-
Medical journals
- Career
Post-traumatic peritonitis
Authors: Jan Ulrych 1; Miroslav Zeman 1; MUDr. Václava Adámková, Ph.D. 2
Authors‘ workplace: 1. chirurgická klinika – klinika břišní, hrudní a úrazové chirurgie, 1. lékařská fakulta Univerzity Karlovy a Všeobecná fakultní nemocnice v Praze 1; Klinická mikrobiologie a ATB centrum, Ústav lékařské biochemie a laboratorní diagnostiky, 1. lékařská fakulta Univerzity Karlovy a Všeobecné fakultní nemocnice v Praze 2
Published in: Úraz chir. 26., 2018, č.1
Overview
Post-traumatic peritonitis is an intra-abdominal infection caused by hollow viscus injury and leak of intraluminal content into the peritoneal cavity. Early recognition of abdominal hollow viscus injury may be difficult, due to the non-specific clinical symptoms and limitations of the imaging investigations. In the diagnosis of hollow viscus injury, the ultrasonography (US) is associated with a very low sensitivity (38 %) and it is highly expert-dependent examination as well. Computed tomography (CT) has a high sensitivity (86–95 %) and a good specificity (73–88 %), however, this diagnostic modality may be used only in the assessment of hemodynamically stable patients. Symptoms of peritonitis in trauma patients may occur because hollow viscus injuries can be missed in initial radiologic imaging. In case of mesenteric trauma or mural hematoma, subsequent ischaemia of bowel may take time to develope and secondary intestinal perforation leads in late manifestation of peritonitis. Moreover, clinical symptomatology of post-traumatic peritonitis is often modified by the trauma itself (multiple injuries, disturbances of consciousness in brain trauma, intoxication), and subsequent treatment (administration of analgesics, surgical procedure). Selective non-operative management of abdominal trauma further accented the importance of repeated clinical examination and observation, with a special focus on the clinical manifestations of peritonitis. Decision-making related to selective non-operative management of abdominal trauma requires erudite surgeons and an accurate knowledge of post-traumatic peritonitis. The principles of treatment of post-traumatic peritonitis include surgery (surgical repair of the injured organ and the contaminated peritoneal cavity) and systemic antibiotic therapy. Delay in diagnosis and treatment is associated with an increased morbidity and mortality. Therefore, the authors have decided to present this summary overview dealing with post-traumatic peritonitis, summarising the current knowledge on this topic.
Keywords:
diagnosis – Post-traumatic peritonitis – abdominal hollow viscus injury – surgery
Characteristics of post-traumatic peritonitis
Post-traumatic peritonitis is classified as a secondary peritonitis. It is an intra-abdominal infection caused by hollow viscus injury with transmural perforation (gastrointestinal tract, bile ducts, urinary bladder). This abdominal trauma results in a leak of the intraluminal contents and contamination of the peritoneal cavity. Depending on the size of wall perforation, and the amount and character of intraluminal contents leaking to peritoneal cavity, diffuse peritonitis with sepsis and septic shock is developed. Early recognition of hallow viscus injury facilitates surgical source control including repair of injured abdominal organ and intra-abdominal lavage et drainage. Early surgery may prevent further development of diffuse peritonitis and abdominal sepsis. Post-traumatic peritonitis is also characterized by a number of factors, which may alter clinical symptomatology. The most frequent factors are simultaneous trauma of hollow and parenchymal abdominal organs, post-traumatic analgesic therapy or an extra-abdominal injury. The difference between post-traumatic peritonitis and other types of secondary peritonitis may be explained by a different aetiology (trauma mechanism), modification of clinical symptomatology by the injury itself, and a specificity in diagnosis and treatment.
Mechanism of abdominal hollow viscus injury
Penetrating abdominal injuries may be caused by two different trauma mechanisms – stab wounds (SWs) and gunshot wounds (GSWs). Stab wounds represent a direct injury with significantly less kinetic energy. Sharp objects (often knife) may result in trauma of several abdominal organs, moreover, multiple injuries of single abdominal organ (particularly small intestine) are frequent. It is important to recognize the importance of two mechanisms of GSWs (projectile injury and splinter injury) and the velocity of the agent. Depending on the trajectory, the projectile may induce a direct injury, with perforation of an abdominal hollow viscus. High-velocity bullets (over 340 m/s) ussually result in a damage of abdominal organs due to the associated shock wave and cavitation effect. The penetrating projectile causes a temporary negative pressure in the abdominal cavity leading to a rapid increase in the volume of intestinal gasses. It results in seromuscular tears or even rupture of the intestine, often multiple perforation of the bowel. Also, the mesentery is usually damaged in this way. In case of blunt abdominal injuries, it is possible to distinguish among three different trauma mechanisms leading to injuries of abdominal hollow viscus – compression, expansion and deceleration. In the compression mechanism, kinetic energy causes serous or seromuscular tears in the wall of the hollow viscera, or even in a full-thickness perforation of the wall. If the serosa remains intact, tissue laceration of the visceral wall leads to the progression in an intramural haematoma. The pressure of intramural haematoma results in ischemia and necrosis of the wall, a secondary perforation of the bowel may develope subsequently. Late complication of bowel ischemia is a segmental stenosis of intestine. In an enclosed compartment (rotated bowel loop, filled urinary bladder), external compression results in a sudden increase of intraluminal pressure and wall rupture. Injuries caused by expansion may be observed in the large bowel particularly (insertion of tube into the anus). Insuflation of gas or liquid leads to an increase of the intraluminal pressure, associated with an increased pressure. Tears and perforations appear when the elasticity of the hollow viscus wall is exceeded. In the deceleration trauma mechanism, shear forces are applied on tissues. The extent of tissue damage depends on the strength of the shear forces and rigidity/elasticity of tissue. Deceleration mechanism mostly results in tears, lacerations and complete avulsion of the mesentery. It is typically happened where mobile and fixed segments of bowel are attached and are vulnerable to shear force injury. These mesenteric injuries may be associated with immediate haemorrhage or may cause a devascularisation of a segment of intestine, with subsequent ischemia and secondary bowel perforation. However, a combination of all previous mechanisms is also frequently observed.
Epidemiology
Penetrating abdominal injuries are less frequent in the area out of the military conflict. Most of the victims are young and middle-aged people with the majority of being young men [30]. SWs account for most of the penetrating abdominal injuries (95–97 %). SWs are often associated with criminality and it is a result of homicidal intent. GWs are unusual in Europe. Based on the data, approximatelly 50–75 % of SWs penetrate in the peritoneal cavity – penetrating abdominal injuries [6]. Penetrating abdominal injuries are associated with an increased risk of trauma of abdominal organs including hollow viscus injury. Regardless of the type of sharp object causing the trauma, the abdominal organ most commonly injured is the small bowel accounting 49 to 60% of all injuries [30]. Blunt abdominal trauma is more common in civil life. These injuries may be caused by road traffic accident (75–80%), falls from height and sport-related injuries. Hollow viscus injury in blunt abdominal trauma is a rare occurrence (7.5–15%) [10, 16]. Nevertheless, specific mechanisms of injury, such as seatbelt injuries in victims of road traffic accidents, should keep a suspicion of an increased risk of intestinal injury [27]. Solitary hollow viscus injury ranges 31–62% [10, 21]. However, hollow viscus injury is often associated with a trauma of parenchymal organs – spleen trauma (20–25%), liver trauma (14–29%), and kidney injuries (13%). Moreover, simultaneous extra-abdominal trauma is common – limb injuries (72%), head injuries (31–42%) and thoracic trauma (27–45%) [13].
Clinical symptomatology
The objective of the initial clinical assessment in patient with abdominal injury is to assess the risk of abdominal organ injuries, assess the haemodynamic stability and search for any symptoms of peritonitis. Especially in patients with history of high-energy trauma, it is necessary to keep in mind the possibility of abdominal hollow viscus injury. Abrasions and bruises caused with the seat belt may point towards possible injuries of the intestines and the mesentery [27]. In patients with SWs and GWs, it is necessary to explore the assumed trajectory of the injuring object. Surgical exploration of the wound is performed in order to assess the risk of the penetrating character of the injury (surgical wound exploration is unnecessary in the case of evisceration) [6]. Abdominal organs may be injured also in patients with wound accidents in the thoraco-lumbar and gluteal body region. In the course of the initial clinical examination, it is necessary to assess the haemodynamic stability and vital signs of the patients – consciousness, blood pressure and pulse, respiratory rate and oxygen saturation. Clinical examination is also focused on the symptoms of acute peritonitis. Repeated clinical assessment of the abdomen is crucial in patients with abdominal trauma indicated for selective non-operative management. The clinical manifestations of peritonitis may appear early after the injury, or the clinical symptomatology may be manifested with a delay, due to a secondary ischemic perforation of the intestine. Abdominal pain, initially localised, soon becomes diffuse and symptoms of peritoneal irritation appear. The patient suffers from nausea and vomiting, distension of the abdomen is clearly apparent, together with obstipation. The progression of clinical symptomatology of acute peritonitis depends on the volume and character of the contents leaking into the peritoneal cavity (gastric juice and intestinal contents, bile, urine), on the size of perforation, bacterial load and virulence of the bacteria. The clinical manifestations of post-traumatic peritonitis may be modified by the trauma itself and its treatment. Simultaneous abdominal wall contusion may be associated with pain, therefore to recognize developing acute peritonitis can be a clinical challange. The required post-traumatic analgesic treatment may initially hide the symptoms of acute peritonitis. More serious extra-abdominal injuries, especially severe craniocerebral trauma with disturbance of consciousness, make valid clinical assessment impossible.
Laboratory tests
Laboratory inflammatory markers are a standard part of laboratory testing in patients with suspected post-traumatic peritonitis. The most common inflammatory biomarker is white blood cells count. In trauma patients, the sensitivity and specificity of this marker are rather low, nevertheless, this biomarker is available and relatively cheap. White blood cells count is useful for monitoring of inflammation dynamics. Another inflammatory marker is the C-reactive protein (CRP), the values of CRP become significantly elevated even in cases of non-infectious activation of the systemic inflammatory response (SIRS). On the basis of CRP values, it is challange to distinguish whether the patient suffers from a post-traumatic SIRS or early acute peritonitis. Procalcitonin (PCT) is the most frequently used biomarker for the diagnosis of sepsis. The production of PCT in the course of inflammation depends upon the volume of released bacterial endotoxin. However, PCT levels are elevated also after an extensive surgical procedure, or a severe trauma; in these circumstances, the PCT levels usually do not exceed 5 μg/l and drop rapidly [33, 35]. PCT has a high sensitivity (88 % vs. 75 %) and specificity (81 % vs. 67 %) for distinguishing between an infectious and non-infectious systemic inflammation when compared with CRP [31, 36].
Imaging examination
The basic imaging examinations in patients with abdominal trauma include native roentgenogram of the abdomen, abdominal ultrasound (US) and computed tomography (CT). The contribution of native abdominal roentgenogram is marginal. A finding of pneumoperitoneum is direct indication for surgery, however abdominal roentgenogram is not useful imaging investigation for identification of injured abdominal organ and diagnosis of extra-abdominal trauma. Patient´s status and haemodynamic stability plays an important role in the dicision-making related to imaging examinations. In haemodynamically unstable patients, focused abdominal ultrasonography examination for trauma (FAST) is recommended. FAST may be performed at the patient’s bedside during the primary initial assessment in emergency department without a risk of delay because patients transport is not necessary. Generally, FAST is used for detection free peritoneal fluid and solid organ injury in abdominal cavity; nevertheless, FAST is not helpful in diagnosis of hollow viscus injury and it can be quite misleading [22]. In the blunt abdominal trauma, FAST has the sensitivity of 71 % and specificity of 35 % for abdominal organ injury, in detection of bowel trauma and mesenteric injuries the sensitivity of FAST drops down to only 38 % [21, 22]. In the abdominal SWs, US has also low sensitivity for abdominal organ injury with a wide variance (28–100 %) [28]. FAST is a highly expert-dependent examination, and negative findings during the initial US assessment do not reliably rule out an abdominal trauma. CT is the imaging modality of choice in case of haemodynamically stable patients with abdominal injuries. Contrast-enhanced CT may be considered the most reliable imaging examination (accurency 73–99 %) in the diagnosis of abdominal organ injuries [14, 24, 34]. In patients with blunt abdominal trauma including bowel trauma and mesenteric injuries, CT has a high sensitivity (86–95 %) but the specificity is lower (73–88 %) [2, 15, 34]. CT is strongly recommended as a diagnostic modality to facilitate management decisions in patients with abdominal trauma [32]. CT may be inaccurate in the evaluation of bowel trauma and mesenteric injury and diagnosis often relies on secondary rather than organ-specific symptoms. Moreover, radiology evaluation of the extent of abdominal trauma is often embarrassed with simultaneous injury of solid organs. The limitations of imaging examinations and modification of the clinical symptomatology (due to multiple injuries) are the reason why the abdominal hollow viscus injuries belong among the most frequently unrecognized abdominal injuries in patients with blunt trauma [11, 25]. CT may show organ-specific symptoms (discontinuity of the gastric and bowel wall, thickening and changes in wall density, leak of contrast agent administered per os, infiltration of the mesenteric fat, mesenteric haematoma, etc.) and non-specific symptoms (pneumoperitoneum, free fluid in the abdominal cavity without any symptoms of solid organ injury). False negative CT was reported in up to 8.7 % of abdominal trauma patients and injuries of small bowel were the most frequent unrecognized abdominal trauma (47 %) [4]. In patients with SWs, CT is still a matter of debate, however, many experts advocate for CT scanning in the evaluation of patients with penetrating abdominal trauma. On the other hand, in stable patients with penetrating SWs the non-operative management and serial physical examination is recommended regardless negative CT.
Impact of diagnostic laparoscopy
The laparoscopy plays a crucial role in diagnosis of penetrating abdominal injuries. Diagnostic laparoscopy may be applied as a tool to avoid unnecessary laparotomy. Decreased number of explorative laparotomies by up to 52 % was reported [23]. Despite the technically more difficult laparoscopic exploration of the abdominal cavity (intraoperative exploration of the posterior gastric wall and retroperitoneal duodenum), up to 92 % of abdominal injuries may be treated with laparoscopy [18].
Therapy
The principle of treatment of post-traumatic peritonitis is based on three cornerstones – surgical management, systemic antibiotic therapy and intensive care in ICU. The objective of surgical management is the source control (repair of injured hollow viscus), prevent further contamination of the peritoneal cavity, and lavage and drainage of the peritoneal cavity. The objective of antibiotic therapy is to prevent further spreading of infection and to decrease the risk of postoperative abdominal abscesses. Intensive care, including a patient´s monitoring and support of vital functions, is crucial for patients whith more severe trauma. Post-traumatic peritonitis is a complication of perforating injury of abdominal hollow organs, and the character of abdominal trauma determine the further therapy. The basic difference is in the therapy management of the patients with a serious polytrauma and devastating abdominal injuries, and in the therapy management of the patients with an isolated abdominal trauma.
Polytrauma. Critically ill patients with devastating abdominal injuries are threatened especially by life-threatening haemorrhage associated with development of the lethal triad (acidosis, hypothermia and coagulopathy). The surgical management of these patients is based on the principles of Damage Control Surgery [17]. Damage Control Surgery is a staged surgical treatment of patients, whose critical status does not allow immediate more complex surgical procedures. Only simple surgical procedures are performed during emergency laparotomy, including haemostasis and controlling abdominal contamination from injured hollow organs, to rapidly stabilize the patient’s physiological functions [17, 20]. More complex surgery and definite anatomical reconstructions are performed only after 24–36 hours, when the physiological derangement has been corrected and the patient´s status has been stabilized. The source of haemorrhage may be treated finally (ligation of a blood vessel, splenectomy, renal resection), or temporarily (hepatic tamponade). In the damage control setting the objective is to simply prevent continued leak and abdominal contamination. Simple hollow viscus injuries may be treated with a primary suture of small perforations, intestine resection using staplers is recommended in cases of more extensive bowel trauma, leaving the intestine in discontinuity or performing quickly a stoma. Injury of bile ducts and the pancreas may be initially managed with an external drainage and formation of a so-called controlled fistula. Injuries of the urinary bladder are usually treated with suture and insertion of a permanent urinary catheter for derivation of urine. In the explorative laparotomy fascial closure of the abdominal cavity is not recommended, due to the high risk of abdominal compartment syndrome. Increase of intra-abdominal pressure is caused be reperfusion and continuous capillary leak, leading to oedema of the bowel, abdominal wall and the retroperitoneum. Laparostomy and the temporary closure of the abdominal cavity is the treatment of choice, with the most common technique being a negative-vacuum type device [8]. Temporary abdominal closure facilitates a rapid access to the abdominal cavity, and it also prevents complications that can result from having an open abdomen (enteral fistulas and lateralization of the abdominal fascia). Surgery and definitive anatomic reconstruction are performed only when the patient´s status is improving. In cases of abdominal hollow viscus injury, re-exploration of the abdomen allows to identify potentially missed injuries during the initial explorative laparotomy and perform definitive repair (bowel anastomosis).
Isolated abdominal injury. Over the past century, routine explorative laparotomy was mandatory for all patients with SWs of the abdomen. Surgical management ensures early identification of hollow viscus injury and surgical repair of injured organs may prevent from intra-abdominal infection – post-traumatic peritonitis. Routine explorative laparotomies result in a non-therapeutic laparotomy rate of 23–53 %, moreover, non-therapeutic laparotomies are associated with increased risk of postopertavive morbidity (2,5–41 %), prolonged length of hospital stay and high financial cost [6, 9]. The desire to avoid non-therapeutic laparotomy the concept of non-operative management in selected patients with penetrating abdominal wounds was introduced. There is uniform agreement that immediate explorative laparotomy is warranted for patients with hemodynamic compromise, acute peritonitis or evisceration. Also, surgical exploration should be considered if the valid physical examination cannot be performed (alteration of consciousness, intoxication, other extra-abdominal injuries requiring a surgical procedure). Selective non-operative management of abdominal SWs has become accepted for asymptomatic hemodynamicly stable patients with negative CT. The required observation period is 24–48 hours because the most perforating hollow viscus injuries become clinically apperent within 12 hours [1]. Delayed laparotomy is indicated in case of worsening patient´s status or manifestation symptoms of peritonitis. Reported morbidity and mortality of delayed laparotomy is not exceded compared to results of primary explorative laparotomy [5]. It should be mentioned that selective non-operative management is associated with significant risk of incorrect interpretation of clinical symptoms and it may delay the surgery. Therefore, high erudition of physicians and repeat physical examination is required. In cases of abdominal GWs, the risk of abdominal hollow viscus injury is quite high. If the projectile penetrates in the peritoneal cavity, the incidence of non-therapeutic laparotomy reaches only 2–4% [3]. Explorative laparotomy is a preferred approach in all abdominal GWs, with the exception of tangential extraperitoneal trajectory of wound verified on CT. In cases of blunt abdominal trauma, the treatment management is based on patient´s status, haemodynamic stability and CT. Primary explorative laparotomy is indicated for haemodynamically unstable patients and patients with symptoms of peritonitis. In blunt abdominal trauma CT is used for diagnosis of injury and dicision to non-operative management or surgery, particularly in solid organ injury. The use of CT scans in the diagnosis of hollow viscus injury is widespread. However, CT is not always a reliable radiologic method for the prediction of hollow viscus injury requiring surgery. Strong critera for surgery are CT-verified pneumoperitoneum and discontinuity of intestinal wall. On the other hand, initial radiologic finding of intestine wall haematoma or mesenteric infiltration justify primary non-operative management; nevertheless, it is very difficult to predict further progression and the risk of secondary bowel perforation. Non-operative management of patients with blunt abdominal trauma requires careful clinical observation. Early identification of peritonitis and adequate treatment including surgery is crucial, delay of surgical therapy is associated with increasing mortality [12, 19].
Surgical treatment. The type of surgery and repair of injured organ is determined by location and size of perforation, vitality of injured organ, contamination of peritoneal cavity and duration of peritonitis. In early recognition of limited hollow viscus injury (small perforation, minor contamination of peritoneal cavity) immediate roconstructive surgery may be considered (Tab. 1). The most frequently performed surgical procedure is a primary suture of the perforation, or resection of the injured organ and primary anastomosis [29]. Borderline vitality of the injured organ and diffuse peritonitis are contraindications for primary reconstructive surgery. Derivation of the intraluminal content using a stoma is recommended in extensive trauma and diffuse contamination of peritoneal cavity [29]. The definitive reconstructive procedure should be performed with a delay, after the peritonitis has been sustained (Tab. 1). Surgical therapy of contaminated abdominal cavity includes drainage of pathologic content and lavage of peritoneal cavity. The objective of this procedure is bacteria load reduction in peritoneal cavity.
1. Choice of surgical procedure depending on the localization and extent of the injury. 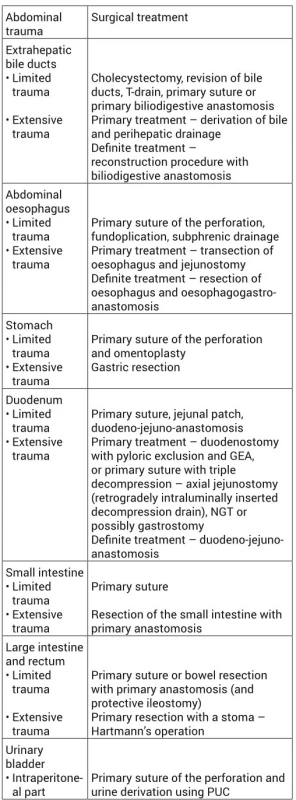
GEA – gastro-entero-anastomosis; NGT – nasogastric tube; PUC – permanent urinary catheter. Antibiotic therapy. Antibiotic therapy plays a crucial role in the treatment of patients with post-traumatic peritonitis. In patients with penetrating abdominal trauma antibiotic administration is fully accepted, although the reduction of the risk of surgical site infection has not been validated by any randomized study [7]. There is strong recommedation for systemic antibiotic therapy in patients with post-traumatic peritonitis. However, the length of the antibiotic administration remains the matter of discussion. Only 24-hours antibiotic administration is recommended for patients with minor organ injury, limited contamination of the peritoneal cavity, and surgical treatment within 6-12 hours of injury [26]. Several days antibiotic therapy is justified for patients with extensive injury, diffuse peritonitis and delayed surgery. Empiric antibiotic therapy should be based on the knowledge of the microbial flora colonizing the injured organ. Also, regional epidemiology and incidence of antibiotic resitant bacteria in community play an important role in choice of appropriate antibiotic regimen. Recommendation for the choice of antibiotics for post-traumatic peritonitis is summarized in Tab. 2. The failure of antibiotic therapy can be caused by inadequate antibiotic administration, most frequently due to underdosing of antibiotics. The chart of the most common antibiotics including antibiotic dosing is shown in Tab. 3.
2. Recommended ATB treatment of post-traumatic peritonitis, depending on the localization of the injury 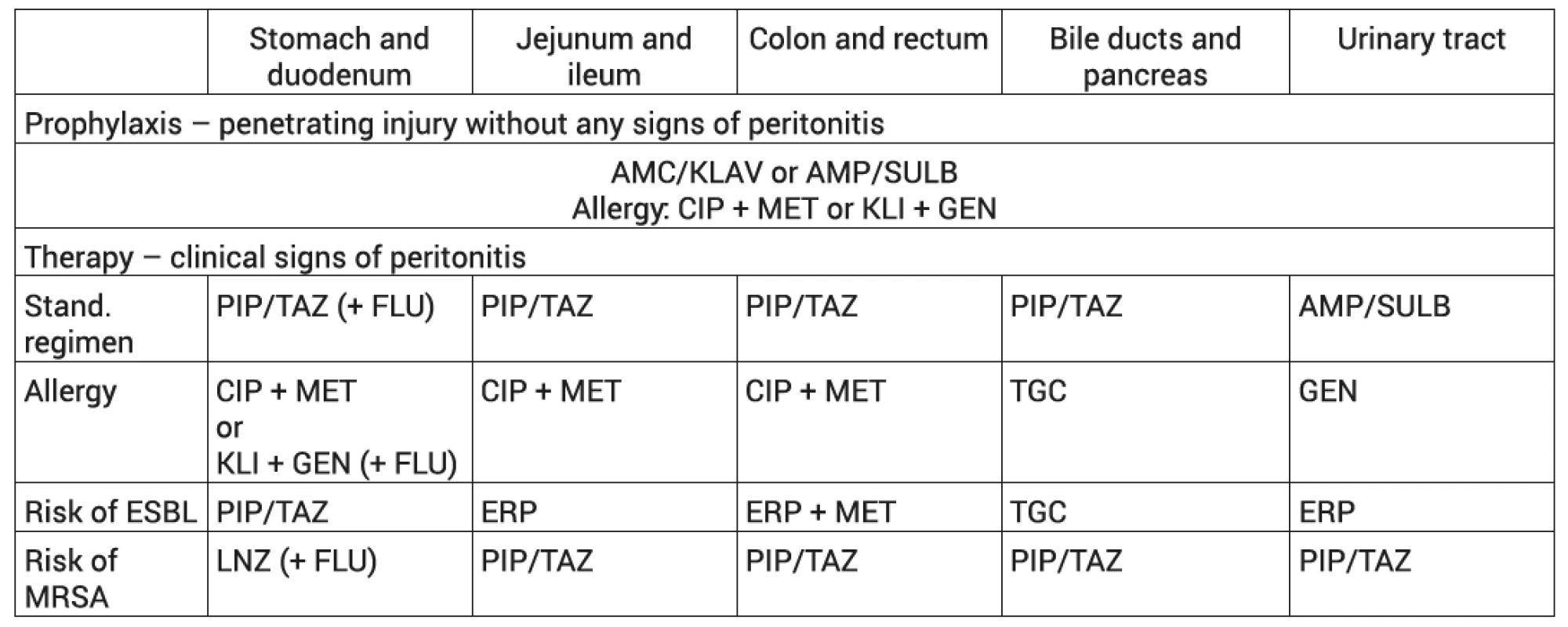
AMC/KLAV - Amoxicilin/ clavulanic acid; AMP/SULB - Ampicilin/Sulbactam; CIP - ciprofloxacin; ERP - Ertapenem; ESBL - producers of extended spectrum beta-lactamases; FLU - Fluconazole; GEN - Gentamicin; KLI - Clindamycin; LNZ - Linezolid; MET - Metronidazole; MRSA - methicilin resistant Staphylococcus aureus; PIP/TAZ - Piperacillin/ tazobactam; TGC - Tigecycline 3. Antibiotics and antibiotic dosing. 
LD - initial dose. Summary
Post-traumatic peritonitis is associated with significantly unfavourable prognosis in patients with abdominal trauma. Early recognition of hollow viscus injury allows immediate surgical repair. Rapid surgical source control prevents continued contamination of peritoneal cavity and development of diffuse peritonitis. The symptoms of acute peritonitis may be manifested with a delay, due to a misdiagnosed hollow viscus injury or due to a secondary ischemic perforation of the intestine. The clinical symptomatology of post-traumatic peritonitis is often modified by the trauma itself, causing the making correct diagnosis of hollow viscus injury more difficult. The principle of treatment is surgical repair of injured abdominal organ and control of contaminated peritoneal cavity. Antibiotic therapy plays crucial role in the treatment of post-traumatic peritonitis, as well.
MUDr. Jan Ulrych, Ph.D.
Sources
- ALZAMEL, HA., COHN, SM. When is it safe to discharge asymptomatic patients with abdominal stab wounds? J Trauma. 2005, 58, 523–525. ISSN 0022-5282
- ATRI, M., HANSON, JM., GRINBLAT, L. et al. Surgically important bowel and/or mesenteric injury in blunt trauma: accuracy of multidetector CT for evaluation. Radiology. 2008, 249, 524–533. ISSN 0033-8419
- BALL, CG. Current management of penetrating torso trauma: nontherapeutic is not good enough anymore. Can J Surg. 2014, 57, E36–43. ISSN 0008-428X
- BARON, BJ., BENABBAS, R., KOHLER, C. et al. Accuracy of Computed Tomography in Diagnosis of Intra-abdominal Injuries in Stable Patients With Anterior Abdominal Stab Wounds: A Systematic Review and Meta-analysis. Acad Emerg Med. 2018, 25, 744–757. ISSN 1553-2712
- BIFFL, WL., KAUPS, KL., PHAM, TN. et al. Validating the Western Trauma Association algorithm for managing patients with anterior abdominal stab wounds: a Western Trauma Association multicenter trial. J Trauma. 2011, 71, 1494–1502. ISSN 0022-5282
- BIFFL, WL., LEPPANIEMI, A. Management guidelines for penetrating abdominal trauma. World J Surg. 2015, 39, 1373–1380. ISSN 1432-2323
- BRAND, M., GRIEVE, A. Prophylactic antibiotics for penetrating abdominal trauma. Cochrane Database Syst Rev. 2013, 18, CD007370. ISSN 1469-493X
- COCCOLINI, F., ROBERTS, D., ANSALONI, L. et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg. 2018, 13, 7. ISSN 1749-7922
- COMO, JJ., BOKHARI, F., CHIU, WC. et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010, 68, 721–733. ISSN 0022-5282
- COSTA, G., FRANSVEA, P., FREZZA, B. et al. Hollow viscus injury due to blunt trauma. Epidemiology and outcome in a large urban area. Ann Ital Chir. 2016, 87, 230–236. ISSN 2239-253X
- EKEH, AP., SAXE, J., WALUSIMBI, M. et al. Diagnosis of blunt intestinal and mesenteric injury in the era of multidetector CT technology-are results better? J Trauma. 2008, 65, 354–359. ISSN 0022-5282
- FARIA, GR., ALMEIDA, AB., MOREIRA, H. et al. Prognostic factors for traumatic bowel injuries: killing time. World J Surg. 2012, 36, 807–812. ISSN 1432-2323
- HARMSTON, C., WARD, JBM., PATEL, A. Clinical outcomes and effect of delayed intervention in patients with hollow viscus injury due to blunt abdominal trauma: a systematic review. Eur J Trauma Emerg Surg. 2018, 44, 369–376. ISSN 1863-9933
- IASELLI, F., MAZZEI, MA., FIRETTO, C. et al. Bowel and mesenteric injuries from blunt abdominal trauma: a review. Radiol Med. 2015, 120, 21–32. ISSN 1826-6983
- JOSEPH, DK., KUNC, A., KINLER, RL. et al. Diagnosing blunt hollow viscus injury: is computed tomography the answer? Am J Surg. 2013, 205, 414–418. ISSN 0002-9610
- KURANE, SB., UGANE, SP. A clinical study of hollow viscus injury due to blunt trauma abdomen. Int J Res Med Sci. 2017, 5, 5017–5020. ISSN 2320-6071
- LAMB, CM., MACGOEY, P., NAVARRO, AP. et al. Damage control surgery in the era of damage control resuscitation. Br J Anaesth. 2014, 113, 242–249. ISSN 0007-0912
- LIN, HF., CHEN, YD., CHEN, SC. Value of diagnostic and therapeutic laparoscopy for patients with blunt abdominal trauma: A 10-year medical center experience. PLoS One. 2018, 13, e0193379. ISSN 1932-6203
- MALINOSKI, DJ., PATEL, MS., YAKAR, DO. et al. A diagnostic delay of 5 hours increases the risk of death after blunt hollow viscus injury. J Trauma. 2010, 69, 84–87. ISSN 0022-5282
- MICHEK, J., PLEVA, L., WENDSCHE, P. Poranění orgánů dutiny břišní a retroperitonea. Ostrava: Česká společnost pro úrazovou chirurgii, 2001. Úrazová chirurgie. ISSN 1211-7080.
- MOHAMMADI, A., GHASEMI-RAD, M. Evaluation of gastrointestinal injury in blunt abdominal trauma „FAST is not reliable“: the role of repeated ultrasonography. World J Emerg Surg. 2012, 7, 2. ISSN 1749-7922
- NNAMONU, MI., IHEZUE, CH., SULE, AZ. et al. Diagnostic value of abdominal ultrasonography in patients with blunt abdominal trauma. Niger J Surg. 2013, 19, 73–78. ISSN 0974-2700
- O´MALLEY, E., BOYLE, E., O´CALLAGHAN, A. et al. Role of laparoscopy in penetrating abdominal trauma: a systematic review. World J Surg. 2013, 37, 113–122. ISSN 1432-2323
- PAL, JD., VICTORINO, GP. Defining the role of computed tomography in blunt abdominal trauma: use in the hemodynamically stable patient with a depressed level of consciousness. Arch Surg. 2002, 137, 1029–1032. ISSN 0004-0010
- PATEL, S., KOTO, ZM., BALABYEKI, M. The role of CT scan in penetrating abdominal trauma. S Afr J Surg. 2017, 55, 63. ISSN 0038-2361
- POOLE, D., CHIEREGATO, A., LANGER, M. et al. Systematic review of the literature and evidence-based recommendations for antibiotic prophylaxis in trauma: results from an Italian consensus of experts. PLoS One. 2014, 9, e113676. ISSN 1932-6203
- POPLIN, GS., MCMURRY, TL., FORMAN, JL. et al. Nature and etiology of hollow-organ abdominal injuries in frontal crashes. Accid Anal Prev. 2015, 78, 51–57. ISSN 0001-4575
- QUINN, AC., SINERT, R. What is the utility of the Focused Assessment with Sonography in Trauma (FAST) exam in penetrating torso trauma? Injury. 2011, 42, 482–487. ISSN 0020-1383
- SARTELLI, M., CHICHOM-MEFIRE, A., LABRICCIOSA, FM. et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017, 12, 29. ISSN 1749–7922
- SIDDHARTH, BR., KEERTHI, MSS., NAIDU, SB. et al. Penetrating Injuries to the Abdomen: a Single Institutional Experience with Review of Literature. Indian J Surg. 2017, 79, 196–200. ISSN 0972-2068
- SIMON, L., GAUVIN, F., AMRE, DK. et al. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004, 39, 206–217. ISSN 1058-4838
- SOTO, JA., ANDERSON, SW. Multidetector CT of blunt abdominal trauma. Radiology. 2012, 265, 678–693. ISSN 0033-8419
- SPOTO, S., VALERIANI, E., CAPUTO, D. et al. The role of procalcitonin in the diagnosis of bacterial infection after major abdominal surgery: Advantage from daily measurement. Medicine (Baltimore). 2018, 97, e9496. ISSN 0025-7974
- STEENBURG, SD., PETERSEN, MJ., SHEN, C. et al. Multi-detector CT of blunt mesenteric injuries: usefulness of imaging findings for predicting surgically significant bowel injuries. Abdom Imaging. 2015, 40, 1026–1033. ISSN 2366-0058
- WOJTASZEK, M., STAŚKIEWICZ, G., TORRES, K. et al. Changes of procalcitonin level in multiple trauma patients. Anaesthesiol Intensive Ther. 2014, 46, 78–82. ISSN 1731-2515
- YANG, SK., XIAO, L., ZHANG, H. et al. Significance of serum procalcitonin as biomarker for detection of bacterial peritonitis: a systematic review and meta-analysis. BMC Infect Dis. 2014, 14, 452. ISSN 1471-2334
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2018 Issue 1
Most read in this issue- Surgical treatment of diaphyseal humeral fractures
- Developmental morphology of the elbow joint in relation to injuries of the paediatric skeleton
- Post-traumatic peritonitis
- Arthroscopy-assisted osteosynthesis of triplane fracture – case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

