-
Medical journals
- Career
Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
Authors: P. Studený 1; J. Hlaváček 2; R. Chaloupka 2; Ľ. Veselý 1; A. D. Baxant 1
Authors‘ workplace: Oční klinika FNKV a 3. LF UK Praha, přednosta doc. MUDr. Pavel Studený, Ph. D. 1; Medicem Institute s. r. o., Kamenné Žehrovice, Medicem Institute s. r. o. je centrum pro vývoj a výzkum skupiny Medicem Group, výrobce nitrooční čočky WIOL-CF 2
Published in: Čes. a slov. Oftal., 74, 2018, No. 6, p. 219-224
Category: Original Article
doi: https://doi.org/10.31348/2018/6/1Overview
Pupose:
To experimentally compare the visual acuity and the subjective perception of different types of multifocal intraocular lenses (IOL) using a VirtIOL device/simulator in a group of volunteers with artephakia.
Material and methods:
This was an experimental study involving a total of 20 volunteers with artephakia (35 eyes). Each volunteer rated 5 types of IOLs, 4 presbyopia-correcting IOLs - WIOL-CF, Tecnis Symphony ZXR00, Acrysof IQ PanOptix TFNT00, M-flex 630 F, and as a reference lens, we used the monofocal IOL Acrysof SA60AT. The corrected distance visual acuity (CDVA), distance corrected intermediated visual acuity (DCIVA) and distance corrected near visual acuity (DCNVA) were measured. Additionally, volunteers evaluated the quality of vision under normal or changed lighting conditions, and ranked IOL on scale from 1 to 5.
Results:
The CDVA evaluated using the VirtIOL device was very good for all tested IOLs (0.04-0.09 log MAR) with minimum differences. However, CDVA without simulator (-0.01 logMAR) was statistically significantly better in all cases. DCIVA was also very similar in each of the investigated IOLs, surprisingly even with monofocal IOL (0.21-0.23 logMAR), without using simulator the DCIVA was statistically significantly worse (0.36 logMAR). The DCNVA was the best for PanOptix intraocular lens (0.22 logMAR); M-flex, Symphony and WIOL-CF lenses had comparable results (0.31-0.34 logMAR). Again, surprisingly similar results were obtained with the use of monofocal IOL (0.36 ± 0.14). Subjective perception of vision through the IOLs was best rated for the monofocal control IOL, whereas Symphony, WIOL-CF and M-flex did not show any statistically significant difference either with or without glare. All tested IOLs were statistically significantly better if compared to PanOptix with or without glare.
Conclusion:
Simulation of vision through IOLs using VirtIOL simulator allows to compare different models of multifocal IOLs from the viewpoint of visual acuity and subjective perception. However, some caution should be exercised when evaluating the results, given that in our experiments, the monofocal IOL achieved relatively good results at near distance, which does not correspond to clinical experience. On the contrary, from the comparison of the results of CDVA without and with VirtIOL, it is obvious that visual acuity is slightly adversely affected by added optics.
Keywords:
vision simulator – VirtIOL – multifocal intraocular lens – presbyopia correction
INTRODUCTION
The problem of loss of accommodation and surgical solution of presbyopia still remains a substantial challenge in patients for whom cataract surgery is planned. At present a whole range of multifocal intraocular lenses (MF IOL) and lenses with extended depth of focus (EDOF) are available on the market, which to a certain degree provide artephakic patients with quality vision at multiple distances. Nevertheless the construction of the lenses itself entails certain problems (light effects of glare and halo type, worsened contrast sensitivity, insufficient visual acuity at certain distances etc.). Patients may perceive these side effects very negatively, especially in the early postoperative period, and in some cases these may be the cause of frustration and subjectively poor evaluation of the effect of surgery. In extreme cases they may even be the reason for explantation of the IOL [15]. Careful and patient consultation with the patient before surgery is essential, in order to determine the patient’s needs and specific requirements. Even despite this, however, it is often difficult to describe to the patient the manner of vision and optical phenomena which he or she will perceive after the operation [5].
According to the manufacturing technology and the expected effect, we can in principle at present divide the used intraocular lenses (IOLs) into four groups. Monofocal IOLs, which have excellent results in terms of distance vision, as a rule do not enable sufficiently good vision at middle distance and close up, while on the other hand the incidence of adverse optical phenomena is very small. EDOF lenses (in our cohort WIOL-CF, Tecnis Symfony) theoretically provide very good distance and intermediate vision, worse near vision, and in comparison with other groups of lenses should theoretically have a lower risk of occurrence of adverse optical phenomena [1]. Refractive multifocal lenses (in our cohort M-flex) as a rule enable quality distance and near vision, and partially limited middle distance vision. Similarly the last group, diffractive multifocal lenses or more precisely diffractive/refractive (in our cohort PanOptix) provide very good distance and near vision, but are often linked with the incidence of adverse light phenomena. The difference between the trifocal PanOptix lens and for example certain similarly constructed bifocal lenses (ReSTOR) consists primarily in the presence of a third focus (to middle distance) in the case of the PanOptix lens [5].
A comparison of the individual types of multifocal lenses among themselves is relatively complicated, and to date has not yet been reliably resolved. Optical systems have been described which are capable of objectively comparing the purely optical properties of the individual IOLs on models [3,8,9,13]. However, these procedures are not able to faultlessly identify the passage of light through the actual eye, the influence of the retina and the processing of the image by the patient’s central nervous system etc. The results therefore may not actually correspond to subjective evaluation. On the other hand, a whole range of studies have been published in the professional literature, comparing individual types of IOLs in clinical practice. The VirtIOL device provides a new type of examination, which to a certain degree is capable of simulating vision for the patient after the operation, in which the patient’s lens is removed and a specific IOL is implanted. The device functions on the principle of an optical bench, into which the relevant type of planned IOL is inserted, and the patient is able to observe near and distant objects via the optics, to evaluate secondary visual phenomena, contrast sensitivity etc. (fig. 1). With regard to the fact that in the case of cataract the patient’s subjective vision is worsened by the turbidity of the lens itself, the examination is suitable above all for patients with planned extraction of a clear lens or for patients in whom cataract does not yet contribute significantly to worsened visual acuity.
The aim of our study was to compare visual acuity and subjective perception of various types of MF IOL and EDOF in a group of volunteers – patients who had undergone cataract surgery, with the aid of a VirtIOL device. On the basis of this comparison we then intended to determine the applicable usability of this technology for simulating visual perception in patients before the planned extraction of a clear lens and implantation of a multifocal IOL.
METHOD
This concerned an experimental trial, the patients signed an informed consent to their inclusion in the study, and the trial was conducted in accordance with the Helsinki Declaration of 1975, as amended by the revision of 1983. The cohort comprised 20 volunteers (35 artephakic eyes) at minimum 3 months after performed cataract surgery with the implantation of a monofocal IOL. The average age of the volunteers was 71 ± 7 years (58–89 years). We chose examination on artephakic eyes in order to exclude the possibility of any applicable residual accommodation. Exclusion criteria for volunteers in the study were the presence of another ocular pathology which could have adversely influenced visual acuity, and corneal astigmatism higher than 0.75 D (measured by automatic keratometer). All the examinations were conducted at the Department of Ophthalmology at the Královské Vinohrady University Hospital and 3rd Faculty of Medicine, Charles University Prague.
Preparation of the VirtIOL device – the tested lens was hermetically sealed in a testing chamber filled with saline solution. The order of the tested lens was chosen by random selection with the aid of a permutation calculator (http://users.telenet.be/vdmoortel/dirk/Maths/permutations.html) in order to eliminate potential error (the last types of evaluated lenses could have been disadvantaged for example due to fatigue on the part of the patient etc.).
Each volunteer evaluated a total of 5 types of IOL, which were progressively inserted into the device. The evaluated lenses were WIOL-CF + 22 D (Medicem Technology), Tecnis Symphony ZXR00 +22 D (Abbot Medical Optics), Acrysof IQ PanOptix TFNT00; +22 D, ADD: +2.2 and +3.2 D (Alcon) and M-fLex 630 F, + 22 D, ADD +3.0D (Rayner). We used a monofocal IOL Acrysof ASA60AT + 22 D (Alcon) as a reference lens. Any postoperative spherical defect of the volunteers was corrected with the aid of a corrective lens, in order to ensure that the result of the evaluation could not be influenced. Measured visual acuity at the stipulated distances was therefore examined with the aid of distance correction. Corrected distance visual acuity (CDVA) was measured – 4.2 m, as well as distance corrected intermediate visual acuity (DCIVA) at 70 cm, and distance corrected near visual acuity (DCNVA) at 40 cm. Visual acuity was examined with the aid of an LCD optotype and expressed in values of LogMAR. The size of the screen was stipulated at 3 mm upon distance examination and 2.5 mm upon evaluation of intermediate and near vision, which corresponds to the size of the pupil in the given group [2]. Upon further examination, the volunteers evaluated the quality of vision under ordinary or altered lighting conditions (comparison of occurrence of adverse visual effects). The examined volunteer observed an image without glare through the evaluated IOL, placed in random order. The task was to attribute to the lens the relevant ranking of 1-5, with 1 indicating the fewest phenomena and 5 the worst subjective perception. Subsequently an image with glare (fig. 2) was projected and evaluated in the same manner. The five samples consisted of the aforementioned 4 types of examined IOLs, the fifth sample was again a monofocal lens without addition.
2. Images designed for evaluation of subjective vision without and with glare 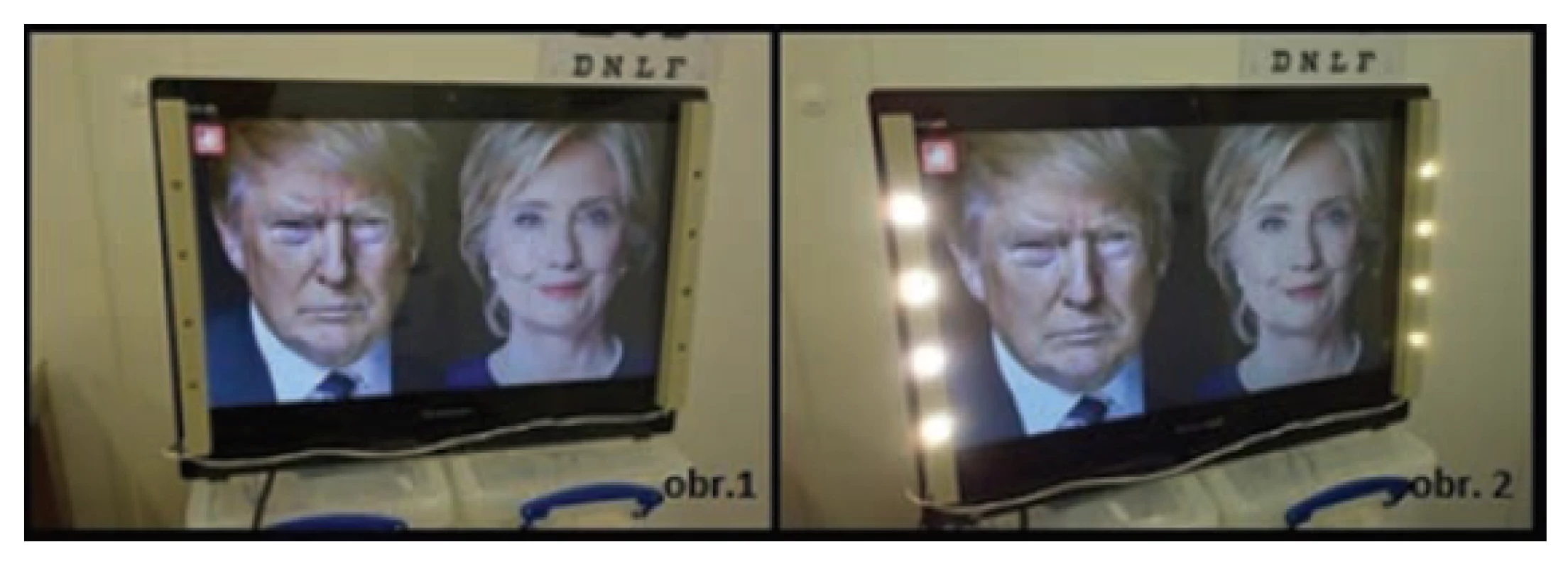
We statistically evaluated the results with the aid of a Student paired test. We considered a value of p ≤ 0.05 to represent statistically significant differences.
RESULTS
CDVA examined via the VirtIOL device was very good for the examined lenses (graph 1). The mutual differences between the lenses were minimal, but were nevertheless statistically significant in certain cases (table 1). However, if we compare CDVA examined with the aid of the VirtIOL device and regular CDVA without the use of the device in the volunteers taking part (-0.01 logMAR), this was statistically significantly worse in all cases, even in the case of use of a monofocal IOL (0.04 logMAR). It is therefore evident that visual acuity examined via the VirtIOL instrument is slightly adversely influenced by the added optics.
1. Statistical differences (p values) between the different types of evaluated intraocular lenses tested in corrected distance visual acuity. The values marked in red were statistically significant. 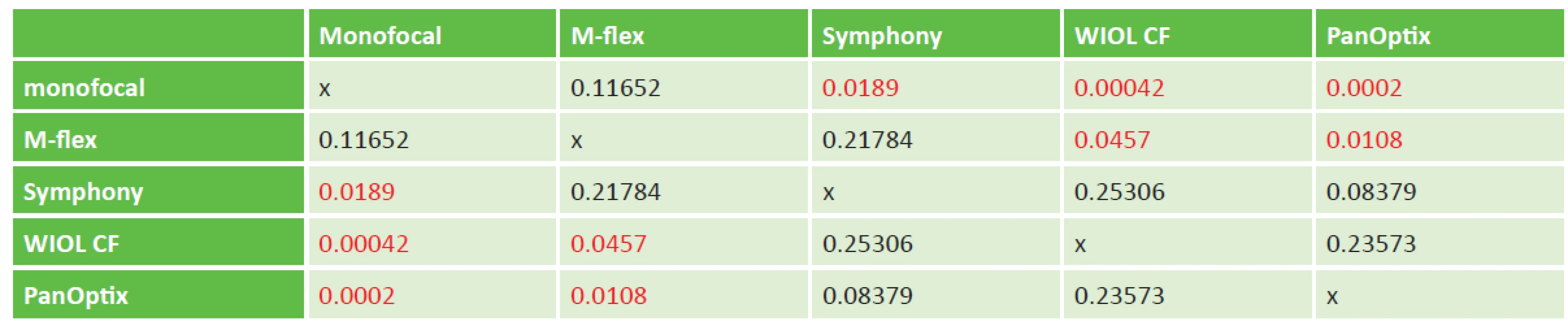
1. Corrected distance visual acuity without/with VirtIOL 
DCIVA was also very similar for the individual tested IOLs, and surprisingly also in the case of the monofocal IOL (graph 2). The only small but statistically significant difference we recorded was in a comparison of M-flex and WIOL-CF lenses, in which the results of the M-flex lens were better. However, clinically the difference of 0.02 logMAR is insignificant, and corresponds to worsening/improvement by one read symbol on ETDRS optotype (table 2).
2. Statistical differences (p values) between the different types of evaluated IOLs in distance corrected intermediate visual acuity. The values marked in red were statistically significant. 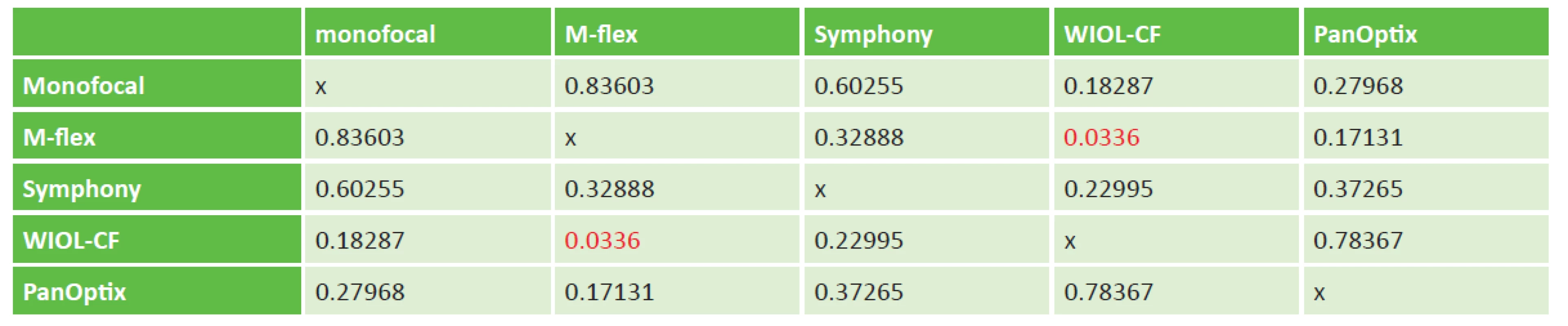
2. Distance corrected intermediate visual acuity without/ with VirtIOL 
Upon a comparison of ordinary DCIVA examined without the use of the VirtIOL device (0.36 logMAR) and DCIVA with the use of the device for the individual tested IOLs, this value was statistically significantly worse (including in the case of using the monofocal IOL in the device).
Graph 3 presents the overall results of DCNVA for the tested lenses. The patients attained the best near vision upon use of the PanOptix lens; the lenses M-flex, Symphony and WIOL-CF had comparable results. We again obtained surprisingly similar results upon the use of the monofocal IOL (value 0.36±0.14). The statistical significance of the individual results is described in table no. 3.
3. Statistical differences (p values) between the different types of evaluated IOLs in distance corrected near visual acuity. The values marked in red were statistically significant. 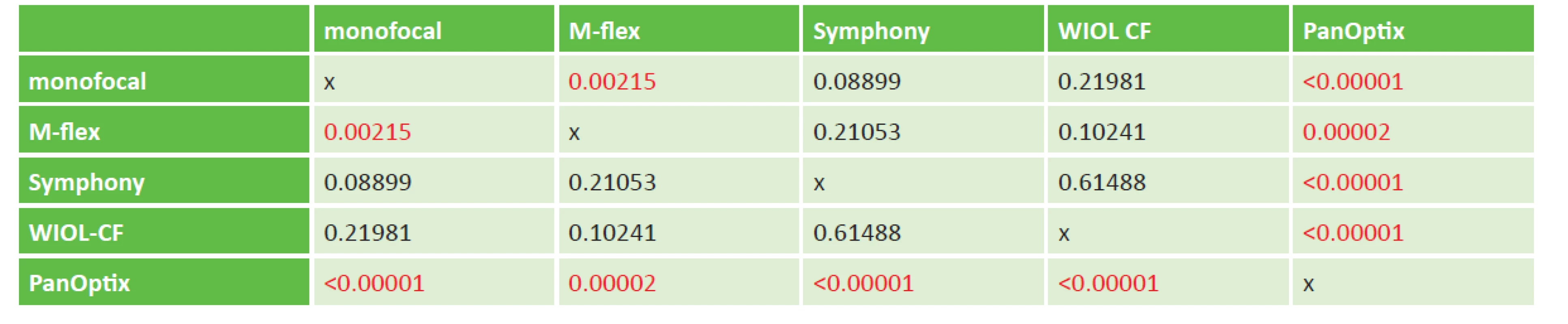
3. Distance corrected near visual acuity without/with VirtIOL 
Upon a comparison of ordinary DCNVA examined without the use of the VirtIOL device (0.56 logMAR) and DCNVA for the individual tested IOLs with the use of the device, this value was statistically significantly worse (and again also in the case of the monofocal IOL in the device).
Table 4 presents the results of subjective evaluation of patients both “with/without glare”. In comparison with all the other types of IOL, the monofocal lens was statistically significantly better “with/without glare”. There was no statistically significant difference “with/without glare” between Symfony, WIOL-CF and M-flex. All the tested lenses were statistically significantly better evaluated in comparison with PanOptix “with/without glare”.
4. Subjective evaluation of secondary phenomena when viewed to distance with the appropriate IOL, with and without glare (average, standard deviation) 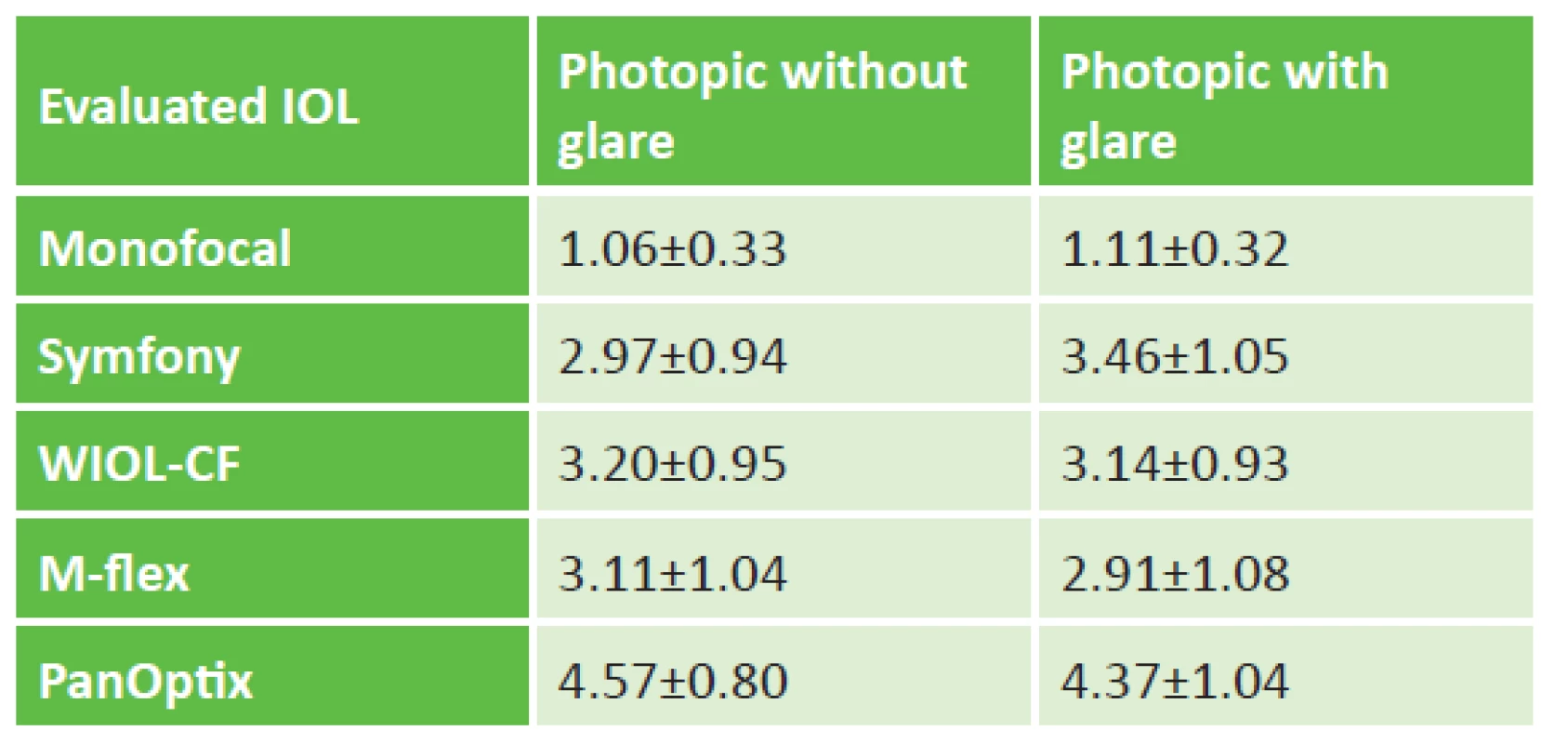
DISCUSSION
With regard to the fact that resolving loss of accommodation after removing a natural lens and inducing pseudoaccommodation by means of the implantation of multifocal and EDOF IOLs is currently one of the primary themes of ophthalmology, it is possible to find a relatively large quantity of studies on this issue in the professional literature. However, practically all the studies relate to the clinical results upon the use of the individual lenses. The majority of the published results describe a specific type of MF IOL and compare it with the results for monofocal lenses, or mutually compare 2 types of MF IOL. Cochener et al. published an extensive meta-analysis incorporating the clinical results of 11 monofocal and 35 multifocal IOLs (both diffractive and refractive, as well as 2 accommodative). Average uncorrected distance visual acuity for the multifocal IOLs was 0.165 (0.090-0.240) logMAR, for the monofocal lenses 0.093 (0.088-0.098) logMAR. In comparison with monofocal lenses, the patients with multifocal lenses attained statistically significantly better uncorrected near vision – 0.141 (0.131-0.152) logMAR versus 0.470 (0.322-0.618) logMAR. In a comparison of diffractive and refractive IOLs, the authors describe comparable uncorrected distance vision (0.105 [0.098-0.111] logMAR versus 0.085 [0.029-0.140] logMAR) and better uncorrected near vision in favour of diffractive lenses (0.217 [0.118-0.317] logMAR versus 0.082 [0.067-0.098] logAMR). As regards the occurrence of secondary visual phenomena, these were similar for all types of multifocal IOLs [4]. In our experimental study we did not record larger differences between a refractive (M-Flex) and diffractive IOL (PanOptix) for distance vision, nevertheless the diffractive PanOptix lens was statistically significantly better for near vision. By contrast, upon subjective evaluation of secondary visual phenomena, somewhat surprisingly the diffractive lens was evaluated statistically significantly worse in comparison with all the other tested types of IOL.
Studies have also been published comparing the effect of implantation of trifocal and bifocal IOLs, above all with respect to intermediate distance visual acuity. For example, Vilar et al. demonstrated better intermediate distance visual acuity and better contrast sensitivity under photopic conditions in patients with a bilaterally implanted trifocal PanOptix lens in comparison with patients with an implanted bifocal diffractive/refractive ReSTOR lens [16]. Mojžíš et al. describe significantly better intermediate distance vision in patients with an implanted trifocal AT LISA lens in comparison with an analogous bifocal lens [10].
Veliká et al. examined the difference between classic bifocal lenses (Lentis Mplus) and bifocal lenses with extended depth of acuity (Lentis MplusX), which theoretically enable better middle distance vision, nevertheless in their study the authors did not record any statistically significant differences [14].
In our experiment it was not possible to demonstrate a positive effect of a trifocal IOL at intermediate distance, the values of all the tested IOLs (including the monofocal reference lens) were practically comparable at intermediate distance.
By contrast, there are very few studies in the literature to date which have focused on the possibility of simulating visual acuity and subjective perceptions with the aid of the VirtIOL simulator, or by another method.
Pujol et al. for example used the VirtIOL device for testing a prototype of a new multifocal lens – NDIOL Ophtec with addition of +2.0 D, which they compared with the commercially available lens Mplus Oculentis (addition +3 D). As a reference they used a monofocal lens. For distance vision, visual acuity was best in the case of the monofocal lens (-0.2), followed by the Mplus lens (-0.1) and NDIOL (0.0). For near vision, visual acuity was best in the case of the NDIOL lens (0.0), followed by Mplus (0.1), and relatively worse for the monofocal lens (0.4) [11]. However, in this study the tested group of patients was without artephakia (age 53.2±6.7), and so the result could have been influenced by their residual accommodation. In our cohort the tested individuals did not attain such good near visual acuity, and also the differences between the monofocal lens and the multifocal lenses were less pronounced.
Another study again by Pujol et al. compared monofocal, bifocal and trifocal IOLs on 3 tested individuals with the aid of a VirtIOL simulator. They measured visual acuity in the patients through lenses from +1 to -5 D, and thereby attained a virtual pseudoaccommodation curve for the individual tested IOLs. Near visual acuity was better in this experiment in the case of the bifocal and trifocal lenses in comparison with the monofocal lens, visual acuity to middle distance was similar in all 3 cases (similarly as in our experiment) [12].
Guthoff et al. compared the simulated size of secondary visual phenomena (halo, starburst) with the aid of the VirtIOL device. Under mesopic conditions the patients preferred monofocal IOLs for distance vision in comparison with a MF lens and EDOF [7].
The question naturally arises as to what extent simulated results can correspond to actual results. Giner et al. evaluated the difference between simulated and actual postoperative visual acuity in 10 patients. Three weeks after implantation of a bifocal Mplus IOL, actual distance visual acuity was better by 0.1 ± 0.13 in comparison with simulated, in the case of near vision this difference was 0.16 ± 0.12. The patients in this study also subjectively compared the similarity of the preoperative simulation and actual postoperative vision on a scale of 0-5 (0 – different, 5 – exactly the same). The average value of accordance was 3.20 ± 0.79 upon observing a letter and 2.50 ± 0.71 upon observing a light source. Nevertheless, the authors attribute this relative difference between the simulated and actual results to turbidities of the lens which appeared in the tested individuals before surgery [6].
The results of our experimental study evaluating individual types of MF and EDOF IOLs with the aid of a VirtIOL simulator produced a number of interesting discoveries. In general it applies that subjective perception of secondary phenomena worsens from monofocal, via EDOF lenses to the refractive and diffractive type of MF IOL. According to expectations, patients indicated the monofocal control IOL as the best in all lighting conditions. Correction of presbyopia with the aid of an IOL therefore causes certain unpleasant side effects to a greater or lesser extent, which are well manifested upon simulation with a VirtIOL device.
Surprisingly, in our experiment simulated visual acuity to middle distance and close up in individual tested IOLs showed small differences between the individual tested IOLs, and even relatively small differences from the monofocal control IOL. However, a difference appears if the results are compared with visual acuity of the tested subjects without the VirtIOL at all three distances (distance, intermediate, near). The monofocal IOL inserted into the VirtIOL simulator thus behaved to a certain degree as a multifocal lens in the test. We believe that this may be explained by the fact that the spherical aberration (SA) of the tested artephakic persons is significantly increased upon examination using the VirtIOL device. An accumulation of positive SA of the implanted IOL and SA of the tested IOL occurs, which could theoretically lead to an extended depth of acuity. A certain role may also have been played by residual accommodative effort and a certain degree of neuroadaptation in the tested persons with monofocal artephakia.
A partial rectification of this effect could be achieved by conducting research on phakic persons with pharmacologically suppressed accommodation, or in full presbyopic patients with an entirely clear lens. Another possibility would be to use a camera instead of tested subjects, which would however to a certain extent counteract the greatest benefit of simulation with the aid of a VirtIOL device, namely subjective evaluation of the image and its processing by the retina, visual pathway and visual centres.
CONCLUSION
The first results of our experimental study with the VirtIOL simulator indicate that the main clinical benefit of this examination consists in the possibility of the patient to subjectively evaluate perception of the image with the aid of IOLs correcting presbyopia, and to compare them with other IOLs, rather than in the actual simulation of postoperative visual acuity. In addition, to a certain extent it is possible to compare for example new types of IOLs with already available lenses. Nevertheless, a certain degree of caution is essential in evaluating the results, due to the fact that the experimental data may not entirely correspond with clinical experiences.
In our experiment, distance and intermediate visual acuity was practically comparable in the case of all the tested IOLs, whereas in near vision the patients attained the best visual acuity with a trifocal lens. By contrast, upon subjective evaluation of secondary phenomena, this lens was evaluated as the worst, both with and without glare.
Received by the Editorial Department on: 13 October 2018
Accepted for printing on: 16 December 2018
doc, MUDr. Pavel Studený, Ph.D.
Department of Ophthalmology, Královské Vinohrady University Hospital and 3rd Faculty of Medicine, Charles University Prague
Šrobárova 50
Prague 10, 10034
Sources
1. Baldassare, R., Bedi, R.: Symfony Extended Depth of Focus IOL: a Review of Reported Data. Curr Ophthalmol Rep, 5; 2017 : 225-231.
2. Benjamin, WJ.: Borish’s Clinical Refraction – E-Book. Elsevier Health Sciences; 2006
3. Choi, J., Schwiegerling, J.: Optical performance measurement and night driving simulation of ReSTOR, ReZoom and Tecnis multifocal intraocular lenses in a model eye. J Refract Surg, 24; 2008 : 218-222.
4. Cochener, B., Lafuma, A., Khoshnood, B. et al.: Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Opthalmol, 5;2011 : 45-56.
5. Breyer, DRH., Kaymak, H., Ax, T. et al.: Multifocal Intraocular Lenses and Extended Depth of Focus Intraocular Lenses. Asia Pac J Ophthalmol (Phila), 6; 2017 : 339-349.
6. Giner, A., Aldaba, M., Luque, SO. et al.: Analysis of the visual quality with multifocal intraocular lenses before surgery. Invest Ophthalmol Vis Sci, 56 : 2015 : 2983.
7. Guthoff, RF., Gerlach, M., Fuchs, V. et al.: Characterization of starburst and halo size for different virtually implanted intraocular lenses in comparison to subject’s quality of vision. Invest Ophthalmol Vis Sci, 58; 2017 : 338.
8. Kim, MJ., Zheleznyak, L., Macrae, S. et al.: Objective evaluation of through-focus optical performance of presbyopia-correcting intraocular lenses using an optical bench systém. J Cataract Refract Surg, 37; 2011 : 1305-1312.
9. Maxwell, WA., Lane, SS., Zhou, F.: Performance of presbyopia-correcting intraocular lenses in distance optical bench test. J Cataract Refract Surg. 35; 2009 : 166-71.
10. Mojzis, P., Kukuckova, L., Majerova, K. et al.: Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg, 30; 2014 : 666-672.
11. Pujol, J., Aldaba, M., Giner, A. et al.: Visual performance evaluation of a new multifocal intraocular lens design before surgery. Invest Ophthalmol Vis Sci, 55; 2014 : 3752.
12. Pujol, J., Ondategui-Parra, JC., Baiella, L. et al.: Sperical subjective refraction with a novel 3D virtual reality based systém. J Optom, 10; 2017 : 43-51
13. Terwee, T., Weeber, H., van der Mooren, M. et al.: Visualization of the retinal image in an eye model with sperical and aspheric, diffractive and refractive multifocal intraocular lenses. J Refract Surg, 24; 2008 : 223-232
14. Veliká V., Hejsek L, Raiskup F.: Clinical Results of the implantation of Two Types of Multifocal Rotational Asymmetric Intraocular Lenses. Cesk Slov Oftalmol, 73; 2017 : 3-12.
15. Veselá M., Baráková D., Lenčová A.: Analysis of reasons of intraocular lenses explantation. Cesk Slov Oftalmol, 60; 2004 : 30-36.
16. Vilar, C., Hida, WT., de Medeiros, AL. et al.: Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol, 11; 2017 : 1393-1397.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 6-
All articles in this issue
- OČNÍ KLINIKA 1. LÉKAŘSKÉ FAKULTY UNIVERZITY KARLOVY A VŠEOBECNÉ FAKULTNÍ NEMOCNICE V PRAZE SLAVÍ 200 LET OD SVÉHO ZALOŽENÍ
- Vážený a milý pán doc. MUDr. Tomáš Mazalán, CSc.
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
- Ocular Manifestations in Patients with HIV infection
- The Importance of Evaluating the Development of Oct Findings During Conservative Treatment of Vitreomacular Traction Complicated by Macular Hole Formation
- Silent Sinus Syndrome
- Idiopathic Chodoidal Neovascular Membrane in a 12-year-old Girl
- Screening, Treatment and Long-term Observation of Retinopathy of Prematurely Born Children in the Czech Republic
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ocular Manifestations in Patients with HIV infection
- Silent Sinus Syndrome
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


