevalence of incidence is as much as 27% higher in those patients in whom the total dose of corticoid exceeded 2000 mg.
The size of the dose and the prolonged cumulative effect therefore plays a significant role in the potency of the onset of corticoid-induced cataract. In the overall view it is necessary also to take into account the possibility of combined administration of corticoids, with which there increases the problem of differentiating the mechanism of origin of the adverse effects [7].
In our cohort of patients treated for severe atopic dermatitis by a combination of ointment and injection administration, it was no less problematic to determine and separate the degree of effect. However, we know for certain that this cohort manifested the most severe symptoms and stages of PSC within the shortest time of effect from the beginning of application. In one case of a female patient with vision on the level of light perception with unclear projection, we were faced with a more complex decision as to whether to perform the operation, and it was difficult to respond adequately to the patient's question concerning whether the operation would bring any improvement of vision whatsoever. An irreplaceable role in the decision-making process was played by ultrasound examination, which demonstrated only minute hyperechogenicity in the vitreous area. Despite the fact that the patient's postoperative vision of 1.0 decimal CDVA and the physiological finding on the posterior segment ultimately exceeded the given expectations, it can be asserted that as regards the incidence of adverse effects, combined therapy presents the greatest risk.
CONCLUSION
The results of surgery on corticoid-induced cataract in our cohort are comparable with the results of operations on senile cataract. Timely diagnosis and subsequent surgery brings not only a solution to the patient's subjective complaints, but also an early return of the patient to productive life. As in the case of surgery on senile cataract, it therefore represents an effective solution to the given pathology.
It is necessary to emphasise that although corticosteroids are in many respects an irreplaceable component of the treatment of a wide spectrum of pathologies, they also represent a figurative trigger of potential risks and adverse effects of use.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received by the Editorial Department on: 20 July 2018
Accepted for printing on: 16 December 2018
MUDr. Kačmar
Gemini oční klinika, a.s.
Zdroje
1. Allen, DB., Bielory, L., Derendorf, H. et al.: Inhaled corticosteroids: past lessons and future issues. J Allergy Clin Immunol, 112; 2003 : 1-40.
2. Agrawal, R., Murthy, S., Ganesh, SK. et al.: Cataract Surgery in Uveitis. [online] Int J Inflam. 548453; 2012: dostupné z www <http://doi.org/10.1155/2012/548453>
3. Black, RL., Oglesby, RB., Sallmann, L. et al.: Posterior subcapsular cataracts induced by corticosteroids in patients with rheumatoid arthritis. JAMA, 174; 1960 : 150-155.
4. Bureš J, Horáček J.: Základy vnitřního lékařství. Praha, Galén 2003 : 870.
5. Cantrill, HL., Palmberg, PF., Zink, HA. et al.: Comparison of in vitro potency of corticosteroids with ability to raise intraocular pressure. Am J Ophthalmol, 79; 1975 : 1012–1017.
6. Crews, S. J.: Posterior Subcapsular Lens Opacities in Patients on Long-term Corticosteroid Therapy. BMJ, 1(5346); 1963 : 1642.2–1647.
7. Cumming, RG., Mitchell, P.: Inhaled corticosteroids and cataract: prevalence, prevention and management. Drug Saf. 20; 1999 : 77–84.
8. Cumming, RG., Mitchell, P., Leeder, SR.: Use of inhaled corticosteroids and the risk of cataracts. N Engl J Med, 337(1); 1997 : 8-14.
9. Dickerson, JE. Jr., Dotzel, E., Clark, AF.: Cataract: New Perspectives from In vitro and Lens Culture Studies. Exp Eye Res, 65; 1997 : 507–516.
10. François, J., Victoria-Troncoso, V.: Corticosteroid Glaucoma. Ophthalmologica, 174; 1977 : 195-209.
11. Global strategy for asthma management and prevention. [online] Global Initiative for Asthma. Updated 2018: dostupné z WWW <https://www.ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/>
12. Gordon, DM., McLean, JM.: Effect of pituitary adrenocorticotropic hormone (ACTH) therapy in ophthalmologic conditions. JAMA, 142(16); 1950 : 1271–1276.
13. Hench, PS., Kendall, EC., Slocumb, CH. et al.: The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone: compound E) and of pituitary adrenocortical hormone in arthritis: preliminary report. Ann Rheum Dis, 8; 1949 Jun: 97-104.
14. Hutyrová, B.: Inhalační kortikosteroidy v léčbě bronchiálního astmatu máme se jich bát nebo být rád za jejich efekt. Klin Farmakol Farm, 29(3); 2015 : 105–107.
15. Jirásková, N.: Přehled léčby zánětů oka. v Rozsíval, P. In: Infekce oka, Praha, Grada, 2003 : 65–67.
16. Jobling, AI., Augusteyn, RC.: What causes steroid cataracts? A review of steroid-induced posterior subcapsular cataracts. Clin Exp Optom, 85(2); 2002 Mar: 61-75.
17. Kuchyňka, P.: Oční lékařství 2., přepracované a doplněné vydání, Praha, Grada, 2016 : 479.
18. Oglesby, RB., Black, RL., Sallmann, L. et al: Cataracts in Rheumatoid Arthritis Patients Treated With Corticosteroids: Description and Differential Diagnosis. Arch Ophthal, 66; 1961 : 519-523.
19. Prokofyeva, E., Wegener, A., Zrenner, E.: Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol, 91(5); 2013 Aug. 395-405.
20. Saag, KG., Furst, DE., Barnes, PJ.: Major side effects of inhaled glucocorticoids. [online]. UpToDate. Jun 2018: Dostupný z WWW: < https://www.uptodate.com/contents/major-side-effects-of-inhaled-glucocorticoids >
21. Skalka, HW., Prchal, JT.: Effect of corticosteroids on cataract formation. Arch Ophthalmol, 98(10); 1980 Oct: 1773-7.
22. Viktorinová M.: Kortikosteroidy pro lokální léčbu kožních chorob. Remedia, 13; 2003 : 266–282.
23. Vlček, J., Vytřísalová, M.: Klinická farmacie II, Praha, Grada, 2014, 24.
Štítky
Oftalmologie
Článek Silent Sinus Syndrome
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2018 Číslo 6- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
-
Všechny články tohoto čísla
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
- Ocular Manifestations in Patients with HIV infection
- The Importance of Evaluating the Development of Oct Findings During Conservative Treatment of Vitreomacular Traction Complicated by Macular Hole Formation
- Silent Sinus Syndrome
- Idiopathic Chodoidal Neovascular Membrane in a 12-year-old Girl
- Screening, Treatment and Long-term Observation of Retinopathy of Prematurely Born Children in the Czech Republic
- OČNÍ KLINIKA 1. LÉKAŘSKÉ FAKULTY UNIVERZITY KARLOVY A VŠEOBECNÉ FAKULTNÍ NEMOCNICE V PRAZE SLAVÍ 200 LET OD SVÉHO ZALOŽENÍ
- Vážený a milý pán doc. MUDr. Tomáš Mazalán, CSc.
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ocular Manifestations in Patients with HIV infection
- Silent Sinus Syndrome
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání