-
Medical journals
- Career
Patient´s respiratory curve synchronization by visual feedback application
Authors‘ workplace: Faculty Hospital, Oncology Clinic, Ostrava, Czech Republic 2
Published in: Lékař a technika - Clinician and Technology No. 1, 2018, 48, 17-21
Category: Original research
Overview
In radiation therapy, irradiation systems are focused to target using a CT scan. In the case of target which is moving by breathing, the CT scan is performed in the patient's inhale or exhale. However, ensuring that the patient is breathing same way as during the CT scan is really problematic. This project deals with the issue by using special respiratory sensor and software application, which presents respiratory curve to patient via video goggles. During the planning CT scan, the patient's breathing curve is captured by a special sensor and is displayed using a software application that allows insertion of the limit markers, which are represented by stripes, which indicate how much the patient inhaled. The application has possibilities to store the location of stripes during CT scan and retrieve it again during a scheduled radiotherapy, when patient can surely breathe the same way as during a planning CT scan. The application was developed, implemented and successfully tested at the Oncology Clinic of the Faculty Hospital Ostrava.
Keywords:
radiotherapy, CT, respiratory curve capturing, video goggles, C#Introduction
Radiotherapy is a method of treatment that uses ionizing radiation to destroy tumor tissues. Ionizing radiation is a stream of electromagnetic or corpuscular particles that transmit energy through the body and have a degenerative effect on living tissues. Today’s irradiation systems are partially or completely robotic and focus on tumor deposits using previously scheduled CT scanning. During the irradiation process, the patient is in the same position as during the CT scan, and CT images are used as a navigation plan. [1–4]
Problem definition
In oncological practice the tumor bearing can be located somewhere, where is moved by patient’s respiratory activity. It includes for example breasts, lungs or prostate. Tumor movement means lower accuracy, which also leads to the delivery of irradiation dose into healthy tissue. [5–8]
Possible solution is to irradiate tumor tissue only during inhalation or exhalation, but there is no assurance, that patient’s inhalation or exhalation is every time exactly same. Today’s irradiation systems are focused on tumor bearing using planning CT scan, which was done right during patient’s inhalation and exhalation. That approach should exclude dislocation of tumor by respiratory activity of patient, but there is no way to ensure same inhalation and exhalation during irradiation process. This issue is resulting into significant decrease of irradiation precision and damaging of healthy tissue because of delivery of radiation dose to wrong location as could be seen on figure 1. [9–13]
1. Irradiation process without breathing control. 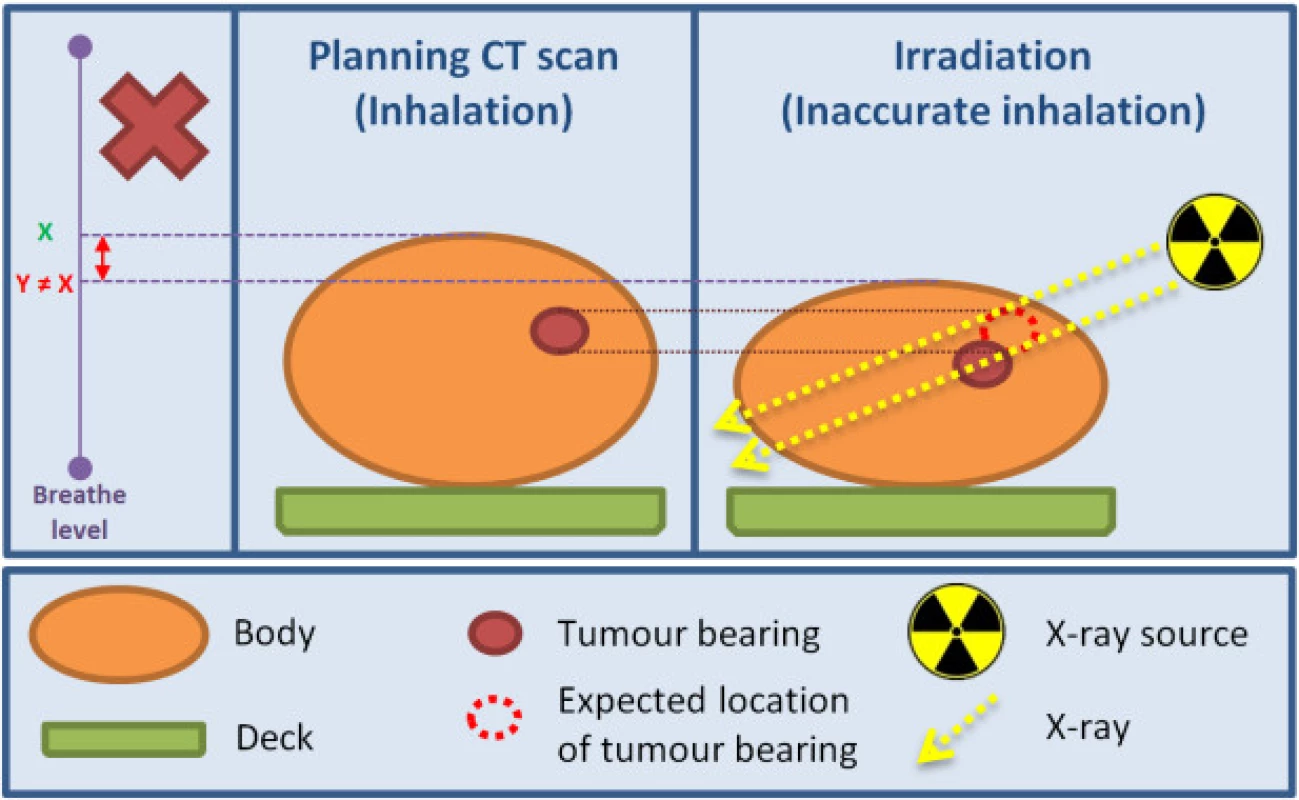
Problem solution
Same level of inhalation and exhalation can be ensured using visual feedback. The visual feedback offers patient to see change of his breathe level in realtime. Visual representation of breathe level should be as simple as possible, because patients are usually in different age group and are not technicians. Visual feedback of breathe level is presented to patient using video goggles during CT scan and during irradiation process. [14–16]
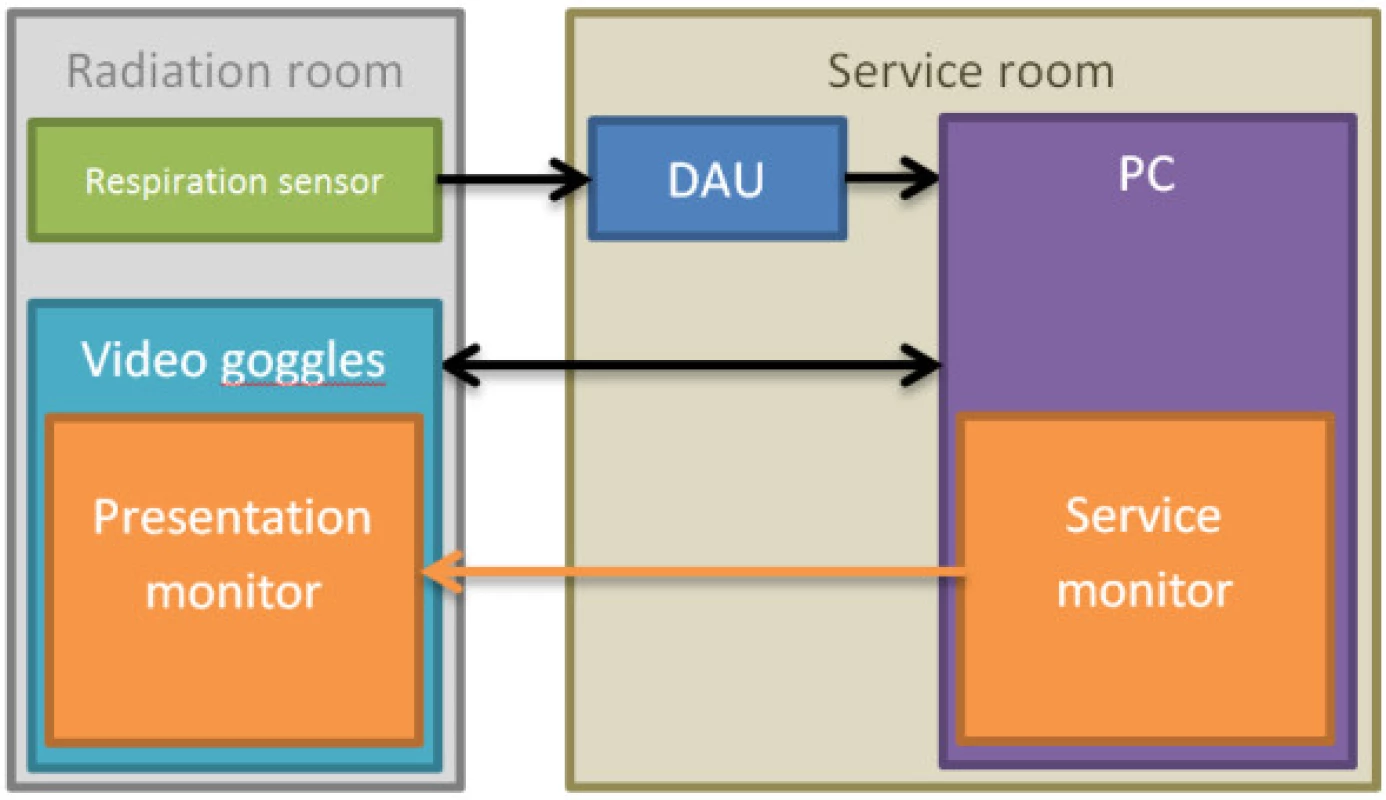
Breathe level is captured by special sensor realized as chest band. Measured signal is sent to universal data acquisition unit (DAU) and downloaded into computer via USB connection. DAU was constructed to acquire bioelectrical signals at VSB – Technical University of Ostrava. Finally, downloaded data are processed by software application and presented to patient. [17–19]
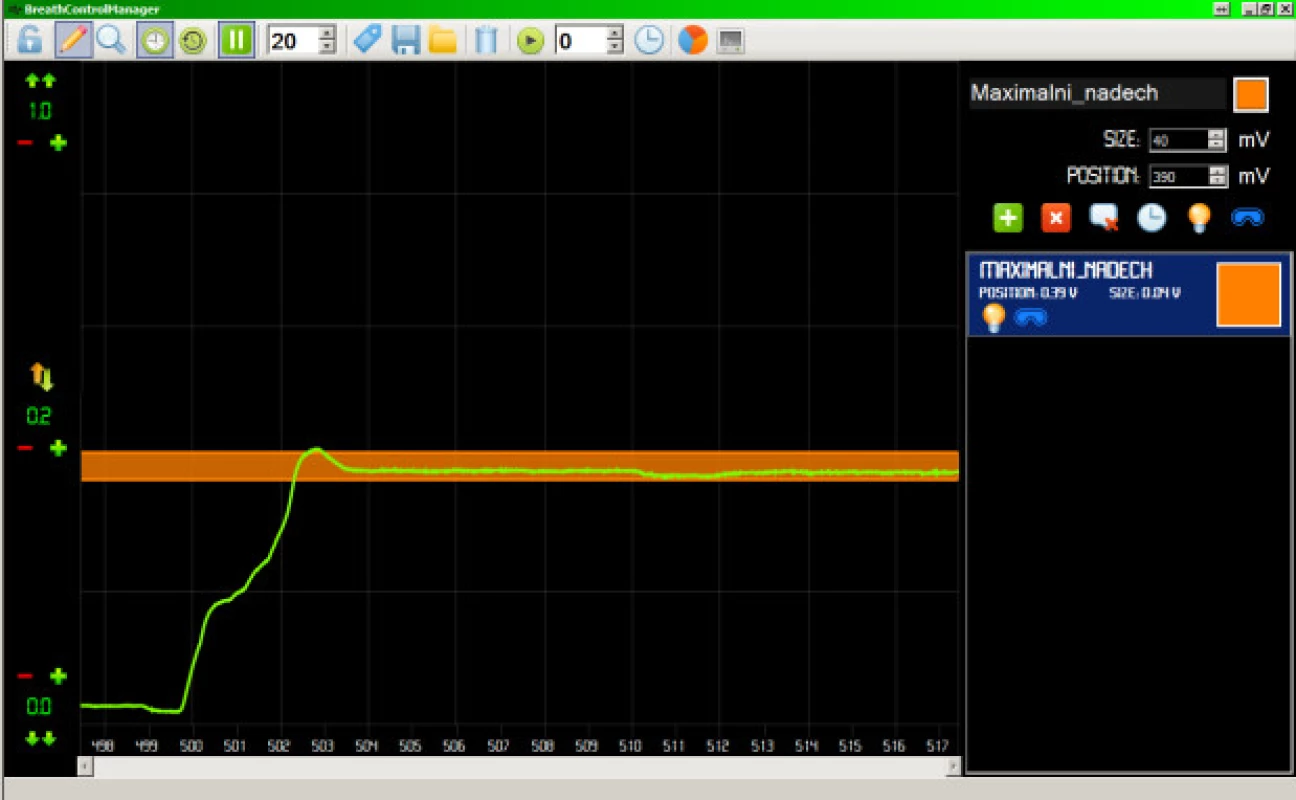
Breathe information is captured during CT scan and loaded during irradiation process. Achieve exactly same breathe level is impossible, therefore only breathe limits are captured during CT scan. Breathe limits are represented by horizontally placed stripes. Breathe limits are represented by horizontally placed stripes surrounding patient inhalation and exhalation. Stripe limits are defined manually by technician according to respiratory possibilities of patient. During irradiation process, patient is guided by video goggles to hold his breathe level within stripe limits. [20–22]
Approach mentioned above offers significant increase of precision and efficiency of irradiation process. The most important benefit is ensuring the radiation dose is delivered to the right place, which means minimal irradiation of healthy tissues as could be seen on Figure 2.
2. Irradiation process with breathing control via visual feedback. 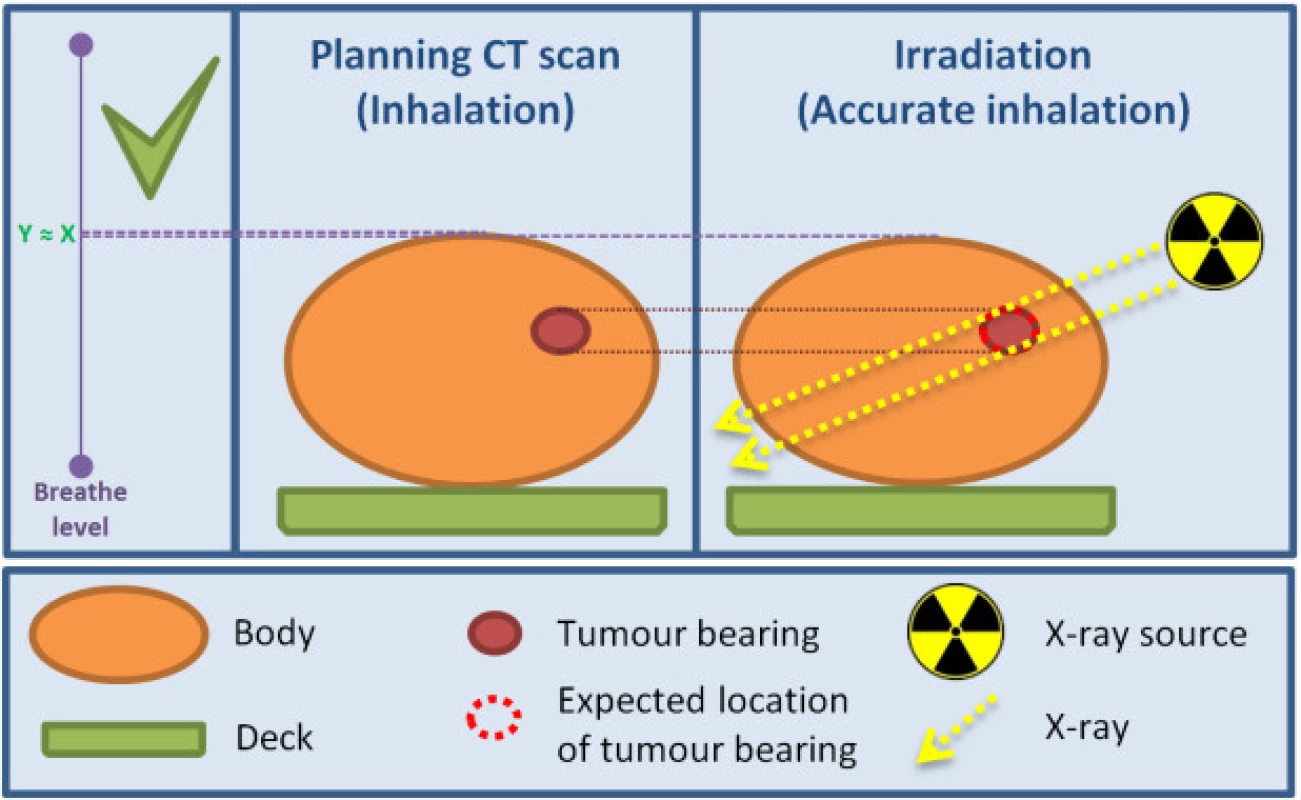
Design and Implementation
Respiratory measuring and presentation system
Breathe information is captured using special sensor and represented as analog signal, which is converted to digital one via DAU device. DAU communication with computer is established via USB cable.
The sensor contains several metal parts but is still usable during CT scans and output radiographs are negligibly impaired. In case of problems, metal parts can be shifted out of region of interest.All hardware of measuring and presentation system is consisted of breathe level sensor, DAU device, computer, video goggles and connection wires.
Software is graphical application implemented in programming language C#. The software application is divided into two parts: Service Monitor and Presentation Monitor.
Patient equipped with video goggles and sensor is located in irradiation room. Other parts of system are located in service room. All measuring and presentation system is shown in Figure 3.
4. Data acquisition unit (DAU). 
6. Presentation Monitor window. 
Software application
The software application is divided into two parts. First part is window called Service Monitor and is used for presentation of respiratory curve to technician.
Second part is window called Presentation Monitor and is used for presentation of current breathe level to patient via video goggles.
Service Monitor is main window of application, therefore respiratory curve is shown there as timedependent voltage for presentation to technician. Main purpose of application is creation and management of stripes representing patient's respiration limits. Every stripe has several properties like position, width, name, color. There are also possibilities to assign text comment to stripe or change its visibility. Visibility of stripe could be set as globally or relative to patient, means that every stripe can be visible to everyone (technician and patient), invisible to everyone or invisible just for patient. There are also possibilities of automatic timing.
These precautions prevent incorrect manipulation with stripes during irradiation therapy, where the stripes must be in the same condition as during the planning CT scan.For security reasons the application offers two work modes: Editor and Viewer Mode. Viewer Mode offers only functions which do not affect stripe position or size. Viewer Mode is set as default upon startup of application and password is required to enter Editor Mode.
Service Monitor window is able to display respiratory curve in two display modes. First mode displays data same way as oscilloscope do. Curve samples are drawn from left to right and at the end of
view curve is cleared and drawing starts again from beginning of view. Second mode displays data as continuous time span shifted with every new sample of signal. Span and resolution of both axes can be changed in both modes.Real-time signal measurement could be paused and displayed view can be moved to anywhere from beginning of measurement. Creation of stripe ex post is also available.
All created stripes can be saved to file containing all properties of stripes. Extra information saved is display settings and patient personal information. Saved personal information is name, surname and personal identification number.
Very important function is countdown timer function. When timer set by technician is activated countdown is displayed to patient. Displayed time tells patient how long he must hold his breath within stripe limits until CT scan or irradiation process is complete.
Countdown timer function is activated manually by technician or automatically. Automatic activation of timer function is triggered by reaching of breathe level to bottom limit of stripe which has triggering flag.
Countdown timer function is important assistance to patient because offers visual feedback of remaining time to holding breath. The function also offers extra information for technician because records time when patient’s breathe level entered and left the stripe. The recorded times can be used to recover CT scan unfinished because of patient was not able to hold his breath until its end and prematurely left the stripe.
By default new stripe created via Service Monitor is not displayed to patient. This approach is used to remove distraction of patient during managing of stripes by technician.Presentation Monitor window is presented to patient via video goggles. Current value of breathe level is displayed there in simplified way as small airplane and guiding horizontal line. Both move vertically in Y axis up and down.
Airplane moves just on the left side of screen and for easier watching is followed by red guiding horizontal
line. When activated, countdown timer is shown on the right side of screen and for better reading occupies 80 % of screen height. The pleasant environment is enhanced with slowly moving peaceful background. In the future, the application will offer more visual themes to cover all age groups of patients.Discussion and conclusion
Combination of software application and respiratory level sensing system offers almost complete reconstruction of patient’s breathe level recorded during planning CT scan. The patient can achieve better serenity and confidence during irradiation therapy thanks to the visual feedback and the pleasant environment in which it is presented. It is very powerful tool for improvement of precision and efficiency of irradiation process using visual feedback. Another benefit is assurance of delivery of irradiation dose only into targeted tumor bearing and associated protection from possible injury of healthy tissues due to shift of tumor bearing to different position by unequal patient respiration.
Because of use of DAU as a data acquisition tool, the software application can be modified and it would be possible to capture other different signals and present them in a visually-friendly way. Such approach would be found useful also in other areas than oncology and may be a new way of the data representation to patients of all ages.
Acknowledgements
The work and the contributions were supported by the project SV4507741/2101, 'Biomedicínské inženýrské systémy XIII', This study was supported by the research project The Czech Science Foundation (GACR) No. 17-03037S, Investment evaluation of medical device development.
Ing. David Oczka
Department of cybernetics and biomedical engineering
Faculty of Electrical Engineering and Computer Science
VSB – Technical University of Ostrava
17. listopadu 15
Ostrava - Poruba 708 33
Email: david.oczka@vsb.cz
Sources
- Oczka, D., Penhaker, M., Knybel, L., Kubicek, J., Selamat, A.: Design and Implementation of an Algorithm for System of Exposure Limit in Radiology, in Recent Developments in Intelligent Information and Database Systems. vol. 642, Krol, D., Madeyski, L., Nguyen, N. T., Eds., ed, 2016, pp. 433–443.
- Penhaker, M., Novakova, M., Knybel, J., Kubicek, J., Grepl, J., Kasik, V., et al.: Breathing Movement Analysis for Adjustment of Radiotherapy Planning, in Advanced Topics in Intelligent Information and Database Systems. vol. 710, Krol, D., Nguyen, N. T., Shirai, K., Eds., ed, 2017, pp. 105–116.
- Araki, F., Moribe, N., Shimonobou, T., Yamashita, Y.: Dosimetric properties of radiophotoluminescent glass rod detector in high-energy photon beams from a linear accelerator and Cyber-Knife, Medical Physics, vol. 31, pp. 1980–1986, Jul 2004.
- Bogart, J. A.: Stereotactic body radiotherapy for poor-risk lung cancer: More cyber, less knife?, Cancer Journal, vol. 13, pp. 75–77, Mar–Apr 2007.
- Hudak, R., Zivcak, J., Toth, T., Majernik, J., Lisy, M.: Usage of Industrial Computed Tomography for Evaluation of Custom-Made Implants, in Applications of Computational Intelligence in Biomedical Technology. vol. 606, Bris, R., Majernik, J., Pancerz, K., Zaitseva, E., Eds., ed, 2016, pp. 29–45.
- Rashid, A., Mone, P., Sarfaraz, M.: Predicting late lung complications following lung tumor radiosurgery with cyber knife using biologically effective doses and normalized dose-surface histograms, Medical Physics, vol. 34, pp. 2482–2482, Jun 2007.
- Telka, E., Cieslak-Stec, M.: Use of the cyberk knife stereotactic radiosurgery for the treatment of lymph node in the ovarian folliculoma metastasis, International Journal of Gynecological Cancer, vol. 25, pp. 1511–1511, Oct 2015.
- Glavatskyi, O., Buryk, V. M. K., Kardash, A., Pylypas, O. P., Chebotaryova, T. I.: Usage of cyber knife hypofractionated radiosurgery in high grade gliomas complex treatment, Neuro-Oncology, vol. 16, Sep 2014.
- Mancini, M., Brignani, D., Conforto, S., Mauri, P., Miniussi, C., Pellicciari, M. C.: Assessing cortical synchronization during transcranial direct current stimulation: A graph-theoretical analysis, Neuroimage, vol. 140, pp. 57–65, Oct 2016.
- Cvek, J., Knybel, L., Molenda, L., Otahal, B., Jonszta, T., Czerny, D., et al.: A single reference measurement can predict liver tumor motion during respiration, Reports of Practical Oncology and Radiotherapy, vol. 21, pp. 278–283, May–Jun 2016.
- Cvek, J., Knybel, L., Skacelikova, E., Otahal, B., Havranek, O., Krhut, J., et al.: Ultrahypofractionated Stereotactic Radiation Therapy for Low-Intermediate Stage Prostate Cancer-Results From a Single Institution, International Journal of Radiation Oncology Biology Physics, vol. 96, pp. E246–E246, Oct 2016.
- Cvek, J., Knybel, L., Skacelikova, E., Stransky, J., Matousek, P., Zelenik, K., et al.: Hyperfractionated stereotactic reirradiation for recurrent head and neck cancer, Strahlentherapie Und Onkologie, vol. 192, pp. 40–46, Jan 2016.
- Xie, Y., Xing, L.: Intrafractional Motion of the Pancreas During Cyber Knife Radiation Therapy, International Journal of Radiation Oncology Biology Physics, vol. 81, pp. S789–S789, 2011.
- Lustig, R.: Use of Fractionation With Cyber Knife in Children: A Report of 5 Cases, Journal of Pediatric Hematology Oncology, vol. 32, pp. 441–441, Aug 2010.
- Fariselli, L., De Santis, M., Broggi, G., Bergantin, A., Bianchi, L., Milanesi, I.: Peliminary results of newly diagnosis and recurrent high grade glioma treated with cyber knife radiosurgery, Radiotherapy and Oncology, vol. 84, pp. S294–S294, Sep 2007.
- Bassalow R., Rodebaugh, R.: Evaluation of six dosimetric indices for Cyber Knife stereotactic radiosurgery treatment planning, Medical Physics, vol. 33, pp. 2100–2100, Jun 2006.
- Knybel, L., Cvek, J., Molenda, L., Stieberova, N., Feltl, D.: Analysis of Lung Tumor Motion in a Large Sample: Patterns and Factors Influencing Precise Delineation of Internal Target Volume, International Journal of Radiation Oncology Biology Physics, vol. 96, pp. 751–758, Nov 2016.
- Knybel, L., Cvek, J., Stieber, N., Molenda, L., Otahal, B., Feltl, D.: Analysis of Respiratory Movement of Lung Tumors on a Large Sample: Patterns and Factors Influencing Precise ITV Definition," International Journal of Radiation Oncology Biology Physics, vol. 96, pp. S210–S210, Oct 2016.
- Kubicek, J., Penhaker, M., Feltl, D., Cvek, J.: Guidelines for modelling BED in simultaneous radiotherapy of two volumes: tpv(1) and tpv(2), in IEEE, 2013.
- Kasik, V., Cerny, M., Penhaker, M., Snášel, V., Novak, V., Pustkova, R.: Advanced CT and MR image processing with FPGA, in Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) vol. 7435 LNCS, ed, 2012, pp. 787–793.
- Kasik, V., Penhaker, M., Duciuc, E., Korpas, D.: Influence of ionising radiation on intelligent electronic implantable devices, in IEEE 10th Jubilee International Symposium on Applied Machine Intelligence and Informatics, SAMI 2012 - Proceed-ings, 2012, pp. 345–348.
- Grepl, J., Penhaker, M., Kubícek, J., Liberda, A., Selamat, A., Majerník, J., et al.: Real time breathing signal measurement: Current methods, IFAC-PapersOnLine, vol. 28, pp. 153–158, 2015.
Labels
Biomedicine
Article was published inThe Clinician and Technology Journal

2018 Issue 1-
All articles in this issue
- Median method for determining cortical brain activity in a near infrared spectroscopy image
- Patient´s respiratory curve synchronization by visual feedback application
- A comparsion of the quality of dental crowns from TI-6AL-4V and cocr alloys made with SLM technology
- Dimensionality reduction methods for biomedical data
- Agcu bimetallic nanoparticles modified by polyvinyl alcohol - the cells viability study in vitro
- The Clinician and Technology Journal
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Median method for determining cortical brain activity in a near infrared spectroscopy image
- A comparsion of the quality of dental crowns from TI-6AL-4V and cocr alloys made with SLM technology
- Dimensionality reduction methods for biomedical data
- Patient´s respiratory curve synchronization by visual feedback application
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career