-
Medical journals
- Career
Current position of eHealth care in the management of IBD patients
Authors: I. Romanko
Authors‘ workplace: Joint Admission of the General University Hospital for People with Medical Problems, Clinic of Anesthesiology, Resuscitation and Intensive Medicine, 1st Faculty of Medicine and General University Hospital in Prague
Published in: Gastroent Hepatol 2017; 71(4): 315-322
Category: IBD: Review Article
doi: https://doi.org/10.14735/amgh2017315Overview
The capacity of specialised centres to cope with the requirements of all patients suffering with lifelong chronic diseases, such as inflammatory bowel diseases (IBD), is often limited. The main reasons are the increasing incidence of Crohn’s disease and ulcerative colitis, and the higher proportion of more severe IBD cases requiring complex care. Currently, there are various ways to facilitate communication between patients and IBD centres, such as web interfaces, virtual clinics, video communication, smartphones and e-mail. Application of these and other technological modalities in medicine is referred to as telemedicine and it has recently become a topic in many discussions and investigations. There is evidence that telemedicine is feasible, beneficial and cost-effective for clinicians, patients and the healthcare system. This article reports recent trials and reviews discussing the current and future role of telemedicine or eHealth in IBD management, and discusses how it could be implemented and used in daily clinical practice.
Key words:
inflammatory bowel disease – Crohn disease – ulcerative colitis – telemedicine – eHealthIntroduction
Inflammatory bowel diseases (IBD) are a group of chronic inflammatory disorders of the gastrointestinal tract [1]. Their course is lifelong and typical for intermitent periods of relapses and remissions. Due to its long-time duration, these diseases have a critical impact on patients’ quality of life. Regular follow-up of patients by their gastroenterologist is necessary either for drug administration or monitoring of disease course. Patients with acute relapse or complications require more frequent visits compared to those in remission. Patients who have to travel long distances to visit their IBD specialist particularly experience problems with obtaining a physician’s appointment in cases of serious health deterioration [2].
In some cases, a simple change in medication or adjustment of drug dosage can be sufficient to solve patient’s acute problems [3,4] and this could possibly be done distantly, assuming that a tool exists to enable real-time distant contact of patients with their physician. Such communication could be established online or via applications for smartphones, which are currently widely used in public. Use of telemedicine, or eHealth [5], in this field is emerging.
Creating a virtual interface, which allows patients to communicate with their physicians opens a new dimension in patient care. Using specially developed patient-reported outcome measures (PROMs), a patients’ well-being (or quality of life, medication adherence, etc.) could be easily and regularly assessed and data stored in the database available for their physician at any time. Moreover, data about the clinical course of the disease could be collected, even during periods between regular controls. For example, a patient in long-term remission can visit a physician just once or twice a year, but clinical activity scores, quality of life scores, or other varieties of PROMs could be filled in according to intervals recommended by the physician. Results can then be assessed during appointment. This way of follow-up also enables patients to report changes in clinical activity of disease. Patient and physician are therefore able to inform and communicate with each other even before the appointment itself, and adequate measures could be taken more promptly. Moreover, patients are encouraged in self-management of their disease, they can adjust medication according to recommendations from their physician or healthcare team via eHealth programme, and together work on their better well-being. Evidence shows patients are satisfied with such a form of care [2,6,7].
PROMs are tools used to assess clinical activity (or quality of life, medication adherence, work productivity, etc.) according to patient provided data, e. g. number of stools, severity of abdominal pain, presence of blood in stools. They are validated either to physician’s global assessment, endoscopy, or routinely used clinical scores (e. g. HBI – Harvey Bradshaw Index, SCCAI – Simple Clinical Colitis Activity Index) [8]. These tools provide quick assessment without use of invasive (blood sample, endoscopy) or non-invasive (ultrasound, stool sample, physical examination) diagnostic methods. A number of various PROMs have been developed for assessment of clinical activity [9–12]. Their aim is to screen patients for possible relapses and warn physicians that further investigations or therapeutic interventions are necessary. PROMs represent tools suitable for use in a telemedicine approach; however, finding the most appropriate one remains a challenge due to different methods of validation, sensitivity, and specificity values.
There is continuously growing evidence that telemedicine in IBD care helps to detect relapses in earlier stages, reduces duration of hospital admissions, facilitates clinical practice, reduces duration of relapses and even reduces cost of health care [2,13,14]. Telemedicine is showing to be an effective tool for patient–physician communication, not only in the field of IBD, but other fields of medicine as well, e. g. gastroenterology in general (bowel preparation education, education in dealing with HCV patients) or rheumatology [7].
In the first part of this review we discuss recent broad review of IBD telemedicine and focus on points which, we believe, have not been emphasized enough. Discussion on aspects not mentioned in this article can be found in original review [15]. In the second part, we discuss other technological ongoing trials and present ideas about what, in our opinion, appropriate telemedicine tools should be like.
Impact of technologies implemented for eHealth on various outcomes
In 2016 Jackson et al. [15] published a systematic review of eHealth technologies in IBD. They analysed six randomized control trials (RCT) and nine other studies comprising a cohort study, case series and two studies where the study design was not specified. In the original article 17 studies are listed, but two of them were not completed by publication of the review, and their findings and/or conclusion were not stated. Studies worked with web-based interventions, telemedicine, virtual clinics, and other eHealth interventions. The majority of the studies were implemented on ulcerative colitis (UC) patients. Analysis included impact of eHealth management on indices of disease activity, patient reported outcomes – PRO (quality of life, work productivity, psychological outcome), and other outcome measures (e. g. medication adherence or healthcare costs). Only 6 studies out of 17 have a change in disease activity as their primary or secondary endpoint.
Web-based interventions
RCTs and two cohort studies worked with web-based interventions. Participants worked with interfaces accessible by web browsers. Findings show that impact on disease activity is very modest and most likely beneficial for UC patients [16–18]. Jackson et al. suggest that web-based intervention may reduce duration of relapse, but that has only been reported in the study of Elkjaer et al.; however, this is one of the leading studies of eHealth in UC [13,15].
These statements have arisen from six studies, two of which did not use a control cohort followed by standard care. It is unclear whether a difference between standard and intervention groups would be significant. One study of Crohn’s disease (CD) used only psychological intervention to influence disease activity [15], therefore the benefit of web-based interventions with regards to therapy guidance cannot be assessed.
Disease activity has been a primary outcome in only two studies. We believe that the impact of telemedicine on disease activity should be studied further and should be one of the primary endpoints. Further data are required for CD, and impact on disease course should also be assessed further, as so far it has been done so only in one RCT [13].
Objective markers of disease activity have been used for assessment together with PROMs in works of Pedersen (both for UC and CD) and Elkjaer et al., to help guide web-based therapies [13,16,17]. According to Jackson et al. results suggest that faecal calprotectin (FC) may correlate with luminal disease activity in UC, but may not be as effective for CD patients in guiding web-based therapy [15]. In our opinion this statement comes from very limited evidence and it has to be emphasized that further investigation of the role of FC in telemedicine is necessary, along with a determination of proper cut-off values. Data on disease activity stratification due to FC levels are still non-consistent. The reason could be interindividual variability of FC levels, which has already been reported [19]. The feasibility of FC for disease activity assessment has been discussed in our previous article in more detail [8]. We suggest further study of the dynamics of FC within individuals to determine an association of change in FC level with change of disease course (i.e. recognition or prediction of relapse).
Other impacts have been discussed by Jackson, such as medication adherence, cost effectivity, work productivity, general IBD knowledge and quality of life. More detail can be found in the original review [15]. In our opinion, work productivity is one of the very important factors in IBD management, as most patients are in their productive age. Therefore their disease affects not only their lives, but the society they live in, too. We believe it is necessary to prove whether telemedicine could improve long-term activity impairment of patients. It might encourage funding institutions of healthcare to support this form of management, if it could save funds for both the healthcare and social system. This should be investigated in more detail in future trials, as it has only been done directly in one study [17]. Moreover, we also regard assessment of fatigue and disablity in IBD management as necessary. It could be done using a FACIT-fatigue questionnaire, available for CD and UC [20].
A statement on medication adherence came out of three studies on UC patients only [15]; therefore data for CD are missing and could be a useful outcome of future studies.
Virtual clinics
Three analysed studies worked with virtual clinics [15, 21–23]. The term “virtual clinic” refers to a form of contact arranged between a physician and patient prior to a face-to-face meeting, for the purpose of advice, consultation and/or changes of treatment. This can be done via e-mail, telephone, smartphone application, or a web-based portal, and has to meet certain specified criteria [24]. Only two out of three had available results. Johnson et al. reported a cost effectivity of virtual clinics, saving 130,000 £ per year of treatment, and patient satisfaction with this type of intervention. Hunter et al. showed a 20% decrease in physical clinic attendance in patients treated through a virtual clinic, and 83% of patients reported decreased personal costs; however, the size of patient cohort has not been specified [22]. Of high importance, in our opinion, is the other secondary endpoint in the study of Hunter, i.e. that a transfer of patients to a virtual clinic generated more space in standard outpatient clinics for those who needed face-to-face contact. None of these studies has evaluated the impact of virtual clinics on indices of disease activity.
Johnson’s and Hunter’s papers included patients with stable IBD. Many patients with long-term disease-free periods do not require face-to-face visits and can be managed distantly. In cases of deterioration, they can quickly contact their physician and arrange an appointment, if necessary. Therefore, more close observation can be arranged between physician and patient, but those who are clinically stable are freed from regular visits to their IBD centres. In our opinion, the work of Hunter is a good example of how eHealth can facilitate management of outpatient clinics.
According to Jackson et al., data regarding efficacy of virtual clinics are limited to non-validated qualitative questionnaires [15]. We would like to add that both studies mentioned above had not specified duration of follow-up and had no control groups.
Both Hunter and Johnson reported the cost-effectiveness of virtual clinics. Due to absence of control groups, the savings were only estimated and it is questionable how it would turn out to be in practice. Cost-effectiveness is another important endpoint that has also been studied in two [13,17] web-based intervention studies. Only the work of Elkjaer used a control group. We believe this aspect should be studied further, but with specified follow-up duration and control group on standard care for comparison.
Video link
Two studies used video link to review patients. Both showed satisfaction of patients with telemedicine; moreover, Hommel et al. showed increased medication adherence to 5-ASA (but decrease of adherence to immunomodulators) and cost-efficiency. Unfortunately, both studies of Hommel et al. and Krier et al. (RCT) worked with a very small number of patients, being nine and 34, resp. Disease activity was not used as an outcome in either of these studies [25,26].
Smartphone application
A systematic review of 26 existing IBD applications for smartphones has been made by Con et al. None showed efficacy of self-management due to lack of decision support offered in these applications. There are two RCTs planned to work with smartphone applications, and study their impact on IBD [27]. Applications are intended to have a decision support system for medical staff, along with alert plans for management of patients with flare-ups. While Atreja et al. focus more on quality of life and feasibility with eHealth tool, Cross et al. plan to assess disease activity (Seo index, CDAI – Crohn’s disease activity index), quality of life, utilization of healthcare resources, self-efficacy, patient knowledge and satisfaction [7,28,29].
Only one study using a cohort of 76 patients studied the impact of e-mail communication on IBD. Plener et al. showed patients’ satisfaction with combined clinic and e-mail consultations compared to clinic alone, along with reduced levels of stress. Other aspects mentioned above have not been studied [30].
A systematic review similar to Jackson’s was published in February 2015 by Aguas et al. [31] Their conclusions are similar to Jackson’s; eHealth technologies seem to be safe, well-accepted by patients, feasible and have been proven to improve quality of life, disease knowledge and medication adherence.
Confirmation of these results is necessary in future trials along with proper cost efficacy, work productivity, or disease activity assessment.
Other recent eHealth ongoing trials
In 2015, Van Deen at al. developed a PRO index for disease activity in CD and UC for use in mobile phones. For development, they used existing clinical activity index and developed a new one based on number of liquid stools, abdominal pain, general well being and patient reported disease control for CD, and abdominal pain, rectal bleeding, number of stools and patient reported disease control for UC. Indices were validated on a broader cohort of patients. The authors found that indices identified clinical disease activity with ROC 0.9 for CD and 0.91 for UC, and identified endoscopic activity with ROC 0.63 and 0.82 for CD and UC, resp. This index showed to be useful for mobile phone applications to monitor disease activity at home [32].
Marín-Jiménez et al. studied differences in SCCAI scoring by gastroenterologists and patients alone. Patients self-administered the questionnaire online at specific intervals. The authors found out that self-administration had a high percentage of agreement with scoring of gastroenterologists, the correlation coeficient beeing 0.79, with 85% agreement for disease remission or activity [33].
There is an ongoing RCT with 10 Dutch IBD centres working with 180 teenagers aged 10–19, who are randomized into web-guided therapy and their usual care group. Patients regularly fill out a “flarometer”, which is a series of questions derived from UCDAI (Ulcerative Colitis Disease Activity Index) or CDAI. After completion, they are asked to send a stool sample to the laboratory. If the score is in the high risk range, the patient is advised to contact their IBD centre directly, without waiting for calprotectin analysis, which is done in 24 hours. Proper action is then taken according to the IBD team decision and the patient is appropriately informed. The aim of the study is to compare the effect of web-guided, calprotectin assisted therapy to standard care, along with cost-efficiency and quality of life. Results are not available yet [34].
Hommel et al. are running a RCT using telemedicine video conferences to improve medication adherence in teenagers, who score positive for a low medication adeherence [25]. They intend to randomize such patients into an eHealth behavioral treatment group and an education only group. Groups will be assessed by Medication Event Monitoring System 6 at baseline, post-treatment, and 3, 6 and 12 months to compare medication adherence [35].
De Jong et al. have published a development and feasibility study of telemedicine tool myIBDcoach, which has been designed for all types of IBD patients in the Netherlands [36]. Patients complete expert-opinion derived questionnaires on either a regular or patient required basis. There are several modules: monitoring for disease course surveillance, intensified monitoring for improved flare-up control, an outpatient module to be completed before an upcoming outpatient visit, and e-learning to increase self-management and education of patients. An option for communication with the healthcare provider is also implemented. This tool is accessible via internet, smartphone or tablet. The authors state that patients showed high adherence and satisfaction to this method and 93% would recommend it to other patients. They have pushed their work further and prepared RCT comparing standard care and myIBDcoach care for one year. Primary outcomes are number of outpatient visits and quality of IBD helathcare. Secondary outcomes are number of flares, hospitalizations, medication adherence, need for corticosteroid use, and quality of life.
Summary and conclusions
eHealth use in IBD management is progressing and evolving. There is evidence showing that web-based management and smartphone applications are feasible ways of constant care. Medicine tries to keep up with information technologies to offer better care for patients.
Validated questionnaires in their electronic form are suitable to monitor quality of life [8] and could be very useful in assessment of productivity (many IBD patiens are limited in work because of IBD symptoms), or IBD self-management. eHealth gave an impulse to develop new PROMs focused on disease activity, competing with widely used tools like HBI and SCCAI [8,11,32]. It is necessary to validate these new measures against objective markers of disease activity, most suitably against endoscopic grades of disease severity.
Further trials with eHealth tools should be conducted to properly compare cost-efficiency (both direct and indirect costs) between standard care and telemedicine interventions [15], and to also assess impact on work productivity.
Proper FC cut-off levels for IBD patients still remain a challenge and require further trials to determine appropriate values. Moreover, FC levels should be assessed at baseline and after a specified time of eHealth interventions. There are still limited data to show whether guidance by FC is appropriate (in a work of Elkjaer, a comparison was not possilble after three months due to the small number of samples).
Medication adherence in patients with CD could be an important endpoint in future studies, as appropriate data are still missing. Another endpoint could be assessment of distant management efficacy in patients with active or complicated IBD. Most of the trials have so far included patients with stable IBD only.
We see a promising perspective in a combination of web-based intervention and virtual clinics, which could also be accessible via smartphone applications. Such eHealth tools could serve to demonstrate the impact of smartphone applications on IBD self-management. A disease activity PROM, validated against endoscopy (which remains a gold standard to assess disease activity [35]), should be used. For proper validation of eHealth PROMs for disease activity, conventional clinical indices should be used, as they are accepted by specialists.
Quality of life is so far the only PROM proved to have improved by using eHealth web-based interventions [15]. Others, like medication adherence or self-management, have either inconsistent results or we presently do not have sufficient evidence for conlusions apart from the necessity for further investigation. During a follow-up, an eHealth tool should work with an objective marker, which can be measured at home, and results sent to physicians electronically. FC home tests – smartphone kits – have been shown to be appropriate for this purpose [37,38]. Using other inflammatory markers (C reactive protein, full blood count) would require a patient visit to conduct a blood test, which is not feasible for screening, but necessary in case of alert symptoms. Tab. 1 summarizes features, advantages and disadvantages of several eHealth modalities mentioned in this review. For future studies, combinations of the modalities mentioned above are possible, or new ones could be created as information technologies and PROMs continue to evolve.
1. Summary of features of several eHealth modalities. Tab. 1. Přehled charakteristik několika forem eHealth. 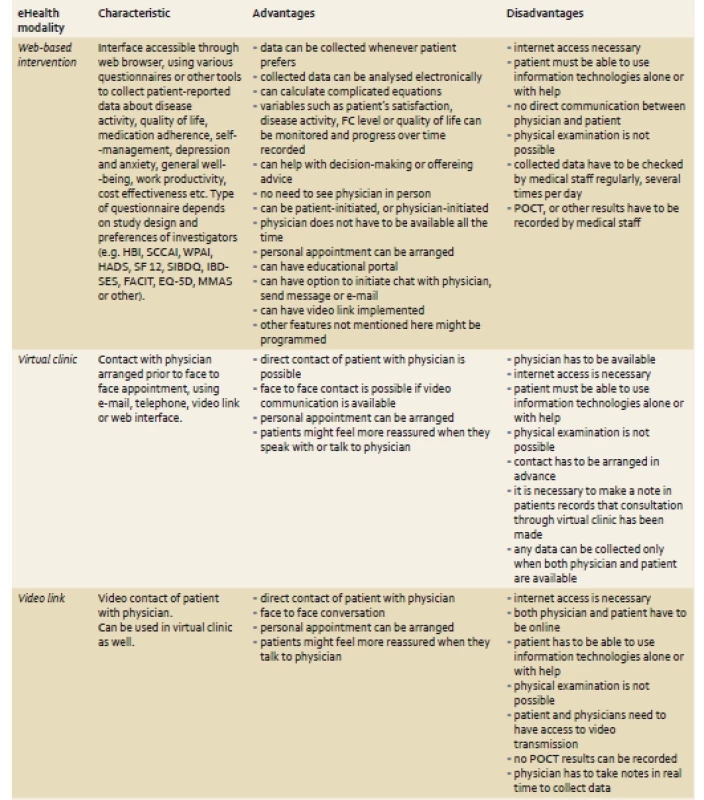
Investigators should try to include all categories of patiens into the trials (UC, CD, monotherapies, immunomodulators, biological therapy, complicated and uncomplicated courses) to obtain the most objective results.
The evidence mentioned above suggests that eHealth has a potential for use in IBD follow-up and can facilitate clinical practice. More complex controlled trials comprising web-based guidance, smartphone applications, virtual clinics, or else are necessary to assess its efficacy. Moreover, evidence given about ongoing trials shows that there exists an interest among researchers to develop and use eHealth technologies in IBD. There is still a long way to go to create an appropriate eHealth tool for IBD management, but advancing the telemedicine approach seems to be the right way of facilitating follow-up of IBD patients.
The author would like to thank Clinical and Research Center for Inflammatory Bowel Diseases ISCARE I.V.F., a. s. for cooperation in writing this review.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE „uniform requirements“ for biomedical papers.
Submitted: 17. 5. 2017
Accepted: 31. 7. 2017
Igor Romanko, MD
Joint Admission of the General University Hospital for People with Medical Problems
Clinic of Anesthesiology, Resuscitation and Intensive Medicine
1st Faculty of Medicine and General University Hospital in Prague
U Nemocnice 1
128 08 Prague 2
Czech Republic
igor.romanko89@gmail.com
Sources
1. Vora P, Shih DQ, McGovern DP et al. Current concepts on the immunopathogenesis of inflammatory bowel disease. Front Biosci (Elite Ed) 2012; 4 : 1451–1477.
2. Huang VW, Reich KM, Fedorak RN. Distance management of inflammatory bowel disease: Systematic review and meta-analysis. World J Gastroenterol 2014; 20 (3): 829–842. doi: 10.3748/wjg.v20.i3.829.
3. Berman M1, Fenaughty A. Technology and managed care: patient benefits of telemedicine in a rural health care network. Health Econ 2005; 14 (6): 559–573.
4. Krier M, Kaltenbach T, McQuaid K et al. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol 2011; 106 (12): 2063–2067. doi: 10.1038/ajg.2011. 329.
5. Capalbo SM, Heggem CN. Valuing rural health care: issues of access and quality. Am J Agri Econ 1999; 81 : 674–670.
6. Barlow C, Cooke D, Mulligan K et al. A critical review of self-management and educational interventions in inflammatory bowel disease. Gastroenterol Nurs 2010; 33 (1): 11–18. doi: 10.1097/SGA.0b013e 3181ca03cc.
7. Siegel CA. Transforming gastroenterology care with telemedicine. Gastroenterology 2017; 152 (2): 958–963. doi: 10.1053/j.gastro.2017.01.048.
8. Romanko I, Lukáš M, Bortlík M. New approaches in follow-up of patients suffering from inflammatory bowel diseases. Gastroent Hepatol 2015; 69 (5): 441–448. doi: 10.14735/amgh2015441.
9. Surti B, Spiegel B, Ippoliti A et al. Assessing health status in inflammatory bowel disease using a novel single-item numeric rating scale. Dig Dis Sci 2013; 58 (5): 1313–1321. doi: 10.1007/s10620-012-2500-1.
10. Bodger K, Ormerod C, Shackcloth D et al. Development and validation of a rapid, generic measure of disease control from patient’s perspective: the IBD-control questionnaire. Gut 2014; 63 (7): 1092–1102. doi: 10.1136/gutjnl-2013-305600.
11. Keefer L, Kiebles JL, Taft TH et al. The role of self-efficacy in inflammatory bowel disease management: preliminary validation of a disease-specific measure. Inflamm Bowel Dis 2011; 17 (2): 614–620. doi: 10.1002/ibd.21314.
12. Alrubaiy L, Rikaby I, Dodds P et al. Systematic review of health-related quality of life measures for imflammatory bowel diseases. J Crohn Colitis 2015; 9 (3): 284–292. doi: 10.1093/ecco-jcc/jjv002.
13. Elkjaer M. E-health: Web-guided ther-apy and disease self-management in ulcerative colitis. Impact on disease outcome, quality of life and compliance. Dan Med J 2012; 59 (7): B4478.
14. Kim ES, Park KS, Cho KB et al. Development of a web-based, self-reporting symptom diary for Crohn’s disease, and its correlation with the Crohn’s Disease Activity Index: web-based, self-reporting symptom diary for Crohn’s disease. J Crohns Colitis 2014; pii: S1873-9946[14]00268-2. doi: 10.1016/j.crohns.2014.09.003.
15. Jackson BD, Gray K, Knowles SR et al. EHealth Technologies in Inflammatory Bowel Disease: A Systematic Review. J Crohns Colitis 2016; 10 (9): 1103–1121. doi: 10.1093/ecco-jcc/jjw059.
16. Pedersen N, Thielsen P, Martinsen L et al. eHealth: individualization of mesalazine treatment through a self-managed web-based solution in mild-to-moderate ulcerative collitis. Inflamm Bowel Dis 2014; 20 (12): 2276–2285. doi: 10.1097/MIB.0000000000000199.
17. Pedersen N, Elkjaer M, Duricova D et al. eHealth: individualisation of infliximab treatment and disease course via a self-managed web-based solution in Crohn’s disease. Aliment Pharmacol Ther 2012; 36 (9): 840–849.
18. Mc Combie A, Gearry R, Andrews J et al. Does Computerized Cognitive Behavioral Therapy Help People with Inflammatory Bowel Disease? A Randomized Controlled Trial. Inflamm Bowel Dis 2016; 22 (1): 171–181. doi: 10.1097/MIB. 0000000000000567.
19. Calafat M, Cabré E, Mañosa M et al. High within-day variability of fecal calprotectin levels in patients with active ulcerative colitis: what is the best timing for stool sampling? Inflamm Bowel Dis 2015; 21 (5): 1072–1076. doi: 10.1097/MIB.0000000 000000349.
20. Webster K, Odom L, Peterman A et al. The Functional Assessment of Chronic Ill-ness Therapy (FACIT) measurement system: Validation of version 4 of the core questionnaire. Qual Life Res 1999; 8 : 604.
21. Johnson M, Lithgo K, Price T. IBD-SSHAMP (Supported, Self help and Management Programme); UK’s first Internet based Remote Management System for Managing Stable IBD. Gut 2013; 62: A34–A35. Abstract OC-080.
22. Hunter J, Claridge A, James S et al. Improving outpatient services: the Southampton IBD virtual clinic. Postgrad Med J 2012; 88 (1042): 487–491. doi: 10.1136/ postgradmedj-2012-100123rep.
23. Lichtenstein GR, Rubin D. Gastroenterology Virtual clinic. [online]. Available from: http: //ibdvirtualclinic.com/.
24. ISD Scotland. SMR Datasets, Virtual clinic. [online]. Available from: www.ndc.scot.nhs.uk.
25. Hommel KA, Hente E, Herzer M et al. Telehealth behavioral treatment for medication nonadherence: a pilot and feasibility study. Eur J Gastroenterol Hepatol 2013; 25 (4): 469–473. doi: 10.1097/MEG.0b013e 32835c2a1b.
26. Krier M, Kaltenbach T, McQuaid K et al. Potential use of telemedicine to provide outpatient care for inflammatorz bowel disease. Am J Gastroenterol 2011; 106 (12): 2063–2067. doi: 10.1038/ajg.2011.329.
27. Con D, De Cruz P. Mobile phone apps for inflammatory bowel disease self-management: A systematic assessment of content and tools. JMIR Mhealth Uhealth 2016; 4 (1): e13. doi: 10.2196/mhealth.4874.
28. Cross RK, JAmbaulikar G, Langenberg P et al. Telemedicine for patients with inflammatory bowel disease (TELE-IBD): Design and implementation of randomized clinical trial. Contemp Clin Trials 2015; 42 : 132–144. doi: 10.1016/j.cct.2015.03.006.
29. Atreja A, Khan S, Rogers JD et al. Impact of th Mobile HealthPROMISE platform on the quality of care and quality of life in patients with inflammatory bowel disease: study protocol of pragmatic randomized controlled trial. JMIR Res Protoc 2015; 4 (1): e23. doi: 10.2196/resprot.4042.
30. Plener I, Hayward A, Saibil F. E-mail communication in the management of gastroenterology patients: a review. Can J Gastroenterol Hepatol 2014; 28 (3): 161–165.
31. Aguas Peris M, Del Hoyo J, Bebia P et al. Telemedicine in inflammatory bowel disease: opportunities and approaches. Inflamm Bowel Dis 2015; 21 (2): 392–399. doi: 10.1097/MIB.0000000000000241.
32. Van Deen WK, van der Meulen-de Jong AE, Parekh NK et al. Development and Validation of an Inflammatory Bowel Diseases Monitoring Index for Use With Mobile Health Technologies. Clin Gastroenterol Hepatol 2015; 14 (12): 1742–1750. doi: 10.1016/j.cgh.2015.10.035.
33. Marín-Jiménez I, Nos P, Domènech E et al. Diagnostic Performance of the Simple Clinical Colitis Activity Index Self-Administered Online at Home by Patients With Ulcerative Colitis: CRONICA-UC Study. Am J Gastroenterol 2016; 111 (2): 261–268. doi: 10.1038/ajg.2015.403.
34. Heida A, Dijkstra A, Groen H et al. Comparing the efficacy of a web-assisted calprotectin-based treatment algorithm (IBD-live) with usual practices in teenagers with inflammatory bowel disease: study protocol for a randomized controlled trial. Trials 2015; 16 : 271. doi: 10.1186/s13063-015-0787-x.
35. Annese V, Daperno M, Rutter MD et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis 2013; 7 (12): 982–1018. doi: 10.1016/j.crohns.2013.09.016.
36. de Jong M, van der Meulen-de Jong A, Romberg-Camps M et al. Development and Feasibility Study of a Telemedicine Tool for All Patients with IBD: MyIBDcoach. Inflamm Bowel Dis 2017; 23 (4): 485–493. doi: 10.1097/MIB.0000000000001034.
37. Vinding KK, Elsberg H, Thorkilgaard T et al. Fecal calprotectin measured by patiens at home using smartphones – a new clinical tool in monitoring patiens with inflammatory bowel disease. Inflamm Bowel Dis 2016; 22 (2): 336–344. doi: 10.1097/MIB.0000000000000619.
38. Peyrin-Biroulet L, Sandborn W, Sands BE et al. Selecting therapeutic targets in inflammatory bowel disease (STRIDE): Determining therapeutic goals for treat-to-target. Am J Gastroenterol 2015; 110 (9): 1324–1338. doi: 10.1038/ajg.2015.233.
Labels
Paediatric gastroenterology Gastroenterology and hepatology Surgery
Article was published inGastroenterology and Hepatology
2017 Issue 4-
All articles in this issue
- Clinical and experimental gastroenterology
- Effect of nitroglycerin on high resolution manometry parameters in patients with achalasia
- Graft-duodenal fistula – a cause of massive gastrointestinal bleeding
- Potential use of non-invasive methods for non-alcoholic fatty liver disease
- Adenocarcinoma of the small intestine as an unusual cause of hypochromic anemia
- Acute appendicitis – a rare complication of colonoscopy
- Epidemiological study of obesity in populations of different racial, cultural, economic and dietary backgrounds
- 35th Slovak and Czech Gastroenterological Congress and 39th Slovak and Czech Endoscopic Days
-
Komentář k lékovému profilu
Rifaximin – terapeutické vlastnosti - The selection from international journals
- Remsima® – the first biosimilar infliximab CT-P13
- Serum concentration of S100P protein in patients with colorectal cancer
- Self-expandable coated metal Danis stent as a bridge to liver transplantation
- Outcome of treatment of Helicobacter pylori infection based on microbiological susceptibility testing following the unsuccessful second-line eradication treatment
- Current position of eHealth care in the management of IBD patients
-
Comment on article
Biosimilar infliximab in anti-TNF naïve IBD patients – 1-year clinical follow-up -
Endoscopic achievements in the upper gastrointestinal tract and small bowel
Christian Ell Lecture – Gastro Update Europe 2017, Vienna
- Gastroenterology and Hepatology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Outcome of treatment of Helicobacter pylori infection based on microbiological susceptibility testing following the unsuccessful second-line eradication treatment
- Self-expandable coated metal Danis stent as a bridge to liver transplantation
- Acute appendicitis – a rare complication of colonoscopy
- Graft-duodenal fistula – a cause of massive gastrointestinal bleeding
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


