-
Medical journals
- Career
Silent Sinus Syndrome
Authors: R. Hlaváčová 1,2; T. Kuběna 2; P. Černošek 2
Authors‘ workplace: Oční oddělení Krajské nemocnice Tomáše Bati, a. s., Havlíčkovo nábřeží 600, 762 75, Zlín, primář MUDr. Erika Dugová 1; Oční ordinace MUDr. Tomáš Kuběna, s. r. o., U zimního stadionu 1759, 760 01 Zlín, zastoupená MUDr. Tomášem Kuběnou 2
Published in: Čes. a slov. Oftal., 74, 2018, No. 6, p. 245-248
Category: Case Report
doi: https://doi.org/10.31348/2018/6/5Overview
Silent sinus syndrom is rare and slow progressive disorder associated with asymptomatic chronic maxillary sinusitis and collapse of the orbital floor. The most common manifestations are enophtalmos, hypoglobus and pseudoretraction upper eyelid. Silent sinus syndrome is almost a unilateral condition and is usually diagnosed in patients in their 30´s and 40´s. The largest risk factors is underlaying aberrant nasal anatomy. The subsequent osteomeatal complex obstruction leads to hypoventilation of the maxillary sinus and negative pressure development. The sinus cavity is filed with a combination of mucus and acellular transudate. This proces create a chronic mucosal inflammation with demineralization and collapse of the orbital floor. CT imaging is pathognomonic and shows ipsilateral maxilar sinusitis and the orbital floor is inferiorly displaced. The differential diagnosis includes chronic sinusitis, osteomyelitis, malignat sinus infiltration and orbital trauma. The endoscopic antrostomy is the gold standard to re-establish normal sinus aeration. In this article we describe patient with silent sinus syndrome, who has been treated at our clinic and his symptoms were corrected ad integrum after the surgery.
Keywords:
silent sinus syndrome – pseudo-Grafe´s sign – eyelid pseudoretraction – maxilar sinusitis – antrostomy
INTRODUCTION
Silent sinus syndrome is a pathology of the maxillary sinus, which is outwardly manifested only by ocular symptoms: enophthalmos, hypoglobus and retraction of the upper eyelids with pseudo-Graefe's sign. These symptoms occur as a consequence of collapse of the orbital floor into the jaw cavity, and are caused by chronic asymptomatic sinusitis following a closure of the aperture of the maxillary cavity into the nasal cavity. In the English speaking literature this disease is also referred to as chronic maxillary atelectasis (CMA). To the best of our knowledge, this pathology has not yet been described in the Czech ophthalmological literature.
This pathology was first published in 1964 by Montgomery, who described two cases of diplopia and enophthalmos associated with homolateral maxillary inflammation [11].
However, the term “silent sinus syndrome” was first used by Soparkar et al. in 1994 [12]. The authors described 14 patients with spontaneous unilateral enophthalmos or hypoglobus due to collapse of the floor of the orbit, and turbidity of the maxillary sinus. Since these first cases, over one hundred similar case reports have been published [3].
Silent sinus syndrome is usually diagnosed in patients between the ages of thirty and forty [3]. The majority of the published studies state the same incidence in men and women [13], although a large study containing 84 patients states a slight predominance of men [10].
The largest risk factor of this pathology is hidden deformation of the nasal septum (deviation of the nasal septum and middle nasal concha). These abnormalities lead to a closure of the aperture of the maxillary sinus with all the described consequences.
Pathophysiology
Initially silent sinus syndrome was linked with hypoplasia of the maxillary sinus. However, this association was disproven after 1999, when Davidson et al. documented normal maxillary sinus several years before the onset of the first symptoms [5]. Silent sinus syndrome originates due to hypoventilation of the maxillary sinus following obstruction of the osteomeatal complex [7, 12], i.e. the area beneath the middle nasal concha with the aperture of the maxillary, frontal and ethmoidal sinus. Obstruction can originate as a consequence of deviated medial concha [1, 7], mucocele or polyp, which occludes the aperture of the jaw cavity [12]. Cases of iatrogenic silent sinus syndrome are also described, in which damage to the aperture of the maxillary sinus occurred during surgery [8]. Occlusion and reduced ventilation lead to reabsorption of secretion, with the build-up of underpressure in the maxillary sinus. This was demonstrated by Kass et al., who measured pressure in the sinus with the aid of an 18-gauge needle and determined negative sub-atmospheric pressure - 6 mm Hg to - 13 mm Hg [6]. Another study states underpressure as much as -23 mm Hg [5]. As soon as the sinus remains occluded and underpressure develops, the sinus cavity is filled with a combination of acellular transudate and sputum [7]. This process leads to chronic inflammation with atelectasis of the maxillary sinus, demineralisation of the bone of the orbital floor, with its subsequent collapse.
Clinical symptoms
The symptoms develop over a period of weeks to months, most often within the range of 4-8 months [10, 13]. In the largest number of cases, silent sinus syndrome is manifested by enophthalmos and hypoglobus [11]. Endophtalmos occurs in 98-100% of cases, hypoglobus is less common and occurs in only 53% of patients [2]. In 90% of patients we can observe a retraction of the upper eyelid and pseudo-Graefe's sign.
Less common symptoms include diplopia. In a large study covering 84 patients, 65% of patients had diplopia [5]. Vision, intraocular pressure and the visual field are mostly within the norm [14]. Silent sinus syndrome is unilateral in most cases, although two described cases of bilateral syndrome appear in the literature [9, 14].
TREATMENT
The gold standard of treatment is endoscopically performed antrostomy, which restores normal ventilation of the maxillary sinus. If a regression of the clinical symptoms is not achieved, there follows reconstruction of the orbit with the aid of implants. Babar-Craig et al. advise waiting for at least 6 months after the performance of antrostomy, since in their group of patients only 2 patients out of 16 required reconstruction of the orbit [1].
Moreover, further surgery increases the risk of infection, postoperative diplopia or even loss of sight.
CASE REPORT
A 38-year-old patient was entirely without ocular or general complaints. However, his relatives and co-workers had noticed an asymmetry between his eyes persisting for approximately six months, with his right eye more widely open than his left. On 19 June 2016 the patient first visited an outpatient ophthalmologic department in the locality of his residence with the following finding: Vision in both eyes with correction -0.5 D 1.0, intraocular tension 14/16 mm Hg. The finding was physiological on the anterior segment and ocular fundus, with the exception of epicanthus on the upper eyelid of the left eye. On the right eye it is possible to suspect a deep orbitopalpebral sulcus (Fig. 1). The following diagnosis was determined: Blepharochalasis palp.sup.l.sin.a, plastic surgery of the left upper eyelid was recommended.
1. Blefarochalasis of the left eye, deep orbitopalpebral sulcus on right eye 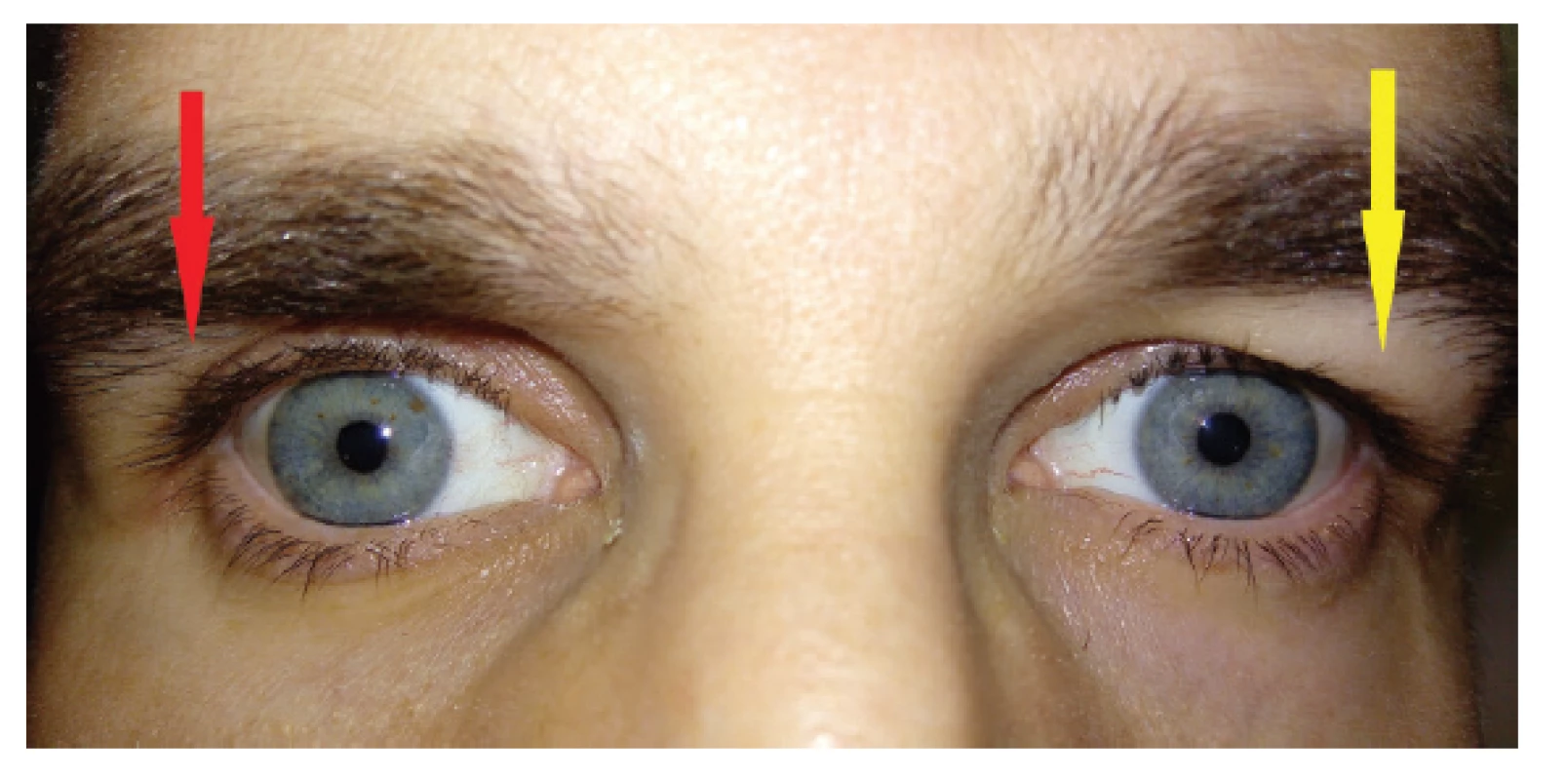
Before the operation took place, the patient met an old friend, who remembered that from an early age the patient had had overhanging upper eyelids on both eyes. His friend (unlike the ophthalmologist) noted a change by contrast in the right eye, which appeared unusually wide. The patient reported to our centre with this anamnesis on 11 November 2016. In addition to the basic ocular examination with the same finding as in the one conducted on 19 June 2016, we also determined retraction of the upper eyelid of the right eye, Graefe's sign in right eye (absent convergence of upper eyelid of right eye upon downward gaze) (Fig. 2), mild enophthalmos in right eye - Hertel 13/112/15 mm and mild hypoglobus in right eye (downward shift of right eye by 1 mm in comparison with left eye).
2. Retraction of the right upper eyelid with Graefe’s sign 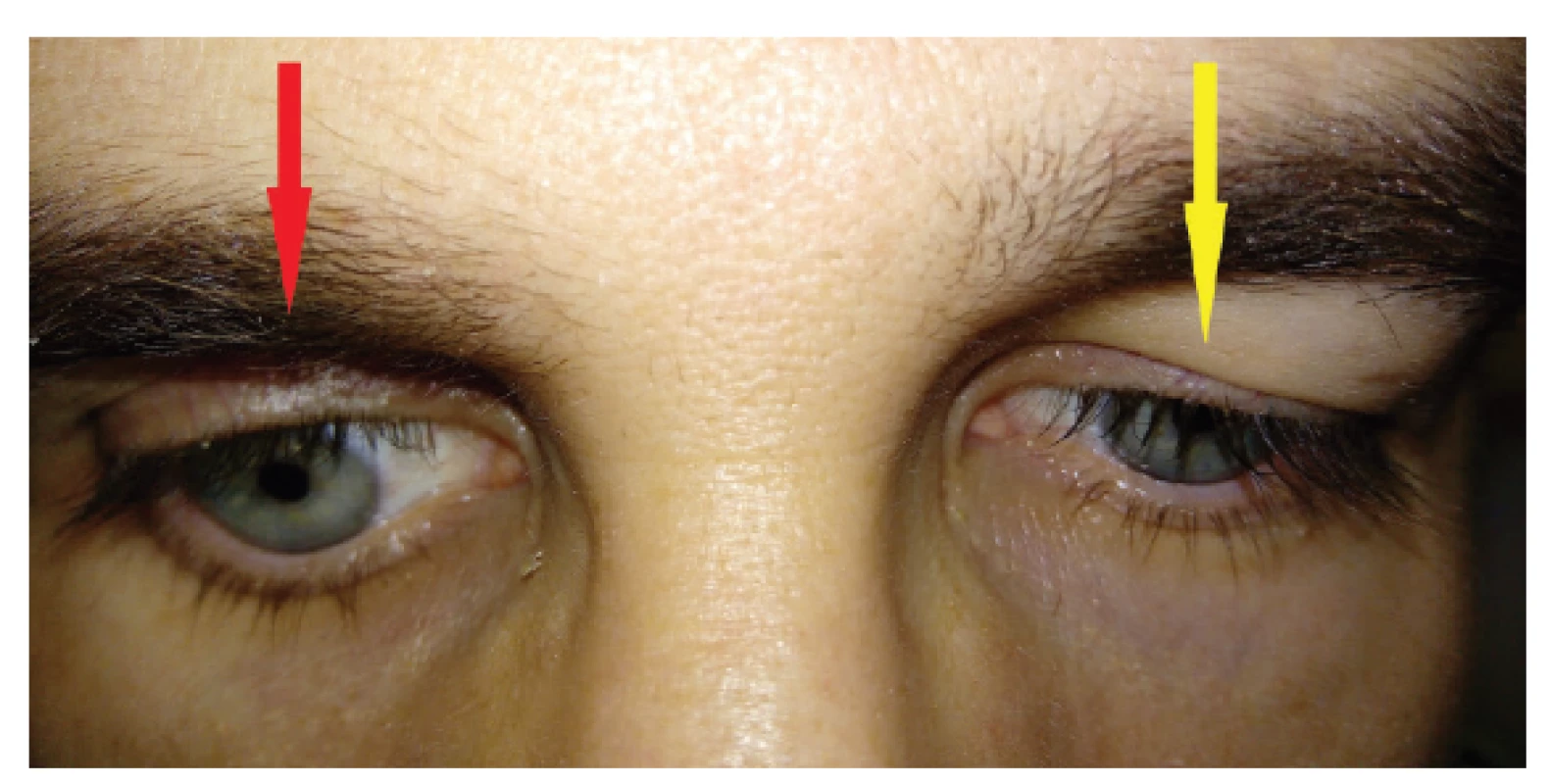
At this time the diagnosis of silent sinus syndrome was not known to us, and as a result, with regard to Graefe's sign we suspected endocrine orbitopathy, which however was not sonographically or endocrinogically confirmed. Our working diagnosis was retraction of the upper eyelid with Graefe's sign and hypoglobus of the right eye of unknown origin.
An MR examination excluded the possibility of tumorous pathology of the brain. Upon focusing MR at the region of the orbits and nasal cavities, on the transverse cross-section of the nasal cavity there was an evident deviation of the septum to the right (Fig. 3.). On a coronary cross-section (Fig. 4.) there was an evident downward shift of the floor of the right orbit, a contraction of the maxillary sinus and its filling with tissue of similar reflectivity as the vitreous body. The left maxillary sinus was of normal size and ventilation. On a saggital cross-section of the right jaw cavity (Fig. 5.) there was an evident deepening of the lower wall of the right orbit and a filling of the contracted right maxillary cavity with homogeneous tissue. On the basis of the MR examination we suspected tumorous infiltration of the right maxillary sinus.
3. MR scan: nasal septum deviation to the right side 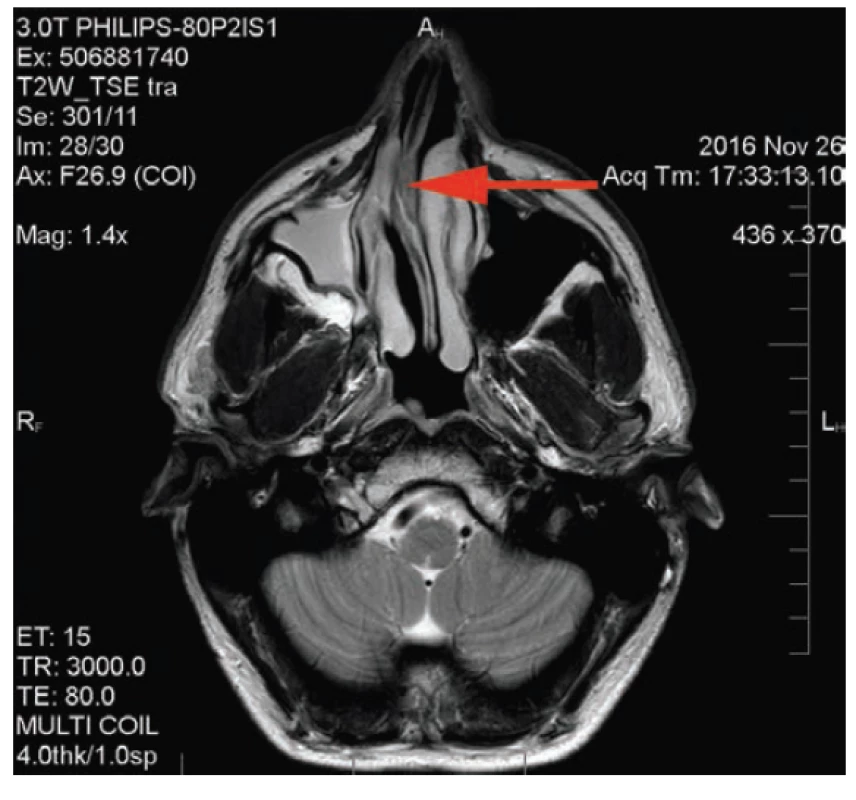
4. MR scan: reduction of the right maxillary sinus, left maxillary sinus normal size and ventilation 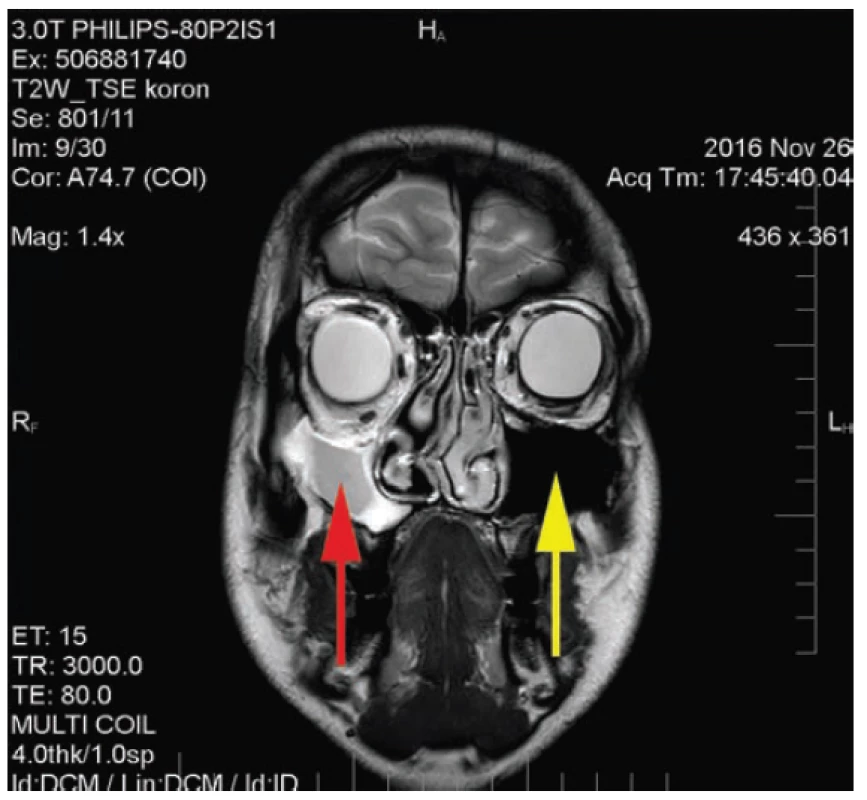
5. MR scan: orbital floor displaced inferiorly 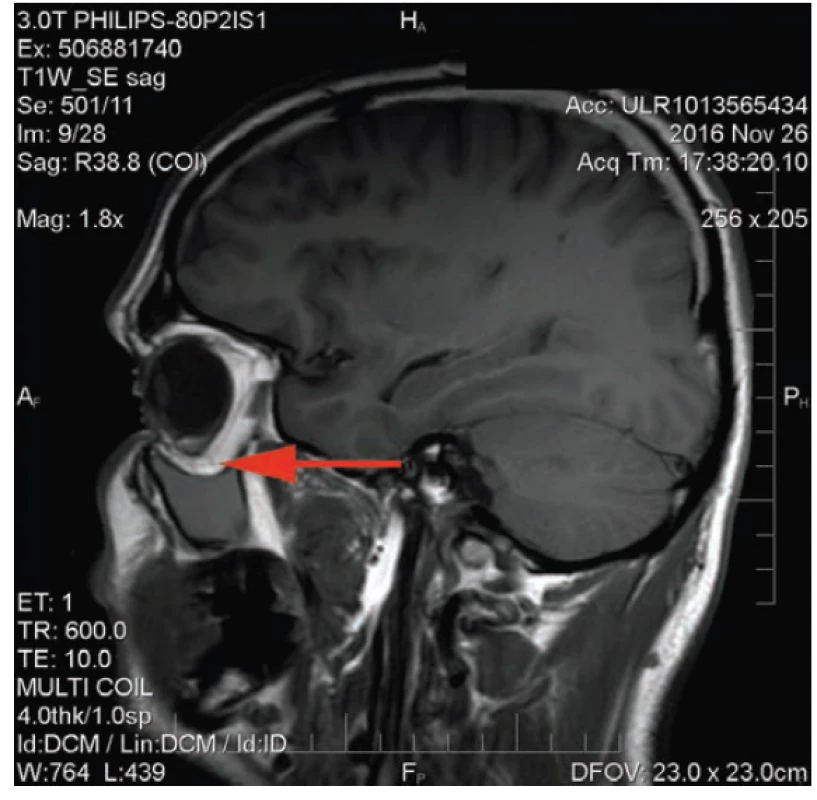
On 17 December 2016 an endoscopic antrostomy was performed by transnasal approach in order to confirm the diagnosis. Hyperplastic mucosa was found in the right jaw cavity, with gelatinous secretion. Antrostomy restored communication between the jaw and nasal cavity. At the same time, repositioning of the deviated septum was performed to the medial level, in order to prevent recurrence of the pathology. It was only on the basis of MR and the surgical finding that a diagnosis of silent sinus syndrome was eventually determined. One month after surgery a regression of the ocular symptoms took place, especially retraction of the upper eyelid and reduction of enophthalmos. Blepharochalasis again formed on the upper right eyelid, and asymmetry of the ocular apertures had entirely disappeared at a follow-up examination 1 year after surgery (Fig. 6.). At a follow-up MR examination of the orbit and the adjacent cavities 1 year after surgery, however, deepening of the orbital wall and contraction of the right jaw cavity persisted in the same extent as before the operation. There was a difference in the disappearance of hyperplastic mucosa and secretion from the right jaw cavity and in its normal aeration.
6. Symmetry of the upper eyelids of both eyes 1 year after antrostomy 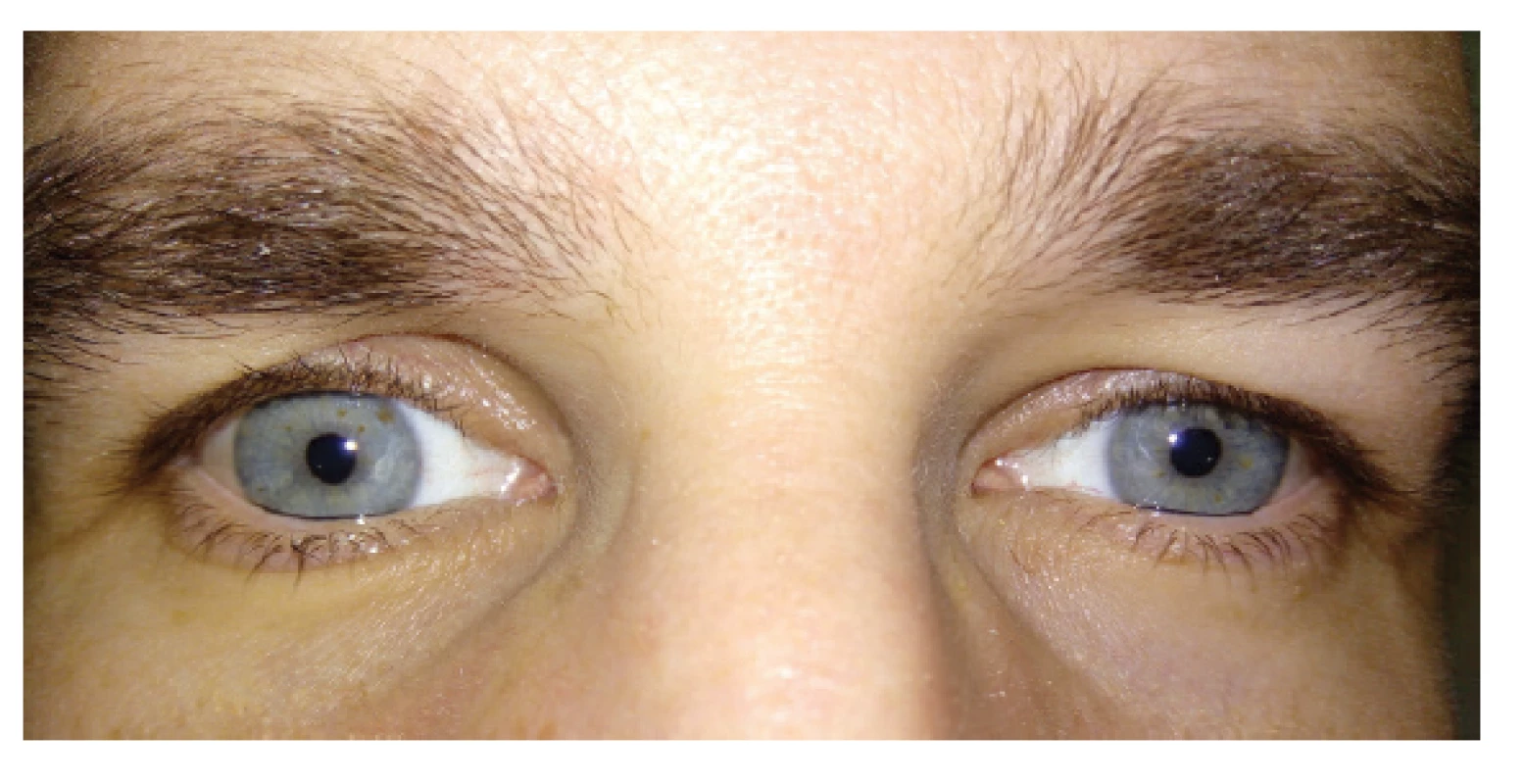
DISCUSSION
Silent sinus syndrome ranks among multidisciplinary pathologies. The pathological process takes place in the maxillary cavity (field of ENT), whereas its symptoms can be observed by ophthalmologists (field of ophthalmology). With regard to this fact and also due to its rare incidence, the diagnosis of this pathology may present difficulties. In our patient we first of all considered Parry-Romberg syndrome (progressive hemifacial atrophy) and endocrine orbitopathy. After MR examination we then considered tumorous infiltration of the right jaw cavity. The definitive diagnosis of silent sinus syndrome was arrived at only after antrostomy. The fundamental symptoms of silent sinus syndrome include spontaneous enophthalmos, hypoglobus, retraction of the upper eyelid, absence of subjective symptoms of sinusitis and then upon MR examination contraction and occlusion of the maxillary sinus homolaterally. According to Bartley, it is possible to divide the mechanism of retraction of the upper eyelid into three causes – neurogenic, myogenic and mechanical [2]. The authors believe that in the case of silent sinus syndrome, retraction of the upper eyelid, enophthalmos and disappearance of blepharochalasis is contributed to not only by hypoglobus, but also by underpressure in the orbit caused by a deepening of its floor downwards and an enlargement of its volume. Graefe's sign probably appears here only as an optical illusion upon hypoglobus, and for this reason should be referred to as pseudo-Graefe's sign. In the diagnosis MR or CT examination is of fundamental importance, since it demonstrates a contraction and diffuse occlusion of the maxillary sinus homolaterally, with areas of loss of bone and collapsed orbital floor [3]. Deviation of the nasal septum and medial nasal concha is also described on the affected side [1, 13]. In differential diagnostics we consider chronic sinusitis, osteomyelitis, malignant infiltration, orbital trauma and pseudo-enophtalmus. Burroughs et al. published 19 cases of false positive diagnosis of silent sinus syndrome. The most common genuine causes include orbital trauma, congenital facial asymmetry, contralateral exophthalmos and Parry-Romberg syndrome [4].
CONCLUSION
Silent sinus syndrome is a rare pathology caused by progressive and asymptomatic atelectasis of the maxillary sinus. The diagnosis is often determined by an ophthalmologist due to manifestations of enophthalmos, hypoglobus and pseudo-retraction of the upper eyelid. Despite the fact that it is possible to determine the diagnosis only on the basis of the clinical symptoms, MR examination is indicated, which is highly beneficial for demonstrating this pathology. Treatment takes place in co-operation with ENT, and consists in restoration of normal ventilation of the maxillary sinus by endoscopic antrostomy, and if applicable reconstruction of the orbital floor with the aid of implants. The patient referred to in our case report experienced a rapid regression of the clinical symptoms after the operation, without the necessity of a further surgical intervention.
This lecture was presented in an abridged form at the Zlínský oční festival [Zlín Opththalmological Festival], 2017 and at the Seminář oční kliniky [Eye Clinic Seminar] of the University Hospital in Olomouc, 2017
Received by the Editorial Department on: 28.11.2018
Accepted for printing on: 19.12.2018
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Radka Hlaváčová
Tomáše Bati, a.s.
Havlíčkovo nábřeží 600
Zlín 762 75
Sources
1. Babar-Craigh, H., Kayhanian, H., De Silva DJ.: Spontaneous silent sinus syndrome (imploding antrum syndrome): Case series of 16 patients. Rhinology; 2011, 49(3): 315-317.
2. Bartley, G.B., MD.: The differential diagnosis and classification of eyelid retraction. Trans Am Ophtalmol soc; 1995, 93 : 371-389.
3. Brandt, MG., Wright, ED.: The silent sinus syndromies a form of chronic maxillary atelectasis: A. Systematic review of all reported caes. Am J Rhinol; 2008, 22(1): 68-73.
4. Burroughs, JR., Hernandez, Cospin, JR., Soparkar, CN.: Misdiagnosis of silent sinus syndrome. Ophtal Plast Reconstr Surg; 2003, 19(6): 449-454.
5. Davidson, JK., Soparkar, CN., Williams, JB.: Negative sinus pressure and normal predisease imaging in silent sinus syndrome. Arch Ophtalmol; 1999, 117(12): 1653-1654.
6. Hunt, SM., Tami, TA.: Sinusitis-induced enophtalmos the silent sinus syndrome. Ear Nose Throat J, 79 (8): 576-584.
7. Kass, ES., Salman, S., Montgomery, WW.: Manometric study of complete ostial occlusion in chronic maxillary atelectasis. Laryngoscope; 1996, 106(10): 1255-1258.
8. Levine, SB., Mitra, S.: Maxillary sinus involution after endoscopic sinus surgrey i a child: a case report. AmJ.Rhinol; 2000, 14 : 7-11.
9. Liss, JA., Patel, RD., Stefko, ST.: A case of bilateral silent sinus syndrome presenting with chronic ocular surface disease. Ophthal Plast Reconstruct sur; 2011, 27(6): 158-160.
10. Numa, WA., Desai, U., Gold, DR.: Silent sinus syndrome: A case presentation and comprehensive review of all 84 reported cases. AnnOtol RhinoLaringol; 2005, 114(9): 688-694.
11. Montgomery, WW.: Mucocele of the maxillary sinus causing enophtalmos. Eye Ear Nose Throat Mon; 1964, 43 : 41-44.
12. Soparkar, CN., Patrinely, JR., Cuaycong, MH. et al.: The silent sinus syndrome. A cause of spontaneous enoptahlmos. Ophtalmology; 1994, 101(4): 772-778.
13. Soparkar, CN., Patrinely, JR., Davidson, JK.: Silent sinus syndrome - new perspectives. Ophtalmology; 2004 : 111(2): 414-5, author reply 415-416.
14. Suh, JD., Ramakrishan, V., Lee, JY.: Bilateral silent sinus syndrome. Ear Nose Throat J, 2012; 91(12): 19-21.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 6-
All articles in this issue
- OČNÍ KLINIKA 1. LÉKAŘSKÉ FAKULTY UNIVERZITY KARLOVY A VŠEOBECNÉ FAKULTNÍ NEMOCNICE V PRAZE SLAVÍ 200 LET OD SVÉHO ZALOŽENÍ
- Vážený a milý pán doc. MUDr. Tomáš Mazalán, CSc.
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
- Ocular Manifestations in Patients with HIV infection
- The Importance of Evaluating the Development of Oct Findings During Conservative Treatment of Vitreomacular Traction Complicated by Macular Hole Formation
- Silent Sinus Syndrome
- Idiopathic Chodoidal Neovascular Membrane in a 12-year-old Girl
- Screening, Treatment and Long-term Observation of Retinopathy of Prematurely Born Children in the Czech Republic
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ocular Manifestations in Patients with HIV infection
- Silent Sinus Syndrome
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

