-
Medical journals
- Career
Necrotic fasciitis of the lateral muscle group of the thigh following outside-in transobturatory tape procedure
Authors: Ondřej Dvořák; D. Leško; J. Kestřánek
Authors‘ workplace: Kralove, přednosta kliniky doc. MUDr. J. Špaček, Ph. D., IFEPAG ; Department of Obstetrics and Gynecology, Medical Faculty of Charles University and Faculty Hospital Hradec
Published in: Ceska Gynekol 2016; 81(6): 411-413
Overview
Objective:
Sling procedures are the preferred surgical treatment of stress urinary incontinence (SUI) due to their high success rate and low risk of complications.Design:
Case report.Setting:
Department of Obstetrics and Gynecology, Medical Faculty of Charles University and Faculty Hospital Hradec Kralove.Case report:
Necrotic fasciitis is a rare infectious complication, the mortality of which varies by age and can reach 73% if untreated. We present a case of a rare yet serious complication, necrotic fasciitis (NF), of a lateral muscle group of the thigh following antiincontinence implantation. Polypropylene transobturatory midurethral outside-in tape (TOT) was inserted, and NF occurred shortly after surgery.Conclusion:
Effective treatment was based on a timely diagnosis, administration of wide-spectrum antibiotics, intensive care unit support, surgical treatment, and multidisciplinary cooperation. Timely initiation and adequate treatment are critical in preventing mortality.Keywords:
multidisciplinary approach, necrotising fasciitis, TOTINTRODUCTION
Sling procedures are the preferred surgical treatment of stress urinary incontinence (SUI) due to their high success rate and low risk of complications. Most common early complications include bleeding, retention of urine, and de novo overactive bladder (OAB) and less frequently, perforation of the urinary bladder, urethra, or bowels. Late complications include protrusion or erosion of the tape, infection, and inguinal pain – Galloway syndrome. A rare infectious complication is NF [1], the mortality of which varies by age and can reach 73% if untreated. Patients aged over 50 years have a mortality rate of 37% versus 62% in those aged over 60 years. Thus, timely initiation and adequate treatment are critical in preventing mortality[5].
CASE REPORT
A 55-year-old woman who was hypertonic and obese with a history of deep vein thrombosis, two spontaneous deliveries, no abortions. The patient had been followed up and treated since 2008 in our urogynecological outpatient clinic for symptoms of mixed urinary incontinence. During the first examination, mixed urinary incontinence (SUI predominating) was diagnosed, treatment of OAB with parasympatholytics was prescribed and TOT was recommended for SUI.
We inserted outside-in TOT under general anesthesia with standard antibiotic prophylaxis. The procedure was uncomplicated, the patient went home with no residuum the following day. On day 10 after the surgery, the patient returned with a fever of over 39.5 °C and pain in the right inner thigh. A brownish, odorous vaginal discharge was noted, the right vaginal wall was painful. An ultrasonographic scan and subsequent CT showed no pathology.
The patient was hospitalized, with leukocytosis 14.5 k/mL, CRP 328 mg/L, for which we administered antibiotics (gentamicin 240 mg qd, klindamycin 600 mg tid, and metronidazol 500 mg tid). Extraction of the tape was planned, vaginal and urine cultures were performed.
On the following day, the venous system of the lower extremities was scanned by ultrasonography and an orthopedic examination was performed, with negative results. The fever persisted, a finding on the dorsal right thigh progressed to a large, reddish, painful infiltration, spanning the upper third of the femur to the popliteal fossa. There were no significant findings around the skin and vaginal incisions after TOT.
Because we suspected NF or an abscessing locus in the thigh, MRI was performed, detecting edema in the lower part of the gluteal muscles that propagated to the dorsal adductor group, reaching the distal quarter of the femur; superficial collection of liquid over the fascia was also observed (Fig. 1). Based on this information, we transferred the patient to the orthopedic clinic.
Fig. 1 T2-weighted MR images with fat saturation reveal areas of extensive myofascial edema of the right thigh, extending into the subcutaneous fatty tissue (prof. MUDr. J. Žižka Ph.D.) 
CRP levels rose to 458 mg/L, the septic fever persisted, and the local finding progressed. The antibiotic therapy was adjusted to gentamicin 320 mg qd, klindamycin 1200 mg qid, metronidazol 500 mg tid, and penicilin G 5*106 IU/4 hours. As concluded in an interdisciplinary consultation, the tape was left in situ due to unremarkable findings in the vagina, and a surgical revision of the right thigh was indicated.
A lateral part of the thigh was incised longitudinally (the location of the most severe impairment, according to the MRI and clinical signs). The subcutaneous layer was soaked and semisolid, and the fascia had thickened. Debridement of soft tissues with wide fasciotomy of the anterior and posterior muscle compartments was performed. The wound was left without sutures and covered with grease.
One week after the procedure, the leukocytosis and CRP levels began to decline. Septic fever persisted for 2 weeks after the surgery. A second round of debridement and necrectomy was performed 11 days after the initial procedure. By histology: hypocellular collagenous and adipous tissue with phlegmonous infiltrate. Vaginal cultures showed a massive presence of beta-hemolytic Streptococcus F and E. coli, and there was Enterococcus and alfa-hemolytic Streptococci in the urine.
After 4-week treatment with 4 antibiotics, klindamycin and metronidazol were administered i.v. for 10 days, followed by 14 days of oral klindamycin. The patient was released in good condition, with a CRP level of 5 mg/L. The outcome of the TOT was excedent. Twenty-four months after the surgery, the patient was continent without any problems.
DISCUSSION
NF is a rare infection that results in necrosis of the skin, subcutaneous tissue, and fascia. Its etiology is primarily multibacterial (type I) (eg, group A streptococcus, Staphylococcus aureus, Vibrio vulnificus, Clostridium perfringens, Bacteroides fragilis) and less frequently monobacterial (type II). Risk factors are obesity, hypertension, higher age, immunosuppression, and diabetes mellitus [3]. NF is diagnosed based on clinical and laboratory signs, but a definitive diagnosis is often difficult to make.
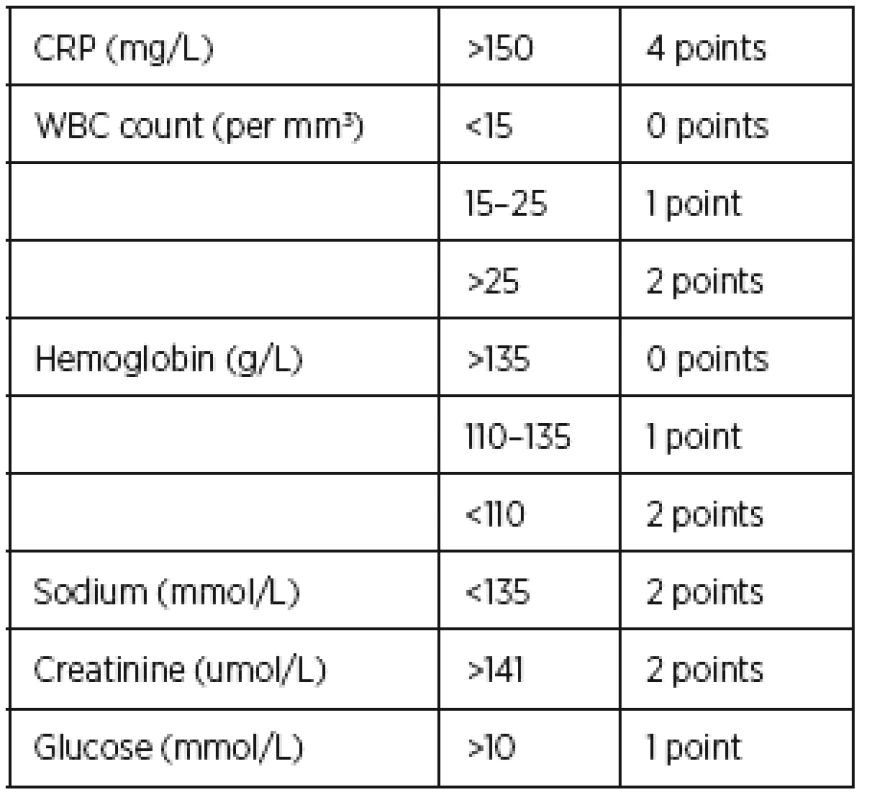
Patients tend to be febrile and exhausted, complaining of pain in the affected area, often experiencing diarrhea and vomit. The affected area is usually swollen and ruborous. Laboratory risk indicators for necrotizing fasciitis (LRINEC) score can contribute to a diagnosis of NF [2] . LRINEC scores comprise 6 laboratory signs (Table 1). A score over 6 reflects a high risk of NF. Our patient had a score of 5 on admission.
Treatment with antibiotics, followed by tape extraction, must be timely and vigorous to decrease the risk of mortality. Surgical debridement should follow, amputation is a last resort. Hyperbaric oxygenotherapy can be helpful in serious cases [4].
Treatment for necrotizing fasciitis should be multidisciplinary (gynecologist, orthopedist, antibiotic center specialist, infectiologist, and radiologist).
CONCLUSION
Necrotic fasciitis is a very rare complication following antiincontinence implantation. Effective treatment is based on a timely diagnosis, administration of wide-spectrum antibiotics, intensive care unit support, surgical treatment, and multidisciplinary cooperation. Timely initiation and adequate treatment are critical in preventing mortality.
MUDr. Ondřej Dvořák
Porodnická a gynekologická klinika
LF UK a FN
Sokolská 581
500 05 Hradec Králové
e-mail: dvorino@centrum.cz
Sources
1. Desouza, R., Shapiro, A., Westney, OL. Adductor brevis myositis following transobturator tape procedure: a case report and review of the literature. Int Urogynecol J Pelvic Floor Dysfunct, 2007, 18, p. 817–820.
2. Flam, F., Boijsen, M., Lind, F. Necrotizing fasciitis following transobturator tape treated by extensive surgery and hyperbaric oxygen. Int Urogynecol J Pelvic Floor Dysfunct, 2009, 20, p. 113–115.
3. Milam, MR., Stauble, E., Milam, RA. Atypical presentation of abdominal group A streptococcal-necrotizing fasciitis after pessary removal. Int Urogynecol J Pelvic Floor Dysfunct, 2012, 23, p. 241–242.
4. Trent, JT., Kirsner, RS. Diagnosing necrotizing fasciitis. Adv Skin Wound Care, 2002, 15, p. 135–138.
5. Wong, CH., Khin, LW. Clinical relevance of the LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score for assessment of early necrotizing fasciitis. Crit Care Med, 2005, 33, p. 1677.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicine
Article was published inCzech Gynaecology

2016 Issue 6-
All articles in this issue
- Current options of preimplantion genetic screening and preimplantation genetic diagnostics
- Mutations in genes affecting fertility of men – current routine laboratory genetic diagnostics and searching for more DNA segments and genes influencing spermatogenesis
- The role of trefoil factor family in gynecological disease
- The possibility of using progesterone receptor modulators in the treatment of myomas
- Sarcoidosis of the female genital tract
- Breast self-examination. Yes or no?
- Coeliac disease as a possible cause of some gynecological and obstetric abnormalities
- Cesarean section incidence and vaginal birth success rate at term pregnancy after myomectomy
- Cesarean scar ectopic pregnancy
- Pregnancy in women with congenital bleeding disorder
- Original Bishop score with modifications
- Necrotic fasciitis of the lateral muscle group of the thigh following outside-in transobturatory tape procedure
- Czech Gynaecology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Original Bishop score with modifications
- Cesarean scar ectopic pregnancy
- Breast self-examination. Yes or no?
- Coeliac disease as a possible cause of some gynecological and obstetric abnormalities
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career