-
Medical journals
- Career
Ocular Manifestations in Patients with HIV infection
Authors: D. Linzerová 1,2; A. Stepanov 3,4; J. Němčanský 1,2
Authors‘ workplace: Fakultní nemocnice Ostrava, Oční klinika, přednosta MUDr. Jan Němčanský, Ph. D. 1; Ostravská univerzita v Ostravě, Lékařská fakulta, Katedra kraniofaciálních oborů, vedoucí katedry: prof. MUDr. Pavel Komínek, Ph. D., MBA 2; Univerzita Karlova, Lékařská fakulta v Hradci Králové, Katedra očního lékařství, vedoucí katedry: prof. MUDr. Naďa Jirásková, Ph. D., FEBO 3; Fakultní nemocnice Hradec Králové, Oční klinika, přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO 4
Published in: Čes. a slov. Oftal., 74, 2018, No. 6, p. 232-239
Category: Original Article
doi: https://doi.org/10.31348/2018/6/3Overview
Background and aims:
To evaluate the characteristics and incidence of ophthalmic manifestations in patients with HIV (Human Immunodeficiency Virus) infection.
Materials and methods: A retrospective evaluation of medical records of 147 patients with HIV infection (22 female, 125 male), the average age of 41 (range 22–79 years) examined by an ophthalmologist at the Clinic of Ophthalmology at the University Hospital Ostrava in years 1987 - 2015.
Results:
Ophthalmic manifestations of HIV were observed in 16 patients (11.9 %). There was not observed ocular involvement in patients in asymptomatic stage of HIV infection. Ophthalmic complications were observed in 1 patients (0.7 %) in early symptomatic stage and 15 patients (10.2 %) with stage AIDS (Acquired Immune Deficiency Syndrome). The most frequent ocular symptoms were caused by the virus (HIV retinopathy, mikroangiopathy) - total of 13 infected (76.5 %). Three patients had opportunity infections (17.6 %). As a result of the underlying AIDS disease 5 patients died. Ocular findings were observed at 2 of those (40.0 %).
Conclusion:
Ocular manifestation are common finding in late stages of HIV infection. Ophthalmic examination is an integral part of the diagnostic algorithm of patients with HIV infection. Most frequently, ocular symptoms have been found within the group of patients with advanced part of disease, which is in relation with the body´s immune defense decrease thus death itself.
Keywords:
HIV infection – AIDS – ophthalmic complication – opportunistic infections – HIV retinopathy – CMV retinitis
INTRODUCTION
The Human Immunodeficiency Virus (HIV) belongs to the group of retroviruses. It is transmitted by sexual intercourse, through blood and blood derivatives, infected needles, transplacentally, during birth and through mother's milk [7,14,15], resulting in HIV infection and in the advanced stage the development of AIDS (Acquired Immune Deficiency Syndrome). This virus has the ability to embed its genetic information into the genome of the host cell and bring about its chronic, lifelong persisting infection, which causes the progressive destruction of the immune system [7]. In the Czech Republic, the first case of HIV infection was diagnosed in the autumn of 1985 [7]. According to statistical data from the National Institute of Public Health (NIPH), a total number of 2620 cases of HIV positive persons have been determined in the Czech Republic in the period since the beginning of observation of the HIV infection (i.e. 1 October 1985 – 31 December 2015), of whom 2046 were citizens of the Czech Republic and 574 residents (persons with other state citizenship, with long-term residence within the territory of the Czech Republic) [24]. In recent years the Czech Republic has recorded a pronounced increase in the incidence of this infection, while worldwide this constitutes a pandemic [8, 20].
Manifestations of HIV infections are highly diverse and variable, depending on the phase of the pathology. The course of untreated infection mostly has 4 stages: primary infection (acute retroviral syndrome), asymptomatic stage, early symptomatic stage and late symptomatic stage (AIDS). The stage of primary infection of HIV usually persists for one to three weeks. The patient then enters the period of latency, during which there is a gradual intensification of immune deficiency. This stage lasts for 2-15 years, and generally produces very few clinical symptoms. The only manifestation may be persistent tumescence of the lymph nodes. Laboratory tests demonstrate a gradual deterioration of cellular immunity, characterised by a reduction of the number of CD4+ lymphocytes and accompanied by mild anaemia. A reduction of CD4+ to values below 500/μl of blood is linked with the occurrence of “small” opportunistic infections, and the patient progresses into the symptomatic stage of the pathology. Characteristic manifestations include oral candidiasis, recurring shingles, oropharyngeal candidiasis, vulvovaginitis, adnexitis, while general symptoms include fatigue, fever, diarrhoea, loss of body weight, and laboratory tests demonstrate a depletion of red blood cells. Upon a reduction of CD4+ below values of 200/μl of blood, “large” opportunistic infections appear, as well as certain tuberculous diseases (cerebral toxoplasmosis, pneumocystis pneumonia, systemic infections generated by cytomegalovirus (CMV), candida albicans, cryptosporidium, cryptococcus, atypical mycoplasmas, tuberculous diseases include Kaposi's sarcoma, lymphomas etc.), and the patient progresses into the stage of AIDS. The developed stage of HIV infection leads to the exhaustion of the organism, cachexia and death of the patient [7, 14, 15, 16].
Ocular manifestations of HIV infection
The ocular manifestations which accompanied approximately 70-80% of HIV positive patients 3, 9, 10, 12]before the introduction of antiretroviral therapy (ART) afflict the ocular adnexa, the anterior and posterior segment of the eye. They may be generated both by the HIV virus itself (microangiopathy, retinitis, neuroretinal disorder), and by opportunistic infections (CMV retinitis) and tumours (Kaposi's sarcoma, lymphoma) in the deep stage of immune deficiency [1, 6, 9, 15]. The clinical course of ocular manifestations may be influenced by ART, and similarly can be modified in the case of their coincidence. A range of these take place rapidly and have devastating consequences. However, they can be well influenced by treatment, and for this reason it is very important to ensure their timely diagnosis 1].
Manifestations not connected with opportunistic infections
The pathogenesis of these pathological changes has not been unequivocally explained. The following mechanisms are assumed – disorder of perfusion, infection of the endothelial cells with HIV, accumulation of circulating immune complexes, toxic influence of treatment of the basic pathology, leading to damage of the vascular wall, and in the case of ocular manifestations – breach of the blood-retinal barrier [1, 9, 13, 23].
Microvasculopathy is the most common ocular complication of HIV infection. It occurs in as many as 70% of patients with AIDS and in 40% of patients infected with HIV [1]. It afflicts the anterior and posterior segment of the eye, including the optic nerve. Tortuous, dilated capillaries are generally perceptible on the conjunctiva, with a discontinuous blood column and microaneurysms (MA) (Fig. 1). A typical finding on the retina is transient cotton-wool spots, caused by infarctions in the nerve fibre layer (Fig. 2). On the ocular fundus we then observe MA, haemorrhages and teleangiectasias. In rarer cases cystoid macular edema may occur. Microvascular occlusion may ultimately lead to atrophy of the disc of the optic nerve [1-3,13]. However, HIV-related microvasculopathy and retinopathy are not a sight-threatening finding. In the majority of cases they are asymptomatic, identified as a chance finding upon examination of the ocular fundus.
1. HIV microvasculopathy of the anterior segment of the eye - vascular tortuosity, intermittent blood flow, microaneurysms 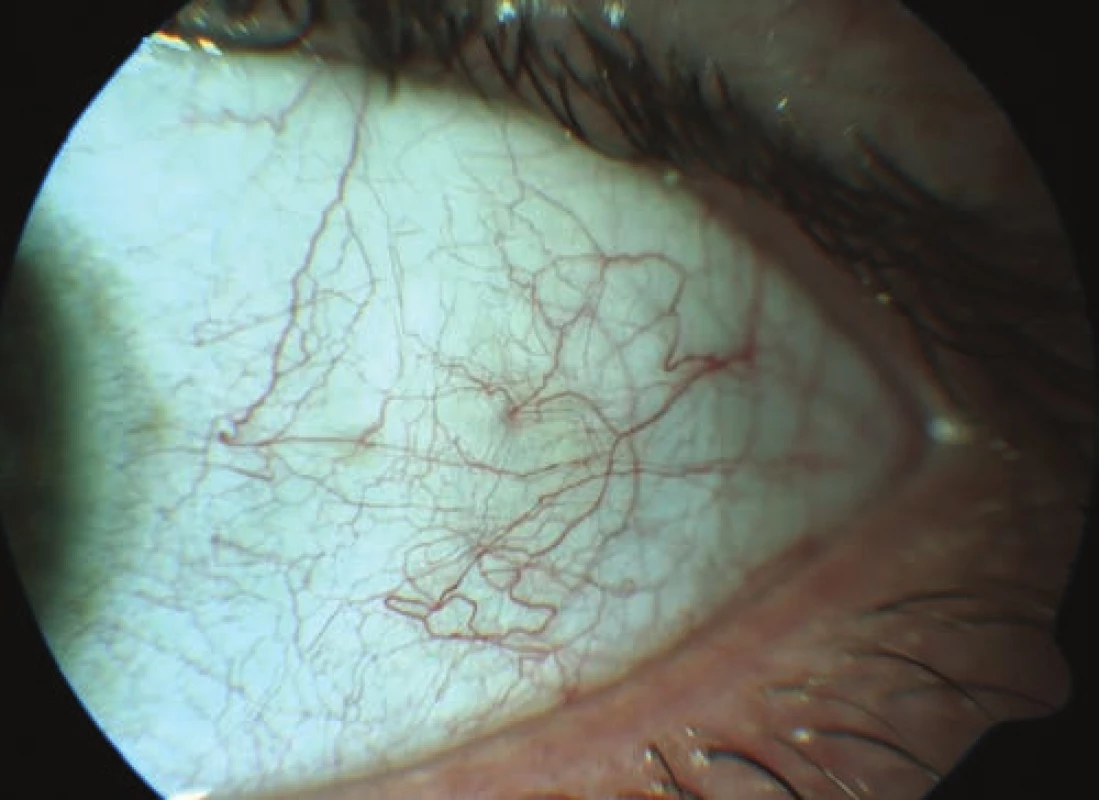
2. HIV microvasculopathy and retinopathy - haemorrhage, cotton wool spots, small microaneurysms 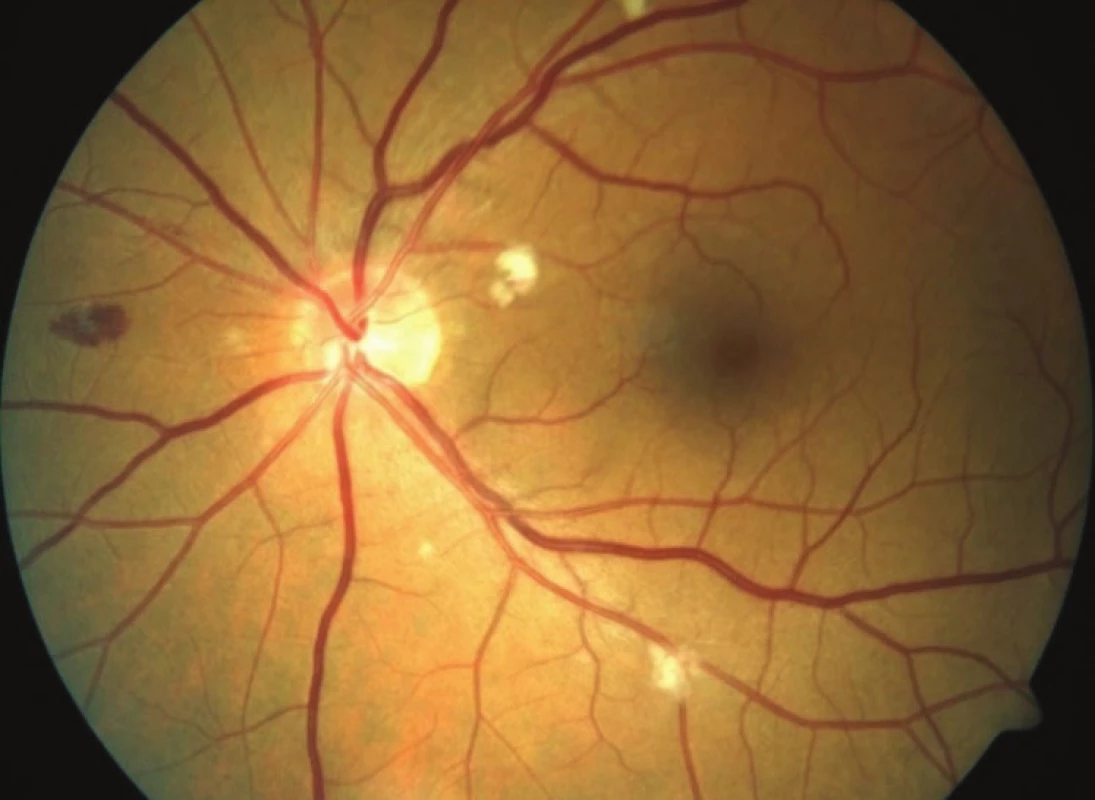
Manifestations in connection with opportunistic infections
These are caused by micro-organisms with low virulence, which trigger illness only in immune deficient individuals. Typical opportunistic pathogens are viruses, bacteria, fungi and parasites [17]. Human CMV from the group of herpetic viruses is the cause of the most common and most serious ocular opportunistic infection in HIV positive patients – CMV retinitis [1, 9, 11]. This clinical unit occurs in the stage of deep immune deficiency, in which values of CD4+ are below 100/μl of blood [22]. At present its incidence has been reduced to below 5.0 % thanks to more frequent identification of HIV infection and timely commencement of treatment [9, 11]. It nevertheless remains the most common cause of loss of sight in patients with AIDS [11, 22]. In typical cases an ophthalmological examination reveals diversely large, irregular, indistinctly bordered, yellowish-white deposits of the infiltrated retina, accompanied by haemorrhage beginning usually in the periphery, and gradually spreading along the retinal capillaries (Fig. 3). The damaged retina necrotises, and partially pigmented atrophic deposits are formed in its place, representing a locus minoris resistentiae for the occurrence of retinal detachment [1, 4, 9, 11].
3. Cytomegalovirus retinitis in a patient with HIV 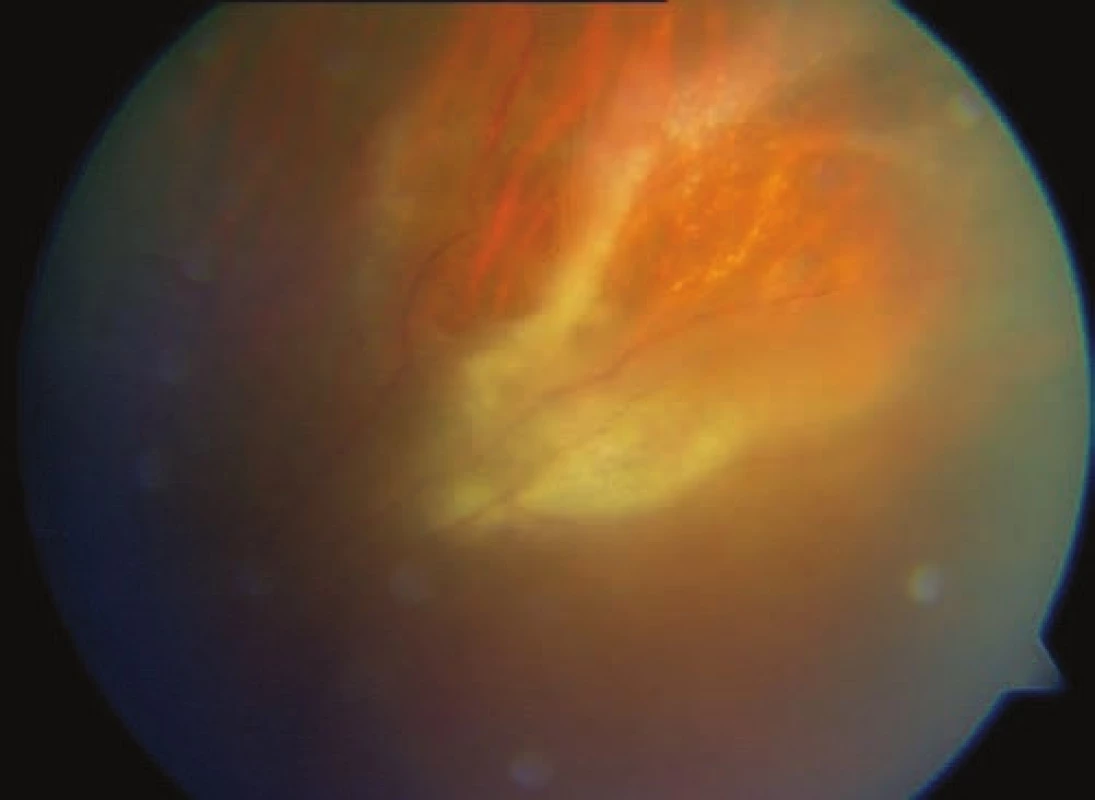
Infection triggered by the varicella zoster virus is manifested as herpes zoster ophthalmicus, afflicting the eyelids, conjunctivas and corneas, accompanied with subsequent scarry changes or post-herpetic neuralgias, or anaesthesia of the cornea with the occurrence of neurotrophic keratopathy, the development of anterior uveitis, inflammation of the optic nerve and paresis of the extraocular muscles, or as rare but very serious progressive outer retinal necrosis [4, 9].
The ocular form of toxoplasmosis, triggered by the obligate intracellular parasitic protozoa Toxoplasma gondii, is a further opportunistic infection in HIV positive patients, in whom it takes place under an image of progressive, more frequently bilateral, recurring, multifocal, necrotising chorioretinitis. Rounded, whitish, edematous saturated lesions are perceptible on the ocular fundus, accompanied by mild anterior uveitis, vitritis, vasculitis, and less frequently papillitis [1, 3, 19].
Infection caused by the herpes simplex virus may lead to a scattering of typical skin efflorescences on the eyelids, keratoconjunctivitis, anterior uveitis or in rare cases to acute retinal necrosis [9].
Tuberculous ocular manifestations
Kaposi's sarcoma, a highly vascularised formation of reddish-purple colour, is the most common tuberculous pathology in HIV positive patients. It occurs in 30-35 % of patients in the stages of AIDS [1, 3]. In the ocular localisation it is found above all on the eyelids, conjunctivas, in isolated cases also in the orbit. Malignant lymphoma occurs in HIV positive patients 100 times more frequently than in the healthy population. It may have intraocular, intraorbital and intracranial localisation [3].
METHODOLOGY
In the period from 1987 until 2015, 147 patients were examined at the Department of Ophthalmology at the University Hospital Ostrava with newly diagnosed HIV infection before the commencement of ART treatment of the basic pathology. The ocular examination included determination of best corrected visual acuity (BCVA) on a Snellen chart, determination of the values of intraocular pressure by the noncontact method, examination of the anterior segment of the eye on a slit lamp and examination of the posterior segment of the eye biomicroscopically in artificial mydriasis.
The observed parameters included: incidence and nature of ocular affliction, clinical stage of pathology and depth of immune deficiency characterised by the absolute number of CD4+ lymphocytes, age, sex, manner of transmission of infection and mortality rate of HIV positive patients. The epidemiological parameters of the patients from our cohort are presented in table 1.
1. Epidemiological data of patients in our study 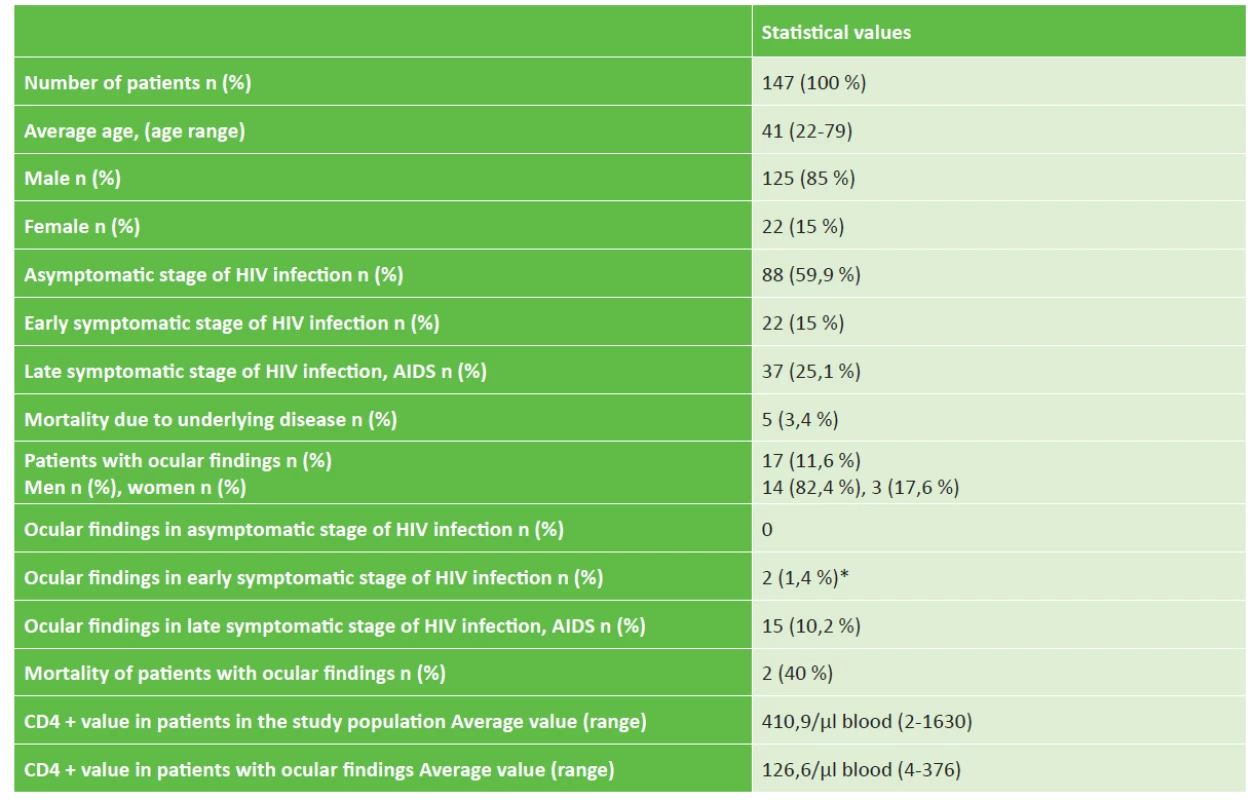
* U jednoho pacienta se jednalo o inaktivní oční formu toxoplazmózy RESULTS
The observed cohort comprised a total of 147 HIV positive persons (22 women, 125 men) with an average value of CD4+ 410.9/μl of blood. From this cohort a pathological ocular finding (table 2) was described in 17 patients (11.6 %) with an average value of CD4+ 126.6/μl of blood. In 14 cases this concerned patients of male sex (82.4 %), in 3 cases of female sex (17.6 %). In the patients in the asymptomatic stage we did not record any pathological ocular manifestations of HIV infection. In the patients in the early symptomatic stage of HIV infection, a pathological ocular finding was described in two cases. In one patient this concerned an inactive ocular form of toxoplasmosis. However, it is debatable as to whether this finding had any connection with the HIV infection. It is probable that activity of toxoplasma chorioretinitis had occurred in the distant past and so we did not evaluate it as an ocular complication of HIV. In the second case a finding of conjunctival microangiopathy was documented (fig. 1). In patients who had developed AIDS (late symptomatic stage of HIV infection), ocular affliction was found in 15 cases (10.2 %). Here the predominant part comprised manifestations brought about by the action of the virus itself (HIV retinopathy and microangiopathy) – 12 cases (8.2 % of the total number, 80 % of patients in the advanced stage of HIV). Opportunistic infections in this group of patients were represented in 3 cases (2.0 % of the total number, 20.0 % of patients in the advanced stage of HIV). Ocular form of toxoplasmosis was diagnosed in one patient (0.7 % of total number, 6.7 % of patients in the advanced stage of HIV). A finding of severe CMV retinitis was determined in two cases (1.3 % of total number, 13.3 % of patients in the advanced stage of HIV) (table 3, graph 1). The appearance of malignant ocular pathologies was not recorded in any of the patients in the observed cohort. As a consequence of the basic pathology, which led to a complete exhaustion and subsequently to a failure of the defensive capabilities of the organism, 5 patients died during the observation, in which a pathological ocular finding (CMV retinitis) was present in two cases (40.0 %). Sexual intercourse was confirmed as the most frequent manner of transmission of the infection in the group as a whole, wherein homosexual men were represented in the largest percentage. Transmission by means of a transfusion of blood derivatives in a patient with haemophilia was recorded in one case from the entire cohort of patients, which occurred before the introduction of mandatory testing of blood donors.
2. Ocular manifestations in HIV / AIDS patients - basic distribution 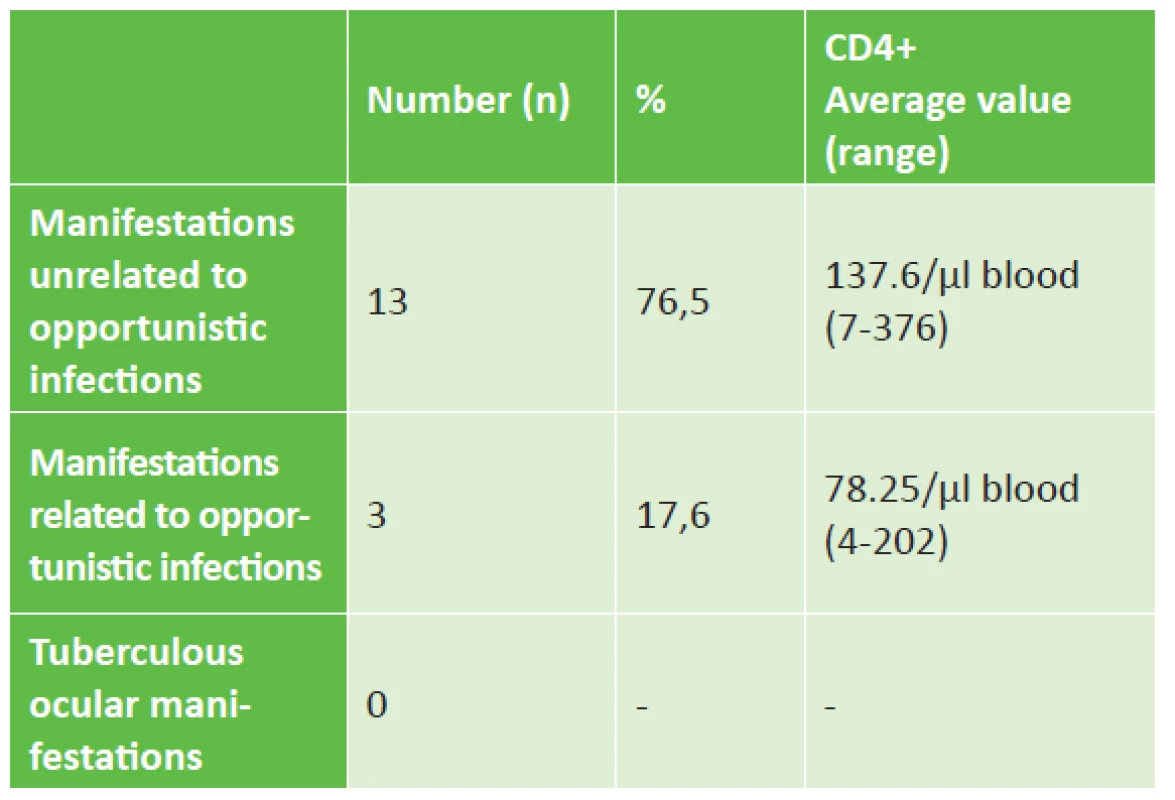
3. Ocular manifestations in HIV / AIDS patients in our study 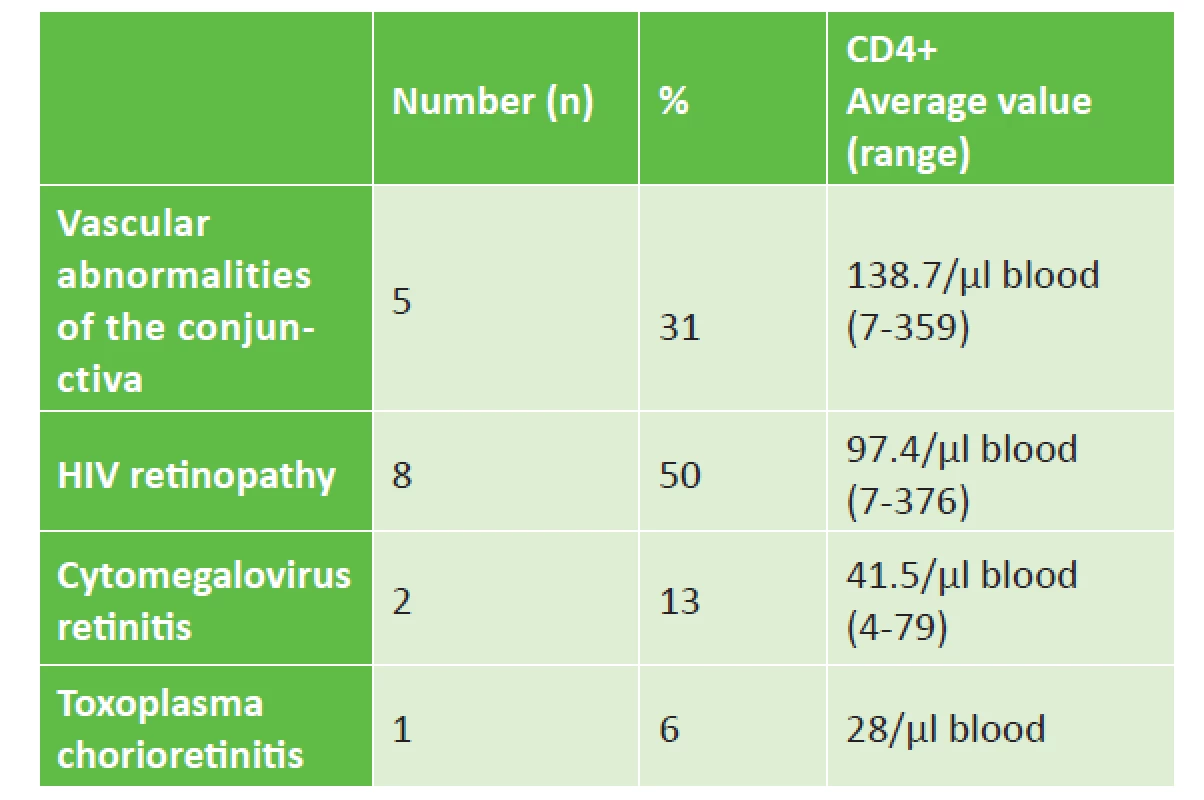
1. Ocular symptoms in HIV / AIDS patients in our study 
DISCUSSION
In terms of the representation of men and women, the manner of infection with the HIV virus and the correlation of the immune condition of the infected patients with ocular manifestations, our results corresponded with the previously published studies [5, 18, 21, 22].
Kožner et al., as well as other authors, state an incidence of ocular manifestations at approximately 70-80 % of all HIV positive patients [3, 9, 12]. However, thanks to the introduction of highly effective combined ART their incidence has been markedly reduced [10, 11, 18, 22]. In our cohort, an ocular finding was determined in a total of 17 patients (11.6 %), with the highest prevalence in patients in the developed stage of AIDS (15 cases – 10.2 %). This number is slightly lower in comparison with the cited publications. In addition to advances in the treatment of HIV positive patients, it is possible to explain this fact also by means of the early diagnosis of this pathology, and the thus ensuing higher representation of patients in the asymptomatic stage of HIV at the initial ophthalmological examination (59.9 % of all HIV positive patients in the observed cohort). Another reason for the low incidence of ocular symptoms in our cohort is the evaluation only of the initial examination, in contrast with the above-stated authors.
The most common ocular manifestation of HIV infection is microangiopathy on the ocular fundus [1, 9, 10], which we observed also in our cohort. Bowling and a range of other authors [1, 3, 4, 9, 10, 15, 19] state its incidence in 50-70 % of cases in patients with AIDS. In numerical values our results diverge from the cited literature. We observed HIV microangiopathy in 15 patients (10.2 %). In 14 cases this concerned patients in the late symptomatic stage of HIV (which represents 37.8 % of all patients in the stage of AIDS) and in one case in the early symptomatic stage of HIV infection (4.5 % of all patients in this stage). In addition to the above-stated factors (effective ART, higher representation of patients in the asymptomatic stage), this discrepancy could also be explained by the fact that the presence of microangiopathy is a transitional, ephemeral finding, which in the majority of cases is asymptomatic. Its incidence ensues from the immune condition of the patient, which is highly variable during the course of the pathology. HIV retinopathy therefore need not be identified during the initial examination.
The incidence of CMV retinitis was recorded in two cases (1.4 %), toxoplasma chorioretinitis in only one case (0.7 %). A similar prevalence of the symptoms can be seen also in the cited literature [3, 9, 11].
This study has a number of limitations. The chief limitation is the absence of an evaluation of the development of the ocular finding over time in the individual patients, which could give our results an entirely different dimension. However, the scope of such an evaluation comes up against a number of obstacles (e.g. the transition of the individual patients between stages) and overall exceeds the framework of the given study, though it shall be the subject of a further analysis. Another limit is the absence of the observed data in the patients in the terminal stage of HIV infection, who were not included in the observed cohort because it was not possible to perform an ocular examination in them over time.
CONCLUSION
Ocular manifestations are very diverse and relatively frequent in the case of HIV infection, which we demonstrated in our cohort of patients. Regular ophthalmological examination ranks among standard care of HIV positive patients. Its primary aim is the prevention of irreversible damage to sight. It also enables indirect monitoring of long-term compensation of the immune condition of the HIV positive patient, the effectiveness of treatment, any applicable development of resistance or compliance of the patient. In some patients ocular manifestations are the first clinical symptom of HIV infection, and may thus reveal that a patient is HIV positive. Thanks to timely prophylaxis of opportunistic infections and the introduction of highly effective ART, there has been a pronounced reduction of ocular manifestations, above all of sight-threatening CMV retinitis, which, despite intensive treatment, remains the most frequent cause of blindness in HIV positive patients.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received by the Editorial Department on: 30 September 2018
Accepted for printing on: 19 December 2018
Corresponding author:
MUDr. Alexandr Stepanov, Ph.D., FEBO
Ophthalmology Clinic at the University Hospital in Hradec Králové
Sokolská 581
Hradec Králové, 500 05
Sources
1. Ahmed, I., Ai, E., Chang, E. et al.: Ophthalmic manifestations of HIV. HIV insite knowledge base chapter [online]. University of California, San Francisco, USA. August 2005; Content reviewed January 2006. [cit. 10. 4. 2016]. Dostupné na www: http://hivinsite.ucsf.edu/InSite?page=kb-04-01-12
2. Bartsch, D.U., Kozak, I., Grant, I. et al.: Retinal nerve fiber and optic disc morphology in patients with human immunodeficiency virus using the Heidelberg Retina Tomography 3. PLoS One, 10 (8); 2015: e0133144.
3. Boguszaková, J.: Oko a celková onemocnění. In Kuchynka, P., a kol., Oční lékařství. Praha, Grada, 2016, s. 859-861.
4. Bowling, B.: Kanski‘s Clinical Ophthalmology. Elsevier, 2016, p. 437-443.
5. Chiotan, C., Radu, L., Serban, R. et al.: Cytomegalovirus retinitis in HIV/AIDS patients. J Med Life, 7 (2); 2014 : 237–240.
6. Jabs, D.A., Drye, L., Van Natta, M.L. et al.: Incidence and long-term outcomes of the human immunodefıciency virus neuroretinal disorder in patients with AIDS. Ophthalmology, 112 (4); 2015 : 760-768.
7. Jilich, D., Kulířová, V. a kol.: HIV infekce – Současné trendy v diagnostice, léčbě a ošetřovatelství. Praha, Mladá fronta a.s., 2014, 173 s.
8. Konvalinka, J., Machala, L.: AIDS – mor pro 21. století. In Konvalinka, J., Machala, L., Viry pro 21. století. Praha, Academia, 2013, s. 42-66.
9. Kožner, P., Machala, L., Filouš, A. et al.: Přehled vývoje okulárních oportunních infekcí u HIV pozitivních pacientů. Cesk Slov Oftalmol, 65 (1); 2009 : 36-38.
10. Kožner, P., Machala, L., Rozsypal, H. et al.: HIV retinopatie. Klin mikrobiol inf lék, 15 (5); 2009 : 183-184.
11. Kožner, P., Rozsypal, H., Machala, L. et al.: Dva typy cytomegalovirového postižení oka u pacientů s HIV infekcí. Klin mikrobiol inf lék, 15 (5); 2009 : 180-182.
12. Kraus, H.: Oko a celková onemocnění. In Kraus, H., Kompendium očního lékařství. Praha, Grada, 1997, s. 277-284.
13. Pichi, F., Romani, P., Carrai, P. et al.: Think out of the box, think out of the eye reappraisal of HIV/AIDS retinopathy. Med Hypothesis Discov Innov Ophthalmol, 3 (3); 2014 : 65-70.
14. Podrobný popis HIV/AIDS. Národní program boje proti AIDS v České republice. Státní zdravotní ústav. Praha. [cit. 31. 3. 2016]. Dostupné na www: http://www.prevencehiv.cz/informace/podrobny-popis-hivaids/
15. Rozsypal, H.: AIDS klinický obraz a léčba. Praha, Maxdorf, 1998, 236 s.
16. Rozsypal, H.: Infekce lidským virem imunodeficience (HIV): Rozpoznání a počáteční posouzení. In Rozsypal, H., Základy infekčního lékařství. Praha, Karolinum, 2015, s. 381-387.
17. Rozsypal, H.: Zdravotní komplikace infekce lidským virem imunodeficience (HIV). In Rozsypal, H., Základy infekčního lékařství. Praha, Karolinum, 2015, s. 393-401.
18. Ruiz-Cruz, M., Alvarado-de la Barrera, C., Ablanedo-Terrazas, Y. et al.: Proposed clinical case definition for cytomegalovirus-immune recovery retinitis. Clin Infect Dis, 59 (2); 2014 : 298-303.
19. Říhová, E.: Uveitidy. Praha, Grada, 2009, s. 29-36.
20. Staňková, M., Marešová, V., Vaništa, J.: Nákaza virem HIV. In Staňková, M., Marešová, V., Vaništa, J.: Repetitorium infekčních nemocí. Praha, Triton, 2008, s. 139-143.
21. Staňková, M., Rozsypal, H., Hynie, J.: Cytomegalovirivá retinitida – současné terapeutické možnosti (První použití cidofoviru v ČR). Klin mikrobiol inf lék, 4 (5); 1998 : 150-153.
22. Stepanov, A., Feuermannová, A., Hejsek, L. et al.: Cytomegalovirivá retinitida u pacienta se syndromem získané imunodeficience. Cesk Slov Oftalmol, 70 (4); 2014 : 132-137.
23. Tan, S., Duan, H., Xun, T. et al.: HIV-1 impairs human retinal pigment epithelial barrier function: possible association with the pathogenesis of HIV-associated retinopathy. Lab Invest, 94 (7); 2014 : 777–787.
24. Trendy vývoje a výskyt HIV/AIDS v ČR v roce 2015. Tisková zpráva Národní referenční laboratoře pro HIV/AIDS. Praha. Státní zdravotní ústav. 29. 1. 2016. [cit. 25. 5. 2016]. Dostupné na www: http://www.szu.cz/uploads/documents/CeM/HIV AIDS/rocni_zpravy/2015/Tiskova_zprava_NRL pro HIV AIDS v CR v roce 2015.pdf
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 6-
All articles in this issue
- OČNÍ KLINIKA 1. LÉKAŘSKÉ FAKULTY UNIVERZITY KARLOVY A VŠEOBECNÉ FAKULTNÍ NEMOCNICE V PRAZE SLAVÍ 200 LET OD SVÉHO ZALOŽENÍ
- Vážený a milý pán doc. MUDr. Tomáš Mazalán, CSc.
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
- Ocular Manifestations in Patients with HIV infection
- The Importance of Evaluating the Development of Oct Findings During Conservative Treatment of Vitreomacular Traction Complicated by Macular Hole Formation
- Silent Sinus Syndrome
- Idiopathic Chodoidal Neovascular Membrane in a 12-year-old Girl
- Screening, Treatment and Long-term Observation of Retinopathy of Prematurely Born Children in the Czech Republic
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ocular Manifestations in Patients with HIV infection
- Silent Sinus Syndrome
- Virtiol – Simulation of Quality of Vision with Multifocal and Edof Intraocular Lenses
- Corticosteroid Induced Posterior Subcapsular Cataract
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

