-
Medical journals
- Career
Changes of Central Corneal Thickness in Normotensive and Hypertensive Glaucoma
Authors: J. Lešták; Š. Pitrová; E. Nutterová
Authors‘ workplace: Oční klinika JL Fakulty biomedicínského inženýrství ČVUT, V Hůrkách 1296/10, 158 00 Praha 5 – Nové Butovice, přednosta: doc. MUDr. Ján Lešták, CSc, MSc, MBA, LLA, DBA, FEBO, FAOG
Published in: Čes. a slov. Oftal., 74, 2018, No. 5, p. 186-189
Category: Original Article
doi: https://doi.org/10.31348/2018/5/3Overview
The objective of the study
was to determine whether there exists a difference in the central cornea thickness (CCT) in patients with hypertensive (HTG) and normotensive glaucoma (NTG), and subsequently, to compare the application of prostaglandins by corrected CCT (CCT correction) for both types of glaucoma.
Material and methods:
100 eyes of 50 patients (the average age of 67) with HTG and 100 eyes of 50 patients (the average age of 62.6) with NTG were examined. Antiglaucomatics, if indicated, were taken by the patients for at least the preceding five years. The excluding criteria in the study were: cornea diseases, post-laser procedure conditions and high ametropia. CCT was measured by means of Tomey Handy Pachymeter SP100 by the same physician.
Results:
A two-sample t-test was applied in order to compare the measurement values of CCT and the subsequent correction of these values (CCT correction) in patients with HTG and NTG. The statistical evaluation showed that in case of both CCT and CCT correction, the values were lower in the group of NTG patients in comparison with HTG patients. With respect to CCT, the difference was statistically insignificant (NTG 554.9±35.7 vs. HTG 561.4 ± 32.7, p = 0.181). In case of CCT correction, the difference was more considerable, but still statistically insignificant (NTG 550.8 ± 35 vs. HTG 559.6 ± 33.1, p = 0.06).
Conclusion:
CCT was higher in NTG than in HTG; however, these values were statistically insignificant. A comparison of the application of prostaglandins of corrected CCT (CCT correction) for both types of glaucoma increased the difference, but this difference was still statistically insignificant. This difference was caused by an uneven representation of patients treated with prostaglandins in both groups.
Key words:
hypertensive glaucoma, normotensive glaucoma, central cornea thickness, prostaglandins
INTRODUCTION
Glaucoma is still considered one of the main causes of pronounced disorders of vision and blindness in advanced countries. It is generally known that intraocular pressure is indicated as the most significant risk factor of this pathology. Hypertensive glaucoma (HTG) is defined as chronic progressive neuropathy with excavation and atrophy of the disc of the optic nerve and subsequent changes in the visual field, where the main role is played by higher intraocular pressure. In the case of HTG, the ganglion cells are damaged diffusely throughout the entire retina, with subsequent necrosis of their axons. At the same time, however, there is also damage to the ganglion cells of subcortical and cortical centres in the brain.
In comparison with HTG, NTG is different in a number of aspects: in addition to the level of intraocular pressure, there are also changes in the visual field which in NTG cause more damage to the central part, and have deeper defects of sensitivity, the nerve fibres in NTG are more damaged in the central part of the retina and the damage is of a focal character, excavation is generally wider and deeper, furthermore patients with NTG manifest vasospasms, nocturnal systemic hypotension, decrease of ocular pulse amplitude and fluctuation of ocular perfusion pressure, constricted retinal veins and even deteriorated haemorheological properties of blood and other factors (12). In HTG the pattern electroretinogram (PERG) and the pattern visual evoked potentials (PVEP) are pathological. In NTG, PERG is virtually normal, but PVEP responses are markedly altered (12).
Central corneal thickness (CCT) is an important parameter for determining the diagnosis and subsequent observation of glaucoma pathology.
In the majority of cases, treatment of glaucoma begins with the local application of drops. Prostaglandin analogues (PGAs) are highly effective, and as a result are widely used as the drugs of first choice (19). Regardless of the hypotensive effect of these pharmaceuticals, their long-term application brings a reduction of CCT (7, 11, 15, 17, 18, 23, 24).
One of the possibilities behind the occurrence of this phenomenon is degradation of collagen through the activation of the prostaglandin E receptors in the corneal stroma (16).
In general it is stated that CCT is lower in the case of NTG in comparison with HTG. For this reason, it was the aim of our study to determine and compare CCT in both of the observed groups, also taking into account the applied medication with prostaglandin analogues.
Cohort and method
Within the framework of this study, over the course of two months we examined a total of 200 eyes of 100 patients with glaucoma who came for a follow-up examination with the framework of supervisory care. The evaluated cohort comprised 100 eyes of 50 patients (29 women and 21 men) with HTG, and 100 eyes in 50 patients (25 women and 25 men) with NTG. The average age in HTG was 67 years and in NTG 62.6 years. The exclusion criterion for this study was corneal pathology, conditions following corneal laser procedures, combined antiglaucomatous therapy, conditions following glaucoma surgery and high ametropia. The group of hypertensive glaucomas included eyes only with chronic simple primary open-angle glaucoma, in which the diagnosis was determined by a complex eye examination and in which both structural changes (ganglion cell complex and nerve fibre layer) and functional changes (perimeter) were confirmed, and the level of intraocular pressure before the application of treatment exceeded the value of 25 mmHg. Similarly, in NTG also the diagnosis was confirmed by both structural and functional changes, and was accompanied by an examination of PERG and PVEP (12). Intraocular pressure in NTG before the relevant applied therapy was lower than 15 mmHg. Medicamentous therapy with locally applied anti-glaucomatous agents, if indicated, had been used by our patients for at least the last five years.
In all eyes, CCT was measured with the aid of an ultrasound pachymeter Tomey Handy Pachymeter SP100, always by the same physician.
We classified the results of CCT determined in patients with HTG and NTG into two groups. The first group had CCT without correction and the second with correction (CCT correction) taking into account corneal thinning following the application of prostaglandins. We adjusted the correction of the CCT values after applications of prostaglandins according to the results of the studies by You and Cho (23), Lee and Cho (11) and Maruyama et al. (15). After two-year application of latanoprost on patients with NTG, You and Cho determined a reduction of CCT from 544.6 ± 38.4 to 540.3 ± 37.8 um (99.2%), while after five-year application on patients with NTG, Lee and Cho determined a reduction from 542.3 ± 36.2 to 533.7 ± 32.9 um (98.4%). Similarly, in the case of HTG also, Maruyama et al. determined a reduction of CCT following four-year and longer application from 537 ± 34 to 526 ± 32 um (98%). On the basis of these results, we used the values we measured in patients who did not take any local medication or to whom other antiglaucomatous agents than prostaglandin were applied, in order to convert the values to 99% of those measured (the average value of the aforementioned studies is 98.5%).
For the statistical processing we used a two sample t-test on a 5% level of significance.
RESULTS
The age representation in the individual sexes and their number is illustrated in table 1. Average values of CCT in table 2.
1. Characteristics of cohort: sex, average age, type of treatment 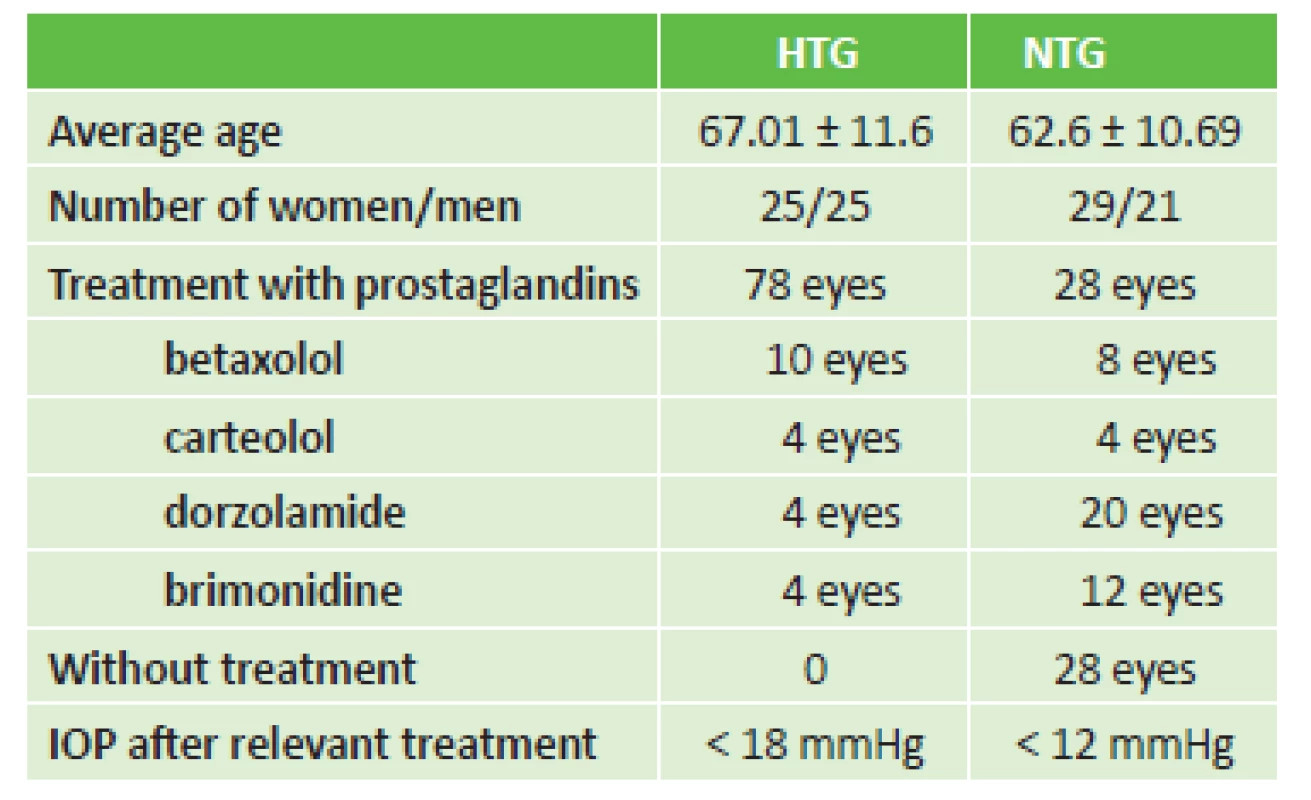
HTG – hypertensive glaucoma, NTG – normotensive glaucoma, IOP – intraocular pressure 2. Values of central corneal thickness in both groups of glaucomas 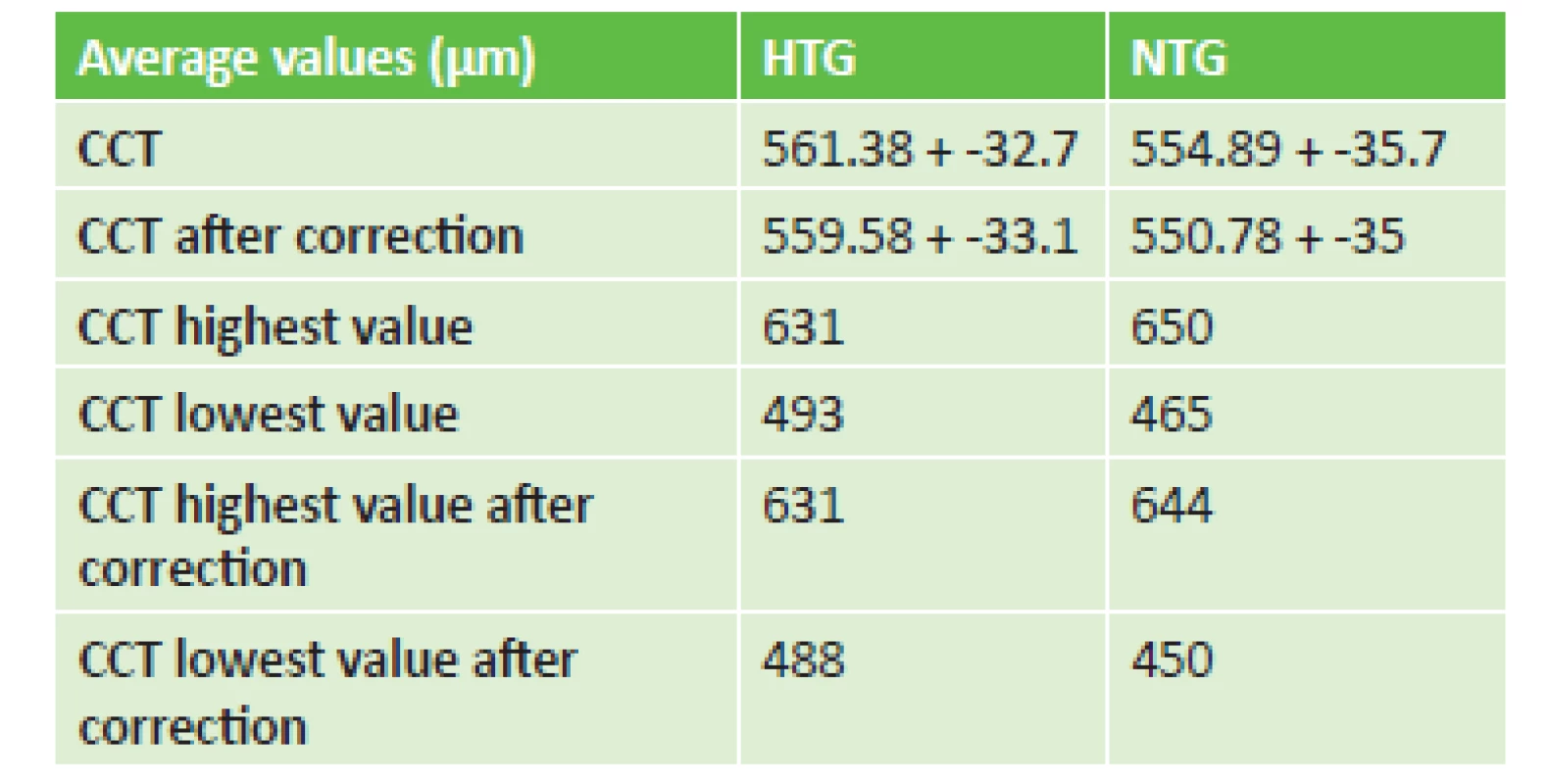
CCT – central corneal thickness, HTG – hypertensive glaucoma, NTG – normotensive glaucoma For comparison of the measured values of CCT and CCT correction in patients with HTG and NTG we used a two sample t-test and graphic illustration with the aid of Box plots (Graph 1 and 2).
1. Uncorrected values of central corneal thickness in normotensive and hypertensive glaucoma 
2. Corrected values of central corneal thickness in normotensive and hypertensive glaucoma 
The statistical evaluation demonstrated that in the case of CCT and corrected CCT the values are lower in the group of patients with NTG than in the patients with HTG. In the case of the measured CCT values in NTG 554.9 ± 35.7 as against HTG 561.4 ± 32.7, the difference upon their comparison was not statistically significant (p = 0.181). Even after the conversion of corrected CCT values, upon the comparison of NTG (550.8 ± 35) against HTG (559.6 ± 33.1), the difference was not statistically significant (p = 0.069).
This difference may be caused by the uneven representation of the patients treated with PGA in both groups.
We also did not determine any influence of age on CCT (r = -0.1446, p = 0.3165).
DISCUSSION
The first to note the influence of CCT on values of intraocular pressure were Morad et al. (16). They determined that CCT is significantly lower in the case of NTG than in HTG. The same conclusions were reached by Hornová and Sedlák (8), who state in the conclusion of their study that in NTG there are significantly lower values of CCT in comparison with HTG.
At the turn of the millennium, Copt et al. (2) attempted a reclassification of NTG or intraocular hypertension into the group of HTG. They determined that CCT in NTG has statistically significantly lower values. Similar conclusions were reached also by Shetgart and Mulimani (16). The effect of the reduction of CCT in HTG and ocular hypertension was recorded over the course of 12 months following the administration of prostaglandins also by Liehneová and Karlovská (14). Of interest for us was the study by Kim and Cho (9), who determined a reduction of CCT by the application of prostaglandins in the case of NTG. Similar conclusions were reached also by You and Cho (23), Lee and Cho (11) and Wu et al. (21). By contrast, studies by other authors did not confirm this finding (3, 10, 19, 20).
Na Wu et al. (21) determined that long-term local treatment with PGA may have a direct influence on the biomechanical properties of the cornea, together with an indirect influence on a decrease of intraocular pressure and a reduction of CCT. The authors did not demonstrate statistically significant differences of the measured biomechanical parameters of the cornea in the observed 3 groups of patients: a control group, newly diagnosed individuals with primary open-angle glaucoma and patients treated long-term with PGAs, in which the last group was further divided according to the type of PGA used (bimatoprost, latanoprost and travoprost). A small, statistically insignificant decrease in the values of CCT was determined only in the group treated with PGAs for a period of at least two years. One of the possible theories concerning the effect of PGAs is their influence on the increased density of keratocytes in the corneal stroma, perhaps due to the influence of activation of metalloproteinases and the limitation of their tissue inhibitors (1).
Also of interest is the finding of Yoo et al. (22), that following the discontinuation of latanoprost therapy in NTG, there was an increase in the CCT value over the course of two years from 531.4 to 544 µm.
The inspiration for our observation was the studies by You and Cho (23), Lee and Cho (11), who determined a long-term reduction of CCT following the application of prostaglandins in NTG, and Maruyama et al. (15) in HTG. We are aware that this study also has its limits. For the conversion we used the results of the above-stated works, because we did not have the opportunity to observe the CCT values before and after the long-term application of prostaglandins.
The short-term influence of beta-blockers on CCT was studied by Grüb et al. After four-day application of timolol maleate they determined increased values of CCT. This increase was not statistically significant (p = 0.0659) (4). In the literature we did not find a study on the long-term application of beta-blockers and their influence on CCT. For this reason, we corrected the CCT values in these eyes. Grüb et al. also determined the short-term influence of topical application (for 96 hours) of brimonidine on CCT in healthy individuals. They determined a temporary reversible increase in CCT (5). They reached similar findings also after 28-day application of 0.5% timolol (6).
Our results of the statistical evaluation of measured CCT demonstrated that in the case of CCT and CCT correction these values are lower in the group of patients with NTG than in patients with HTG. Upon a comparison of the values of CCT in NTG and HTG the difference was not statistically significant. In the case of assessment of the values of CCT correction in both types of glaucomas, the difference was greater, but was not statistically significant. This may also be an explanation for the differing results of measurement of CCT in the studies of different authors. In our cohort this difference was caused by uneven representation of patients treated with PGAs in both groups.
CONCLUSION
CCT was lower in NTG than in HTG, but this difference was not statistically significant. Upon a comparison of CCT corrected by the application of prostaglandins (CCT correction) in both types of glaucomas this difference increased, but was not statistically significant and may have been caused by the uneven representation of patients treated with PGAs in both groups. It is appropriate to count on this effect of reduction of CCT upon the application of treatment with prostaglandins.
Received: 5. 7. 2018
Accepted: 24. 10. 2018
Available on-line: 27. 3. 2019
doc. MUDr. Ján Lešták, CSc, MSc, MBA,
LLA, DBA, FEBO, FAOG
Oční klinika JL Fakulty biomedicínského inženýrství ČVUT
V Hůrkách 1296/10, 158 00 Praha 5 –
Nové Butovice
Sources
1. Bergonzi, C., Giani, A., Blini, M. et al.: Evaluation of prostaglandin analogue effects on corneal keratocyte density using scanning laser confocal microscopy. J Glaucoma, 19; 2010 : 617-621.
2. Copt, RP., Thomas, R., Mermoud, A.: Corneal thickness in ocular hypertension, primary open-angle glaucoma, and normal tension glaucoma. Arch Ophthalmol, 117; 1999 : 14-16.
3. Grise-Dulac, A., Saad, A., Abitbol, O., et al.: Assessment of corneal biomechanical properties in normal tension glaucoma and comparison with open-angle glaucoma, ocular hypertension, and normal eyes. J Glaucoma, 21; 2012 : 486-489.
4. Grüb, M., Leitritz, M., Mielke, J. et al.: Effect of timolol on central corneal thickness and endothelial cell density. Klin Monbl Augenheilkd. 223; 2006 : 894-898.
5. Grüb M., Mielke, J., Schlote ,T., Rohrbach, M.: Effect of brimonidine on central corneal thickness. Klin Monbl Augenheilkd. 229; 2012 : 236-240.
6. Grüb, M., Rohrbach, J.M.: Effect of timolol on central corneal thickness. Eur J Ophthalmol. 23; 2013 : 784-788.
7. Harasymowycz, P.J., Papamatheakis, D.G., Ennis, M. et al.: Realtionship between travoprost and central corneal thickness in ocular hypertension and open-angle glaucoma. Cornea, 26; 2007 : 34-41.
8. Hornová, J., Sedlák, P.: Pachymetrie u pacientů s glaukomem. Cesk Slov Oftalmol, 55; 1999 : 212-215.
9. Kim, HJ., Cho, BJ.: Long-term effect of latanoprost on central corneal thickness in normal tension glaucoma. J Ocul Pharmacol Ther, 27; 2011 : 73-76.
10. Lee, JW., Wong, RL., Chan, JC. et al.: Differences in corneal parameters between normal tension glaucoma and primary open-angle glaucoma. Int Ophthalmol, 35; 2015 : 67-72.
11. Lee, H., Cho, BJ.: Long-term effect of latanoprost on central corneal thickness in normal-tension glaucoma: five-year follow-up results. J Ocul Pharmacol Ther, 31; 2015 : 152-155.
12. Lestak, J., Nutterova, E., Pitrova, S. et al.: High Tension Versus Normal Tension Glaucoma. A Comparison of Structural and Functional Examinations. J Clinic Experiment Ophthalmol, 2012; 5.
13. Lešták, J., Pitrová, Š.: „Ganglion cells komplex“ a vrstva nervových vláken u hypertenzních a normotenzních glaukomů. Cesk Slov Oftalmol, 72; 2016 : 199-203.
14. Liehneová, I., Karlovská, S.: Medikamentozní léčba glaukomu a biomechanické vlastnosti rohovky. Cesk Slov Oftalmol, 70; 2014 : 167-176.
15. Maruyama, Y., Mori, K, Ikeda, Y. et al.: Effects of long-term topical prostaglandin therapy on central corneal thickness. J. Ocul. Pharmacol.Ther 30; 2014 : 440-444.
16. Morad, Y., Sharon, E., Hefetz, L. et al.: Corneal thickness and curvature in normal-tension glaucoma. Am J Ophthalmol, 125; 1998 : 164-168.
15. Sen, E., Nalcacioglu, P., Ikeda, Y., et al.: Effects of long-term topical prostaglandin therapy on central corneal thiskness. J Glaucoma, 17; 2008 : 398-405.
16. Shetgar, AC., Mulimani, MB.: The central corneal thickness in normal tension glaucoma, primary open angle glaucoma and ocular hypertension. J Clin Diagn Res, 7; 2013 : 1063-1067.
17. Schiote, T., Tzamalis, A., Kynigopoulos, M.: Central corneal thickness during treatment with travoprost 0,004% in glaucoma patients. J. Ocul. Pharmacol.Ther 25; 2009 : 459-462.
18. Stefan, C., Dumitrica, D.M., Tebeanu, E., et al.: Prostaglandin analogues and central corneal thickness. Oftalmologia, 51;2007 : 96-99.
19. Ventura, AC., Böhnke, M., Mojon, DS.: Central corneal thickness measurements in patients with normal tension glaucoma, primary open angle glaucoma, pseudoexfoliation glaucoma, or ocular hypertension. Br J Ophthalmol, 85; 2001 : 792-795.
20. Wu, LL., Suzuki, Y., Ideta, R.: Central corneal thickness of normal tension glaucoma patients in Japan. Jpn J Ophthalmol, 44; 2000 : 643-647.
21. Wu, N., Chen, Y., Yu, X., et al.: Changes in corneal biomechanical properties after long-term topical prostaglandin therapy. PLoS One, 17; 2016 : 11(5) :e0155527.
22. Yoo, R., Choi, YA., Cho, BJ.: Change in central corneal thickness after the discontinuation of latanoprost in normal tension glaucoma-change in central corneal thickness after stop of latanoprost. J Ocul Pharmacol Ther, 33; 2017 : 57-61.
23. You, JY., Cho, BJ.: Effect of latanoprost on central corneal thickness in unilateral normal-tension glaucoma. J Ocul Pharmacol Ther, 29; 2013 : 335-338.
24. Zhong, Y., Shen, X., Yu, J., Cheng, Y.: The comparison of the effects of latanoprost, travoprost, and bimatoprost on the central corbeal thickness. Cornea, 30; 2011 : 861-864.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 5-
All articles in this issue
- Ocular Manifestations of Granulomatosis with Polyangiitis
- Yield of Display Modules of Corneal Tomography for Early Diagnosis of Corneal Ectasia
- Changes of Central Corneal Thickness in Normotensive and Hypertensive Glaucoma
- Pilot Results of Implantation of the New Hydrophobic Intraocular Lens Zeiss LUCIA 611P in the Czech Republic
- Merkel Cell Carcinoma of the Eyelids (Clinical-Histological Study)
- Pachychoroid Disease of the Macula – Case Report
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ocular Manifestations of Granulomatosis with Polyangiitis
- Merkel Cell Carcinoma of the Eyelids (Clinical-Histological Study)
- Pachychoroid Disease of the Macula – Case Report
- Pilot Results of Implantation of the New Hydrophobic Intraocular Lens Zeiss LUCIA 611P in the Czech Republic
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

