-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Rational operation of MRI equipment in university hospitals in the Czech Republic
The use of the MRI systems in healthcare facilities is expanding based on the following observations:
1) patients are not exposed to ionizing radiation during MRI examinations (as opposed to computed tomography [CT]) and 2) the imaging options available are greater with the use of the MRI than with the x-ray or CT. Due to the high acquisition and operating costs of an MRI system, it is necessary to pay special attention to the economic components of MRI use. The following recommendations are provided for the rational use of MRI systems in University Hospitals, and are based on data originating from one hospital in particular. A detailed analysis of the economics involved with operating an MRI system was made, and through this analysis parameters were formulated which describe the financial side of MRI operation. This research was done in the context of the reimbursement mechanism of the Czech Republic, and contains the calculations and a complete costs and break-even points for each MRI examination. The results are developed models for the reimbursement of an MRI in the Czech Republic, and particular recommendations for the rational use of an MRI in faculty hospital-type facilities.Keywords:
operation of MRI, management of medical equipment, management of university hospitals, rational operation
Authors: Ilya Ivlev; Lucie Korábová; Jakub Vacek; Peter Kneppo
Authors place of work: Kladno, Czech Republic ; Department of Biomedical Technology, Czech Technical University in Prague
Published in the journal: Lékař a technika - Clinician and Technology No. 1, 2014, 44, 19-25
Category: Původní práce
Summary
The use of the MRI systems in healthcare facilities is expanding based on the following observations:
1) patients are not exposed to ionizing radiation during MRI examinations (as opposed to computed tomography [CT]) and 2) the imaging options available are greater with the use of the MRI than with the x-ray or CT. Due to the high acquisition and operating costs of an MRI system, it is necessary to pay special attention to the economic components of MRI use. The following recommendations are provided for the rational use of MRI systems in University Hospitals, and are based on data originating from one hospital in particular. A detailed analysis of the economics involved with operating an MRI system was made, and through this analysis parameters were formulated which describe the financial side of MRI operation. This research was done in the context of the reimbursement mechanism of the Czech Republic, and contains the calculations and a complete costs and break-even points for each MRI examination. The results are developed models for the reimbursement of an MRI in the Czech Republic, and particular recommendations for the rational use of an MRI in faculty hospital-type facilities.Keywords:
operation of MRI, management of medical equipment, management of university hospitals, rational operationIntroduction
In this article, the authors recommend the rational way of operating MRI imaging systems, especially for healthcare establishment such as faculty hospitals. It is important to focus on the cost structure of the operation and identify the most important influencing factors and parameters. To understand the functioning of the entire system in more detail, it is necessary to realize the overall concept of the Czech Republic healthcare services and the position of radiology in this system. The data from 2011 are used in the analysis of the economy of MRI imaging systems and calculation of costs for negotiated services. The break-even analysis shows the amount of services necessary to balance costs and revenues.
Methods
Classification of costs is the necessary first step for determining the share of contributions of individual cost items to the creation of added value, and for calculating the prices of related healthcare services (1).
As the objective of this calculation is a determination of prices, the detailed price calculations must be based on in-depth cost analyses (2). The calculation methods (3), including all components of direct and indirect costs or variable and fixed costs (according to the methods used), are known as total cost calculations (4). Our analysis was based on the partial costs calculation (5, 6), which comes from the available methods best satisfying the selected criteria (3, 7). The resulting prices will be compared with the prices of services, and a break-even analysis (8) will be performed.
The Model (Pilot) Healthcare Establishment
As the model (pilot) healthcare establishment, the faculty hospital was selected, which belongs to the largest healthcare establishment in the Czech Republic1. Annually, more than 40,000 patients are hospitalized in more than 20 clinics, and approximately 40 % of them undergo surgery. Moreover, this hospital has more than half a million outpatients, performs surgeries of “super specialized” levels and uses modern diagnostic technologies.
The radiological clinic covers the complete spectrum of radiological activities for diagnostics and therapeutic preventive care. It closely cooperates with other hospital clinics and offers the use of the state-of-the-art diagnostic devices (e.g. two MRI imaging systems and CT equipment). In 2011, the clinic realized more than 10,000 magnetic resonance examinations.
Operation of MRI devices in the healthcare establishment
The workloads of the two MRI devices in the model healthcare establishment differ: the workload of one of them is 100 % and it has practically no free capacity in a two-shift operation, and the extent of utilization of the second one is 75 % as its two shifts are not completely covered and it is not in full operation during the weekends. The model healthcare establishment has negotiated capacity with health instance companies for 1 ½ MRI devices, even if it operates two such devices. The workload of the second device is limited by two factors. First, full time operation over two shifts is not possible and it would not be paid for by the insurance companies, and second, this device serves as a reserve. If the availability for hospitalized patients is lower than necessary, it must be possible to open an additional shift in order to prevent prolonged waiting times for examinations. Table 1 summarizes the data for 2011.
Tab. 1. Summary table of total costs and revenues of MRI in 2011 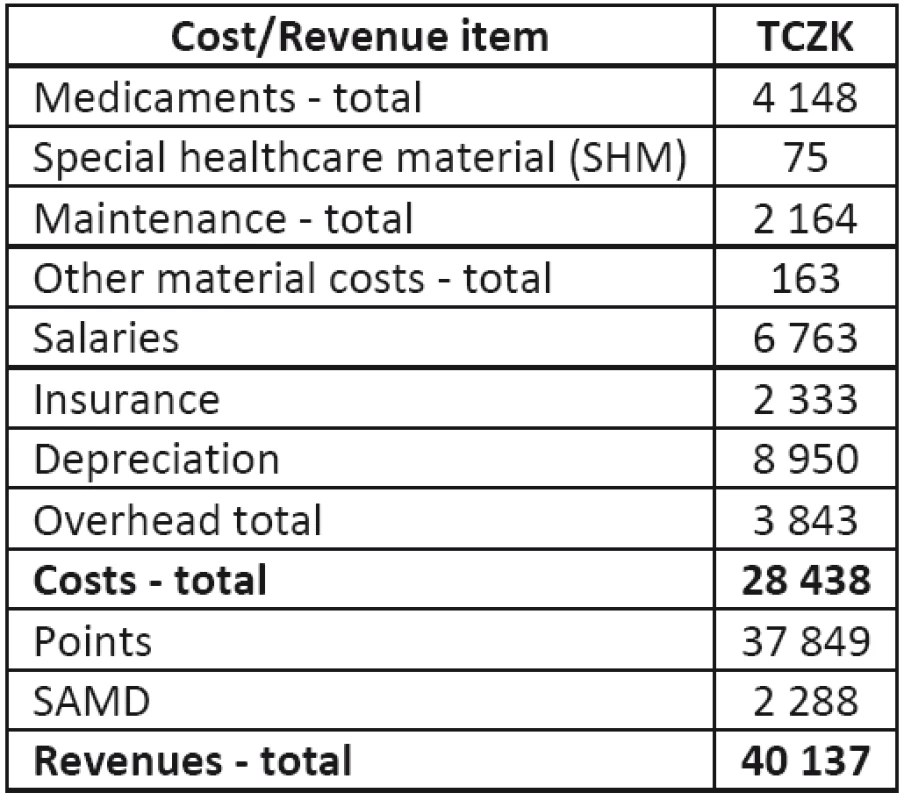
Revenues from MRI operation
The revenues from the MRI operation are summarized in Table 2. If the healthcare establishment reports a medicament as separately accounted medicaments (SAMD) to the health insurance company, the insurance company pays costs in addition to the cost of an operation, and this item therefore appears in both costs (medicaments) and revenues (MRI operation). Separately accounted material (SAMT) does not occur with the MRI. Item “points” include points for performed operations from insurance companies, private patients, foreigners and clinical studies. The total number of points (approximately 54,070,000) was converted to CZK by using the unit price of 0.70 CZK/point, in compliance with regulatory directives.
Tab. 2. Revenues from MRI operation 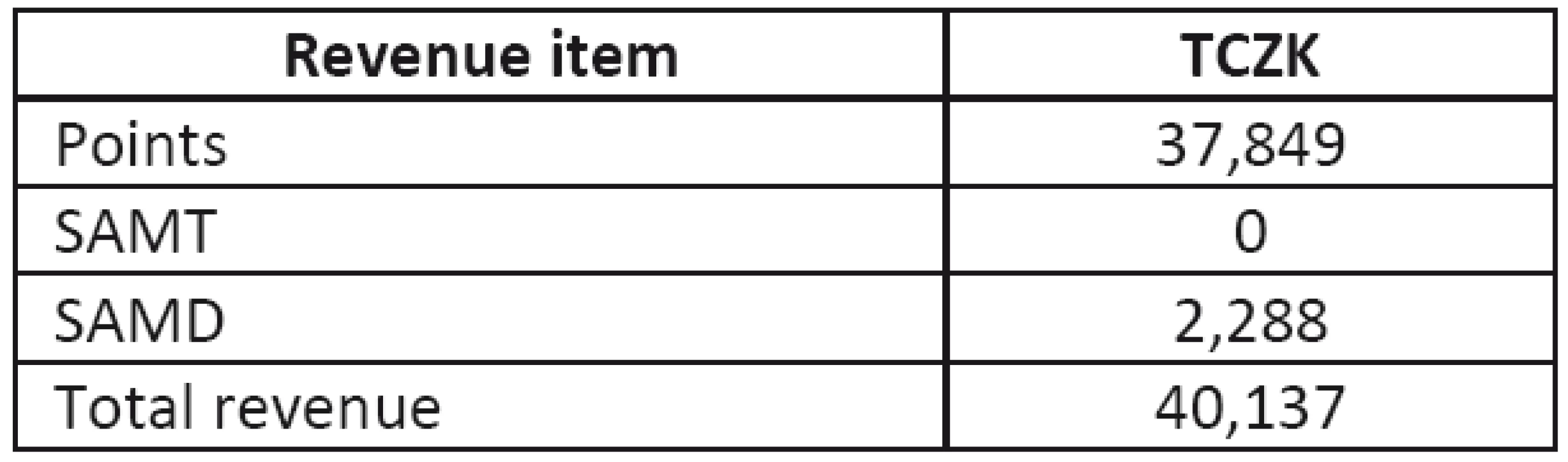
Table 3 shows that the highest cost items are salaries and depreciation due to the high purchase cost of MRI devices (Table 4).
Tab. 3. Costs of MRI operation 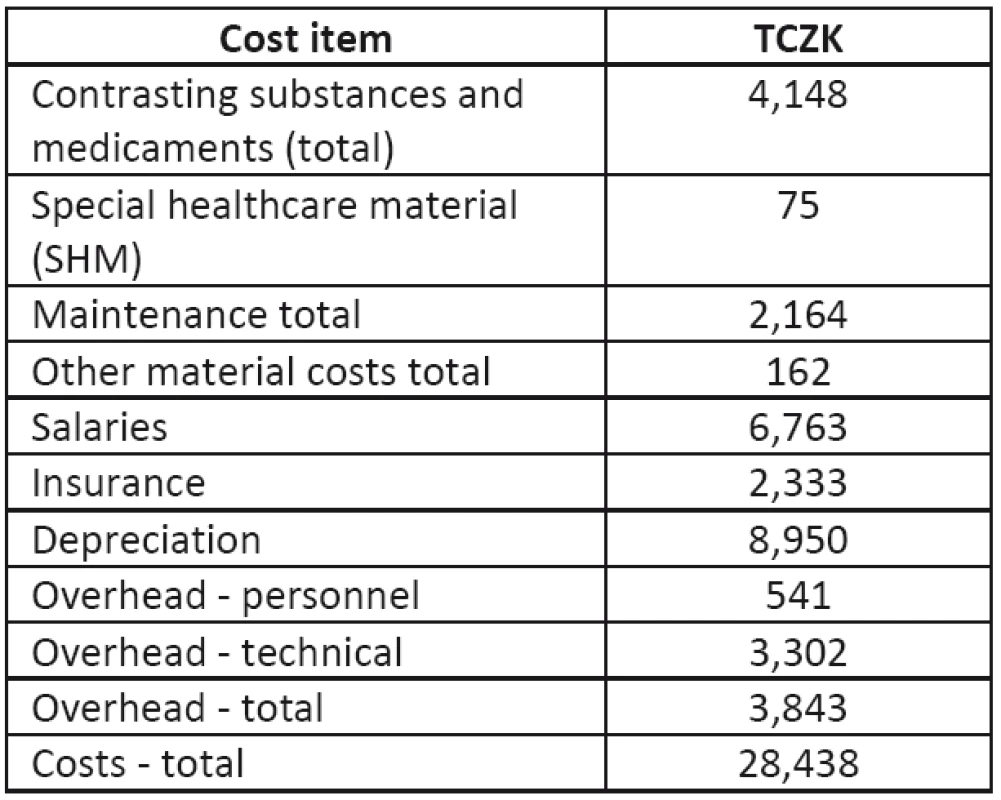
Tab. 4. Depreciation of MRI devices 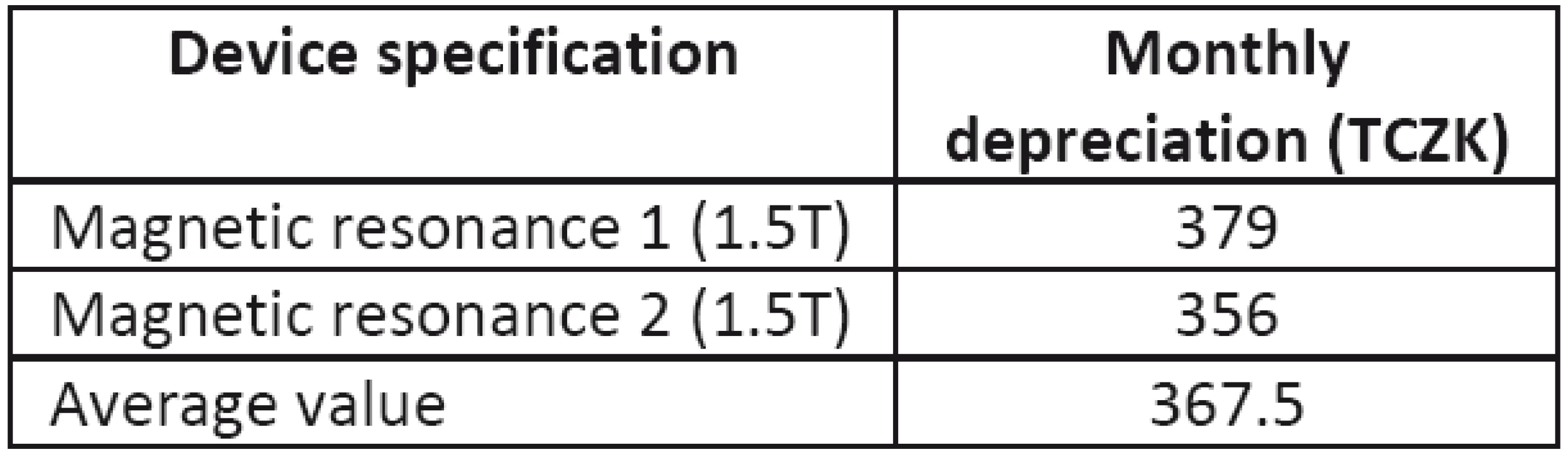
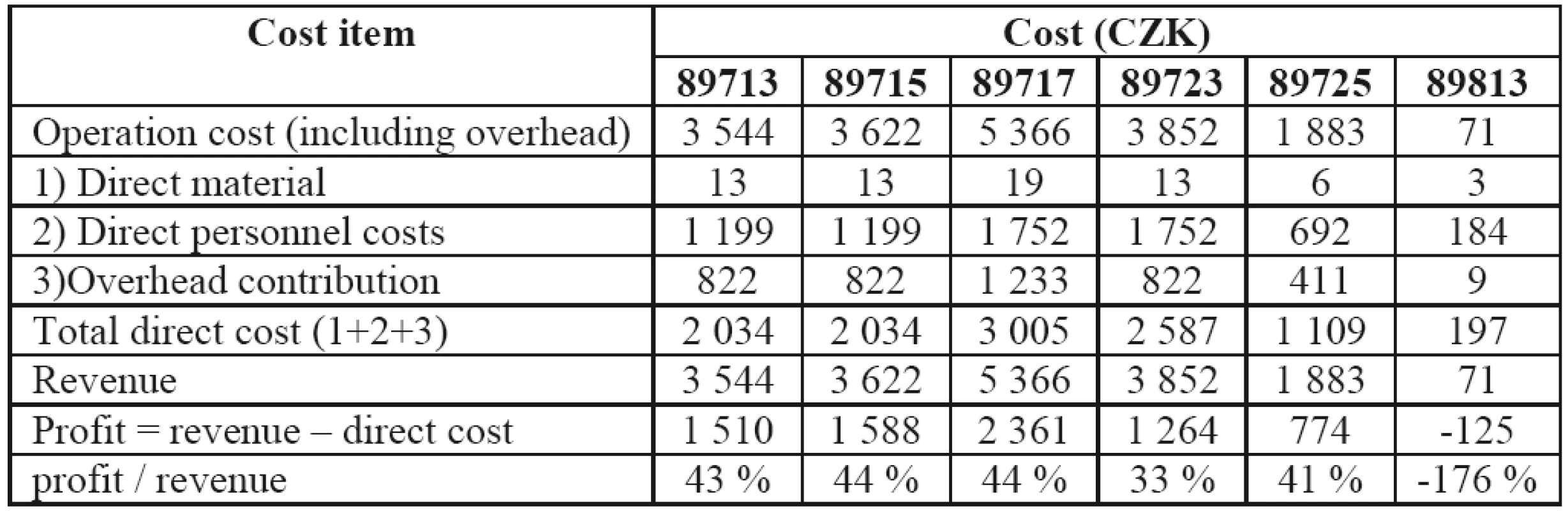
Calculation of incomplete (partial) costs
In 2011, the healthcare establishment contracted with the insurance companies for 6 basic types of operations using magnetic resonance (89713 – MRI of head, limb, joint, one section of the spine [C, TH, or L]; 89715 – MRI of neck, chest, abdomen, and pelvis (including breast); 89717 – heart MRI; 89723 - MRI angiography; 89725 – repeated or complementary MRI; 89813 – consultation with physician-radiologist). A list of the descriptions of these operations and some of their characteristics from the recording lists, and list of operations are presented in Tables 5 and 6.
Tab. 5. Revenues and points per operation 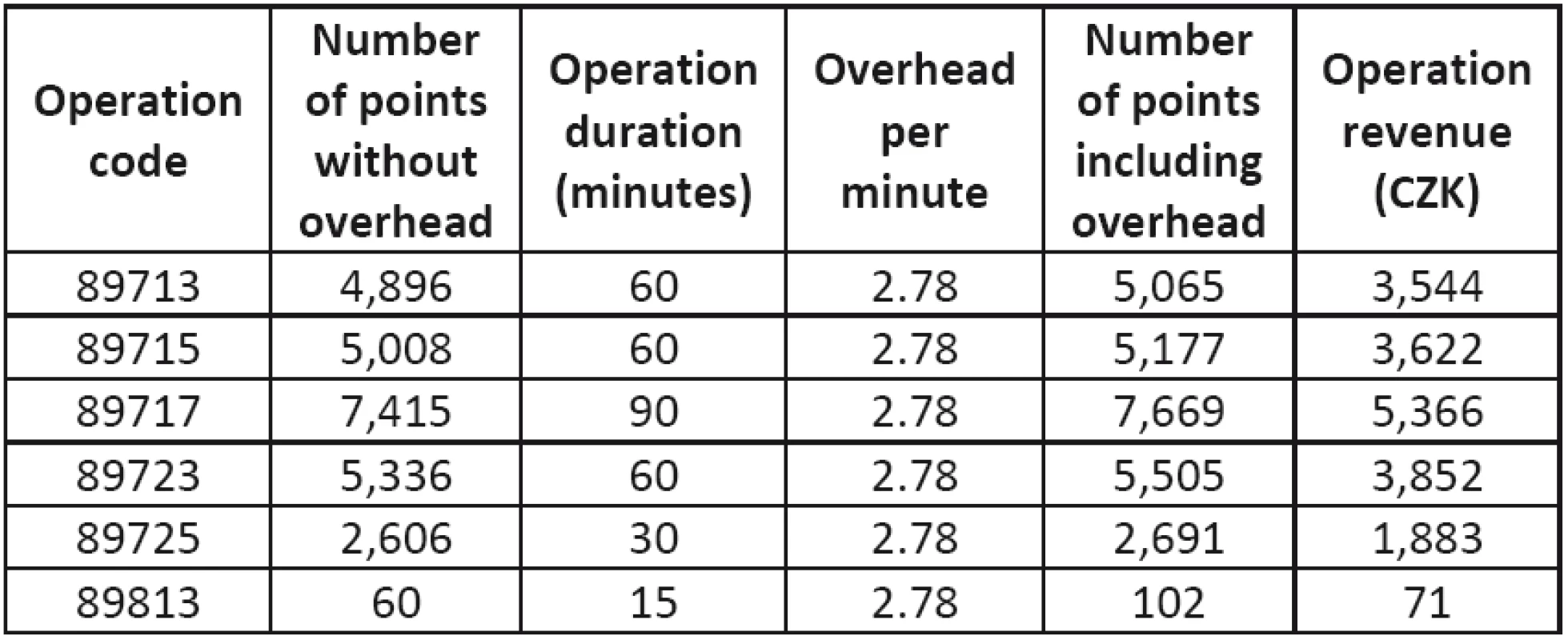
Tab. 6. Personnel costs of operations 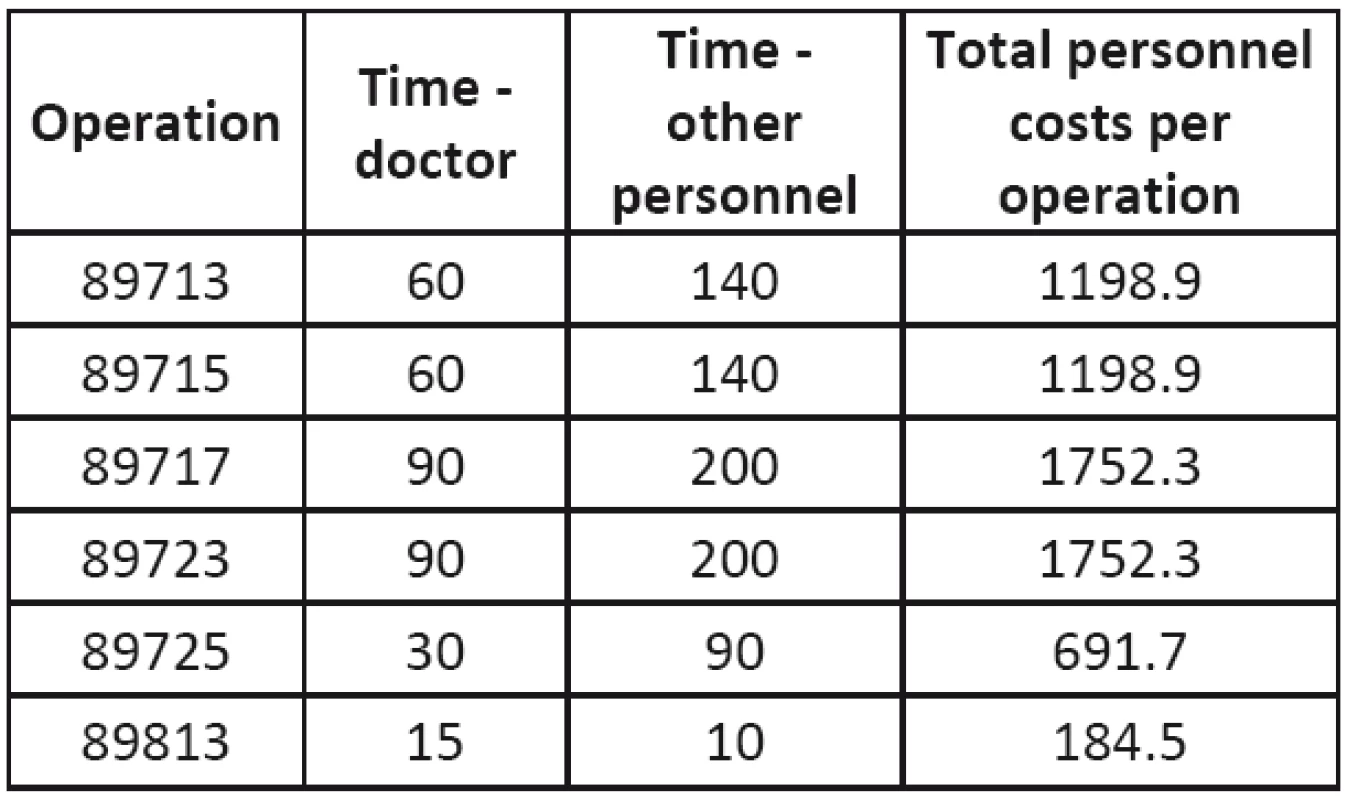
The revenue from an operation was determined as the sum of two point values: points per operation (from the list of operations) and indirect revenue (product of operation time and overhead rate per minute). The sum of the points is converted to CZK using the unit price of 0.70 CZK/point in compliance with the regulatory directives.
Table 6 lists the personnel costs of operations and Table 7 lists the costs of the contrasting substances. These values are used for the calculation of incomplete (partial) costs. Individual item costs are determined per one minute of operation or one operation (for contrasting substances).
Tab. 7. Personnel costs of operations 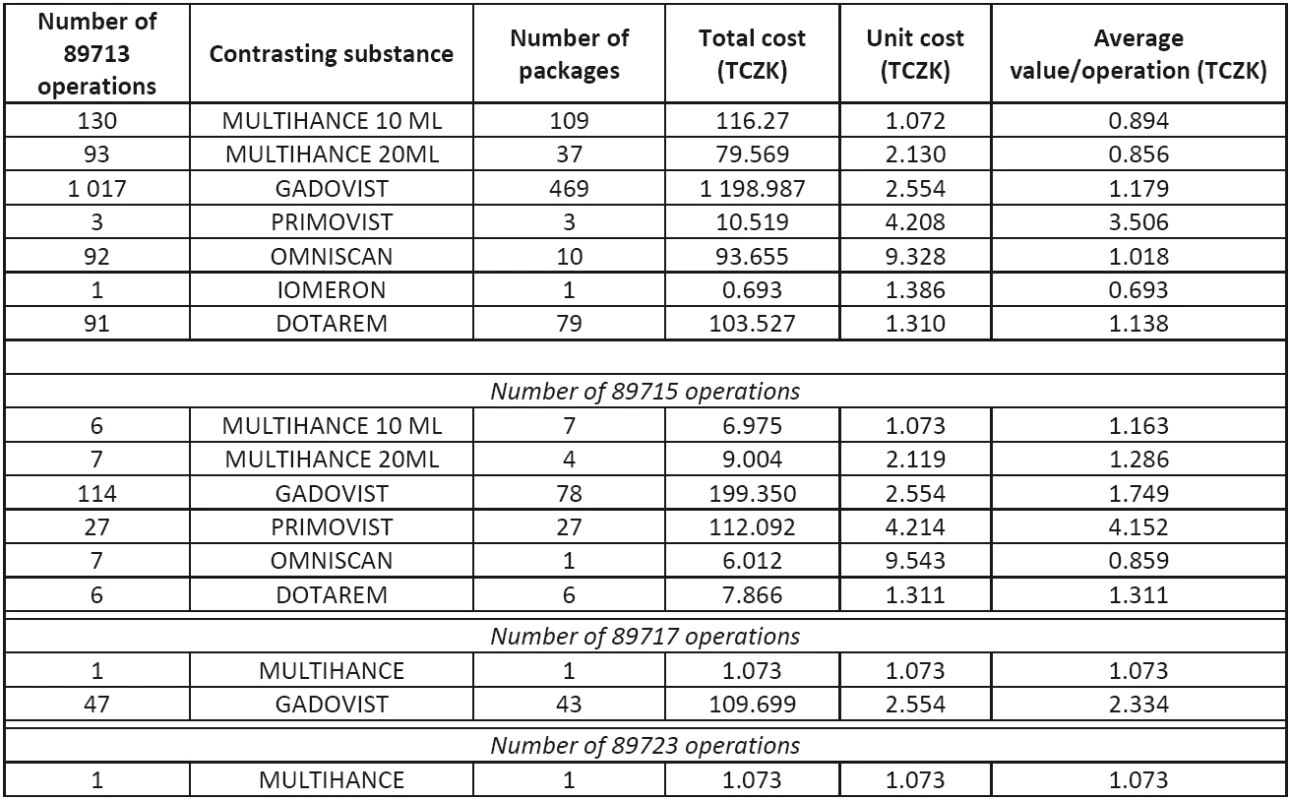
Direct personnel costs are determined as a product of the one-minute personnel cost of those participating in the operation and the operation duration. In each operation a doctor participates with a one minute rate of 9.20 CZK and supporting staff participates with a one minute rate of 4.60 CZK.
Direct material costs
The direct material consumed in an operation consists of the contrasting substances and special medical materials (SMM). The contrasting substance is applied only in the first four operation types. In Table 7, the most frequently used contrasting substance in a specific operation type is emphasized in bold. The average cost of the most frequently used substance (average value/operation) is then used for the following calculations.
It is assumed that the device is in operation for 365 days a year in two shifts (16 hours). The annual cost of SMM is 75 thousand CZK, i.e. approximately 0.20 CZK per minute. The total direct material costs are given in Table 8.
Tab. 8. Total direct material costs for individual operations 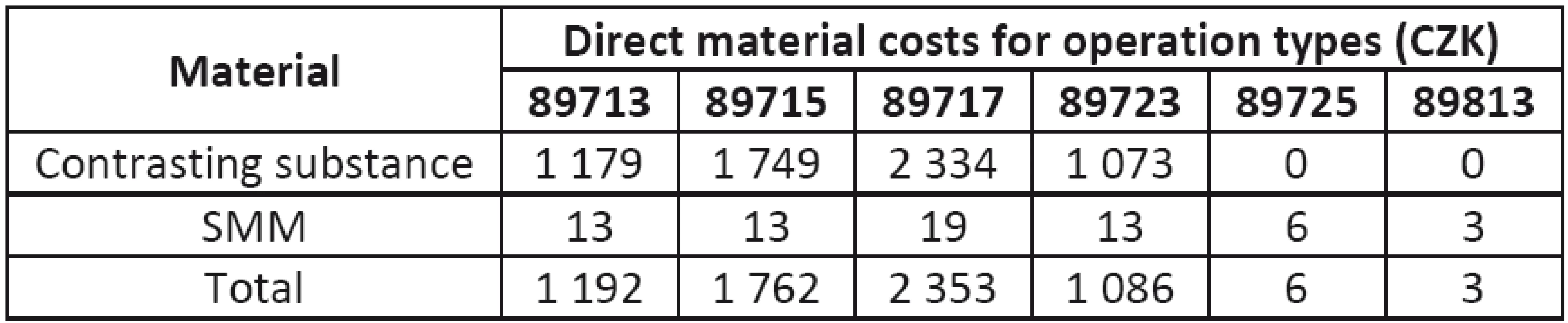
Tab. 9. Descriptions of figures and tables are of the same style. Do not center the description! 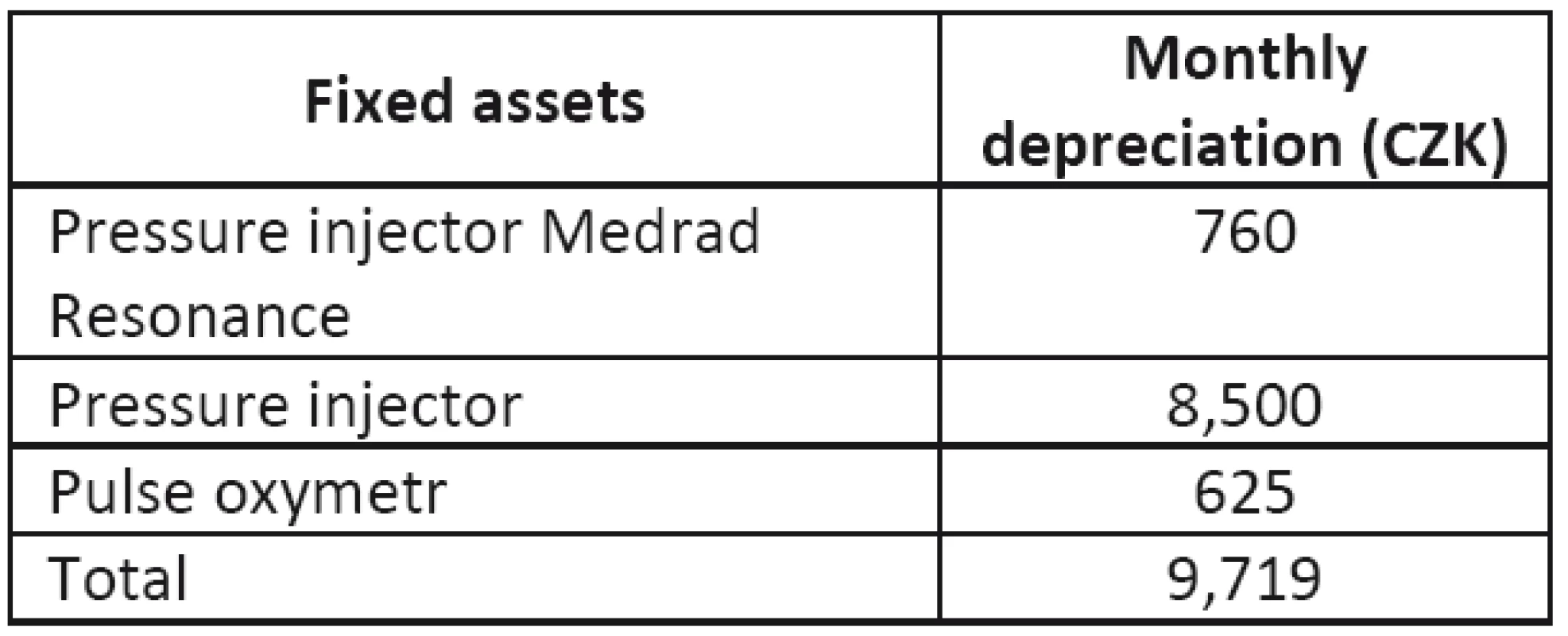
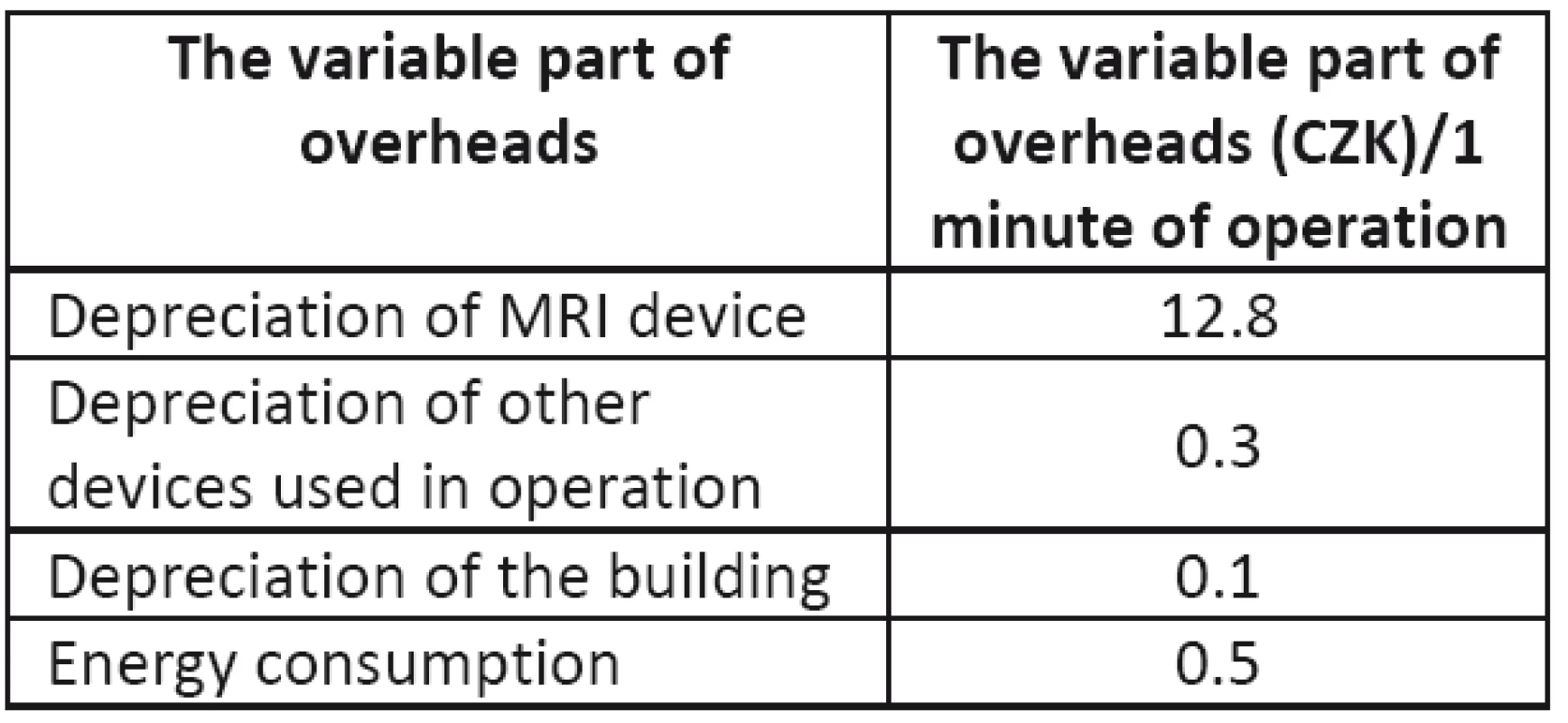
The depreciation of the MRI devices was determined in Table 4 as the average value for both of them, and some of the equipment used in the operations has already been depreciated, therefore, there are no costs for their depreciation.
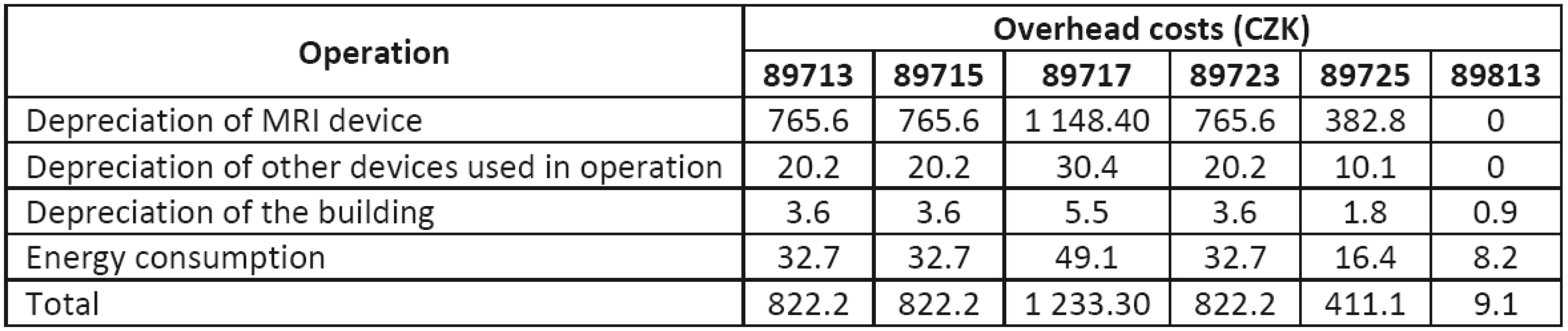
Among them are the air-conditioning unit, non-magnetic trolley, console Magic View, etc. The depreciation of the pressure injector (that is still depreciating) is approximately 8,500 CZK/month. The corresponding overhead costs for individual operation types are given in Table 11.
The depreciation of the MRI device and other equipment cannot be allocated to operation type 89813, as it is only a consultation of findings with a radiologist.
Determination of break-even point for individual examinations.
Table 13 presents the results of the break-even analysis. Break-even is defined as the point at which the cost equals the revenue, and it means that from this point on the operation is profitable (9, 10).
Tab. 13. Break-even points for individual operations 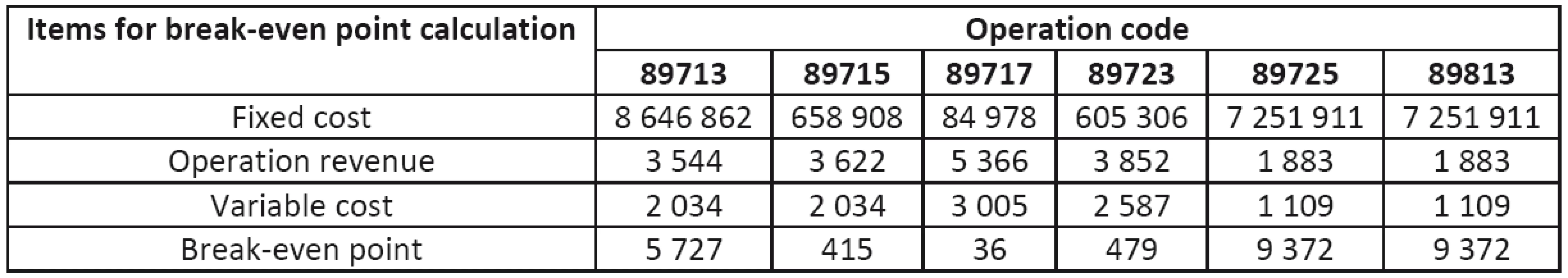
The fixed cost of individual operations was determined for each operation as the share of the total fixed cost corresponding to the share of the number of specific operations to the total number of operations performed in 2011. The total fixed cost includes personnel costs (9,096 TCZK), depreciation (4,475 TCZK) and overhead.
Conclusions and Recommendations for Rational Operation of MRI Devices
On the basis of the 2011 data, it can be concluded that the operation of MRI devices is profitable. With 13,500 examinations and 21,011 in total revenues, they profit at more than 1.4 times higher than the corresponding costs. The highest components of the cost are depreciation, personnel costs and medicaments. The purchase prices of MRI devices are high (34 to 45 million CZK), resulting in a high depreciation (31 % of the total costs), and saving depreciation costs is not possible.
The third highest cost component was the cost of contrasting substances. Their purchase price was 4,148 TCZK, while the amount obtained in this instance was only 2,288, indicating that the difference between the cost and revenue is more than 2 million CZK. The price of the other medicaments used in the examinations is negligible in relation to the contrasting substances (approximately 0.5 %) and cannot significantly contribute to such a loss. The cause of this difference was found in the reporting of the consumption of the contrasting substance: the hospital purchased the complete package of the substance, however only a part of it (e.g. half) is really used in the examination, and the rest is disposed of. The hospital then reports to the health insurance only the amount used in the examination, and the unused amount is not paid for. It is therefore recommended that the entire amount be reported to the health insurance company since the entire package is being consumed and the rest of the contrasting substance cannot be used for another patient. This approach should be combined with decisions about the types of contrast substance packaging. It can also be recommended that increased attention be paid to the delivery of the contrasting substance to the patient before the examination. The correct insertion of the winged infusion set reduces the loss of contrasting substance which can be caused by improper manipulation.
Currently, faculty-type hospitals often operate two or more MRI devices (usually one of them is older, and the second is purchased either as an upgrade or for additional capacity). If these devices are mutually interchangeable, the contracts with insurance companies cover only the actually used capacity; therefore, these imaging systems should be fully utilized, especially in the case of long waiting times. The contracts should cover the full costs of all devices, which require the hiring of new employees, and therefore an increase in personnel costs. On the other hand, the revenues would also increase (by 25 % in the investigated case).
An analysis of the cost structure can lead to the increased efficiency of MRI operation, and assist in decisions about which examinations (and to what extent) should be performed.
Tab. 14. Break-even points for individual operations 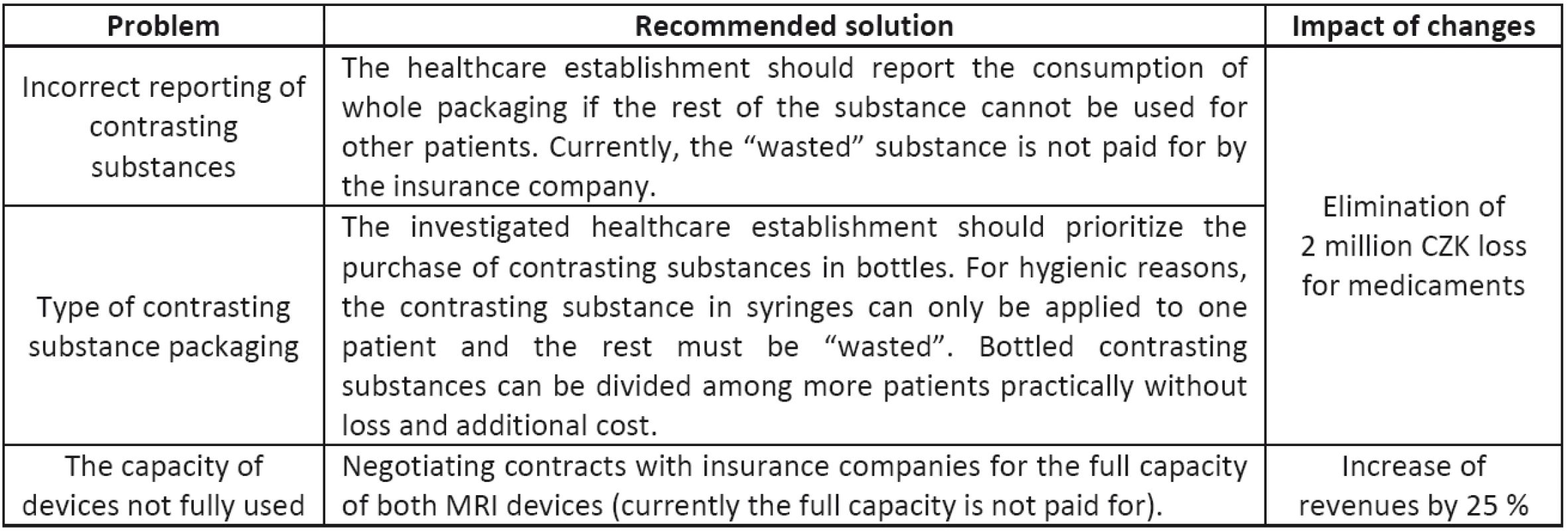
It is important to determine how each individual operation contributes to the costs and revenues, and if the contribution is determined to be negative, then even variable costs are not covered. If it is zero, the revenues should equal the costs, however there is no contribution for covering the fixed costs. Ideally, the contribution should be positive. In our case, the contributions of all types of operations (except 89813) were positive, and since the share of 89813 operations is rather low (51 times less than 89713, and 43 times less than 89725), this small negative contribution is more than compensated for by operations of other types. The contributions of operations of 89717 and 89715 are the highest and should have the largest share among all operations.
Conclusion
With payments of 0.70 CZK per point, the profit margin of MRI devices is nearly 50 % and is one of the highest in the public healthcare insurance system. The cost items of MRI operations, namely the three highest (personnel costs, depreciation and costs of medicaments), and possibilities of their decrease were investigated, and it was found that the only item for which the costs could be influenced, is the medicaments.
The parameters highly influencing the MRI economy are those related to the reimbursement mechanism, in particular the allocation of points per operation and price per point. These influence the revenues, and if they are changed a profitable activity can turn into a losing one. Constant and unpredictable changes in these mechanisms and parameters make long-term planning impossible.
The recommendations for rational operation are focused mainly on a change in reporting the consumption of contrasting substances. It is recommended that the hospital report the consumption of the entire package if the extra must be wasted. It is also recommended that the hospital purchase bottled contrasting substances instead of syringes. The last recommendation relates to negotiating contracts with the insurance companies to cover the full capacity of both MRI devices, and increase their operation time by 25 %. These cost calculations should be integrated into the managerial decision-making processes.
Acknowledgement
The work has been supported by research grants from the Ministry of Health of the Czech Republic IGA No. NT/11532-5 “Medical technology assessment”.
[1] The healthcare establishment prefers to remain confidential. The data used in this paper are based on the annual report.
Ilya Ivlev
Department of Biomedical Technology
Faculty of Biomedical Engineering
Czech Technical University in Prague
nám. Sítná 3105, CZ-272 01 Kladno
E-mail: ilya.ivlev@fbmi.cvut.cz
Phone: +420 774 984 735
Zdroje
[1] Zlámal, J., Bellová, J. Ekonomika zdravotnictví. Brno: Nconzo, 2005. str. 206. ISBN 80-7013-429-1.
[2] Gladkij, I. Management ve zdravotnictví. Brno: Computer Press, 2003. p. 380. ISBN 80-7226-996-8.
[3] Macík K. Kalkulace a rozpočetnictví. Vyd. 2. Praha: Vydavatelství ČVUT, 2002. p. 191. ISBN 80-010-2609-4.
[4] Lievens, Y., et al. Activity-based costing: a practical model for cost calculation in radiotherapy. International Journal of Radiation Oncology*Biology*Physics, 2003, vol. 57, no. 2, p. 522–535.
[5] Gupta, P., Parmar, N. Costing a hospital service product: Marginal Vs absorption costing. Medical Journal Armed Forces India 2001, vol. 57, no. 3, p. 230–233.
[6] Swan, T. et al. Direct Cost Analysis of Intensive Care Unit Stay in Four European Countries: Applying a Standardized Costing Methodology. Value in Health, 2012, vol. 15, no. 1, p. 81–86.
[7] William F, et al. The ISPOR Good Practices for Quality Improvement of Cost-Effectiveness Research Task Force Report. Value in Health, 2009, vol. 12, no. 8, p. 1086–99.
[8] Tsorakidis, N., et al. Break-Even Analysis: Business, 2009. ISBN: 978-87-7681-098-4.
[9] Burton, A., Billingham L. J, Bryan S. Cost-effectiveness in clinical trials: using multiple imputation to deal with incomplete cost data. Clinical Trials, 2007, vol. 4, no. 2, p. 154–61.
[10] Lioui, A., Time consistent vs. time inconsistent dynamic asset allocation: Some utility cost calculations for mean variance preferences. Journal of Economic Dynamics and Control, 2013, vol. 37, no. 5, p. 1066–96.
Štítky
Biomedicína
Článek vyšel v časopiseLékař a technika

2014 Číslo 1-
Všechny články tohoto čísla
- Rational operation of MRI equipment in university hospitals in the Czech Republic
- Individualization of head related transfer function
- Gene expression profiling after angiogenesis inhibitor treatment
- The effect of acetylsalicylic acid on angiogenesis in vitro
- The effect of docetaxel on molecular melting profile of DNA extracted from human breast adenocarcinoma MCF-7 cells
- Metalické nanočástice v prostředí terapeutického ultrazvuku – Studium viability nádorových buněk in vitro
- Metoda měření poddajnosti a těsnosti modelů respirační soustavy pacienta
- Lékař a technika
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Metoda měření poddajnosti a těsnosti modelů respirační soustavy pacienta
- Rational operation of MRI equipment in university hospitals in the Czech Republic
- Metalické nanočástice v prostředí terapeutického ultrazvuku – Studium viability nádorových buněk in vitro
- Individualization of head related transfer function
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání