-
Medical journals
- Career
Pilot Results of Implantation of the New Hydrophobic Intraocular Lens Zeiss LUCIA 611P in the Czech Republic
Authors: A. Stepanov; P. Rozsíval; M. Středová; J. Nekolová; N. Jirásková
Authors‘ workplace: Fakultní nemocnice Hradec Králové, Oční klinika, přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO ; Univerzita Karlova, Lékařská fakulta v Hradci Králové, katedra očního lékařství
Published in: Čes. a slov. Oftal., 74, 2018, No. 5, p. 192-196
Category: Original Article
doi: https://doi.org/DOI: 10.31348/2018/5/4Overview
Background:
Cataract surgery is one of the most common procedures performed by the ophthalmic surgeon. In this paper, we evaluate of postoperative results of the hydrophobic intraocular lens CT LUCIA 611 in patients undergoing routine cataract surgery.
Methods:
The study included 23 patients (29 eyes), average age of 69.0 + 9.2 years (span 53 to 86 years) with uncomplicated senile cataract. After phacoemulsification, CT LUCIA 611 intraocular lenses were implanted. Patients were examined 3 months and 6 months after surgery. Uncorrected visual acuity (UVA), best-corrected visual acuity (BCVA), refraction, occurrence of opacities of the posterior capsule, and subjective contentment of patients according to the questionnaire VF-14 (visual functioning) were examined.
Results:
3 months after surgery, the average UVA was 0.68 ± 0.4, and BCVA 0.92 ± 0.3. Half-a-year after surgery, UVA was 0.82 ± 0.1 and BCVA 0.94 ± 0.2. Good uncorrected visual acuity and a minimal occurrence of opacities of the posterior capsule corresponded with a high degree of contentment of patients.
Conclusions:
On the basis of the author’s present experience it can be concluded that the Zeiss CT LUCIA 611 intraocular lens exhibits good and stable postoperative results.
Key words:
intraocular lens CT LUCIA 611; posterior capsule opacity; phacoemulsification
INTRODUCTION
The single-piece monofocal aspherical intraocular lens CT LUCIA 611P is an innovative model of artificial intraocular lenses from the Zeiss company. It is produced from a unique hydrophobic acrylate polymer, the surface of the lens is covered with heparin, which provides better resistance against the occurrence and progression of posterior capsule opacification (PCO) (5). The material of the lens is also resistant to glistening (7). In hydrated state the diameter of the optical part is 6.0 mm. The patented aspherical Zeiss lens compensates for physiological spherical aberration and preserves the depth of field. The improved construction of the “C-loop” haptics with specialised curvature without angulation guarantees a further improved position in the capsular sac and also eliminates contact with the tissue of the iris. It is implanted in the eye with the aid of a pre-filled injector, without the necessity of folding or direct contact of the lens, with an incision of 2.2 – 2.6 mm. In this report we present the postoperative results of patients in whom this intraocular lens has been implanted.
COHORT AND METHOD
The CT LUCIA 611P intraocular lens (IOL) was implanted in a total of 29 eyes of 23 patients with an average age of 69.0 ± 9.2 (range 53 to 86) years at the Department of Ophthalmology of the University Hospital in Hradec Králové in the period from November 2016 to August 2017. Informed consent was obtained from each patient. Table 1 summarises the information about the patients and the preoperative data. All the operations were performed using the same surgical technique: instillation anaesthesia, corneal incision with a size of 2.2 mm, creation of lateral auxiliary incisions, capsulorhexis of the size of 5 mm, hydro-dissection, phacoemulsification of the nucleus, irrigation and aspiration of the cortex and implantation of the IOL CT LUCIA 611P into the remainder of the lens capsule.
1. Patients and preoperative data 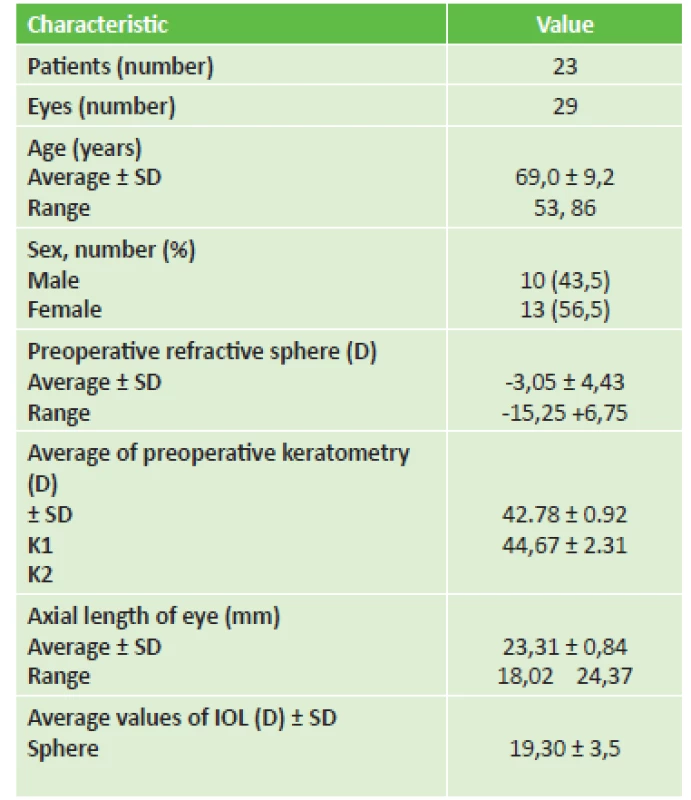
IOL = intraocular lens Preoperatively we examined uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) of the patients on Snellen's optotypes (Decimal) and measured the axial length of the eyeball. For calculation of the optical power of the IOL we used an instrument IOL Master 700 Carl Zeiss Meditec AG, we examined the patients on a slit lamp.
Postoperatively the patients were examined 3 months and 6 months after surgery. At these follow-up examinations we observed refraction, UCVA, BCVA, incidence of PCO on a scale of 1 to 4, and we also evaluated subjective patient satisfaction according to the questionnaire VF-14 (visual functioning) (9). The patients were also asked about postoperative visual phenomena (e.g. halo, starburst, vision with ghosting, decrease of contrast sensitivity). Postoperatively we also evaluated the reaction in the anterior chamber, centration of the intraocular lens and other postoperative complications.
For a statistical analysis of the preoperative and postoperative data, we used SPSS Windows software (version 18.0). A Kolmogorov-Smirnov test was conducted for normality, a pair t-test for comparison of the parameters between the preoperative and postoperative examinations, a P value of 0.05 or less was considered statistically significant.
RESULTS
A total of 23 patients (29 eyes) completed the observation period, of which 16 were eyes of women and 13 of men. No complications were recorded either perioperatively or postoperatively. Table 2 summarises the preoperative and postoperative refractive data, UCVA, BCVA (Decimal) and the incidence of posterior capsule opacities (PCO). Before surgery BCVA was 0.49 ± 0.2, 3 months after surgery BCVA had improved to 0.92 ± 0.3 (p = 0.0475) and 6 months after surgery it was 0.94 ± 0.2 (p = 0.0063). Postoperative BCVA was 0.8 or better in 27 eyes (93%) and 1.0 or better in 16 eyes (55%). Refraction was evaluated preoperatively, in which the average value of spherical correction was -3.05 ± 4.43 D, range -15.25 to +6.75. 3 months after surgery the average value of spherical correction was 0.4 ± 0.8 D, range -1.25 to +1.5. 6 months after surgery this value was 0.3 ± 1.1 D, range -1.75 to +1.75. The median value of incidence of posterior capsule opacities of CT LUCIA 611P 3 months after surgery was 0.05 ± 0.2, 6 months after surgery 0.11 ± 0.2, which documents entirely minimal incidence of PCO. Centration of the IOL in the capsule was correct in all eyes. Optical or visual phenomena did not cause the patients any difficulties. The results of subjective patient satisfaction are presented in table 3 (questionnaire VF-14). All the surgeons evaluated the ease of implantation of the IOL with the aid of a pre-filled injector as very safe and easy
2. Preoperative and postoperative values of visual acuity and refraction 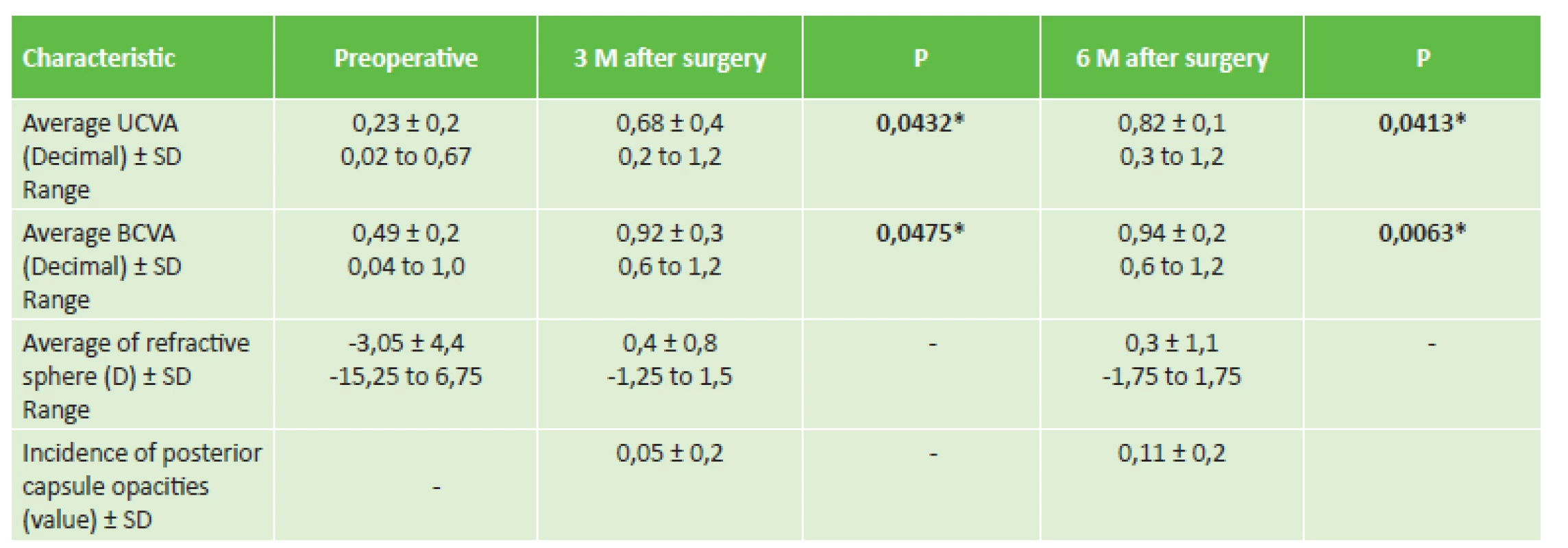
* P value signals statistically significant difference at 5% level of significance
UCVA = uncorrected visual acuity
BCVA = best corrected visual acuity
SD = standard deviation3. Subjective patient satisfaction 6 months after implantation of IOL CT LUCIA 611P (questionnaire VF-14) 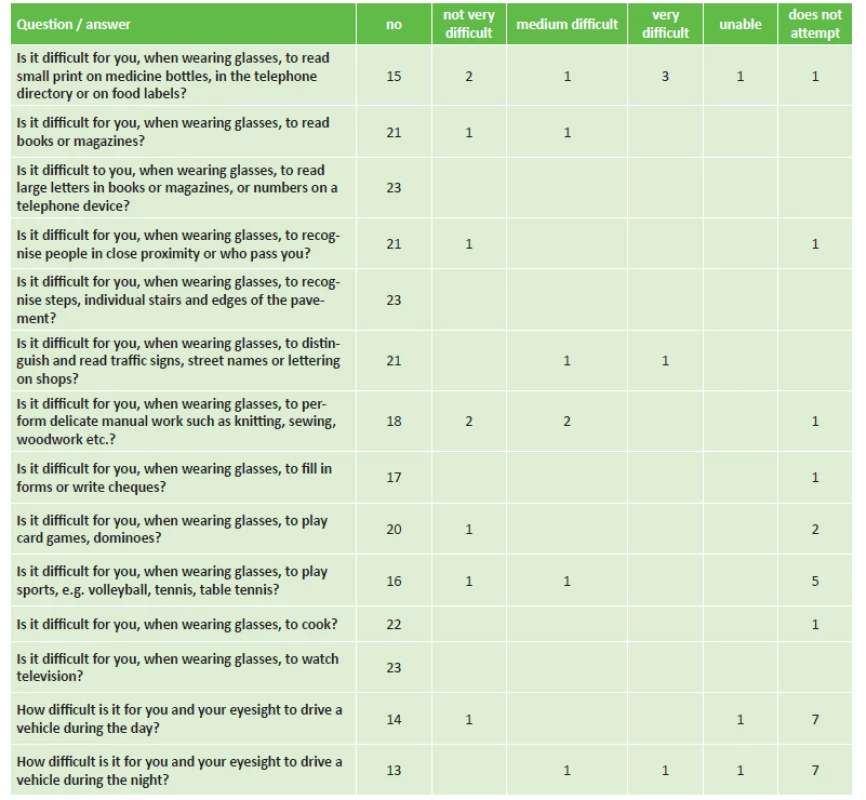
According to Steinberger (9) DISCUSSION
The progression of PCO is a long-term complication, which in the 1970s and 80s led to a deterioration of visual acuity requiring a further surgical procedure in 50 to 100% of the patients within 5 years after cataract surgery. The high prevalence of secondary cataract, the financial costs for its solution and the potential complications were and are the reason for the high level of interest in its prevention among ophthalmologists. In the 1990s, with research into the etiopathogenesis of secondary cataract and the introduction of the first preventive measures, the incidence of secondary cataract within five years of surgery was reduced to approximately 20-30% (10). At the beginning of the 3rd millennium, the incidence of PCO within 5 years of primary surgery had been reduced to values around 10%.
The incidence of PCO is influenced by several factors, some of which we can influence and others not. Those factors which are difficult to influence include race, age and other ocular pathologies. The factors which we can influence include the surgical technique and the properties of the IOL (size, shape and edge of the optical part, shape of the haptic part and last but not least also the material from which the intraocular lens is produced) (1-3, 8, 9). The first and longest-known group is hard (inflexible) materials, for the production of which polymethylmethacrylate is used. With regard to the fact that hard lenses produced from PMMA cannot be folded, a wide incision is required for their implantation. Another group is soft materials and expandable materials, which following implantation increase their volume as a result of hydration. We divide soft materials into silicone elastomers and acrylate/methacrylate polymers, and further divide these according to their water content into hydrophilic and hydrophobic. The main advantages of hydrophilic IOLs include easy handling, quick return of the folded lens to its original shape, lesser susceptibility to damage and the possibility of implantation via micro-incision. Hydrophobic acrylate material forms bioactive bonds with fibronectin, an extracellular protein, which results in the generation of a “sandwich structure” (4). Such a connection improves the rotation stability of the intraocular lens, reduces the incidence of posterior capsule opacification and provides adequate resistance against contraction of the capsular casing. The use of acrylate as a material for the production of intraocular lenses began relatively recently. It was approved by the Food and Drug Administration in December 1994, and after 1998 acrylate became the material of first choice among operating surgeons (11).
In their shape, artificial lenses attempt to approximate a crystalline lens, and are therefore mostly of a biconvex shape. A biconvex shape guarantees good optical properties and easier adherence to the posterior capsule of the lens, thus reducing the risk of occurrence and progression of PCO. The anterior and posterior surface of the biconvex optical parts may have either a rounded contact or may be of a “square-edge” design. It has been demonstrated that square-edge lenses prevent the migration of epithelial cells and thereby reduce the risk of occurrence of PCO, regardless of the material from which the lens is produced (6). The edge of the evaluated lens CT LUCIA 611P has a 360° “square-edge” design, in addition to which the surface of the IOL is covered with heparin, which prevents the occurrence and progression of PCO and provides better resistance against glistening (2, 7, 11). The value of the PCO index for the CT LUCIA 601P 6 months after surgery was 0.11 ± 0.2, which indicates an entirely minimal incidence of PCO.
The improved construction of the “C-loop” haptics, with special curvature without angulation, guarantees a further improved stabilisation and fixation of the lens in the sac. In our cohort also, we demonstrated good stability of the IOL in the capsule. The intraocular lens we observed has neutral asphericity, which eliminates the existing spherical aberration of the lens, compensates for physiological ocular asymmetry (Kappa angle), does not alter the physiological corneal aberration and preserves the depth of field. No complications were observed in connection with the use of new intraocular lenses. A wide range of dioptres are available from +4.0 to +30.0 D. The lens meets the strictest demands: total size 13 mm, the optical part has a diameter of 6 mm, aspherical patented optics Zeiss (fig. 1). A variant of the lens with “natural” yellow filter also exists, which preserves maximum contrast sensitivity and provides maximum protection of the macula – CT LUCIA 611PY (2). A large advantage of the CT LUCIA 611P lens is its packaging, in which the IOL is supplied with an injector (fig. 2), into which a cartridge with the IOL is inserted, and without any further handling and contact with the surface of the eye the IOL is implanted into the remainder of the capsule of the patient's own lens. An improved injector with a soft stop end (Figure 3) enables even easier implantation of IOL. This study is the first in the Czech Republic which describes the results of short-term evaluation following the application of hydrophobic intraocular lenses CT LUCIA 611P in a group of patients undergoing routine cataract surgery.
2. Injector of lens CT LUCIA 611P (Y) 
3. Soft stop end of injector of CT LUCIA 611P (Y) 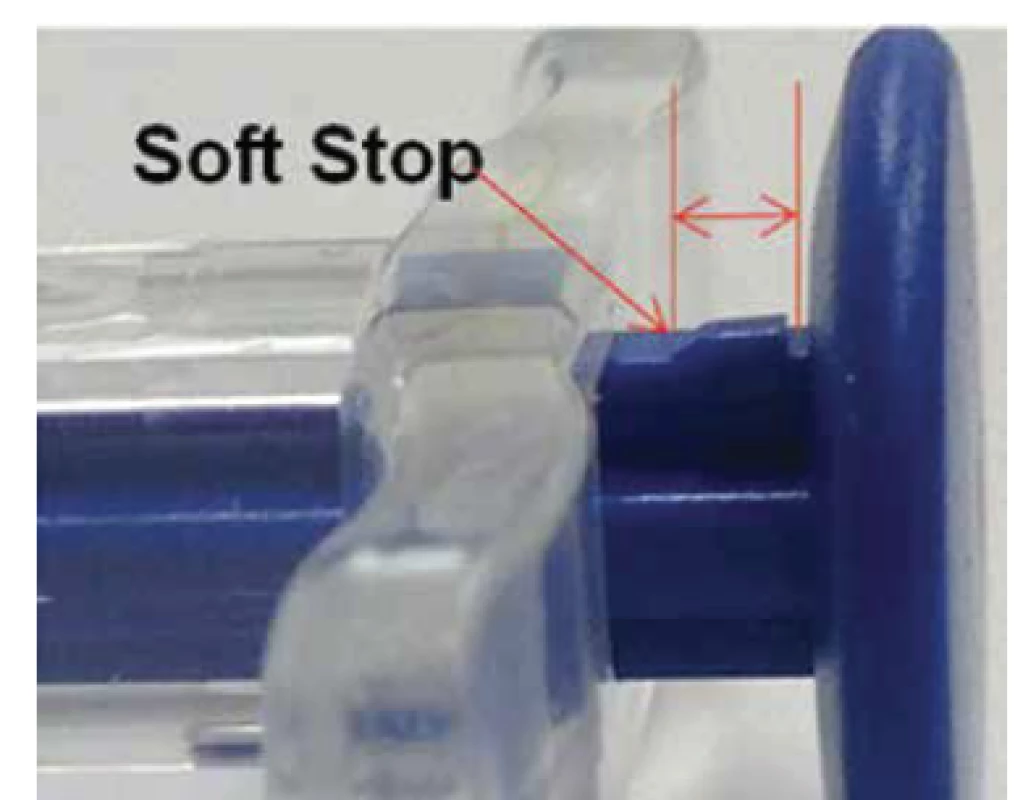
CONCLUSION
On the basis of our experience, it is possible to state that the intraocular lens CT LUCIA 611P from the Zeiss company, thanks to its pre-filled injector, is easily implanted into the eye, and also demonstrates good, and at the time of observation also stable postoperative results in patients undergoing routine cataract surgery. These lenses are linked with a high degree of satisfaction among both patients and surgeons.
This study was presented at the 25th annual congress of the Czech Ophthalmology Society of the Czech Medical Association of J.E. Purkyně in Brno, 14 September 2017.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company
Received: 11. 9. 2018
Accepted: 3. 11. 2018
Available on-line: 27. 3. 2019
MUDr. Alexandr Stepanov, Ph.D., FEBO
Oční klinika Fakultní nemocnice Hradec Králové
Sokolská 581
500 05 Hradec Králové
Sources
1. Adámková, H., Novák J.: Sekundární katarakta, její prevence a léčba. Část první: Prevence vzniku sekundární katarakty. Cesk Slov Oftalmol, 62(3); 2006 : 230–236.
2. Bosc, JM.: Initial impressions and early clinical results of a new single-piece hydrophobic yellow acrylic IOL. Presented at the ASCRS Symposium on Cataract, IOL, and Refractive Surgery, San Francisco, 2009.
3. Jirásková, N., Rozsíval, P.: Metody hodnocení zkalení zadního pouzdra po operaci katarakty. Cesk Slov Oftalmol, 60(2); 2004 : 155–157.
4. Linnola, RJ.: The sandwich theory: a bioactivity based explanation for posterior capsule opacification after cataract surgery. J Cataract Refract Surg, 23; 1997 : 1539-1542.
5. Maedel, S., Hirnschall, N., Chen, YA., et al.: Effect of heparin coating of a foldable intraocular lens on inflammation and capsular bag performance after cataract surgery. J Cataract Refract Surg, 39(12); 2013 : 1810-1817.
6. Nishi, O., Yamamoto, N., Nishi, K., et al.: Contact inhibition of migrating lens epithelial cells at the capsular bend created by a sharp-edged intraocular lens after cataract surgery. J Cataract Refract Surg, 33; 2007 : 1065–1070.
7. Rosca, G.: High precision injection with a new heparin coated hydrophobic one piece IOL. Presented at ASCRS, Chicago, 2012.
8. Spalton, DJ.: Posterior capsular opacification after cataract surgery. Eye (Lond), 13; 1999 : 489–492.
9. Steinberg, EP., Tielsch, JM., Schein, OD., et al.: The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol, 112(5); 1994 : 630-638.
10. Wormstone, IM., Liu, CS., Rakic, JM., et al.: Human lens epithelial cell proliferation in a protein-free medium. Invest Ophthalmol Vis Sci, 38; 1997 : 396–404.
11. Zemaitiene, R., Jasinskas, V., Barzdziukas, V. et al.: Prevention of posterior capsule opacification using different intraocular lenses (result of one-year clinical study). Medicina (Kaunas), 40(8); 2004 : 721–730.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 5-
All articles in this issue
- Ocular Manifestations of Granulomatosis with Polyangiitis
- Yield of Display Modules of Corneal Tomography for Early Diagnosis of Corneal Ectasia
- Changes of Central Corneal Thickness in Normotensive and Hypertensive Glaucoma
- Pilot Results of Implantation of the New Hydrophobic Intraocular Lens Zeiss LUCIA 611P in the Czech Republic
- Merkel Cell Carcinoma of the Eyelids (Clinical-Histological Study)
- Pachychoroid Disease of the Macula – Case Report
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ocular Manifestations of Granulomatosis with Polyangiitis
- Merkel Cell Carcinoma of the Eyelids (Clinical-Histological Study)
- Pachychoroid Disease of the Macula – Case Report
- Pilot Results of Implantation of the New Hydrophobic Intraocular Lens Zeiss LUCIA 611P in the Czech Republic
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career



