-
Medical journals
- Career
Surgical treatment of diaphyseal humeral fractures
Authors: Tomáš Pavlacký; Radek Veselý; Radek Suchomel; Libor Paša; Filip Sládek; Tomáš Pink; Jan Kočiš
Authors‘ workplace: Úrazová nemocnice v Brně, Klinika traumatologie, Masarykova univerzita Brno
Published in: Úraz chir. 26., 2018, č.1
Overview
Introduction:
Conservative approach is the golden standard for treatment of diaphyseal humeral fractures, supplemented with plate osteosynthesis in specific indications. However, nail osteosynthesis is becoming more popular in the recent years, namely due to a significant improvement in the areas of surgical techniques and implants used, which have resulted in a decrease of complications. This technique has become the treatment of choice at our centre.
Aim:
The aim of our work was to assess the success rate of diaphyseal humeral fractures osteosynthesis in a retrospectively evaluated patient population, and also to define the risk factors of potential non-healing.
Methods:
A total of 167 patients who were operated at the Trauma Hospital of Brno between 2011 and 2016 were enrolled into the retrospective clinical trial with 3rd degree quality evidence. The assessed parameters included the outcome of healing and the number of complications, such as paresis of n. radialis, prolonged healing or incidence of non-unions. Furthermore, we assessed in more detail a group of 17 patients with a diagnosed non-union, and concentrated upon possible predisposing factors.
Results:
We identified a total of 9 (5.4 %) patients with the complication of postoperative paresis of n. radialis. Six of these patients were operated using nail osteosynthesis; plate osteosynthesis was used in the remaining three patients. We also observed 10 patients (6.0 %) who manifested signs of prolonged healing, and a total of 17 (10.2 %) patients in whom the definition of non-union was confirmed on radiography examination. Of these patients, 15 (12.2 %) were operated using the nailing technique (12.2 %); two patients were treated with plates (5.6 %). The performed analysis of these patients revealed that the profile patient with a predisposition for occurrence of a non-union is a female in the seventh decade of her life, with a fracture in the middle third of the diaphysis, type A1 or B1 according to AO, with type 2 diabetes mellitus, and body weight on the border of obesity. None of the other observed factors has been proven significant.
Conclusion:
Plate osteosynthesis and intramedullary nailing for the treatment of diaphyseal humeral fractures present fully-fledged alternatives to the conservative approach. According to current literature, there exist no significant differences when comparing these techniques as far as the success rate of healing is concerned, although our experience suggests slightly better outcomes on radiography in patients treated with plate osteosynthesis, and a smaller incidence of n. radialis injury associated with the nailing technique.
Keywords:
complications – Diaphyseal humeral fracture – nail – plate – non-union
Aim: Retrospective analysis of results of nail and plate osteosyntheses in patients with diaphyseal humeral fractures treated at our centre.
Type of work: Retrospective study
Introduction
Diaphyseal humeral fractures account for 1–3 % of all fractures, with the incidence of 12 cases per 100,000 inhabitants. In adult patients, these fractures manifest the typical bimodal age distribution [23], with the maximal occurrence in the third decennium in males, caused predominantly by high-energy injuries, and in the seventh decennium in women, caused by low-energy trauma of the porotic skeleton. The most frequent mechanisms of injury are indirect, including a simple fall at the elbow or wrist, or a traffic accident, indirect impact or sports injuries.
Already since the Böhler’s work from 1964 [2], which strongly opposes surgical management of fresh diaphyseal humeral fractures, most works agree that the conservative approach presents an optimal therapeutic option, with satisfactory results [8, 16, 19, 20, 22]. Conservative treatment, as a definite treatment technique, does not interfere with the primary haematoma at the fracture site, and is associated with a high probability of healing without potential complications associated with the surgical approach and general anaesthesia. Another great advantage of the conservative approach is the possibility of outpatient treatment, which decreases the time burden and financial costs of treatment in these patients. It is possible to say that the technique of functional treatment, which was described by Sarmiento in 1977, is widely practiced all over the world even today [20]. The incidence of non-unions associated with this technique is rare, and should they appear, it is most frequently with fractures of the proximal third of the diaphysis [16]. The most frequently observed negative outcome of conservative treatment is a functional limitation of the shoulder or the elbow joint, or healing in a dislocated position [8].
On contrary, there exists a trend towards surgical management of these fractures in the recent years, namely due to the expected early physiotherapy and more favourable long-term functional outcomes. The available techniques of internal fixation include nail osteosynthesis, ante or retrograde plate osteosynthesis using 4.5 mm DCP (dynamic compression plate), or bridging LCP (locking compression plate) plates.
While the plate osteosynthesis has been considered the golden standard for several decades, the technique of nail osteosynthesis, and especially the materials used, have gone through a significant development in the recent years. The currently used nails, including their fixation elements, are significantly more sophisticated than the ones originally used [18]. They are more rigid, offer angular stability and the possibility of pronounced fracture retention, including the alternative of multidirectional fixation.
However, conclusions of some studies [4] suggest that nail osteosynthesis may be associated with a greater incidence of failures and non-unions when compared with plate osteosynthesis, or even the conservative approach, and does not achieve the success-rate comparable to using nails in the diaphysis of the crus or femur.
In our study, we concentrated upon a critical evaluation of outcomes of surgical management among a group of patients treated surgically at the Trauma Hospital of Brno between 2012 and 2016.
Methods
The aim of our work was to evaluate the success-rate of osteosynthesis in a retrospectively analysed patient population, and to define possible risk factors of potential non-healing.
Patients hospitalized at the Trauma Hospital of Brno between 2011 and 2016 with a diaphyseal humeral fracture were enrolled into this retrospective clinical trial with 3rd degree quality evidence. The patient data were retrieved from the hospital information system, according to the corresponding ICD (International Classification of Diseases) classification. The exclusion criteria were conservative approach, surgical procedure performed at another centre, and pathological fractures. We also excluded patients treated with an external fixator or Prévot’s nails as the definite means of fixation, and furthermore patients who were not followed until complete healing, or at least for the period of eight months post injury.
We assessed radiographic signs of healing, i.e. the presence of bridging callus formation on at least three cortices in the anteroposterior and lateral projections. We based our assumptions upon the reported anticipated period of healing lasting 4–9 months [11]. The category of prolonged healing included patients, in whom healing was achieved after this time interval, and the category of non-unions included only patients, in whom the fracture did not manifest any signs of healing after one year, and in whom the progression of healing on radiographic controls performed within the last three months was minimal or none. Furthermore, we concentrated in more detail upon a relatively numerous group of patients with non-unions. We attempted to analyse this group in more detail, and to identify some common characteristics, which may serve as negative prognostic factors for future therapeutic reasoning. We observed the sex and age of patients at the time of injury, history of comorbidities, BMI and smoking, and the level and characteristics of the fracture. In order to classify the fractures, we used the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classifications [13]. For evaluation of the fracture level, we divided the diaphysis into exact thirds, and categorized the middle of the fracture. Next, we assessed the type of osteosynthesis and the delay in performing the surgical procedure from the initial trauma. In the postoperative period, we concentrated upon the presence of postoperative infection, the earliness of initiation of active physiotherapy, and functional outcome at the last follow-up control.
Nail osteosynthesis was predominantly indicated in fractures, in which it was possible to restore the correct length, axis and rotation of the humerus using a closed reduction or reduction from minimal incision. Other criteria required for performance of nail osteosynthesis were the following: the diameter of the intramedullary cavity of at least 7 mm, so that the insertion of the nail was feasible without the need of reaming, and open fractures type 1 and 2 according to the Gustilo-Anderson classification. The remaining cases were treated with plate osteosynthesis, which was also used in patients in whom revision of the nervus radialis was indicated.
For the nail synthesis, nails of three manufacturers were used. These were most frequently inserted in the beach chair position, antegradely, from anterolateral (Mackenzie) approach, using a short incision in m. supraspinatus and subsequent reconstruction of the muscle at the end of surgery. The intramedullary cavity was reamed only in cases, when required due to its diameter. The proximal fixation was performed using an aimer device, or without it. At the distal end, the nail was always fixed with at least one screw. In fractures where it was possible, the “back slab” technique was used, in order to achieve a greater compression. Spiral fractures with greater dislocation were treated with a cerclage band in several cases, to strengthen the stability of the construction.
Plate osteosynthesis was performed using the 4.5 mm auto-compression plates, or possibly LCP plates, in cases of comminuted fractures, porotic skeleton or localization of the fracture closer to one of the metaphyses. The surgical approach was selected according to the level of the fracture, most frequently lateral, or possibly anterolateral, and rarely also dorsal, while respecting and documenting the course of n. radialis. The plates were applied as compressive, neutralization or bridging, depending on the character of the fracture. The MIO (minimally invasive osteosynthesis) technique was also used in several cases. The plates were fixed with at least three (ideally four) screws inserted into both cortices, proximally and distally.
The beginning of physiotherapy was indicated individually, depending on the character of the fracture and the subjective feeling of the patient, and was supplemented with passive exercises in the S-axis, immediately after the surgical procedure or after the first postoperative control scheduled two weeks after the procedure. Active mobilization and exercises against resistance were initiated after the first signs of healing were apparent on radiography. Extraction of the osteosynthetic material was not routinely planned in patients with problem-free course of healing.
Results
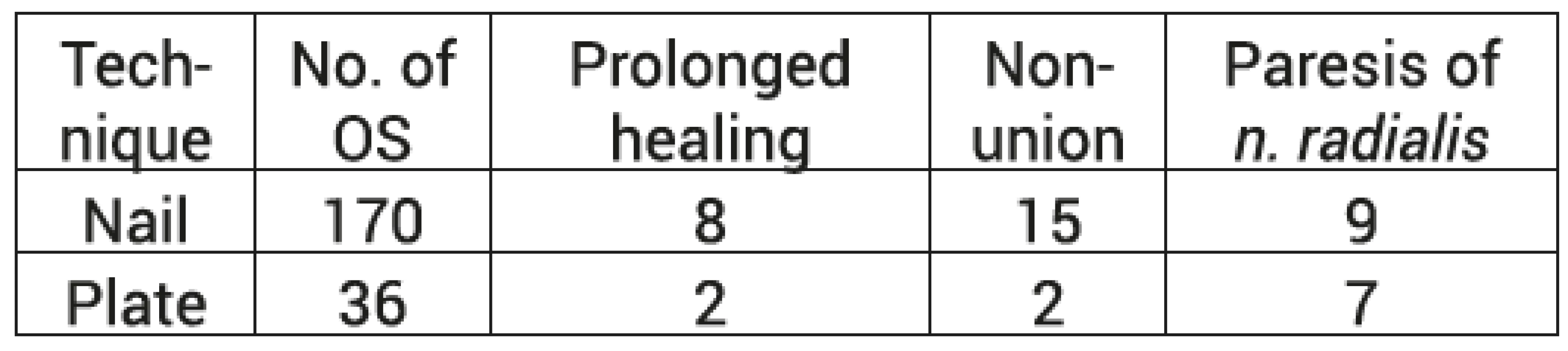
During the analysed period, a total of 349 patients with diaphyseal humeral fractures (ICD S42.3) were treated at our centre. We included 167 into our study population, 74 males (44.3 %) and 93 females (55.7 %), with the average age of 58.4 (17–93) years. In 123 (73.7 %) cases, the patients were treated with a closed reduction, followed with nail fixation. In 36 (21.6 %) patients, open reduction and plate fixation were performed (Chart 1, tab. 1).
1. Number of osteosyntheses of humeral diaphyseal fractures 
In our file, we observed a total of 9 (5.4 %) patients with complications in the form of postoperative paresis of n. radialis. Of these, 6 patients were treated with nail osteosynthesis and 3 patients using plates. Furthermore, we observed 10 (6.0 %) patients who manifested signs of prolonged healing according to the above-defined specification, and a total of 17 (10.2 %) patients, in whom the radiography findings fulfilled the definition of non-union.
According to the AO classification, fractures type A (95) prevailed, over type B (46) and type C (26) fractures. The most frequently observed fractures were simple spiral fractures, i.e. type A1. Similar findings were observed in the group of patients with non-unions and paresis of n. radialis. On contrary, the patients in the group with prolonged healing sustained most frequently type A3 fractures, i.e. fractures with transverse fracture line (Chart 2).
2. Representation of individual AO fracture types in the total patient population 
The patients with non-unions are described in the Table 2.
Among the patients with non-unions, 15 were primarily treated with a nail and 2 using the plate technique. If we concentrate upon the group of patients with nail osteosynthesis, the 15 observed non-unions account for 12.2 % of all patients treated with nails. The same applies to 5.6 % for plate osteosynthesis. This group of patients included only 3 males (17.6 %), the remaining 14 patients were females (82.4 %).
The average age of patients with non-unions was 68.2 years (31–84). Considering the characteristics of the fracture according to the AO classification, there were 8 type A fractures, 6 type B fractures, and 3 type C fractures. The most frequently affected diaphyseal level was the middle one (64.7 %), followed with the proximal (29.4 %) and the distal (5.8 %) levels. The average delay between the injury and surgery was 2.6 days. The most frequently present comorbidity was type 2 diabetes mellitus (26.3 %) and chronic alcohol abuse (15.7 %). The average BMI at the time of injury was 29.9, which is a value exactly on the border of obesity. Only five of the patients were documented smokers. In three of them, the postoperative course was complicated with a surgical wound infection. The average interval between the documented start of active physiotherapy and the surgical procedure was 49 days, i.e. 7 weeks. When evaluating the outcome clinical condition, the patients achieved the average anteflexion of 141 degrees, and average abduction of 132 degrees. Nine patients (47.4 %) reported some form of pain, either permanent or intermittent, during the last follow-up.
Discussion
Treatment of diaphyseal humeral fractures is a topic, which has been discussed in the literature many times. For a long period of time, the presented works reported on the conservative approach only. It is understandable that for example the conclusions of Sarmient’s work were the subject of many follow-up studies, which confirmed the excellent success rate of healing, reaching around 70–90 % with a correctly applied conservative therapy [1, 5, 19, 22]. On contrary, the results of osteosynthetic procedures, using either nail or plate, have only recently become the subject of summary studies with a higher relevance. Comparison of these two surgical techniques was performed by Chinese authors in their systematic overview of meta-analyses from 2015 [3, 7, 9, 10, 15], according to which there exists no significant difference in the healing rate between these two types of osteosynthesis [21]. These conclusions basically correspond with our observations of prolonged healing, which reached 6.6 % for nail and 5.6 % for plate osteosynthesis. When evaluating the incidence of non-unions, we observed a slightly higher number of cases with the nail synthesis (12.2 %), when compared with plate osteosynthesis (5.6 %). And finally, postoperative paresis of n. radialis was observed among our patients more often following plate osteosynthesis (8.3 %) than after nail osteosynthesis (4.9 %).
Both these surgical techniques possess certain limitations. The nailing technique, so successful in the treatment of diaphyseal fractures at lower extremities, was not generally accepted for a long time as a treatment option for similar fractures of the humerus [2]. The main reason for this was the fact that the technique itself and the design of the nail were initially derived from tibial or femoral ones, nevertheless, the specific anatomy and biomechanical characteristics of the humerus are different [11]. Humerus is a long bone, which however does not bear weight, so the compressive forces are not so important during the healing process, as they are in cases of tibial or femoral fractures. Also, possible shortening in length is not such a negative factor as in lower extremities. When using nail synthesis, the stimulating influence of a cyclic axial loading is missing, contrary to other body regions, which is most probably one of the reasons for the observed slower healing following nail osteosynthesis in this area [8]. It is only during the last two decades that we have seen a greater accent upon developments in this area, when, apart from new implants, also a correct surgical technique for intramedullary humeral nailing was developed. This technique decreases the risk of soft tissue complications at the shoulder. On the contrary, plate osteosynthesis has been used as an alternative to the conservative approach for longer period of time, and presents a golden standard of treatment, namely in patients with open or unstable fractures, obese patients, and in cases requiring open revision of nervus radialis [4]. According to the work of Czech authors, the osteosynthesis using a bundle of elastic nails according to Hackethal [14] may be considered another therapeutic alternative, especially in uncomplicated types of fractures.
The major representation of type A fractures according to AO classification in our patient population corresponds with the character of traumas treated at our centre, and is similar to other patient groups [21]. Type A1 fracture is the most common fracture in patients with paresis of n. radialis. In these cases, one end of the spiral bones probably touches n. radialis along its course in the middle or distal third of the humerus.
Considering the common characteristics of patients with non-unions, a non-union most frequently, i.e. in 11 cases, developed in the middle third of the diaphysis. We also observed 5 non-unions in the proximal third and only one case in the distal third. This observation is also closely related to the influence of fracture type upon the potential non-union development, which has been described earlier [17, 22]. However, the presented series contained predominantly type B fractures, which have already been mentioned in this respect. Our patient group contained a large number of A1 fractures, i.e. long and spiral fractures, which could also be considered a risk from this point of view.
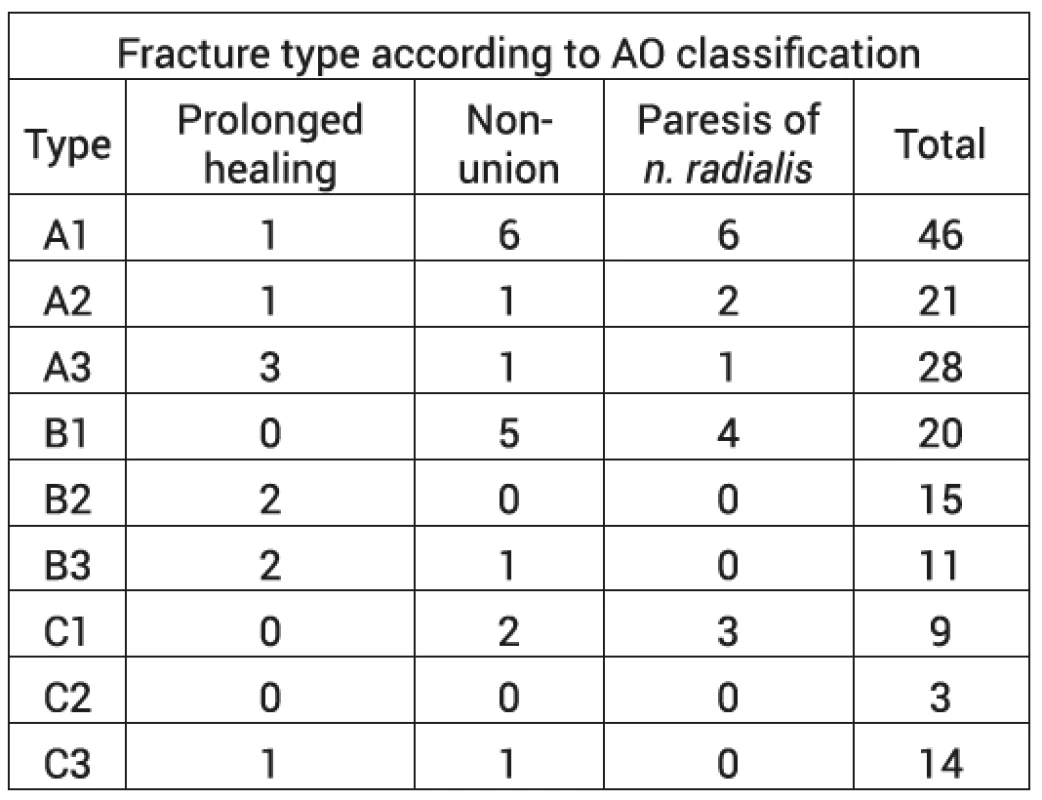
A technical error seems to be a frequent cause of non-healing, which may lead, together with other predisposing factors, to the development of a non-union. In cases of nail osteosynthesis, the error may be an entry point located too laterally or dorsally, or possibly also insufficient distal fixation, either intentional, or caused by inserting the screw outside of the nail (Fig. 1). For plate osteosynthesis, there exists a risk of insufficient compression at the fracture site, associated with attempts to achieve absolute stability (Fig. 2).
1. Radiograph of the humerus in anteroposterior and lateral projections. Postoperative radiograph (1a) and radiograph taken 13 months after injury (1b) depict a nail osteosynthesis of diaphyseal humeral fracture type A3. A non-union developed due to insufficient proximal fixation of the nail and associated instability at the fracture site 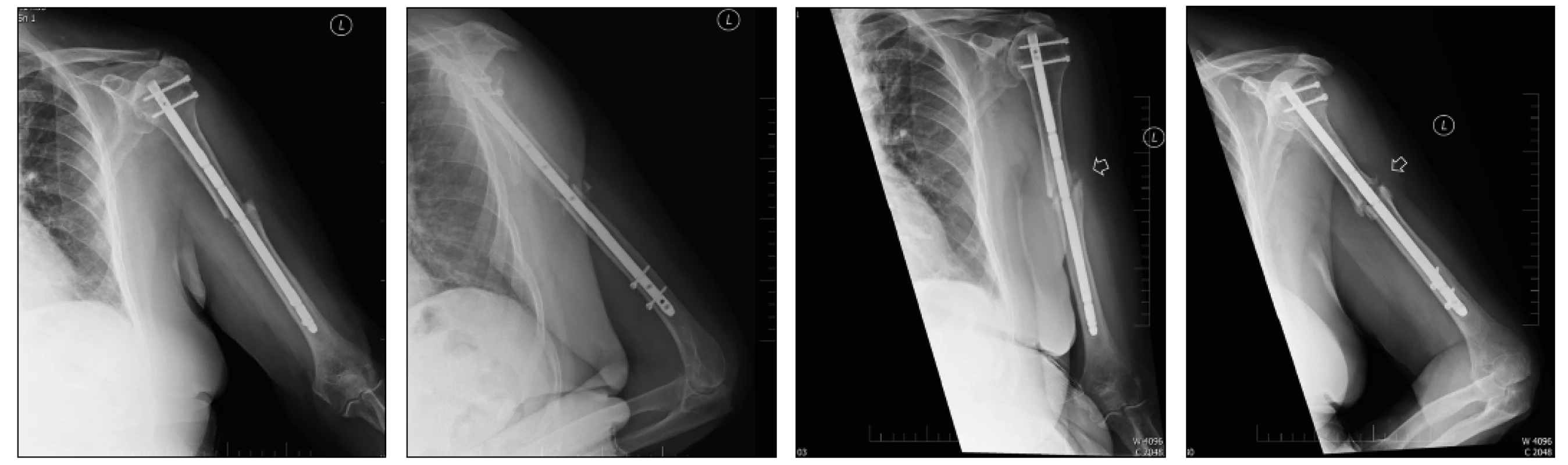
2. Radiograph of the humerus in anteroposterior and lateral projections. Postoperative radiograph (2a) and radiograph taken 9 months after injury (2b) depict a nail osteosynthesis of diaphyseal humeral fracture type A2. Stabilization with auto-compression plate with insufficient compression at the fracture line resulted in a gradual progression into the non-union 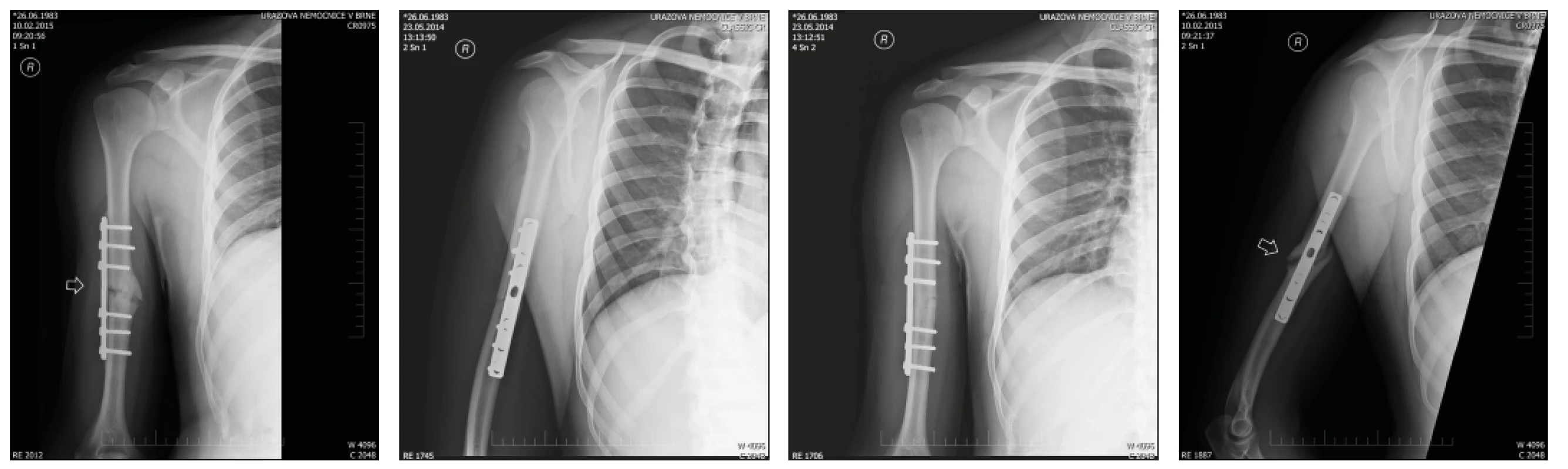
It is also necessary to point out that the average age of our patients was significantly higher than in most of the other studied patient populations (58 vs. 52 years [21], 36 years [20], 34 years [8], 25 years [17]). This fact is also manifested in the composition of the patient group regarding their sex, considering the bimodal distribution mentioned at the introduction of this article – for example in the study performed by Sarmient, male patients prevailed at a ratio of 2 : 1, whereas in our file, female patients prevailed at a rate of approx. 4 : 3 [20]. On the other hand, the average age of patients with non-unions was 66.2 years (median 65.0), which corresponds with the expected trend of impaired healing at an advanced age.
The average interval between the trauma and the surgical procedure among patients with non-unions was 2.6 days (median 1 day). This is a value that corresponds to the treatment standard among patients with this diagnosis, and is shorter when compared with the other presented series [21]. There were 26.3 per cent of smokers in our study group. Declared smokers accounted for 42.1 %, and we were not able to verify the information for the rest of the patients. The most frequent comorbidity was type 2 Diabetes mellitus. The average BMI index of the patients with non-unions was 29.9%, which is a value on the border between being overweight and obese.
The above-presented information show that the profile patient predisposed for the development of a non-union is a female, in her 7th decennium of life, with a fracture type A1 or B1 according to AO classification, located in the middle third of the diaphysis, type 2 Diabetes mellitus, and on the border of obesity. No other of the observed factors has been proven significant. Nevertheless, it remains true that the best prevention against non-union development is a high-quality reduction of the fracture.
It is also worth mentioning the good clinical outcomes in patients with non-unions; the average anteflexion in the shoulder joint during the last follow-up was 141 degrees, and abduction 132 degrees. These are values comparable to a common postoperative condition, according to other studies [12]. This also corresponds with the relatively low number of reoperations in patients with demonstrated non-unions (21.1 %), which directly correlates with the relative subjective satisfaction of these patients. Nine patients (47.4 %) reported intermittent pains during daily activities, only 3 (15.8 %) patients view these pains as strong or restricting. At the same time, we observed 7 (36.8 %) patients who, despite the present non-union, had a full or almost full range of movement during the last follow-up. Considering our empirical experience with earlier or later failure of the implant, we recommend surgical management for all patients with a non-union, i.e. re-osteosynthesis using a plate, with administration of bone grafts. In patients with prolonged healing, decortication and spongioplasty are indicated, in an attempt to support callus formation (Fig. 3).
3. Radiograph of the humerus in anteroposterior and lateral projections, taken postoperatively (3a), 9 months (3b) and 18 months (3c) after injury. The images show a nail osteosynthesis with distal fixation using one screw. No progression of fracture healing is observed 9 months after the procedure. The perfomed decortication and spongioplasty resulted in healing of the fracture 18 months after the initial trauma (3c) 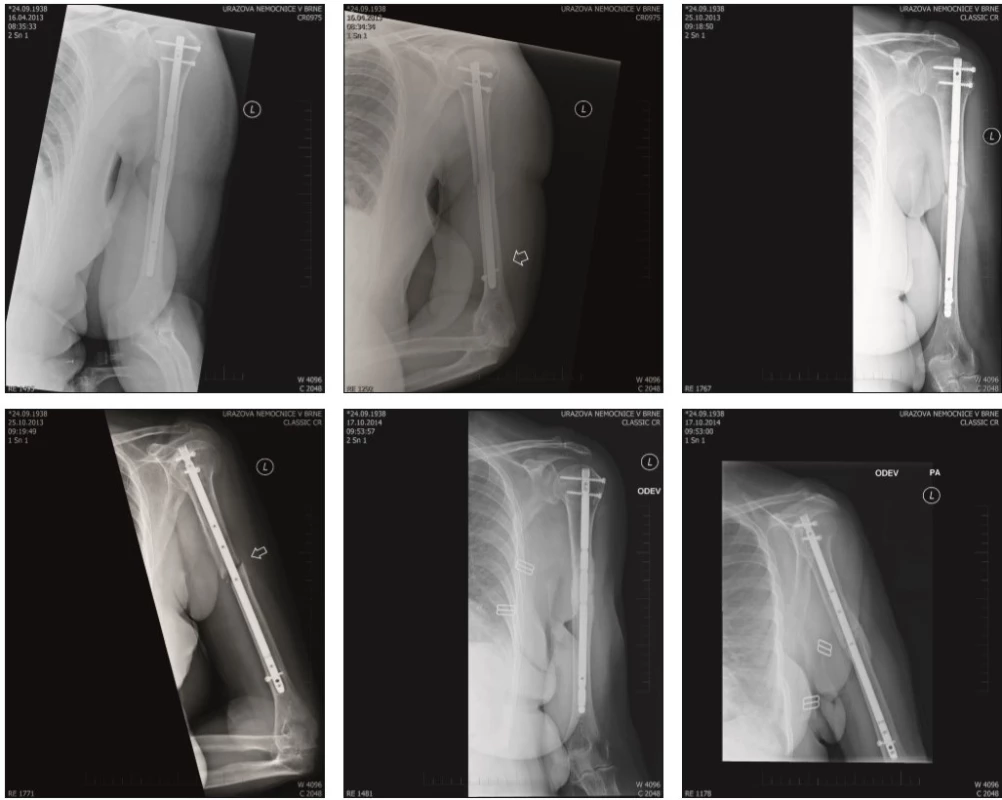
Conclusion
Surgical management of diaphyseal humeral fractures has become a therapeutic standard of today, especially due to the increasing demands for early postoperative physiotherapy and convalescence. Despite the different biomechanical properties of the humerus, when compared with lower extremities, plate osteosynthesis and intramedullary nailing in this locality remain a full-fledged alternative to the conservative approach, provided that the correct surgical technique is applied, using current modern implants.
According to available literature, there exist no significant differences when comparing these techniques, as far at the success-rate of healing is concerned, although our experience indicates a slightly better radiographic results in patients with plate osteosynthesis, and a lower incidence of injuries of n. radialis in patients with nail osteosynthesis.
MUDr. Tomáš Pavlacký
Korespondenční autor :
doc. MUDr. Ján Kočiš, Ph.D.
Úrazová nemocnice v Brně
Klinika traumatologie LF MU Brno
Ponávka 6, 662 50 Brno
email: j.kocis@unbr.cz
Sources
1. ALI, E., GRIFFITHS, D., OBI, N. et al. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg Am. 24, 210–214
2. BOEHLER, L. Against the Operative Treatment of Fresh Humeral Shaft Fractures. Langenbecks Arch. Klin Chir Ver Dtsch Zbl Chir. 1964, 308, 465–475. ISSN 1058-2746
3. DAI, J., CHAI, Y., WANG, C., WEN, G. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures: a meta-analysis of RCTs and nonrandomized studies. J Orthopaed Sci Off J Jpn Orthopaed Assoc. 2014, 19, 282291. ISSN 1435-2451
4. DENARD, A. JR., RICHARDS, EJ., OBREMSKEY, T. et. al. Outcome of Nonoperative vs. Operative Treatment of Humeral Shaft Fractures: A Retrospective Study of 213 Patients. Orthopedics. 2010, 33, 511–515. ISSN 1938-2367
5. DRIESMAN, AS., FISCHER, N., KARIA, R. et al. Fracture Site Mobility at 6 Weeks After Humeral Shaft Fracture Predicts Nonunion Without Surgery. J Orthop Trauma. 2017, 31, 657–662. ISSN 1671-7600
6. GARNAVOS, C. Diaphyseal humeral fractures and intramedullary nailing: Can we improve outcomes? Indian J Orthop. 2011, 45, 208–215. ISSN 0019-5413
7. JIA-GUO ZHAO, JIA WANG, CHEN WANG, SHI-LIAN KAN. Intramedullary Nail Versus Plate Fixation for Humeral Shaft Fractures: A Systematic Review of Overlapping Meta-analyses. Medicine (Baltimore). 2015, 94, e599. ISSN 1536-5964
8. JITENDRA, NP., PRAHAS, B., AVIK, R. et al. Outcome of humeral shaft fractures treated by functional cast brace. Indian J Orthop. 2015, 49, 408–417. ISSN 0019-5413
9. LIU, GD., ZHANG, QG., OU, S. et al. Meta-analysis of the outcomes of intramedullary nailing and plate fixation of humeral shaft fractures. Int J Surg. 2013, 11, 864–868. ISSN 1743-9191
10. MA, J., XING, D., MA, X. et al. Intramedullary nail versus dynamic compression plate fixation in treating humeral shaft fractures: grading the evidence through a meta-analysis. PLoS One. 2013, 8, e82075. ISSN 1932-6203
11. MAST, JW., SPIEGEL, PG., HARVEY, JP. J. et al. Fractures of the humeral shaft: a retrospective study of 240 adult fractures. Clin Orthop Relat Res. 1975, 112, 254–262. ISSN 1528-1132
12. METSEMAKERS, WJ., WIJNEN, V., SERMON, A. et al. Intramedullary nailing of humeral shaft fractures: failure analysis of a single centre series. Orthop Trauma Surg. 2015, 135, 1391. ISSN 1434-3916
13. MULLER, ME., NAZARIAN, S., KOCH, P. et al. The comprehensive classification of fractures of long bones. New York : Springer – Verlag , 1999. 202 s. ISBN 3540181652
14. OBRUBA, P., KOPP, L., EDELMANN, K. Léčba zlomenin diafýzy humeru nitrodřeňovou fixací svazkem hřebů dle Hackethala. Acta Chirurgiae Orthopaedicae et Traumatologiae Čechosl. 2012, 79, 341–346. ISSN 0001-5415
15. OUYANG, H., XIONG, J., XIANG, P. et al. Plate versus intramedullary nail fixation in the treatment of humeral shaft fractures: an updated meta-analysis. J Shoulder Elbow Surg Am Shoulder Elbow Surg. 2013, 22, 387–395. ISSN 1058-2746
16. PAPASOULIS, E., DROSOS, GI., VERVERIDIS, AN. et al. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury. 2010, 41, 21–27. ISSN 0020-1383
17. PEHLIVAN, O. Functional treatment of the distal third humeral shaft fractures. Arch Orthop Trauma Surg. 2002, 122, 390–395. ISSN 1434-3916
18. ROBINSON, CM., BELL, KM., COURT-BROWN, CM. et al. Locked nailing of humeral shaft fractures. J Bone Joint Surg Br. 1992, 74, 558–562. ISSN 0301-620X
19. RUTGERS, M., RING, D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma. 2006, 20, 597-601. ISSN 1531-2291
20. SARMIENTO, A., KINMAN, PB., GALVIN, EG. et al. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977, 59, 596–601. ISSN 1531-2291
21. ŠMEJKAL, K., LOCHMAN, P., DĚDEK, T. et al. Operační léčba zlomenin diafýzy humeru. Acta Chirurgiae Orthopaedicae et Traumatologiae Čechosl. 2014, 81, 129–134. ISSN 0001-5415
22. TOIVANEN, JAK., NIEMINEN, J., LAINE, HJ. et al. Functional treatment of closed humeral shaft fractures. International Orthopaedics. 2005, 29, 10–13. ISSN 1432-5195
23. TYTHERLEIGH-STRONG, G., WALLS, N., MCQUEEN, MM. The epidemiology of humeral shaft fractures. J Bone Joint Surg Br. 1998, 80, 249–253. ISSN 0301-620X
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2018 Issue 1
Most read in this issue- Surgical treatment of diaphyseal humeral fractures
- Developmental morphology of the elbow joint in relation to injuries of the paediatric skeleton
- Post-traumatic peritonitis
- Arthroscopy-assisted osteosynthesis of triplane fracture – case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career