-
Medical journals
- Career
Benefit of Oral Semaglutide for Patients with Type 2 Diabetes in the General Practitioner's Office
22. 5. 2024
Oral semaglutide is a modern antidiabetic suitable within primary care for people with type 2 diabetes, primarily due to its comprehensive action that includes not only reducing blood glucose and body weight but also a number of other favorable non-glycemic effects.
Introduction
From a general perspective, the pharmacological treatment of type 2 diabetes mellitus (DM2) stands on four equivalent pillars. In addition to the classical management of hyperglycemia, it includes the treatment of obesity, the treatment of associated risk factors for cardiovascular diseases (CVD), and the use of modern antidiabetic therapies with proven cardiovascular and renal benefits in patients at high or very high cardiovascular risk. The goal of treating individuals with diabetes is to prolong and improve the quality of life.
Current Position of Modern Antidiabetics in Treatment Management
The position of metformin as the first-choice antidiabetic has not been as strong as it used to be for several years (its prescription is essentially required only for the reimbursement of other antidiabetics). Particularly in patients with atherosclerotic CVD or high cardiovascular risk (without a history of CVD but with the presence of multiple risk factors), chronic heart failure (CHF) regardless of left ventricular ejection fraction, or chronic kidney disease (CKD), the benefits of glucagon-like peptide-1 receptor agonists (GLP-1RA) and sodium-glucose cotransporter 2 (SGLT2) inhibitors (also known as gliflozins) on cardiovascular and renal outcomes have been demonstrated, independent of concurrent metformin use, glycated hemoglobin (HbA1c) levels, or individually set glycemic targets. Therefore, these classes of antidiabetics are recommended to be considered as first-line therapy in the mentioned situations, or to be initiated as part of early combination treatment along with metformin.
Impact on Weight Reduction
Given that most individuals with DM2 are also overweight or obese, it is recommended to choose medications with high efficacy in reducing body weight within pharmacotherapy. This category includes GLP-1RA, such as semaglutide, including its oral form. Weight reduction should be a way to address various obesity-related complications. It is proven that, for example, a 5–10% weight loss can prevent and mitigate dyslipidemia, non-alcoholic steatohepatitis (NAFLD), or sleep apnea, and a more than 15% reduction can lead to diabetes remission, lower cardiovascular mortality, and reduce the risk of heart failure with preserved ejection fraction (HFpEF).
Favorable Impact on Comorbidities
Inadequate diabetes control is associated with the risk of microvascular complications (diabetic retinopathy, neuropathy, and nephropathy) and macrovascular complications (ischemic heart disease /IHD/, stroke /CVA/, peripheral artery disease). Patients with DM2 have a 2–3 times higher risk of developing CVD than individuals without diabetes. In everyday practice, metformin remains the first-line treatment. If this therapy is not sufficiently effective, a number of second-line drugs are available, whose selection depends on the presence of comorbidities (atherosclerotic CVD, HF, CKD), patient preferences and needs (need to minimize hypoglycemia occurrence, need for favorable body weight influence), or treatment costs and prescription restrictions (on these grounds, metformin still has to be indicated as the first-line drug).
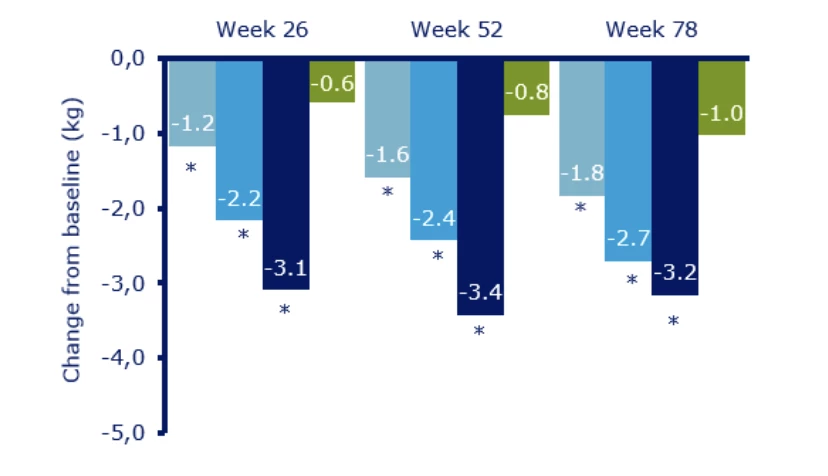
Comparison of Incretin Mimetics
Incretin mimetics, which include dipeptidyl peptidase-4 inhibitors (DPP-4i) and GLP-1RA, are established drugs in the therapy of patients with DM2. When comparing antidiabetics from the incretin group, DPP-4i have a lower potential to reduce blood glucose and a neutral effect on body weight, whereas GLP-1RA are associated with a more significant reduction in fasting glucose, postprandial glucose, HbA1c, and body weight (see Fig. 1 and Fig. 2).
Fig. 1 PIONEER 3 Study - Change in HbA1c from Baseline. Sitagliptin 100 mg is shown in green, and oral semaglutide 3 mg, 7 mg, and 14 mg in shades of blue (dark blue corresponds to the most effective dose of 14 mg).
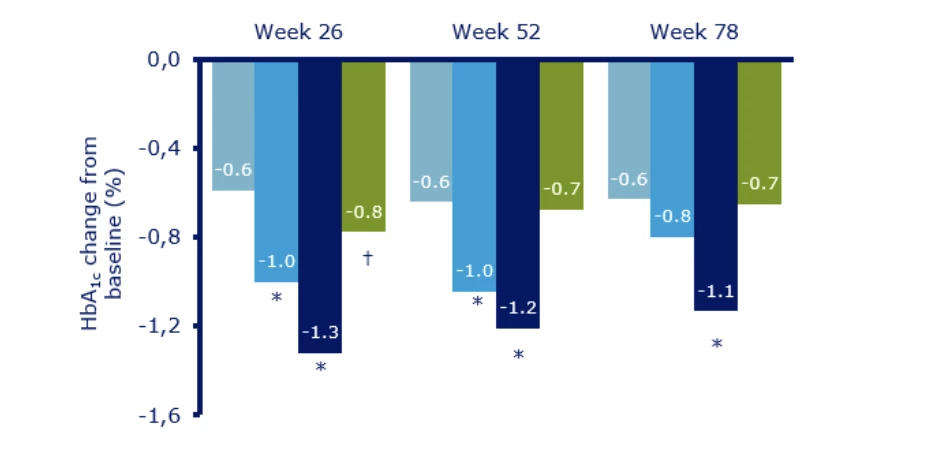
Fig. 2 PIONEER 3 Study - Change in Body Weight from Baseline. Sitagliptin 100 mg is shown in green, and oral semaglutide 3 mg, 7 mg, and 14 mg in shades of blue (dark blue corresponds to the most effective dose of 14 mg).
Prescription of Antidiabetics in the GP's Office
From a practical point of view, after metformin, a general practitioner can prescribe a sulfonylurea derivative (SU), DPP-4i, or oral GLP-1RA semaglutide. Generally, the use of SU is no longer part of modern antidiabetic therapy and should be avoided due to the risk of hypoglycemia (especially dangerous in the elderly or individuals with a history of CVD), adverse effects on the myocardium and increased body weight, and frequent failure of efficacy over time (so-called secondary failure of oral antidiabetics). For several years now, general practitioners have been able to prescribe DPP-4i instead of SU, which is certainly right considering their safety compared to SU. However, given the new possibility to prescribe oral semaglutide at basic reimbursement from HbA1c 53 mmol/mol if previous therapy with metformin (or metformin and SU) did not lead to the target HbA1c < 53 mmol/mol (using the maximum tolerated dose of metformin for at least 6 months), this pathway should be preferred (most often in combination with metformin, less commonly in triple combination with metformin and SU at a lower dose). It is therefore evident that patients can access this modern therapy already in the early stages of diabetes.
Benefits of Oral Semaglutide in Brief
As studies and our practical experience have shown, oral semaglutide is the most effective oral antidiabetic. In studies with subcutaneously (s.c.) administered semaglutide, it demonstrated significant cardioprotective properties in patients with a history of CVD with DM2, beyond glucose and weight reduction, regardless of HbA1c values and other parameters. The PIONEER 6 cardiovascular safety study also showed the potential of oral semaglutide to influence not only cardiovascular but also overall mortality. Oral semaglutide exerts anti-atherogenic effects (lowers CRP levels as a marker of systemic inflammation), slightly reduces blood pressure, and also lowers postprandial lipid levels. A significant benefit in the general practitioner's office is its effect on weight reduction, mainly through actions in the CNS, where it increases the feeling of satiety, decreases the feeling of hunger, and favorably modulates food selection in favor of healthier options. In this significant way, it can positively influence the motivation of individuals with obesity in losing weight. The effect on weight reduction obviously exhibits interindividual differences, and there are approximately 5–10% of individuals in whom it is minimal (this applies generally to the entire GLP-1RA group).
Basic Patient Education
Education before starting oral semaglutide therapy is simple. It is essential to emphasize to the patient the necessity of taking the tablets on an empty stomach with the smallest amount of water possible and, importantly, to leave a gap of at least 30 minutes from other medications and food (the longer, the better). This measure is crucial for the efficacy of semaglutide, not for better tolerance. The dose is titrated monthly from the initial 3 mg through the intermediate 7 mg to the target 14 mg orally. The aim is to achieve the highest dose, as it is the most effective. Gradual titration aims to limit the undesirable gastrointestinal side effects typical for the entire GLP-1RA group. Reducing portion sizes at the beginning of pharmacotherapy also helps, further contributing to positive eating behavior modulation.
Conclusion
In summary, oral semaglutide is a modern antidiabetic suitable within primary care for people with DM2, as it acts comprehensively, reducing weight and blood glucose and having a number of other favorable non-glycemic effects.
The basic reimbursement for oral semaglutide is associated with a relatively high patient co-payment. However, this is fully included in the so-called protective limit, which varies by age, so the total annual amount invested by the patient in oral semaglutide treatment certainly does not outweigh the aforementioned benefits. The amount of co-payment should thus not discourage the general practitioner from offering modern treatment that provides significant benefits to the patient even in the initial stage of DM2.
MUDr. Milan Flekač, Ph.D., MUDr. Eva Flekačová
Comfort Care Ambulance, General Practitioner’s Office Prague 6
FLEDIP, Diabetes Clinic, Prague 6References:
1. Davies M. J. et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2022; 65 : 1925–1966.
2. Ansari H. U. et al. Efficacy and safety of glucagon-like peptide-1 receptor agonists on body weight and cardiometabolic parameters in individuals with obesity and without diabetes: a systematic review and meta-analysis. Endocr Pract 2024 Feb; 30 (2): 160–171.
3. Rosenstock J. et al. Effect of additional oral semaglutide vs sitagliptin on glycated hemoglobin in adults with type 2 diabetes uncontrolled with metformin alone or with sulfonylurea: the PIONEER 3 randomized clinical trial. JAMA 2019; 321 (15): 1466-1480.
4. Verma S. et al. Effects of once-weekly semaglutide 2.4 mg on C-reactive protein in adults with overweight or obesity (STEP 1, 2, and 3): Exploratory analyses of three randomized, double-blind, placebo-controlled, phase 3 trials. EClinicalMedicine 2022; 55 : 101737.
5. Gibbons C. et al. Effects of oral semaglutide on energy intake, food preference, appetite, control of eating and body weight in subjects with type 2 diabetes. Diabetes Obes Metab 2021; 23 (2): 581–588.
6. Aroda V. R. et al. A new era for oral peptides: SNAC and the development of oral semaglutide for the treatment of type 2 diabetes. Rev Endocr Metab Disord 2022; 23 (5): 979–994.Abbreviated product information for Rybelsus® HERE.
CZ24RYB00205
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Diabetology Obesitology General practitioner for adults General practitioner for children and adolescents
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

