-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
Authors: E. Nutterová; Š. Pitrová; J. Lešták
Authors place of work: Oční klinika JL FBMI ČVUT v Praze ; V Hůrkách 10; 00 Praha 5-Nové Butovice, Přednosta: doc. MUDr. Ján Lešták, CSc., MSc, MBA, LL. A, DBA, FEBO, FAOG 158
Published in the journal: Čes. a slov. Oftal., 76, 2020, No. 1, p. 29-36
Category: Původní práce
doi: https://doi.org/10.31348/2020/4Summary
The objective of this study was a retrospective assessment of two-year experience with micropulse cyclophotocoagulation (MP CPC) in the therapy of various types of glaucoma.
Material and method: The cohort of patients consisted of 47 people, out of which 16 men and 31 women. An average age of males was 58.9 years (the range from 35 to 78 years), and an average age of females was 64.7 years (the range from 33 to 86 years). Both eyes were treated in three patients, and therefore the total number of assessed eyes was 50. Patients who underwent the therapy were in different stages of glaucoma disease, with various types of primary and secondary glaucoma. Most of the patients were those with primary open angle glaucoma (POAG): 26 patients, followed by patients with secondary pseudoexfoliative glaucoma (PEXG): 9 patients; diagnoses of the remaining patients: 4 patients – secondary pigmentary glaucoma (PG), 3 patients - primary angle closure glaucoma (PACG), 2 patients normal tension glaucoma (NTG), 3 patients - Posner-Schlossman syndrome, 1 patient - Cogan-Reese syndrome, 1 patient - neovascular glaucoma and 1 patient – secondary traumatic glaucoma. On the operated eye prior to the surgery 3 patients underwent laser iridotomy, 4 patients trabeculectomy, 4 patients EX-PRESS® implant, 3 patients EX-PRESS® implant and trabeculectomy and 1 patient transscleral cyclophotocoagulation. During surgery we opted for from 2,000 to 2,250 mW infrared laser with 810 nm wavelength which uses a micropulse system of laser energy emission. For the procedure we used a new MP3 application probe. 30% drop in intraocular pressure (IOP) compared to the baseline IOP values was set as a success.
Results: Our results correlated with the most of available studies when we achieved drop in the values of intraocular pressure by the minimum of 30% in 53.4% of the eyes. The effect of therapy failed in 9 eyes (18%) where we subsequently selected a different therapeutic procedure.
Conclusion: MP CPC is a non-incisional laser treatment with minimum complications. It is characterized by a high safety profile and predictability of results. In our study we achieved drop in the values of intraocular pressure by the minimum of 30% in 53.4% of treated eyes. Its use is not limited by the type of glaucoma disease. In the event of insufficient effect, it may be repeated.
Keywords:
micropulse cyclophotocoagulation – pulse emission of radiation – MP3 probe
INTRODUCTION
Laser therapy of glaucoma enables the reduction of intraocular pressure (IOP) by a non-invasive method, either by increasing outflow via the trabecular meshwork or by reducing the production of intraocular fluid through the ciliary body [3,10]. Whereas selective laser trabeculoplasty (SLT) uses a Neodymium-doped yttrium aluminium garnet laser (Nd: YAG laser) with a wavelength of 532 nm for the application of laser energy to the region of the trabecular meshwork, with the aim of increasing the outflow of intraocular fluid via this structure, transscleral cyclophotocoagulation consists in the continual effect of a diode laser with a wavelength of 810 nm on the region of the tip of the ciliary body, thereby leading to a reduction of the production of intraocular fluid. A further method – micropulse trabeculoplasty – uses a laser of a shorter wavelength of 532 and 577 nm, the energy is applied to the region of the trabecular meshwork and the effectiveness is comparable with SLT [6]. Complications following the application of SLT are minimal, the method can be used repeatedly, according to AAO Preferred Practice Patterns it is a good choice of therapy in incipient forms of glaucoma [6,17]. It also has very effective use in the therapy of glaucoma in pregnant and breastfeeding women [17,20]. Transscleral cyclophotocoagulation is a highly effective method, but is linked with a higher risk of complications. Among the most frequent are irritation of the eyeball, deterioration of vision, cystoid macular edema (CME), hypotonia, phthisis of the eyeball or sympathetic ophthalmia [2,3,4,6,10,11,19]. As ensues from the above, until recently it was not possible to use a laser method without having to choose between safety with a lesser therapeutic effect or effectiveness with a high risk of complications.
Chew demonstrated in his studies that a clinical effect can be attained without the destruction of the ciliary body. The desired effect can be reached upon breach of the integrity of the pigment epithelium of the ciliary body only in the region of the pars plana, while the pars plicata may remain intact [7]. This revolutionary discovery opened up a space for the introduction of a further laser method, known as micropulse cyclophotocoagulation (MP CPC). A new type of laser probe was developed for precise targeting of the laser beam to the pars plana region. Whereas the G-probe, used in transscleral cyclophotocoagulation, emits radiation in parallel with the optical axis to the tips of the ciliary body, the new MP3 probe is constructed in such a manner that the beam, which is emitted by a probe precisely 3 mm from the limbus, strikes only the pars plana region of the ciliary body.
There is also a difference in the manner of application. In transscleral cyclophotocoagulation we apply the probe to one or both of the hemispheres perilimbally, in the form of individual isolated points, whereas in micropulse cyclophotocoagulation a slow, sliding motion of the probe is used perilimbally within the scope of 360°. However, the fundamental difference consists in the manner of emission of laser energy. Continual emission of laser radiation in classic cyclophotocoagulation is considered to be the reason for pronounced destructive changes in the region not only of the tips of the ciliary body, but also of the stroma and ciliary muscle. This non-selective effect of radiation is the basis of pronounced inflammatory changes and postoperative complications.
MP CPC controls the rise in temperature and the destructive processes in the tissue by dividing the continual laser beam into a series of short, repeated pulses. During the course of application, the ON and OFF phases of the cycle are alternated. The actual coagulation effect represents only 31.3 % of the application time. Because the laser is in the OFF phase for 68.7 % of the application time, damage to the collateral tissue is minimal, in which we refer to the “cool off” effect. This alternation of the active and inactive phase of the laser provides the tissue with time for calming and regeneration [7,10,11,13,16]. Micropulse trabeculoplasty and micropulse photocoagulation, used for example in the therapy of CME [2,6], are based on a similar principle. It is assumed that the increase in the outflow of intraocular fluid via the uveoscleral pathway also contributes to the mechanism of the effect.
Experimental studies [9,18] demonstrate that MP CPC acts upon the lengthwise fibres of the ciliary muscle. This causes a shift of the scleral spur in a posterior direction, and subsequently to a modification of the trabecular meshwork and facilitation of the flow of the chamber fluid. The principle is similar to the mechanism of effect of pilocarpine, which causes an enlargement of the trabecular spaces and an expansion of the Schlemm's canal. At present it is not possible to determine precisely the extent to which these mechanisms influence resulting IOP, or whether the decrease thereof is the result of a combination of all the mechanisms.
The purpose of our study was to present a retrospective evaluation of two-year experiences with micropulose cyclophotocoagulation in the therapy of various different types of glaucoma.
COHORT OF PATIENTS
In the period from December 2016 to December 2018, a total of 47 patients, comprising 31 women and 16 men, were treated at our centre using the method of micropulse cyclophotocoagulation. In three patients both eyes were treated, thus ultimately 50 eyes were evaluated. The average age of the men was 58.9 years (range 35-78 years), of the women 64.7 years (range 33-86 years). Patients with various different types of glaucoma were represented in our cohort: 26 with primary open angle glaucoma (POAG), 9 with secondary pseudoexfoliative glaucoma (PEXG), 4 with secondary pigment glaucoma (PG), 3 with primary angle closure glaucoma (PACG), 2 with normotensive glaucoma (NTG), 3 with Posner-Scholssman syndrome, and one patient each with Cogan-Reese syndrome, neovascular glaucoma and secondary post-traumatic glaucoma respectively (Graph 1). Before the procedure we determined the following information: age and sex of patient, type of glaucoma, best corrected distance visual acuity, IOP value, number of pharmaceutical preparations used before procedure, and any applicable prior surgical or laser procedures. Before treatment using MP CPC, 3 patients had undergone laser iridotomy on the operated eye, 4 patients had undergone trabeculectomy with mitomycin C, 4 patients implantation of an EX-PRESS® P-200 implant with mitomycin C and trabulectomy with mitomycin C, and 1 patient had undergone transscleral cytophotocoagulation (Table 1). The observation period was within the range of 3 to 24 months.
Graph 1. Representation of individual types of glaucoma in cohort. POAG: primary open angle glaucoma, PEXG: pseudoexfoliative glaucoma, PG: pigment glaucoma, PACG: primary angle closure glaucoma, NTG: normotensive glaucoma, Sy. Posner-Schlossman: Posner-Schlossman syndrome, Sy. Cogan-Reese: Cogan-Reese syndrome, Neovascular G: neovascular glaucoma, Post-traumatic G: post-traumatic glaucoma 
Tab. 1. Number and type of procedures before MP CPC 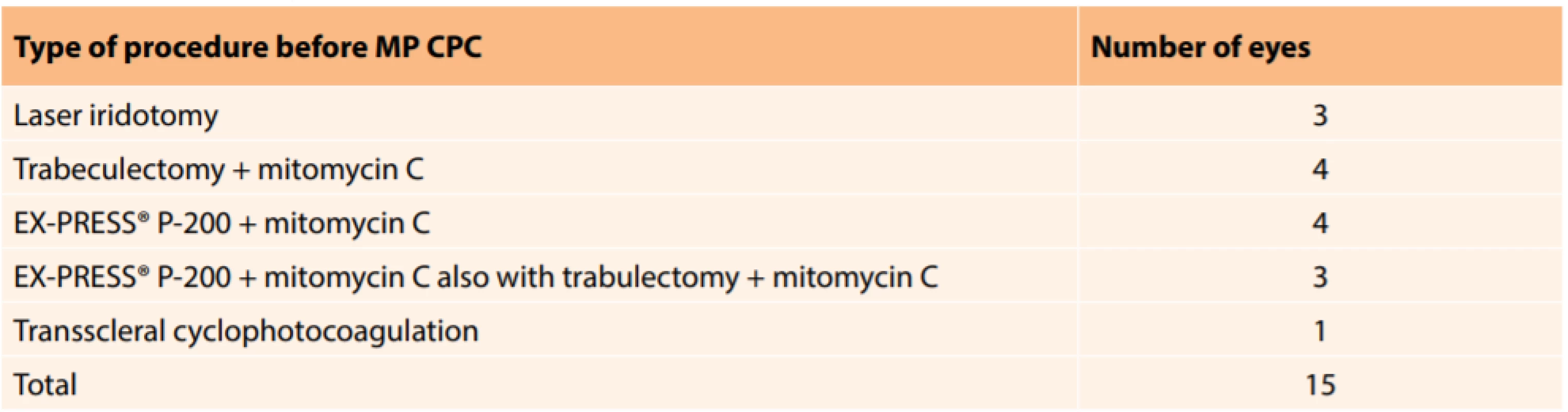
MP CPC: micropulse cyclophotocoagulation METHOD
For the performance of the procedure, we used a laser Cyclo G6TM Glaucoma Laser System, Mountain View, CA, USA, from the Iridex company (Fig. 1). During the operation an MP3 probe was used. The probe is oriented toward the limbus through an incision on the edge. In this position, emission of energy takes place at a distance of 3 mm from the limbus into the pars plana region of the ciliary body (Fig. 2). Method of anaesthesia: in 44 eyes we used topical anaesthesia together with analgosedation. We applied parabulbar anaesthesia to only 6 patients. In the majority of patients we thereby attempted to minimise the increase in pressure in the retrobulbar space by the volume of anaesthetic, which could have caused a progression of pronounced glaucomatous changes. We did not make use of the possibility of either general or subconjunctival anaesthesia.
Fig. 1. Laser Cyclo G6 from Iridex company. Setting of the parameters can be seen on the monitor of the instrument: length of application 80 seconds, energy 2000 mW 
Fig. 2. MP3 application probe. The arrow indicates the incision on the probe. During the course of application the probe is oriented via the incision toward the corneal limbus. 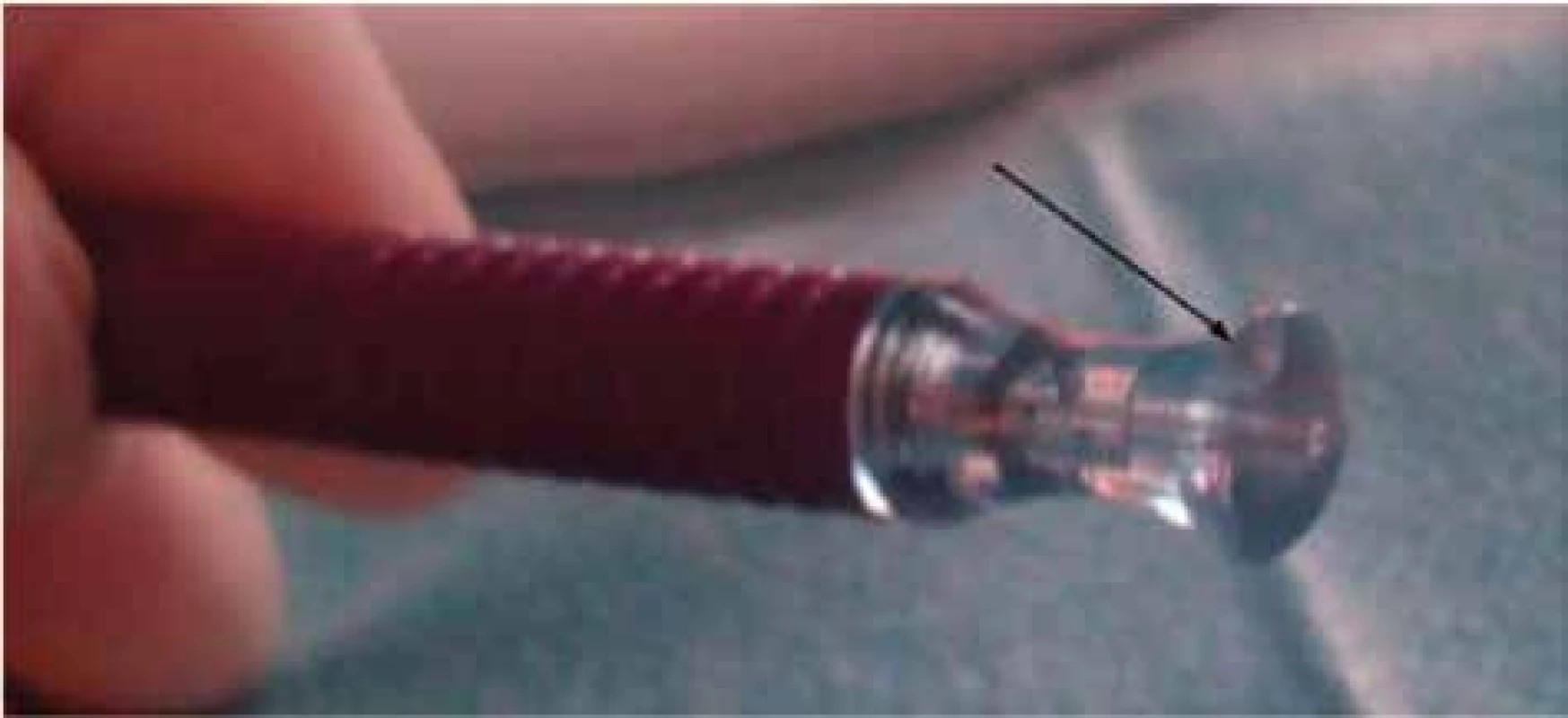
We applied a laser with energy of 2000 mW to 46 eyes for a period of 80 seconds to the upper hemisphere and 80 seconds to the lower hemisphere, within a scope of 9 : 30 to 2 : 30 and from 3 : 30 to 8 : 30 in a slow, sliding movement. As is recommended by the standard procedure, the position in no. 3 and 9 was omitted with the aim of minimising the risk of damage to the long posterior ciliary arteries and nerves. In one eye the application time was prolonged to 2x 90 seconds, while maintaining energy of 2000 mW, and in 2 eyes energy of 2250 mW was used in a length of application of 2x 80 seconds. In one eye, with regard to the complicated terrain on the upper hemisphere following previous surgical operations, energy of 2000 mW was applied in a length of 90 seconds only to the lower hemisphere. After the procedure the patients were applied local corticoid drops for a period of one week. Follow-up examinations took place 1 day, 1 week, 1 month and 3 months after the procedure, and further at an interval of 6 months or more frequently, according to the current finding in the patient. During follow-up examinations, subjective complaints of the patient were observed, as well as inflammatory changes in the anterior chamber, IOP values, which were measured by a noncontact tonometer (Canon TX-F Full Auto Tonometer), best corrected distance visual acuity on a Snellen chart and number of used anti-glaucomatous agents. Immediately after the procedure, the patients continued in the application of the original anti-glaucomatous therapy, the frequency of which was adjusted in the postoperative period according to the current IOP values. We set a reduction of IOP values by a minimum of 30% as the criterion of success.
RESULTS
Our cohort incorporated 50 eyes of 47 patients with various types of glaucoma, as stated in graph 1. The most frequent type of glaucoma treated by MP CPC was POAG. The highest IOP value before the procedure was 58 mmHg. The average reduction of IOP was overall from 25.0 ± 6.7 mmHg to 16.7 ± 4.2 mmHg. The scope of effectiveness of MP CPC in individual types of glaucoma is presented in summary in table 2. As ensues from table 2, we attained the best therapeutic effect in the group with Posner-Schlossman syndrome and in neovascular glaucoma. By contrast, the therapy was not effective in patients with normotensive glaucoma, for whom we indicated MP CPC due to the progression of changes in the visual fields, where anti-glaucomatous therapy was not capable of reducing IOP. Average IOP decreased from 25.0 ± 6.7 mmHg on the first day after the procedure to 17.1 ± 4.5 mmHg, one week after the procedure to 15.8 ± 4.7 mmHg, one month after the procedure to 16.4 ± 5.2 mmHg, three months after the procedure to 16.4 ± 4.0 mmHg, six months after the procedure to 16.3 ± 4.0 mmHg and twelve months after the procedure to 14.0 ± 5.1 mmHg. These results are presented in summary in graph 2. We recorded a pronounced reduction in values of intraocular pressure on the first day after the procedure, and this change was statistically significant (p < 0.05). The reduction in the values of average IOP was statistically significant in every observed period in comparison with the values of average IOP before the procedure. The changes of IOP values between the individual measurements after the procedure were not significant. A reduction of IOP by a minimum of 30 % was achieved in 53.4 % of eyes. By contrast, we observed failure of the effect of therapy in 9 eyes (18 %). In the postoperative period we recorded the following complications: feeling of pain in or around the eye in 7 eyes, subconjunctival suffusion in 7 eyes, superficial injection of conjunctiva in 6 eyes, feeling of burning in 4 eyes, reaction in anterior chamber in 3 eyes. In one patients we observed transitory mydriasis, and in another patient vomiting (Graph 3). We assume that the reason for transitory mydriasis could have been the incorrect position of the probe close to the limbus. We adjusted the condition of the cornea within the course of one month. We did not observe hypotonia, corneal edema, sympathetic ophthalmia or phthisis of the eyeball. We evaluated the success of the procedure and change of the number of pharmaceutical preparations 3 months after the procedure. The number of pharmaceutical preparations before the procedure was within the range of 0-5, after the procedure within the range of 0-4. The average number of pharmaceutical preparations decreased from 2.6 before the procedure to 2.3 three months after the procedure (Graph 4). This change was not statistically significant. We did not attain a satisfactory effect 3 months after the procedure in 9 eyes (18 %). In three eyes we subsequently chose anti-glaucoma surgery with the use of an EX-PRESS® P-200 implant + mitomycin C, in one eye trabulectomy with mitomycin C, in one eye transscleral cyclophotocoagulation, in two eyes adjustment of local therapy. In two eyes (NVG and PEXG) we proceeded to reapplication of micropulse cyclophotocoagulation with an increase of energy used (Table 3). In an eye with neovascular glaucoma, IOP was reduced by as much as 61 % after the first operation, although during the course of further observation retinal detachment occurred with a subsequent postoperative elevation of IOP. As a result we proceeded to reapplication of MP CPC. The effectiveness of the second application in this patient was again high: 45.8 %. In an eye with pseudoexfoliative glaucoma, IOP was reduced after reapplication by 33 %. The selected therapeutic procedure after failure of the first application of MP CPC is presented in table 3. We did not record loss of vision. A deterioration of vision in the eyes of one patient occurred due to progression of cataract. By contrast, in eyes with severe loss of vision before the procedure we recorded a feeling of clarification and extension of the scope of light projection. We observed an improvement of vision by a minimum of 1 row of Snellen chart in 8 eyes. Changes of vision are presented in summary in graph 5.
Graph 2. Values of average IOP before procedure and during course of subsequent follow-up examiantions with standard deviation, n – number of patients at individual follow-ups 
Graph 3. Complications following micropulse cyclophotocoagulation 
Graph 4. Histogram of number of eyes and number of pharmaceutical preparations and average number of pharmaceutical preparations before procedure and 3 months after procedure, NS – not significant 
Graph 5. Changes of vision following micropulse cyclophotocoagulation 
Tab. 2. Range of effectiveness of MP CPC in individual groups of glaucomas 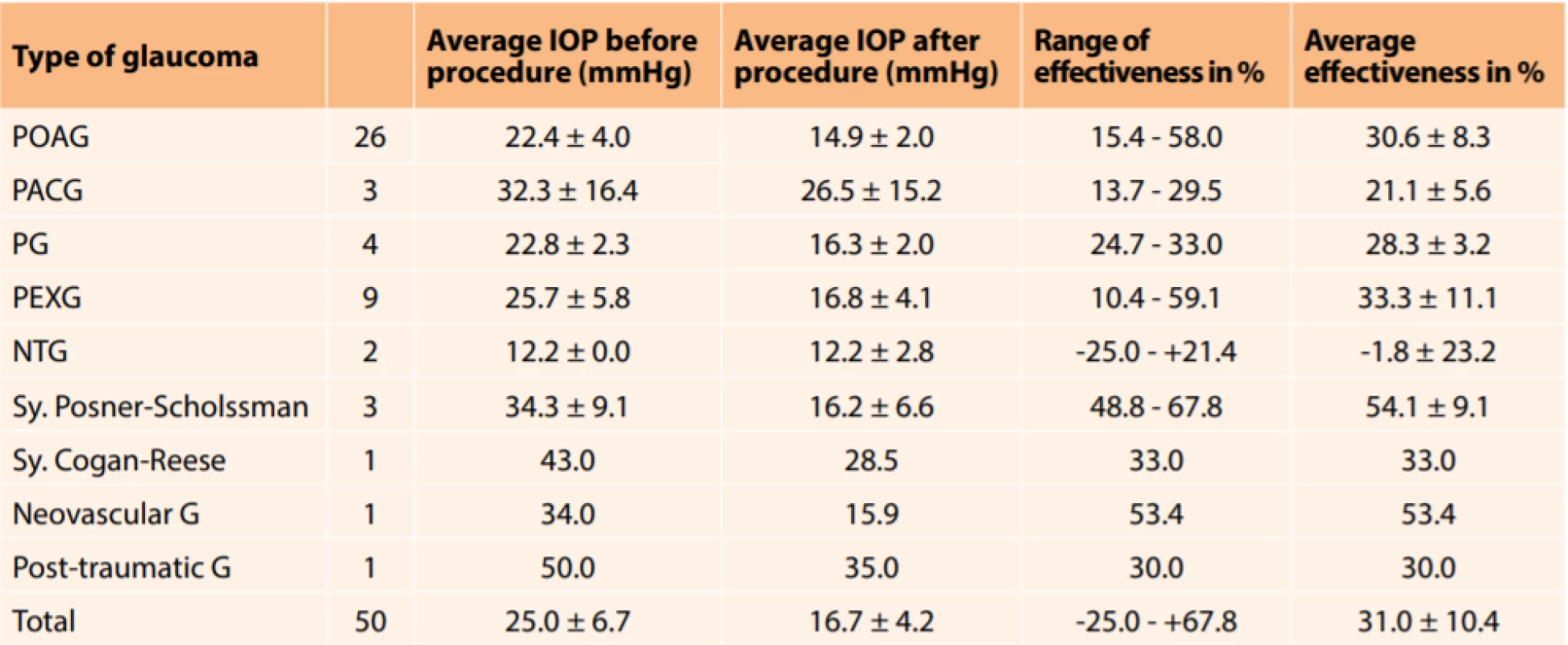
MP CPC: micropulse cyclophotocoagulation, POAG: primary open angle glaucoma, PACG: primary angle closure glaucoma, PG: pigment glaucoma, PEXG: pseudoexfoliative glaucoma, NTG: normotensive glaucoma, Sy. Posner-Schlossman: Posner- -Schlossman syndrome, Sy. Cogan Reese: Cogan-Reese snydrome, Neovascular G: neovascular glaucoma, Post-traumatic G: post-traumatic glaucoma, IOP: intraocular pressure Tab. 3. Failure of effect of first application of MP CPC and its solution in individual types of glaucoma 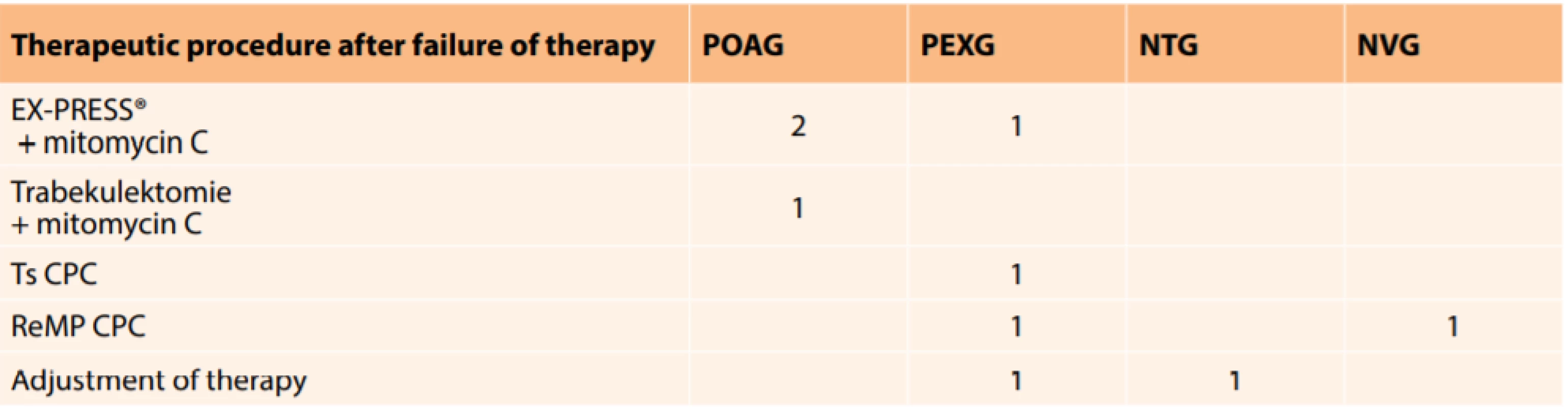
MP CPC: micropulse cyclophotocoagulation, POAG: primary open angle glaucoma, PEXG: pseudoexfoliative glaucoma, NTG: normotensive glaucoma, NVG: neovascular glaucoma, Ts CPC: transscleral cyclophotocoagulation, ReMP CPC: reapplication of micropulse cyclophotocoagulation DISCUSSION
MP CPC is a non-invasive laser treatment with a minimum of inflammatory changes. It uses the principle of repeating functional and non-functional cycles during the course of application. It does not cause visible destructive changes in the ciliary body. The length and intensity of the application can be regulated [18]. If the recommended energy and time of application is adhered to, the risk of complications is minimal. In the case of an insufficient effect, it is possible to repeat the procedure. Micropulse cyclophotocoagulation is a relatively new method of treatment. Despite the basic recommendations of the manufacturer, the energy used and time of application differs in various studies. Sanchez [18] compares the results of studies mapping experiences with micropulse cyclophotocoagulation with the aim of delineating the scope of used energy and application time that guarantees the maximum effect with a minimum of complications. In a comparison of nine carefully selected studies, he draws the conclusion that the best effect with minimum of complications is attained upon the application of energy within the range of 112-150 J, which corresponds to 2000 mW for a time of 180-240 s, or 2250 mW for a time of 160-210 s. Under these conditions, effectiveness is within the range of 30 %, with minimal or no complications. Upon the use of higher levels of energy, the effect of the procedure is increased up to 60 %, but the number of complications increases dramatically. This is demonstrated by Emanuel [4], who refers to the results of application in 84 eyes, in which both the length of application (240-360 s) and the method of application (slow, sliding and quick movement in application) differ markedly.
Postoperatively he describes inflammatory complications with the necessity of applying a corticord for a minimum length of 3 months in 86 % of eyes, and a deterioration of vision in 41 % of patients for various reasons (hypotonia, hyphema, inflammatory complications). The majority of authors compare the overall effect of the method in all types of glaucoma in total [1,2,3,4,5,10,11,19]. We did not encounter a case where the effectiveness was compared in individual types of glaucoma. Some authors [14,19] also include various numbers of reapplication (1-5 times) in the evaluation of the overall effect. In our cohort we proceeded to one application of MP CPC in only 2 eyes (PEXG and NVG), with an increase in the energy used. Even despite this stricter evaluation, we attained the set target – a reduction of IOP by a minimum of 30 % in 53.4 % of eyes. The energy we applied was within the range of the lower limit of the safe values, which was recommended by Sanchez [18] on the basis of comparison. The possibility of further modifying our procedures for further patients without going beyond the limits of the safe zone therefore remains an option. The average reduction in the number of pharmaceutical preparations in our cohort was from 2.6 to 2.3. In comparison with the literature, the reduction in the eyes we treated was smaller, but we believe that this result may also be linked to the fact that in our cohort we used energy in the lower half of the recommended range [1,14,15,16].
The type of anaesthesia is also not standardised. The manufacturer offers the option of using general anaesthesia, or retrobulbar, subconjunctival or a combination of topical anaesthesia with i.v. analgosedation. We did not use general anaesthesia due to the excessive burden placed on the patient. We most frequently selected a combination of topical anaesthesia with i.v. analgosedation, which requires close co-operation with an anaesthesiologist, but places less of a burden on the patient. It ensues from the available literature that the majority of authors use retrobulbar anaesthesia [10,11,13,14,19]. In our cohort we used this only in 6 eyes. According to our experiences, this type of anaesthesia guarantees the patient comfort during the course of the procedure, but at follow-up examinations we recorded feelings of pressure and pain in the surrounding area of the eye, although these feelings persisted only for a few days. In our opinion subconjunctive anaesthesia could limit good contact of the MP3 probe with the perilimbal region upon application, and for this reason we did not use this type of anaesthesia on any of the operated eyes.
The incidence of complications in our cohort was minimal. During the course of the learning curve, we recorded the occurrence of subconjunctival suffusion, which was caused by an injury to the conjunctiva by a projection in the centre of the convexity of the application probe or by necessary fixation of the bulb by forceps during the procedure. The occurrence of transitory mydriasis in one eye after the procedure was caused by incorrect position of the probe close to the limbus, and the condition was corrected within one month. Pain in the eye or the surrounding area described by patients in 7 eyes was evaluated as mild, or at most medium-severe. The use of a non-steroid antiphlogistic agent per os for the period of duration of the complaints was sufficient for its treatment. Irritation of the conjunctiva in 6 eyes and reaction in the anterior chamber in 3 eyes disappeared within 1 week upon application of a local corticoid, we did not need to prolong treatment in any case.
Effectiveness fluctuated within our cohort, depending on the type of glaucoma. The use of MP CPC is not limited by the type of glaucoma, though an exception is represented by uveitic glaucoma, in which the application of a laser could lead to activation of a reaction in the anterior chamber, reduction of outflow via the trabecular meshwork, increase of IOP and a failure of the effect of laser therapy, or also to the occurrence of CME. We achieved the most pronounced reduction of IOP in our patients with Posner-Schlossman syndrome. However, we must state that this concerned individual eyes, and a larger cohort and a longer observation period would be necessary in order to draw definitive conclusions. In two eyes with NTG we indicated MP CPC due to progression of changes in the visual fields, in which anti-glaucomatous treatment was no longer capable of reducing IOP and the patients refused a surgical procedure. We took as our basis the conclusions of the Collaborative Normal-Tension Glaucoma Study Group [8]. We did not record the required effect of therapy in these 2 laser-treated eyes. We are aware of the fact that it is necessary to evaluate a large group of patients with a longer observation period in order to reach valid and definite conclusions.
CONCLUSION
MP CPC is a non-invasive laser method, which provides the advantages of high effectiveness, reduction of local therapy, and thereby an improvement of adherence. In our cohort we recorded a reduction of IOP by a minimum of 30 % in 53.4 % of treated eyes. Failure of the effect of therapy occurred in 9 eyes (18 %), for which we subsequently selected a different therapeutic procedure. The effectiveness of MP CPC is lower in comparison with transscleral cyclophotocoagulation [2,3,5,12], but the incidence of subsequent complications is incomparably lower [2,6,10,14,15,16]. It is also possible to use this method in early stages of glaucoma, and also in patients with good vision. In the case of an insufficient effect it is possible to repeat the procedure, and its use does not prevent subsequent therapeutic procedures (other laser method or anti-glaucoma operation). The use of MP CPC is not limited by the type of glaucoma pathology, with the exception of uveitic glaucoma.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company. The authors further declare that the study has not been submitted to any other journal or printed elsewhere, with the exception of congress abstracts and recommended procedures.
Zdroje
1. Aquino, MC., Chew, P.: Long-term efficacy of micropulse diode transscleral cyclophotocoagulation in the treatment of refractory glaucoma, [online] 2016 [cit.10. března 2018]. Dostupné na: www.medsrl.com.ar/wp-content/uploads/2016/08/Long-term-efficacy-of-MicroPulse-P3.pdf
2. Aquino, MC., Barton, K., Tan, AM. et al.: Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Exp Ophthalmol, Jan-Feb 43 (1); 2015 : 40–46.
3. Bendel, RE., Patterson, MT.: Observational report: Improved outcomes of transscleral cyclophotocoagulation for glaucoma patients. Medicine (Baltimore), Jun 9 (23); 2017: e6946.
4. Emanuel, ME., Grover, DS., Fellman, RL. at al.: Micropulse cyclophotocoagulation: Initial results in refractory glaucoma. J Glaucoma, Aug 26 (8); 2017 : 726-729.
5. Fichtl, M., Betková, J., Janek, M.: Transsklerální cyklofotokoaulace diodovým laserem v léčbě maligního glaukomu. Sborník abstrakt: XXII. výroční sjezd České oftalmologické společnosti, Praha, 19.-21. června 2014. Ústí nad Labem, BOS. org s.r.o., 2014, s. 79.
6. Chadha, N.: New laser therapies for glaucoma. Cataract & Refractive Surgery Today. [online]. 2017 [cit. 26. února 2019]. Dostupné na: https://crstoday.com/articles/2017-sept/new-laser-therapies-for-glaucoma/
7. Chew, P.: Insight into inovation, Developing a new glaucoma laser probe. Glaucoma experts [online]. 2016 [cit. 26. února 2019]. Dostupné na: https://millennialeye.com/articles/2016-jul-aug/insights-into-innovation/
8. Collaborative Normal-Tension Glaucoma Study Group: Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol, Oct 126 (4); 1998 : 487-497.
9. Johnstone, M., Wang, R., Padilla, S. et al.: Transscleral laser induces aqueous outflow pathway motion and reorganisation. [online]. 2017 [cit. 24. ledna 2019]. Dostupné na: https://www.iridex.com/portals/0/pdf/Transcleral-induces-aqueous-outflow-pathway-motion-and-reorganization-Dr.pdf
10. Kuchar, S., Moster, MR., Reamer, CB.: Treatment outcomes of micropulse transscleral cyclophotocoagulation in advanced glaucoma. Lasers Med Sci, Feb 31 (2); 2016 : 393–396.
11. Lee, JH., Shi, Y., Amoozgar, B. et al.: Outcome of micropulse laser transscleral cyclophotocoagulation on pediatric versus adult glaucoma patients. J Glaucoma, Oct 26 (10); 2017 : 936-939.
12. Mlčák, P.: Kongres České glaukomové společnosti, Olomouc, 12.–14. dubna 2018. Dostupné na: Cyklofotokoagulace – 30 měsíců zkušeností v Olomouci, X. Kongres https://www.prolekare.cz/tema/glaukom/detail/zapisky-z-x-kongresu-ceske-glaukomove-spolecnosti-8837
13. Noecker, RJ.: Micropulse P3 glaucoma device revolutionizes cyclophotocoagulation. Insert to Glaucoma Today, March/April 13 (2); 2015 : 1-2.
14. Noecker, RJ.: The benefits of micropulse TSCPC for early-stage glaucoma treatment, Ophthalmology Times Europe, Nov; 2017 : 30-32.
15. Masis, M., Coh, P., Lin, S.: Micropulse transscleral diode laser cyclophotocoagulation: Mid to long term results. AGS, 2017. Coronado, CA
16. Radcliffe, N., Vold, S., Kammer, JA. et al.: Micropulse trans-scleral cyclophotocoagulation (mTSCPC) for the treatment of glaucoma using the micropulse P3 device. [online]. 2015. [cit. 21.února 2018]. Dostupné na: http://s499648585.mialojamiento.es/biblioteca/IRIDEX/MP3%20AGS%202015%20Poster_FINAL.pdf
17. Sičáková, S., Výborný, P.: Selektivní laserová trabekuloplastika v léčbě glaukomu – výsledky v tříletém sledování, Cesk Slov Oftalmol, 66 (5); 2010 : 204-208.
18. Sanchez, FG., Peirano-Bonomi, JC., Grippo, TM.: Micropulse transscleral cyclophotocoagulation: A hypothesis for the ideal parameters. Med Hypothesis Discov Innov Ophthalmol, 7 (3); 2018 : 94–100.
19. Tan, AM., Chockalingam, M., Aquino, MC. et al.: Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Exp Ophthalmol, Apr 38 (3); 2010 : 266–272.
20. Výborný, P., Sičáková, S., Flórová, Z. et al.: Selektivní laserová trabekuloplastika – význam pro přerušení medikamentózní léčby glaukomu u těhotných a kojících žen. Cesk Slov Oftalmol, 73 (2); 2017 : 61-63.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2020 Číslo 1- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Kontaktní dermatitida očních víček
-
Všechny články tohoto čísla
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Current use of the automatic retinal oximetry. Review
- Importance of PET/CT examination in patients with malignant uveal melanoma
- Enucleation after Stereotactic Radiosurgery in Patients with Uveal Melanoma
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Importance of PET/CT examination in patients with malignant uveal melanoma
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



