-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Causes of death and heart pathology in pacemaker or implantable cardioverter-def ibrillator patients who died in hospital
Příčiny smrti a nálezy na srdci u pacientů s kardiostimulátorem nebo implantabilním kardioverterem-defibrilátorem zemřelých v nemocnici
Cílem bylo analyzovat příčiny smrti a pitevní nálezy na srdci u zemřelých s implantabilními kardiostimulátory a implantabilními kardiovertery-defibrilátory (PM a ICD), se kterými se setkávají jak soudní lékař tak patolog. Klinické a sekční nálezy byly analyzovány u 83 zemřelých s PM a 14-ti s ICD. V souboru byla většina mužů. Ve skupině s PM 49 mužů a 34 žen, s ICD 11 mužů a 3 ženy. Muži byli mladší v obou skupinách (76±10 vs. 82±6 roků s PM, 64±9 vs. 68±10 roků s ICD). Zemřelí s ICD byli mladší než s PM (65±9 vs. 78±9 roků). Interval od primoimplantace přístroje do smrti byl u PM 4.0±3.0 roky, u ICD 2.8±2.5 roku. Základní příčina smrti byla kardiovaskulární u 86,7% zemřelých s PM a 71.4% s ICD, což je více než v běžné české (51,1%) a evropské (35,5%) populaci. Ischemická choroba srdeční byla přítomna u 97,6% pacientů s PM a 85,7% s ICD a její závažné důsledky (jizvy, chronická aneurysmata, stenty) byly nalezeny častěji u zemřelých s ICD. Dilatační kardiomyopatie byla potvrzena u 4,8% zemřelých s PM a 28,6% s ICD. Sklerotické (28,9%) a revmatické (7,2%) změny chlopní byly přítomny jen u v průměru starších zemřelých s PM. Bezprostřední příčina smrti byla kardiální (srdeční selhání, infarkt myokardu) u 51,8% zemřelých s PM a 64,2% s ICD. Nekardiální příčiny (embolie, bronchopneumonie, sepse) byly rovněž časté, což může spoluvysvětlovat relativně krátký interval primoimplantace přístroje - úmrtí.
Klíčová slova:
kardiostimulátor – implantaiblní kardioverter-defibrilátor – příčiny úmrtí – nálezy na srdci – pitva
Authors: Petr Dvořák 1; Miroslav Novák 2; Pavel Kamarýt 2; Bronislava Slaná 1; Jolana Lipoldová 2; Pavel Dvořák 3; Karel Veselý 1
Authors place of work: 1st Department of Pathology, Faculty Hospital St Anne's and Masaryk University, , Pekarska St., 656 91 Brno, Czech Republic. 1; 1st Department of Internal Medicine - Cardioangiology and International ClinicalResearch Center, St. Anne‘s University Hospital Brno 2; Department of Physical Electronics, Faculty of Science, Masaryk University, 2, Kotlarska St, 602 00 Brno, Czech Republic. 3; Pekarska St., 656 91 Brno, Czech Republic. 53
Published in the journal: Soud Lék., 59, 2014, No. 4, p. 55-58
Category: Původní práce
Summary
83 pacemaker (PM)/14 implantable cardioverter-defibrillator (ICD) autopsied patients, predominantly males, deceased 4.0±3.0/2.8±2.5 years after implantation in hospital. Coronary artery disease was most frequent. Its consequences were more severe in ICD patients. Sclerotic and rheumatic heart changes were present in older PM patients group only. The immediate cause of death was mostly of cardiac etiology. Relatively short implant-death interval should be explained by rather great part of non-cardiac causes of death in hospitalised patients.
Keywords:
pacemakers – implantable cardioverter – defibrillators-causes of death – heart pathology – autopsy
Implantable pacemakers (PM) have been used for the treatment of bradycardia for more than 50 years and implantable cardioverter-defibrillators (ICD) for the treatment of tachyarrhythmias for more than 30 years. Cardiac resynchronisation therapy by means of biventricular pacing (with or without ICD) has been used in patients (pts) with congestive heart failure in the last 25 years. Indications for implantation of these devices have been established (1-6). The therapy with PM and ICD decreases all-cause mortality, sudden cardiac death and death from congestive heart failure (5-8). Causes of death in PM and ICD recipients are mostly cardiovascular (9-10). Complications following implantation and during follow-up in PM and ICD pts have been described repeatedly (5,6,11,12). Patients with implanted devices represent relatively great and increasing part of population. They die (sometimes suddenly) at home or in the hospital and are autopsied in the departments of both forensic medicine and pathology.
In our earlier publications we described intracardiac findings near PM and ICD leads and electrodes (13) and histological findings around these electrodes (14) in a group of pts on whom a specially focused autopsy was performed. In this study, we present causes of death and pathological findings in hearts for all PM and ICD pts autopsied within a limited period in our department of pathology.
Methods
Between February 2005 and September 2008, autopsies were performed on 97 deceased pts with implanted PMs or ICDs. The devices were implanted in several hospitals. Following the clinical and autopsy examinations the gender, age and first implantation-to-death interval were evaluated and the underlying causes of death, significant diseases, cardiac and extracardiac findings and immediate causes of death were analysed. The PM and ICD pts were compared.
The Student´s t-test was used to compare the age of the pts and the first implantation-to-death interval whereas the binomial distribution test was used to compare the gender occurrence and frequency of various diagnoses and findings in pts with PM vs. ICD. The findings in 2 pts with biventricular PM and 2 pts with biventricular ICD were not evaluated separately because of the limited number.
Results
Autopsy was performed on 83 PM and 14 ICD pts.
Gender and age were analysed. Males outnumbered females, 49 vs. 34 in PM pts (p=0.1, NS) and 11 vs. 3 in ICD pts (p=0.03). Average age was 78±9 (45-95) years in PM pts and 65±9 (48-81) years in ICD pts (p=0.000001). Males were younger in both groups: in PM pts 76±10 (45-95) years in males vs. 82±6 (70-92) years in females, (p=0.004) and in ICD pts 64±9 (48-81) years in males vs. 68±10 (62-79) years in females, (p=0.46, NS).
The interval between first implantation and death (established for 65 PM and in all 14 ICD pts) was 4.0±3.0 (0.08-12.6) years in PM pts and 2.8±2.5 (0.08-8.3) years in ICD pts (p=0.17, NS).
The PMs comprised ventricular VVI (53), dual-chamber VDD (8), dual-chamber DDD (21) and biventricular (2) devices while the ICDs were single-chamber VVI (9), dual-chamber DDD (3) and biventricular (2) devices. All of the atrial and most of the ventricular leads were bipolar. The underlying cause of death was mostly general atherosclerosis with its cardiac, cerebral and other complications in 69 (83.1 %) PM pts vs. 7 (50 %) ICD pts. Other circulatory diseases were found in 3 (3.6 %) PM vs. 3 (21.4 %) ICD pts. Non-circulatory causes of death were present in 11 (13.2 %) PM vs. 4 (28.5 %) ICD pts (tab. 1).
Tab. 1. Underlying causes of death. 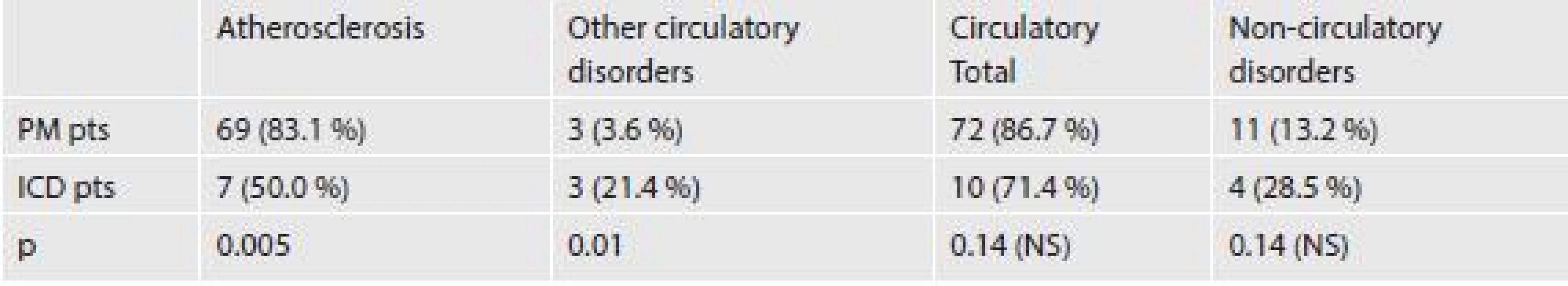
However the pts were mostly polymorbid with underlying cause of death and one or several other significant diseases. The general atherosclerosis with coronary artery disease was the most frequent: 81 (97.6 %) in PM pts vs. 12 (85.7 %) in ICD pts (tab. 2). Hypertension was present in 58 (69.9 %) vs. 8 (57.1 %) pts (p=0.34, NS).
As regards heart pathology, the frequent changes are summarised in tab. 2-4.
Tab. 2. Coronary artery disease related changes and revascularization. 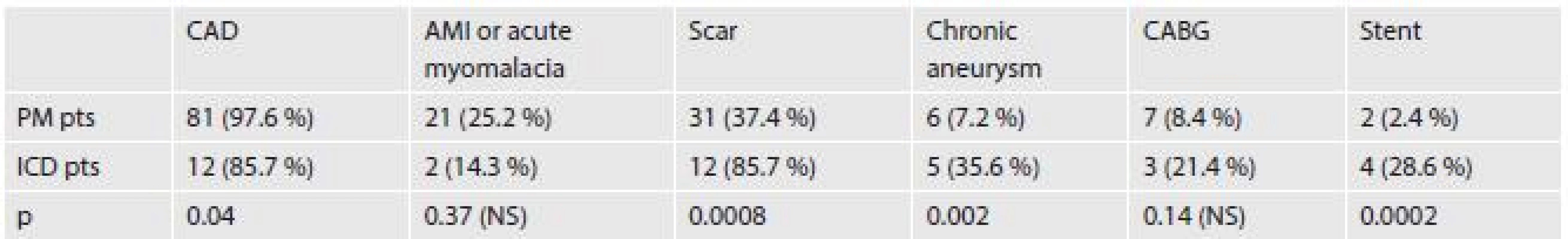
CAD – coronary artery disease, AMI – acute myocardial infarction, CABG – coronary artery bypass grafting. Tab. 3. Other myocardial changes. 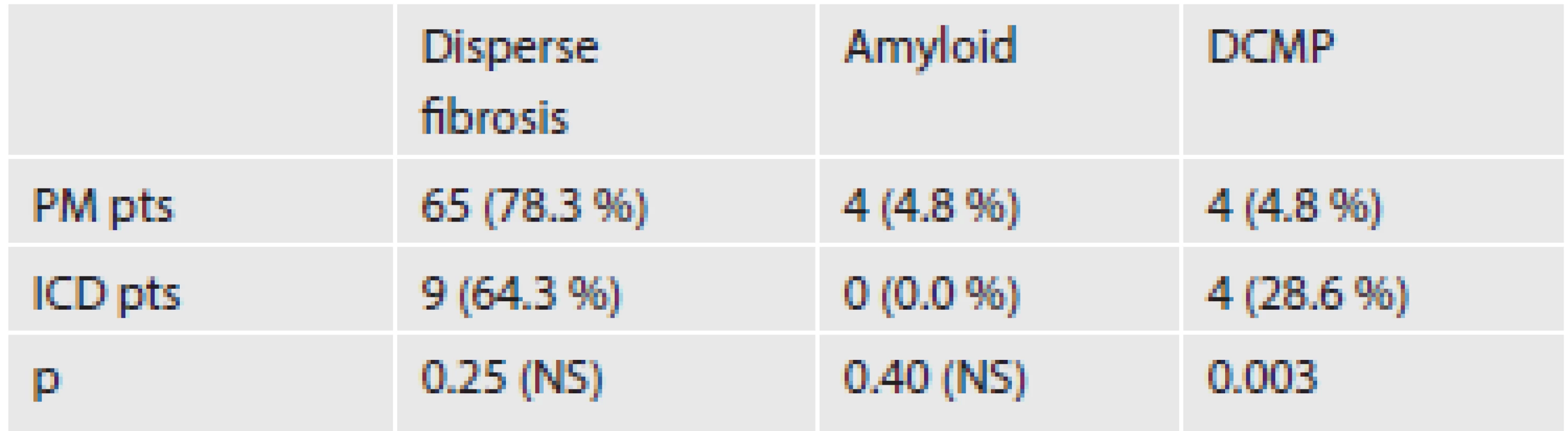
DCMP – dilated cardiomyopathy Tab. 4. Endocardial and valvular changes. 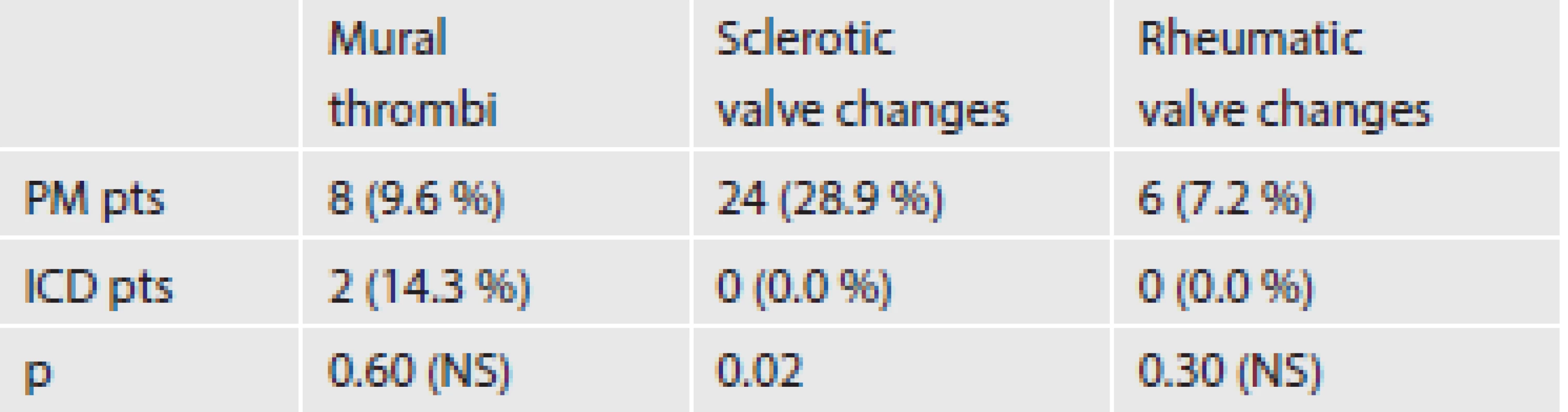
The following findings in the myocardium were compared in PM vs. ICD pts.
Coronary artery disease related changes were acute myocardial infarction and acute myomalacia in 21 (25.2 %) vs.2 (14.3 %) pts, scar in 31 (37.4 %) vs. 12 (85.7 %) pts, out of which with chronic aneurysm in 6 (7.2 %) vs. 5 (35.6 %) pts. Evidence of aorto-coronary bypass was found in 7 (8.4 %) vs. 3 (21.4 %) pts and coronary stent implantation in 2 (2.4 %) vs. 4 pts (28.6 %) pts (tab. 2).
Disperse multiple fibrosis was present in 65 (78.3) PM vs. 9 (64.3 %) ICD pts, amyloid 4 (4.8 %) vs. 0 (0 %) pts, primary dilated cardiomyopathy 4 (4.8 %) vs. 4 (28.6 %) pts (tab. 3). Interesting exceptional findings were: purulent myocarditis 3 vs. 0 (in one case there was abscess close to the electrode tip) and metastasis of lung adenocarcinoma into the wall of the right atrium 1 vs. 0.
In the endocardium, thrombus was found in 8 (9.6 %) PM vs. 2 (14.3 %) ICD pts. (tab. 4). Thrombi and connective tissue encapsulations were frequent on leads and electrodes, as described in our earlier publications (13,14).
The valves exhibited sclerotic and rheumatic changes in PM pts only. The sclerotic changes were present in 24 (28.9 %) PM vs. 0 (0 %) ICD pts. Annular sclerosis of mitral valve was present in 17 and sclerotic calcification of aortic valve in 19 PM pts. In 12 out of these PM pts both valves were affected. The rheumatic valve disease was found in 6 (7.2 %) vs. 0 (0 %) pts (tab. 4).
Other valvular findings were exceptional: acute bacterial endocarditis of the sclerotic aortic valve 1 vs. 0, thrombotic endocarditis of the mitral valve 1 vs. 0. One PM patient had a papillary fibroelastoma of the aortic valve. Two PM and one ICD patients were treated by valvular surgery.
In 2 PM pts radiofrequency ablation was performed.
The most frequent change in the heart size was hypertrophy and dilatation of both ventricles in 35 (42.2 %) PM vs. 10 (71.4 %) ICD pts (p=0.04) or of the left ventricle alone in 22 (25.5 %) vs. 3 (21.4 %) pts (p=0.69, NS).
The immediate cause of death (tab. 5) was cardiac etiology in 43 (51.8 %) PM and 9 (64.2 %) ICD pts. It included heart failure in 35 (42.2 %) PM vs. 9 (64.2%) ICD pts and acute myocardial infarction in 8 (9.6 %) vs. 0 (0 %) pts.
Tab. 5. Immediate cause of death. 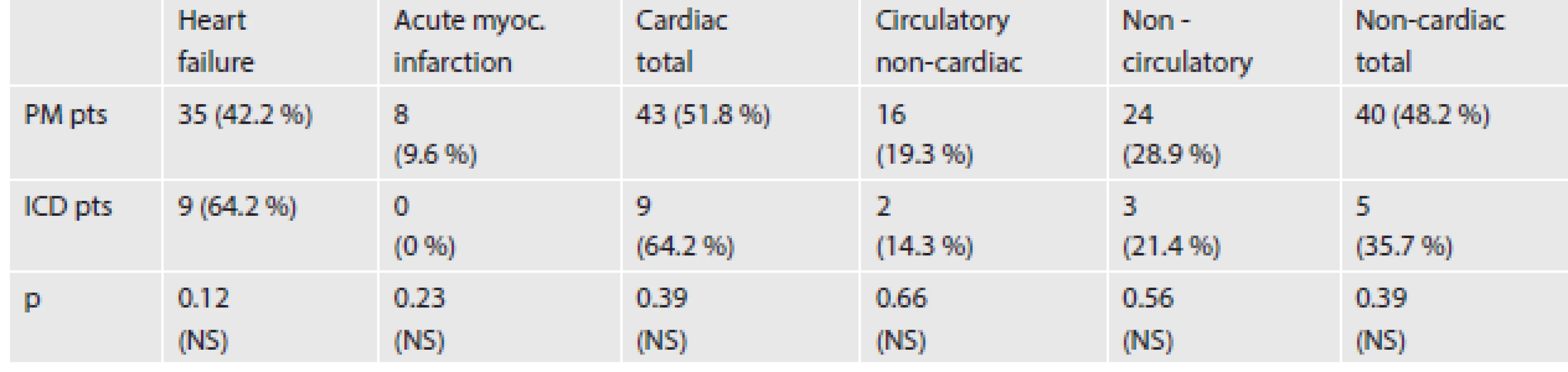
The circulatory non-cardiac cause was present in 16 (19.3 %) PM vs. 2 (14.3 %) ICD pts. A relatively frequent non-cardiac circulatory immediate cause of death was massive pulmonary embolism in 8 (9.6 %) PM vs. 1 (7.1 %) ICD pts (p=0.77, NS). Other non-cardiac circulatory disorders were exceptional: encephalomalacia 4 vs. 0, brain haemorrhage 1 vs. 1, thrombosis or embolism of arteria mesenterica superior 2 vs. 0, ruptured aneurysm of abdominal aorta 1 vs. 0.
Non-circulatory disorders, 24 (28.9 %) PM vs. 3 (21.4 %) ICD pts, included bronchopneumonia in 15 (18.1 %) PM vs. 0 (0 %) ICD pts (p=0.08, NS), sepsis 5 (6.0 %) vs. 1 (7.1 %) pts (p=0.87, NS) and other exceptional causes 4 (4.8 %) vs. 2 (14.3 %) pts (p=0.17, NS).
Three males and one female with biventricular devices (2 PM and 2 ICD) were evaluated in this study. There were 3 pts with the diagnosis of primary dilated cardiomyopathy and one with coronary artery disease, median age 56.8 (48-62) years. In all the hearts examined hypertrophy and dilatation of both ventricles were present. Three pts died from heart failure and in one the immediate cause of death was the rupture of cerebral arterial aneurysm.
Discussion
The number of patients with implanted PM/ICD devices increases continually. These patients die at home or in the hospital, some of them suddenly. Autopsy of persons who die unexpectably at home represents great part of autopsies at departments of forensic medicine. Knowledge of the pathological findings in these persons is therefore important for both forensic medicine physicians and pathologists.
In gender analysis the number of males outnumbered females in this study (significantly only in ICD pts), which is similar to the Kim (9), Duray (10), Sindler (15), and Mase (16) publications, and the Henyan meta-analysis (17). According to this meta-analysis, females, unlike their male counterparts, did not benefit so much from ICD therapy in the primary prevention of all-cause mortality. One potential explanation for this feature is the lower incidence of ventricular dysrhythmias in women.
As regards to the age in our study, ICD pts were younger than PM pts, similar to the Sepsi personal communication. This may be due to the fact that pacemakers are also used in very old and polymorbid pts while in ICD implantation more contraindications are applied.
In our group of pts who died in hospital the interval between the first implantation and death was relatively short, 4.0±3.0 years for PM and 2.8±2.5years for ICD pts. The survival of pts with implanted devices will probably be longer and incidence of sudden death will be higher in pts who died out of hospital. The pts involved in this study were often admitted to hospital due to a non-cardiac condition and the cause of death was frequently of non-cardiac etiology (see below).
In the Sepsi personal communication of PM and ICD pts who died and were autopsied in hospital or died at home and were autopsied in the department of forensic medicine, the implantation-to-death intervals were similar to those in our population (PM VVI 4.0, PM DDD 4.3, ICD VVI 3.7 and ICD DDD 1.9 years). Five-year survival in the MUSTT Study (ICD pts) was 76 % (4). In the Durray study (10) 822 non-selected ICD pts were followed for 43±30 months, during which 222 pts (27.4 %) died. A comparison of the above-mentioned studies is difficult due to the different criteria for patient inclusion and on the mode of evaluation.
The implantation-to-death interval was non-significantly shorter in ICD vs PM pts, similar to the Sepsi personal communication. ICD implantation is often indicated in pts with more severe heart damage.
The underlying cause of death was more often circulatory in our pts (86.7 % in PM and 71.4 % in ICD pts) in comparison with Czech general population 51.1 % (19) and European general population 35.5 % (20) apparently because all pts with implants suffer from cardiac disease.
As regards to the heart pathology the most frequent finding was coronary atherosclerosis with its consequences. The more frequent occurrence of coronary atherosclerosis in PM vs. ICD pts may be explained by the higher age of the PM pts. The consequences of coronary atherosclerosis were more serious in ICD pts. We found a frequent occurrence of scars, chronic aneurysm, aorto-coronary by-pass graftings and coronary stent implantations. Malignant arrhythmias or risk of malignant arrhythmias and therefore indication of ICD implantation is higher in such damaged hearts.
Primary dilative cardiomyopathy was more frequent in ICD vs. PM pts.
Sclerotic valve changes were frequent mostly in old PM pts and not present in relatively young ICD pts. Rheumatic valve changes not so frequent in the last decades were also present in PM pts only. Our results demonstrate increasing the importance of sclerotic valve changes in comparison with rheumatic changes.
In three pts bacterial purulent myocarditis was found, in one case in relation with PM electrode similarly as in Lysenkova study (11). Kim described two cases in which the ICD system required explantation for infection (9). Baman described risk factors for mortality in pts with cardiac device-related infection (18).
The pts were mostly old and polymorbid in this study. Two or more pathological processes affected the heart in many cases. Coronary atherosclerosis, hypertension, valve changes and cardiomyopathies influenced the heart, often in combination. Some features such as hypertrophy, dilatation or dispersed fibrosis may have been the consequence of several pathological processes.
The immediate cause of death was mostly of cardiac etiology and heart failure was the most frequent reason in our study just as in the other publications (9-10). But in relatively great part of hospitalized and autopsied pts the immediate cause of death was of non-cardiac etiology (pulmonary embolism, bronchopneumonia, sepsis etc). It was in 48.2 % PM pts in our study vs. 33.7 % PM VVI and 39.8 % PM DDD pts in Sepsi´s communication (these PM pts died in hospital and were autopsied in department of pathology or died at home and were autopsied in the department of forensic medicine). In ICD pts there were 35.7 % non-cardiac causes of death in our study of hospitalized and autopsied pts vs. 17.6 % in the Kim study (9) and 31.0 % in the Duray study (10) of all implanted ICD pts. It is necessary to bear this difference in mind during examination and therapy in urgently admitted PM/ICD pts.
Conclusions
In PM/ICD pts who died in hospital, males outnumbered females, males were younger than females, and ICD pts were younger than PM pts, similar to other studies. Younger age of the ICD pts may be explained by the fact that pacemakers are used almost without contraindications also in old polymorbid pts while in ICD implantation more contraindications are applied.
The interval between implantation and death was relatively short. The survival of pts with implanted devices will probably be longer in pts who died out of hospitals.
The underlying cause of death was more often circulatory in comparison with general population, coronary atherosclerosis with its consequences was the most frequent cardiac finding. The more frequent occurrence of coronary atherosclerosis in PM vs. ICD pts may be explained by the higher age of the PM pts. The consequences of coronary atherosclerosis were more serious in ICD pts (such as occurrence of scars, chronic aneurysm, aorto-coronary by-pass graftings and coronary stents) because the risk of malignant arrhythmias and indications of ICD implantation are higher in such damaged hearts. Dilative cardiomyopathy was more frequent in ICD pts. Sclerotic and rheumatic valve changes were present in older group of PM pts only. Two or more pathological processes affected the heart in many cases. The immediate cause of death was mostly cardiac etiology, and heart failure was the most frequent cause in our study, similar to other publications. But PM/ICD pts often die in hospital also due to a non-cardiac condition, and the immediate cause of death is frequently of non-cardiac etiology (pulmonary embolism, bronchopneumonia, sepsis, etc). It is necessary to bear this difference in mind during examination and therapy in urgently admitted PM/ICD pts. Both forensic medicine physicians and pathologists must be familiar with findings in PM/ICD implanted patients.
A comparison of studies evaluating the causes of death in PM/ICD pts is difficult, depending on different criteria chosen for assessment and on the mode of evaluation.
Limitations
The limitation of this study arises from the fact that all the PM and ICD pts investigated died in hospital. The findings in pts who died out of hospital could be different.
Another limitation of the study is the relatively low number of ICD and, in particular, cardiac resynchronisation therapy pts (with biventricular pacing).
Unfortunately, the clinical data and ECG findings before death coming from several hospitals did not allow us to establish the diagnosis of sudden cardiac death in this study.
FUNDING
Supported by European Regional Development Fund - Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123)
✉ Correspondence address:
MUDr. Petr Dvořák, CSc.
1st Department of Pathology
Faculty Hospital St Ann and Masaryk University
Pekarska 53, 656 91 Brno, Czech Republic
tel: +420736786005
e-mail: olped@centrum.cz
Zdroje
1. Táborský M, Kautzner J, Bytešník J, et al. Zásady pro implantace kardiostimulátorů, implantabilních kardioverterů-defibrilátorů a systémů pro srdeční resynchronizační léčbu 2009. Cor Vasa 2009; 51(9): 602-614.
2. Vardas PE, Auricchio A, Blanc J, et al. Guidelines for Cardiac Pacing and Cardiac Resynchronization Therapy. European Heart Journal 2007; 28 : 2256–2295.
3. Epstein, Andrew E. An update on Implantable Cardioverter-defibrillator Guidelines. Current Opinion in Cardiology 2004; 19(1): 23-25.
4. Rosanio S, Scharz ER, Vitarelli A, et al. Sudden Death Prophylaxis in Heart Failure. Int J Cardiol 2007; 119 : 291-296.
5. Chapa DW, Lee HJ, Kao CHW, et al. Reducing Mortality with Device Therapy in Heart Failure Patients without Ventricular Arrhythmias. Am J Crit Care 2008; 17(5): 443-452.
6. Trappe HJ, Gummert J. Current Pacemaker and Defibrillator Therapy. Dtsch Arztebl Int 2011; 108(21): 372-380.
7. Bradley DJ, Bradley EA, Baughman KL et al. Cardiac Resynchronization and Death from Progressive Heart Failure (A Meta-analysis of Randomized Controlled Trials). JAMA 2003; 289(6): 730-740.
8. Cleland JGF, Daubert JC, Erdmann E et al. On behalf of The CARE-HF Study Investigators. Longer-term Effects of Cardiac Resynchronization Therapy on Mortality in Heart Failure [the CArdiac REsynchronization-Heart Failure (CARE-HF) Trial Extension Phase]. Eur Heart J 2006; 27 : 1928-1932.
9. Kim SG, Roth JA, Fisher JD et al. Long-Term Outcomes and Modes of Deah of Patients Treated With Nonthoracotomy Implantable Defibrillators. Am J Cardiol 1995; 75 : 1229-1232.
10. Duray ZG, Schmitt J, Richter S, Israel CW, Hohnloser SH. Arrhythmic Death in Implantable Cardioverter Defibrillator Patients: A Long-Term Study Over a 10 Year Implantation Period. Europace 2009; 11(11): 1462-1468.
11. Lysenková A. Typy patomorfologických změn na srdci způsobených kardiostimulační elektrodou. Soud Lek 1980; 16/25 : 39-43.
12. Wilson GJ. The Pathology of Cardiac Pacing. In: Silver: Cardiovascular Pathology. New York; Churchill Livingstrone Inc; 1991 : 1429-1464.
13. Novak M, Dvorak P, Kamaryt P, Slana B, Lipoldova J. Autopsy and Clinical Context in Deceased Patients with Implanted Pacemakers and Defibrillators: Intracardiac Findings Near the Leads and Electrodes. Europace 2009; 11 : 1510-1516.
14. Dvorak P, Novak M, Kamaryt P, Slana B, Lipoldova J, Dvorak P jr. Histological Findings aroud Electrodes in Pacemaker and Implantable Cardioverter-defibrillator Patients: Comparison of Steroid-eluting and Non-steroid-eluting Electrodes. Europace 2012; 14 : 117-123.
15. Šindler M, Sepši M, Krajsa J. et al. Postmortální analýza souboru nemocných léčených implantabilními přístroji – uspořádání studie. Soud Lek 2006; 51 : 16-19.
16. Mase H, Tamura K, Hiromoto A et al. Histopathological Study of Tissue Reaction to Pacemaker Electrodes Implanted in the Endocardium. J Nippon Med Sch 2005; 72 : 52-59.
17. Henyan NN, White CM, Gillespie EL, Smith K, Coleman CI, Kluger J. The impact of gender on survival amongst Patients with Implantable Cardioverter Defibrillators for Primary Prevention against Sudden Cardiac Death. Jounal of Internal Medicine 2006; 260 : 467-473.
18. Baman TS, Gupa SK, Valle JA, Yamada E. Risk Factors for Mortality in Patients with Cardiac Device-Related Infection. Circ Arrhythmia Electrophysiol 2009; 2 : 129-134.
19. Nejčastější příčiny smrti v ČR. http://www.demografie.info
20. Causes of death statistics. http://epp.eurostat.ec.europa.eu/statistics_explained/index.php/Causes_of_death_statistics
Štítky
Patologie Soudní lékařství Toxikologie
Článek vyšel v časopiseSoudní lékařství

2014 Číslo 4-
Všechny články tohoto čísla
- Pathomorphology of inflammatory response following traumatic brain injury, serum values of interleukins, and gene polymorphisms
- NÁZORY A ÚVAHY SOUDNÍHO LÉKAŘE
- Ethanol-induced ketoacidosis as a possible neglected cause of sudden death in chronic alcohol consumers
- 4. Česko-Slovenský sjezd soudního lékařství
- Possibilities of molecular genetic determination of age of an individual from biological traces
- Causes of death and heart pathology in pacemaker or implantable cardioverter-def ibrillator patients who died in hospital
- 92. Jahrestagung der Deutschen Gesellschaft für Rechtsmedizin
- Medzinárodná konferencia
- Soudní lékařství
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Causes of death and heart pathology in pacemaker or implantable cardioverter-def ibrillator patients who died in hospital
- Ethanol-induced ketoacidosis as a possible neglected cause of sudden death in chronic alcohol consumers
- Possibilities of molecular genetic determination of age of an individual from biological traces
- NÁZORY A ÚVAHY SOUDNÍHO LÉKAŘE
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



