-
Medical journals
- Career
Analysis of the Benefits of Combining Enalapril/Bisoprolol in Patients with Acute MI
13. 5. 2024
A recently published retrospective analysis compared the outcomes achieved by administering enalapril alone and in combination with bisoprolol in patients after acute myocardial infarction over a period of 1 year.
Introduction
The goal of treatment for acute myocardial infarction (AMI) is to restore perfusion to the affected artery as quickly as possible and minimize the extent of necrosis. Long-term treatment must be initiated as soon as possible, aimed at improving the patient's prognosis, reducing the risk of further cardiovascular events, and improving quality of life. Long-term treatment includes both lifestyle measures and pharmacotherapy. Antihypertensives are an integral part of pharmacotherapy. Hypertension is the most common risk factor for the development of ischemic heart disease (IHD) and roughly 25% of AMIs can be attributed to hypertension.
Treatment with angiotensin-converting enzyme inhibitors (ACEi) is unequivocally recommended for patients with left ventricular (LV) systolic dysfunction or heart failure, hypertension, or diabetes. It should be considered for all patients with ST-segment elevation myocardial infarction (STEMI).
For all patients after STEMI, the routine use of beta-blockers (BB) should be considered. These are recommended for patients with reduced LV systolic function (LV ejection fraction ≤ 40%) without contraindications such as acute heart failure, hemodynamic instability, or higher-degree atrioventricular (AV) block. For hemodynamically stabilized patients, oral BB treatment should be considered within the first 24 hours.
Beta-blockers and renin-angiotensin system blockers can improve the prognosis of patients after myocardial infarction.
Assessed Data and Study Objectives
The cited retrospective analysis by Chinese authors included data from a total of 104 patients with AMI treated from May 2019 to October 2021. The observation group (n = 56) received combined enalapril and bisoprolol therapy, and the control group (n = 48) received enalapril alone. The inclusion criteria were detailed clinical data and a diagnosis of AMI without concurrent diagnosis of mental disorder or cognitive dysfunction. Patients who took statins or beta-blockers before admission, those with coagulation disorders, chronic myocardial infarction, heart failure, or pregnant women were excluded. All patients also received routine treatment with oxygen, sedatives, acetylsalicylic acid, clopidogrel, atorvastatin, low-molecular-weight heparin, and nitrates.
In both groups, treatment response (based on disappearance of arrhythmia, subjective symptoms, and EKG findings), adverse events, heart function (LV EF), left ventricular end-diastolic diameter (LVED), left ventricular end-systolic diameter (LVES), and left ventricular mass (LVM) were analyzed after 6 months of treatment. Prognosis was compared based on mortality during follow-up for up to 1 year.
Results
Both groups were comparable in terms of main characteristics (age, gender, BMI, disease course, history, smoking).
In the enalapril/bisoprolol combination group, treatment response was achieved significantly more often (p < 0.05).
Effect on Heart Function
After 6 months, LVES, LVED, and LV EF values significantly increased in both groups (p < 0.05), with significantly lower LVES and LVM and higher LV EF observed in the enalapril/bisoprolol group compared to the enalapril-alone group.
Fig. 1 Changes in Heart Function:
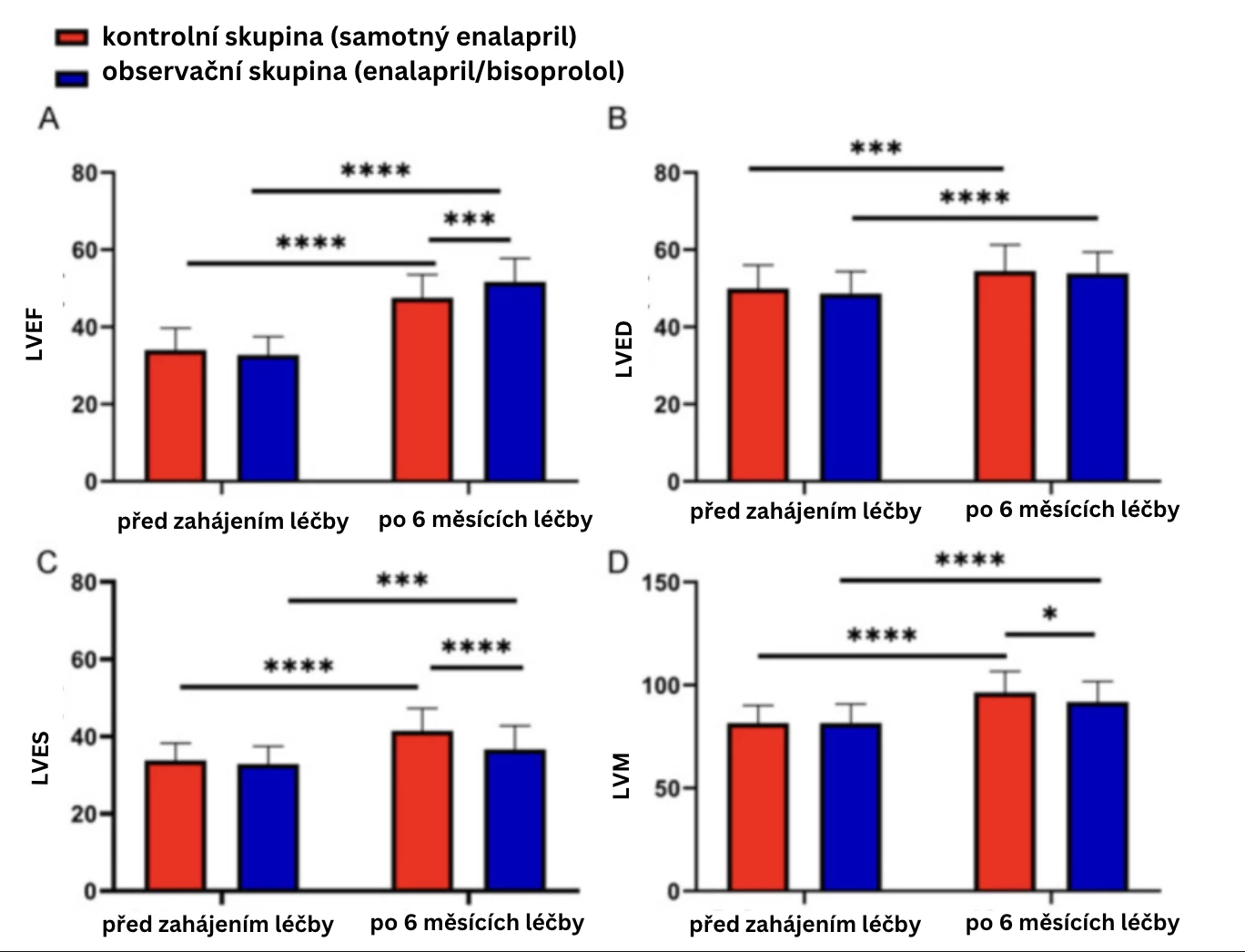
Note: *p < 0.05; **p < 0.01; ***p < 0.001; ***p < 0.0001
EKG Indices
Comparison of EKG indices between the two groups showed that while there were no differences in Q-wave time and ST-segment offset before treatment, there was a significant reduction in Q-wave time and ST-segment offset in both groups after treatment. A shorter Q-wave time and lower ST-segment offset were observed in the enalapril/bisoprolol combination group (p < 0.001).
Fig. 2 Changes in EKG Indices:

Safety of Treatment
Monitoring results revealed no significant differences in the incidence of adverse treatment reactions (p < 0.05).
Tab. Comparison of Adverse Treatment Reactions
Number of Patients Cough Hypotension Rash Sinus Bradycardia Overall Incidence (%) Control Group 48 2 (4.16) 2 (4.16) 0 (0.00) 2 (2.08) 5 (10.42) Observation Group 56 2 (3.57) 3 (5.35) 1 (1.78) 1 (1.78) 7 (12.50) x2 Value 0.110 p Value 0.740 Patient Prognosis
One-year survival was comparable in both groups (p > 0.05).
Conclusion
The combination of antihypertensives enalapril/bisoprolol is an effective and safe therapeutic option in the treatment of acute myocardial infarction with a positive impact on patients' heart function.
(lexi)
Sources:
1. Li M., Gao H., Wang Y., Wang Z. Outcome effects of enalapril with or without bisoprolol in patients with acute myocardial infarction. Am J Transl Res 2023 Mar 15; 15 (3): 2025–2032.
2. Kala P., Mates P., Želízko M. et al. ESC Guidelines for the treatment of acute myocardial infarction in patients with ST-segment elevation, 2017: a summary document prepared by the Czech Society of Cardiology. Cor et Vasa 2017; 59: e613–e644.
3. Oštádal P., Táborský M., Linhart A. et al. Brief summary of recommendations for long-term care of patients after myocardial infarction 2022. Cor et Vasa 2022; 64 (Suppl. 1): 7–23.
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Diabetology Internal medicine Cardiology General practitioner for adults
Latest courses
Authors: doc. MUDr. Jan Bruthans, CSc., doc. MUDr. Miroslav Solař, Ph.D., prof. MUDr. Miroslav Souček, CSc.
Go to courses
Popular this week Whole articleLogin#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


