-
Medical journals
- Career
C-NAIL – 8-YEAR TREATMENT RESULTS
Authors: Martin Pompach 1; Marek Peml 2; David Prchal 3; Martin Carda 1
Authors‘ workplace: Oddělení úrazové chirurgie, Nemocnice Pardubického kraje, a. s. 1; Traumatologické oddělení, Nemocnice České Budějovice a. s., Česká republika 2; Oddělení chirurgie a traumatologie, Kroměřížská nemocnice a. s., Česká republika 3
Published in: Úraz chir. 28., 2021, č.1
Overview
INTRODUCTION: Open reduction and osteosynthesis is associated with a certain risk of impaired healing of the surgical wound, especially with improper timing. Minimally invasive procedures make it possible to reduce this risk, with the advantage of earlier treatment of the fracture. The C-nail is an implant allowing for minimally invasive, highly stable osteosynthesis of calcaneal fractures.
OBJECTIVE: To prospectively evaluate our own cohort of patients treated with the C-nail and compare these results with studies using plate osteosynthesis from an open lateral approach.
HYPOTHESIS: With the use of the C-nail, we expect higher biomechanical stability, a lower incidence of postoperative complications, especially a low percentage of infection development and better functional results compared to the conventional plating method with comparable functional results.
COHORT OF PATIENTS AND METHOD: A total of 249 patients (222 males and 27 females, mean age 47.3 years) with 265 calcaneal fractures indicated for surgical treatment were included in the cohort and were operated on between 2011-2018 with a C-nail implant at the Department of Trauma Surgery, Pardubice Hospital, according to the inclusion criteria. Patients‘ data were evaluated for postoperative complications, restitution of the Böhler’s angle, and reconstruction of the posterior articular surface based on radiographs and CT scans taken preoperatively, postoperatively, and at 12 months. Functional outcome was assessed using the American Orthopaedic Foot and Ankle Society (AOFAS) scoring system - Ankle - Hindfoot Scale. Data from the available literature were used as a control set.
RESULTS: The average AOFAS score after 12 months was 90.5. Marginal wound necrosis was observed in three cases (1.1 %) and soft tissue infection in one case (0.4 %). The Böhler’s angle was restored from an average of 5.9° preoperatively to 32.1° postoperatively. After 12 months, a slight decrease in the Böhler’s angle to 27.6° was observed.
CONCLUSION: The results of our cohort compared with those using conventional plating with an extensive lateral approach show that both methods have comparable AOFAS scores. The use of the nail is burdened with a significantly lower percentage of complications, especially a low risk of infection. C-nail is a method applicable to all types of calcaneal fractures classified according to Sanders. It can preferably be used in dislocated and open fractures.
Keywords:
C-nail – calcaneal fracture – minimally invasive approach
INTRODUCTION
Surgical treatment of dislocated calcaneal fractures has become the standard method in recent decades. Open reduction and osteosynthesis is associated with a certain risk of impaired healing of the surgical wound, especially with improper timing. Minimally invasive procedures make it possible to reduce this risk, with the advantage of earlier treatment of the fracture. The C-nail is an implant that allows both minimally invasive and highly stable osteosynthesis of these fractures. The aim of this study is to prospectively evaluate our own cohort of patients treated with the C-nail nail and to compare these results with studies using plate osteosynthesis from an open lateral approach. With the use of the C-nail, we expect higher biomechanical stability, lower incidence of postoperative complications, especially a low percentage of deep infection development with comparable functional results compared to the conventional plating method.
COHORT AND METHOD
All calcaneal fractures operated on with a C-nail between 2011–2018 at the Department of Trauma Surgery, Pardubice Hospital were included in this prospective study.
Study inclusion criteria: All intra-articular fractures classified according to Sanders - type I, IIA, IIB, IIC, IIIAB, IIIAC, IIIBC and IV on the basis of CT scan, extra-articular fractures indicated for surgical treatment, open and dislocated fractures, fractures with impending compartment syndrome, patients with compensated DM, smokers.
Exclusion criteria: Fractures with minor calcaneus abruptions unsuitable for osteosynthesis, children with active calcaneal apophysis, patients with calcaneus shorter than 65 mm, soft tissue infections with decompensated diabetes, severe vasculopathy, immunodeficiency or uncooperative patients (drug abuse or severe mental illness).
A total of 249 patients with 265 fractures met these criteria.
Examination and monitored parameters: Preoperatively, age and sex were recorded, fractures were classified according to Sanders according to preoperative CT and the Böhler’s angle and degree of dislocation at the articular surface were measured, DM, nicotinism, presence of bilateral fractures were also recorded, soft tissue condition was assessed according to Gustilo and Anderson classification for open fractures and Tscherne and Oestern classification for closed fractures [14]. Postoperatively, X-ray and CT were performed, the Böhler’s angle and the quality of reduction (step off) were measured. Complications in terms of deep infection, injury to the sural nerve, the presence of arthrosis, the need for nail extraction and the formation of a nonunion were also observed. After 12 months, the patients underwent X-ray and CT scans, the Böhler’s angle was measured, and the functional outcome was assessed according to the AOFAS Ankle-Hindfoot Scale.
Description of the implant and surgical technique
Implant: The C-nail is made of surgical steel, 65 mm long and 8 mm in diameter. It is available in left and right hand versions and can be extended by 5, 10, 15 and 20 mm using end plugs. The insertion of 3.5 mm cortical screws passing through the nail is achieved with a three-arm targeting device. These screws are introduced in three directions. The sustentacular arm targets two convergent screws in the oblique, lateromedial direction, two screws are targeted by the upper arm to the tuberosity in the proximodistal direction, and 2–3 screws introduced from the lateral arm provide stability to the tuberosity and processus anterior.
Approach: The minimally invasive approach (sinus tarsi approach) starts below the apex of the fibula and goes about 3–4 cm towards the base of the fourth metatarsus. This approach allows good visualization of the subtalar joint.
Reduction: The use of a heel distractor facilitates the reduction of the calcaneal fragments. It is essential for achieving the correct calcaneal axis, correcting the varus/valgus deformity and at the same time restoring the calcaneal height (Fig. 2). The application of the calcaneal distractor is technically performed by inserting two 6 mm Schanz screws into the distal tibia and into the calcaneal tuberosities from the lateral side. After the distractor body is loaded onto the Schanz screws, the distension is performed. The use of a tourniquet for a limited period of intra-articular repositioning is another option to increase clarity. In all cases, a tourniquet was used during the operation. The reduction of individual fragments of the articular surface in the subtalar joint proceeds from the medial to the lateral side. Once the articular surface is reduced and the Böhler’s angle restored, the position of the fragments is temporarily fixed with Kirschner wires. The congruence of the articular surface is further verified on X-ray using the Broden’s view. The final fixation of the posterior articular surface is achieved by the application of two short-threaded cancellous bone screws, applied under X-ray control (Fig. 3). At this stage, two parallel Kirschner wires with a diameter of 2.0 mm are inserted obliquely ascending from the calcaneal tuberosities into the talus so as not to interfere with the future placement of the nail. At this stage it is possible to cancel the distraction.
Fig. 1: C-nail, targeting device with three arms (sustentacular, upper and lateral), nail length 65 mm, diameter 8 mm, fragments can be fixed with up to 7 screws. Two screws are inserted into the sustentaculum tali, two into the tuber calcanea, and two to three from the lateral arm into the tuberosity and into the processus anterior 
Fig. 2: To insert the heel distractor, it is necessary to place the Schanz screw into the tuber calcaneus and into the distal tibia from the lateral side. By changing the angle of the Schanz screw, followed by distraction, the correct axis, length and height of the calcaneus can be regulated. This makes the reduction of dislocated fragments of the posterior articular surface and access to the subtalar joint easier 
Fig. 3: The picture shows the correct position of two separate screws under the posterior joint surface, their position can be checked in the axial view. After reduction, it is advisable to fix the fragments temporarily with two Kirschner wires from the tuber calcanei to the talus medially and laterally, so that they do not prevent subsequent insertion of the nail. The heel distractor must be removed before commencing the nailing 
Nail introduction: A short horizontal incision of approximately 10–15 mm on the dorsal side of the calcaneal tuberosity just below the insertion of the Achilles tendon is introduced through a guide wire slightly lateral to the medial axis of the tuberosity and follows the longitudinal axis of the calcaneocuboid joint. Achieving the ideal position of the guidewire is checked by X-ray in lateral and dorsoplantar view. The hole for the nail is then reamed with a cannulated drill bit. The guide wire is removed after the reaming. The nail itself with corresponding laterality is then assembled with a three-arm targeting device and is easily inserted into the cavity created. The targeting device is fitted with guide sleeves and the first guide wire is introduced into the sustentaculum tali by point injection. The correct position of the guide wire is verified on the axial view X-ray. If it is correct, a second guide wire is inserted. If the position is not correct, the first wire is pulled out and the position of the nail and the targeting device is corrected by slight rotation. Once the optimal position of both guide wires is achieved, the first one is removed and, after replacing the insert of the guide sleeve, an adequate hole is drilled, its length measured and a screw is applied, passing through the nail to the medial part of the sustentaculum tali (Fig. 4). The application of the second sustentacular screw is easily followed by the application of the other 4-5 screws, again using the targeting device. The operation is completed by the application of a plug of adequate length after dismantling the targeting device. This is followed by insertion of the Redon drainage and soft tissue suture.
Fig. 4: After reaming, a C-nail is inserted using a targeting device under the Achilles tendon. Two sustentacular screws are inserted first, followed by two upper and two to three lateral screws 
Postoperative care
All patients had a standard postoperative course. Deep vein thrombosis prophylaxis with low molecular weight heparin for one month was indicated in all cases. Redon drainage was removed on the second postoperative day. On the first postoperative day, the patients started active rehabilitation, exercises in the ankle joint. Plaster fixation was not indicated in any patient postoperatively. Progressive loading on the operated calcaneus was allowed from the 8th week.
RESULTS
A total of 249 patients with 265 calcaneal fractures who underwent surgery were between 17–73 years of age (mean age 47.3 years + - 12.9 years). Among them, 48.2 % were smokers and 8.4 % were type I/II diabetics with good compensation (Table 1). Based on the preoperative CT scan, the fracture was classified according to Sanders as type I (n=18), type IIA (n=95), IIB (n=53), IIC (n= 16), IIIAB (n=37), IIIAC (n=12), IIIBC (n=12), and IV (n=22). There were six patients with open calcaneal fractures (2.3 %). Table 1 shows the basic demographic and clinical characteristics of all patients included in the study. The mean value of the Böhler’s angle measured preoperatively was 5.9° ± 11.6 (-58°–40°); the mean value of the Böhler’s angle measured immediately after surgery was 32.1° ± 7.2 (15°–40°).
1. Main characteristics of 249 patients with 265 intra-articular calcaneus fractures treated with C-nail calcaneal nail 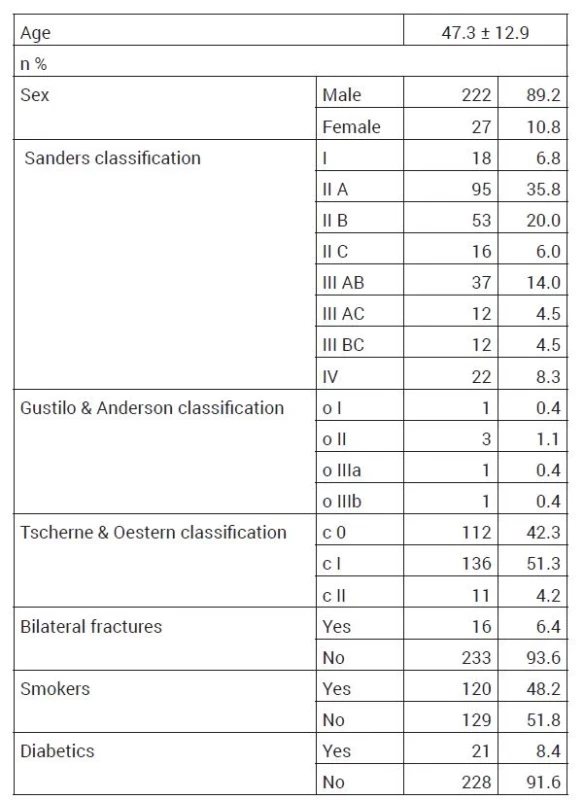
All the operated fractures healed. One year after the surgery, there was a slight decrease in the Böhler’s angle to the average of 27.6° ± 7.4 (15°–40°). Based on the CT scan, the preoperative value of posterior articular surface incongruence (step-off) averaged 5.6mm ± 4.8 mm (0–30 mm), whereas the postoperative value of this parameter averaged 0.7 mm ± 1.4 mm (0–10 mm) (Fig. 5a-e). The average AOFAS value after one year achieved 90.5 points ± 8.19 (75–100) (Table 2). There is a significant correlation between fracture severity as classified by Sanders and functional outcome as assessed by the AOFAS at 12 months (Table 4). For Sanders type 1 fractures (n=18) AOFAS 94.5 points, Sanders type 2 (n=164) AOFAS 92.4 points, Sanders type 3 (n=61) AOFAS 90.7 points, Sanders type 4 (n=22) 89.3 points. Posttraumatic arthrosis of the subtalar joint was detected in six cases (2.3 %) during the eight-year follow-up; only one case (0.4 %) required subtalar arthrodesis due to severe pain. Range of motion at 1 year was fully restored in 27 % of cases (100 % when compared to the uninjured side), slightly limited in 38 % of patients (76–100 % when compared to the uninjured side), partially limited in 32 % of patients (50–75 % when compared to the uninjured side), and substantially limited in 3 % of patients (less than 50 % when compared to the uninjured side). Sural nerve injury has never been diagnosed. In three cases, marginal wound necrosis developed (1.1 %). Only one patient (0.4 %) developed a deep infection (Staphylococcus aureus). The C-nail was used in this case in a beak fracture and the infection developed at the nail insertion site (Table 3). C-nail was extracted in only 6 patients (2.3 %). The time from injury to surgery ranged from day 0 to day 23, on the average day 4. Patients were discharged from the hospital on postoperative day 5 (3 – 63 days). From the above results, it can be concluded that all fractures of the calcaneus healed and no nonunion formation was observed.
Fig. 5: Dislocated intra-articular fracture in a 68-year-old woman, joint depression type, Sanders 3 AB. The X-ray lateral view (a) shows the Böhler’s angle 0˚. Axial CT scan (b) shows fragment and fracture lines on the posterior articular surface, Sanders 3 AB classification. Lateral radiograph at 1 year follow-up (c) shows the Böhler’s angle of 33° and the nail passing through the axis of the calcaneocuboid joint. Axial CT scan showing the correct position of the nail, placement of the screws in the sustentaculum tali (d), reconstruction of the posterior articular surface (e) 
2. Table of mean measurements in 265 cases of intra-articular fractures of the calcaneus. Böhler’s angles preoperatively, postoperatively, and one year postoperatively are recorded. CT images show mean values and ranges of posterior articular surface incongruity measurements before and after surgery 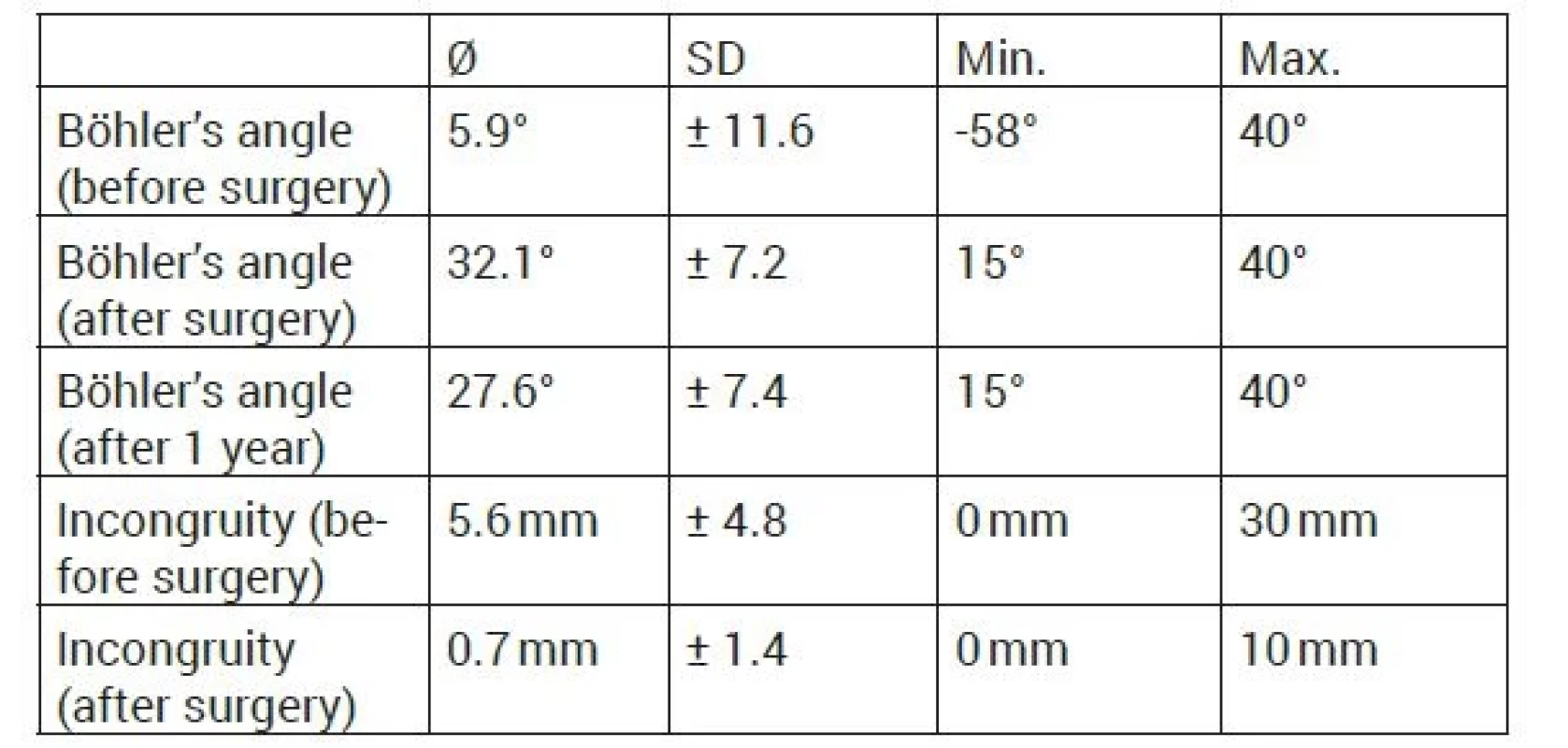
3. Early and late complications, functional scores reported in previous studies in > 100 patients using extended lateral approach and plate fixation for intra-articular calcaneal fracture compared with 265 cases of C-nail nailing (*) 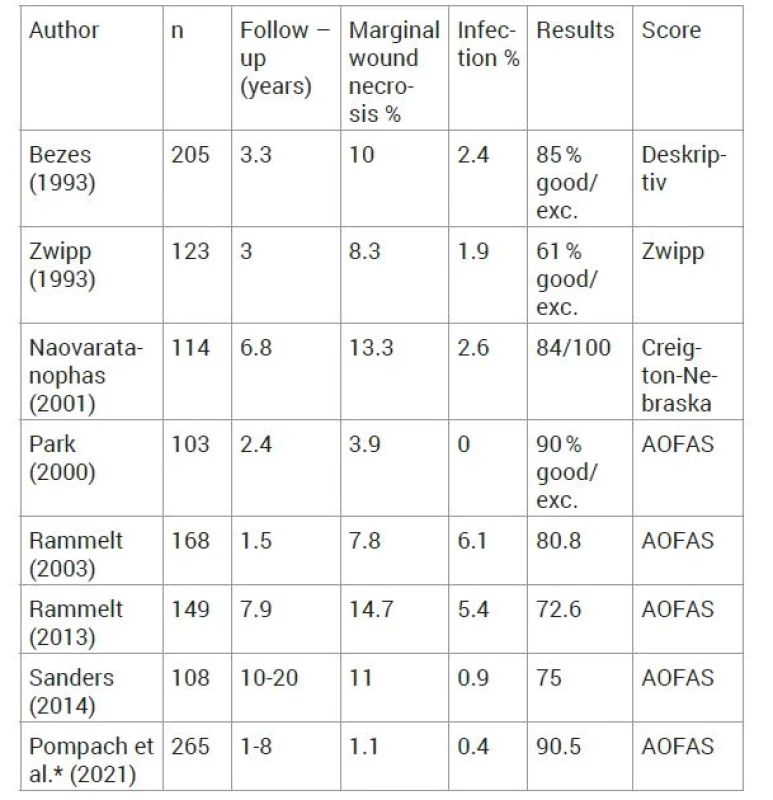
*results of this study DISCUSSION
According to the comparison of the results of our study with the literature, there is no significant difference in the indication for the use of C-nail and conventional implants. The C-nail can also be advantageously used in patients with grossly dislocated calcaneal fragments and expressed compartment syndrome. A well-done reduction is a prerequisite for the successful performance of this method [2, 9, 15, 21, 24, 25] a locking nail system (C-nail). Compared to the conventional extended lateral approach, the sinus tarsi approach is significantly less invasive, yet allows sufficient view into the subtalar joint for quality reduction and fixation of the posterior articular surface without the need for risky preparation of large volumes of soft tissue [7, 17, 22]. To date, the standard procedure for the ORIF of the calcaneus consists of an extended lateral approach in combination with an angle-stable plate [1, 3, 13, 16, 26]. However, a number of complications are associated with this procedure - a higher risk of superficial soft tissue infection (20.1 %) [1], hematoma requiring evacuation (4.7 %) [26], marginal wound necrosis (15 %) [13], deep soft tissue infection (13.6 %) [3], and even the likelihood of developing osteomyelitis of the calcaneus resulting in the need for calcanectomy [10]. To combat these complications, procedures consisting in the application of separate screws inserted percutaneously or in combination with a minimally invasive approach have been introduced. Unfortunately, the use of these procedures is characterized by lower biomechanical stability [12, 18]. In addition, pintract infection (7 %) and deep bone infection (1.7 %) are observed with percutaneous Kirschner wire fixation vs 0.4 % in our prospective study [20]. The above has led to the introduction of the combination of the minimally invasive approach and the biomechanically stable C-nail implant (Figure 1), which substantially reduces the risk of complications while maximizing the stability of the osteosynthesis [2, 9, 15, 21, 24].
The minimally invasive approach (sinus tarsi approach) in combination with C-nail osteosynthesis is a method that is well tolerated by patients. This is evident from the functional follow-up of patients according to the AOFAS score at 1 year after surgery. Surprisingly, a very small percentage of complications such as marginal wound necrosis and infection are observed, which are complications that are very much feared by all those involved in calcaneal fracture surgery. Also, only one patient in the entire cohort of patients included in this study required subtalar arthrodesis. Sanders et al. [16] present long-term results (10–20 years) in 108 patients operated on using the extensive lateral approach combined with plate osteosynthesis, with an AOFAS score of 75. These patients developed wound edge necrosis in 11 %, infection in 0.9 %, sural nerve neuritis in 6.5 %, and 29 % of patients subsequently underwent subtalar arthrodesis. Bezes et al present a 10 % incidence of marginal wound necrosis and a 2.4 % incidence of wound infection in 205 cases of operated calcaneal fractures [4]. Rammelt et al. [13] report in detail in a study following 149 patients for over 7.9 years operated on using the extensive lateral approach combined with plate osteosynthesis 14.7 % of patients with wound edge necrosis, 5.4 % infection and 6 % subtalar arthrodesis as common complications of this conventional method. The AOFAS gives a value of 72.6 points, compared to 90.5 points in our study. Some studies with a shorter follow-up time and a smaller cohort of patients in the study, report superficial soft tissue infection in 19.7 % [5], deep soft tissue infection in 13.6 % and even osteomyelitis of the calcaneus in 9 % of cases in the conventional method with an extensive lateral approach [1]. Rammelt in a 2003 study reported an incidence of postoperative hematoma requiring wound revision of about 5 % [11]. Zeman et al. [23] compared a group of 217 patients operated by the extensive lateral approach in combination with the LCP plate with a group of 19 patients operated by the innovative C-nail method. He observed comparable AOFAS scores and improvements in Böhler‘s angle in both groups. However, the deep infection rate of 1.9 % in the LCP group compared to none in the C-nail group led to the recommendation that the C-nail should be the first choice method for Sanders type 2 and 2 fractures. According to our results, C-nail can be used for all types of Sanders 1-4 classification. Veliceasa et al. [21] present the results of 75 cases treated with C-nail, where the study shows a similarly low incidence of surgical wound margin necrosis (4 %) and superficial infection (1.3 %). No deep infection was observed (0 %), AOFAS at 12 months was 90.2 points. Park et al. reports 0 % incidence of infection in the wound after osteosynthesis [8]. In contrast, Naovaratanophas et al. reported a higher incidence of marginal wound necrosis around 13.3 % [6]. Steinhausen et al. [19] present a retrospective comparative study between C-nail and plate LCP osteosynthesis where 92 patients with 101 calcaneal fractures (C-nail n=52, plate n=49) were assessed. The authors report significantly faster loading and fracture healing in the C-nail group. In addition, the LCP plate group has been shown to have a higher incidence of marginal wound necrosis and is more likely to require subtalar arthrodesis. In our study, the nail was removed in the aforementioned complication of one case of deep infection. Repeated debridement of the surgical wound was performed, NPWT therapy was loaded, and local and total antibiotic therapy was instituted. After two weeks, an antibioticsupplemented PMMA spacer was applied and subsequently the bone infection healed. It was this negative experience that led us to include the beak fractures in the contraindications. In the whole cohort, the reason for implant extraction in one case was a deep infection at the entry point of the nail, in four cases pain in the subtalar joint and in one case the extraction was performed at the patient‘s own request.
Reinhardt et al. [15] compared the biomechanical properties and stability of a standardized human cadaveric calcaneal fracture treated with three implants. C-nail (Medin, Czech Republic), Calcanail (FH Orthopaedics, France) and Rimbus locking plate (Intercus, Germany) were included in the study. This comparative study confirmed that the C-nail is more stable than the Rimbus LCP plate and much more stable than the French Calcanail implant.
CONCLUSION
Osteosynthesis with the C-nail can be used for all types of intra-articular calcaneal fractures. The results of our cohort compared with those using conventional plating with an extensive lateral approach show that both methods have comparable AOFAS scores. The use of the nail is burdened with a lower percentage of complications, especially a low risk of infection. It can preferably be used in dislocated and open fractures.
Sources
1. AL-MUDHAFFAR, M., PRASAD, CV MOFIDI, A. Wound complications following operative fixation of calcaneal fractures. Inj. Int. J. Care Inj. 2000, 31, 461–464.
2. AMLANG, M., ZWIPP, H., POMPACH, M. et al. Interlocking nail fixation for the treatment of displaced intra-articular calcaneal fractures. JBJS Essent. Surg. Tech. 2017.
3. BACKES, M., SCHEPERS, T. et al. Wound infections following open reduction and internal fixation of calcaneal fractures with an extended lateral approach. Int. Orthop. 2014, 38, 767–773.
4. BEZES, H., MASSART, P., DELVAUX, D. et al. The operative treatment of intraarticular calcaneal fractures: Indications, technique, and results in 257 cases. Clinical Orthopaedics and Related Research. 1993, 55–59.
5. COURT-BROWN, CM, SCHMIDT, M. et al. Factors affecting infection after calcaneal fracture fixation. Injury. 2009, 40, 1313–1315.
6. NAOVARATANOPHAS, P., THEPCHATRI, A. The long term results of internal fixation of displaced intra-articular calcaneal fractures. J. Med. Assoc. Thail. 2001, 84, 36–44.
7. NOSEWICZ, T., KNUPP, M, et al. Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures: A prospective computed tomography - Based study. Foot Ankle Int. 2012, 33, 925–933.
8. PARK, IH, SONG, KW. et al. Displaced intra-articular calcaneal fracture treated surgically with limited posterior incision. Foot Ankle Int. 2000, 21, 195–205.
9. POMPACH, M., CARDA, M., AMLANG, M. et al. Versorgung des Fersenbeinbruchs mit einem Verriegelungsnagel (C-Nail). Oper. Orthop. Traumatol. 2016, 28, 218–230.
10. POMPACH, M., CARDA, M., VANÁČ, J. et al. Calcaneal fracture, lifethreatening injury. Úrazová Chir. 2006, 14, 7–12.
11. RAMMELT, S., BARTHEL, S., BIEWENER, A. et al. Kalkaneusfrakturen - Offene reposition und interne stabilisierung. Zentralbl. Chir. 2003, 128, 517–528.
12. RAMMELT, S. ZWIPP, H. Fractures of the calcaneus: current treatment strategies. Acta Chir. Orthop. Traumatol. Cech. 2014, 81, 177 – 196.
13. RAMMELT, S., ZWIPP, H., SCHNEIDERS, W. et al. Severity of injury predicts subsequent function in surgically treated displaced intraarticular calcaneal fractures. Clin. Orthop. Relat. Res. 2013, 471, 2885–2898.
14. RAMON, B., GUSTILO, MD, JOHN, T. et al. Prevention of Infection in the Treatment of One Thousand and Twenty-five Open Fractures of Long Bones. J. Bone Jt. Surg. 1975, 58, 523–527.
15. REINHARDT, S., MARTIN, H. et al. Interlocking Nailing Versus Interlocking Plating in Intra-articular Calcaneal Fractures: A Biomechanical Study. Foot Ankle Int. 2016, 37, 891–897.
16. SANDERS, R., VAUPEL, ZM, ERDOGAN, M. et al. Operative treatment of displaced intraarticular calcaneal fractures: Long-term (10-20 years) results in 108 fractures using a prognostic CT classification. Journal of Orthopaedic Trauma. 2014, 28, 551–563.
17. SCHEPERS, T. The sinus tarsi approach in displaced intra-articular calcaneal fractures: a systematic review. Int. Orthop. 2011, 35, 697–703.
18. SCHEPERS, T. Sinus Tarsi Approach with Screws-Only Fixation for Displaced Intra-Articular Calcaneal Fractures. Clin. Podiatr. Med. Surg. 2019, 36, 211–224.
19. STEINHAUSEN, E., MARTIN, W. et al. C-Nail versus plate osteosynthesis in displaced intra-articular calcaneal fractures — a comparative retrospective study. J. Orthop. Surg. Res. 2021, 16, 1–10.
20. STULIK, J., STEHLIK, J., RYSAVY, M. et al. Minimally-invasive treatment of intra-articular fractures of the calcaneum. J. Bone Jt. Surg. - Ser. B. 2006, 88, 1634–1641.
21. VELICEASA, B., FILIP, A. et al. Treatment of Displaced Intra-articular Calcaneal Fractures With an Interlocking Nail (C-Nail). J. Orthop. Trauma. 2020, 34, e414–e419.
22. WEBER, M., LEHMANN, O., SÄGESSER, D. et al. Limited open reduction and internal fixation of displaced intra-articular fractures of the calcaneum. J. Bone Jt. Surg. - Ser. B. 2008, 90, 1608–1616.
23. ZEMAN, J., ZEMAN, P., MATĚJKA, T. et al. Comparison of lcp and intramedullary nail osteosynthesis in calcaneal fractures. Acta Ortop. Bras. 2019, 27, 288–293.
24. ZWIPP, H., PAŠA, L. et al. Introduction of a New Locking Nail for Treatment of Intraarticular Calcaneal Fractures. in Journal of Orthopaedic Trauma. 2016, 30, e88–e92.
25. ZWIPP, H., RAMMELT, S., AMLANG, M. et al. Operative treatment of displaced intra-articular calcaneal fractures. Oper. Orthop. Traumatol. 2013, 25, 554–568.
26. ZWIPP, H., RAMMELT, S., BARTHEL, S. Calcaneal fractures - Open reduction and internal fixation (ORIF). Injury. 2004, 35, 46–54.
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2021 Issue 1-
All articles in this issue
- IN MEMORIAM prof. MUDr. Libor Paša, PhD.
- IN MEMORIAM MUDr. Pavel Kopačka
- IN MEMORIAM prof. MUDr. Miroslav Zeman, DrSc.
- OSTEOSYNTHESIS OF HUMERAL DIAPHYSEAL FRACTURE BY INTRAMEDULLARY NAIL WITH ELECTROMAGNETIC DISTAL LOCKING - INTRODUCTION OF THE METHOD AND FIRST EXPERIENCE
- C-NAIL – 8-YEAR TREATMENT RESULTS
- POSTPARTUM SYMPHYSIOLYSIS - CASE STUDY SERIES - ANALYSIS OF LITERATURE AND OUR EXPERIENCE
- OSTEOSYNTHESIS OF THE POSTERIOR PELVIC SEGMENT WITH ILIOSACRAL SCREWS UNDER 3D NAVIGATION CONTROL
- Trauma Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- POSTPARTUM SYMPHYSIOLYSIS - CASE STUDY SERIES - ANALYSIS OF LITERATURE AND OUR EXPERIENCE
- OSTEOSYNTHESIS OF HUMERAL DIAPHYSEAL FRACTURE BY INTRAMEDULLARY NAIL WITH ELECTROMAGNETIC DISTAL LOCKING - INTRODUCTION OF THE METHOD AND FIRST EXPERIENCE
- IN MEMORIAM prof. MUDr. Libor Paša, PhD.
- OSTEOSYNTHESIS OF THE POSTERIOR PELVIC SEGMENT WITH ILIOSACRAL SCREWS UNDER 3D NAVIGATION CONTROL
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


