-
Medical journals
- Career
Eyelid Schwannoma. A Case Report
Authors: S. Sheikhghomi; M. Shafaat; H. Hasani
Authors‘ workplace: Department of Ophthalmology, Madani Hospital, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran
Published in: Čes. a slov. Oftal., 3, 2023, No. Ahead of Print, p. 1001-1011
Category: Case Report
doi: https://doi.org/10.31348/2023/34Overview
In this case report, we describe a 53-year-old woman who presented with a slow-growing lower lid mass in her right eye. On gross examination, a remarkable lower lid bulging was noted. On palpation, a subcutaneous oval-shaped mass with a firm consistency, measuring about 2cm, was noted. The uncorrected visual acuities of the patient were 20/20 (by Snellen chart) bilaterally, and the examinations of the anterior and posterior segments of both eyes were unremarkable. On the orbital Computed Tomography scan of the patient, a solitary and homogenous solid globular mass with the same density of the brain tissue was obvious. The patient underwent surgical excision. Microscopic assessment of the lesion revealed a biphasic hypercellular area (Antoni A) and myxoid hypocellular areas (Antoni B), containing slender cells with tapered ends, interspersed with collagen fibers, consistent with a diagnosis of schwannoma. In addition, some foci of nuclear palisading around the fibrillary process (Verocay bodies) could frequently be found throughout the highly cellular regions. Schwannomas rarely occur in the eyelids, but have clinical and paraclinical indicators which indicate the probable diagnosis. In conclusion, we suggest that eyelid schwannoma be considered as an element of the differential diagnoses list for subcutaneous lesions of the eyelid.
Keywords:
tumor – schwannoma – eyelid – mass
INTRODUCTION
The peripheral nervous system is enriched with neural crest-derived glial cells, known as Schwannoma cells (SCs) or Neurolemmocytes. In general, these cells participate in myelination, nourishment and regeneration of the peripheral nerves. Schwannoma cells may produce a sheath of myelin around a single thick nerve fiber (myelinating SCs), or simply wrap around the multiple thin nerve fibers (non-myelinating SCs) [1,2]. Excessive proliferation of schwannoma cells may lead to formation of the mostly benign and encapsulated tumors called Schwannoma or Neurilemmoma. The most common locations for the occurrence of schwannomas are the head and neck, particularly those arising from the vestibulocochlear nerve and peripheral nerves in the extremities including brachial plexus and sciatic nerves. Eyelid schwannomas account for a rare site of these tumors. In this case report, we describe a case of eyelid schwannoma and also provide a summarized review of the clinical and paraclinical features of this unusual entity [1–4].
CASE PRESENTATION
A 53-year-old woman presented with a slow-growing lower lid mass in her right eye, starting from 1 year ago. She had no further complication of pain or reduced vision. She also denied any history of systemic diseases or previous surgeries. On gross examination, a remarkable lower lid bulging, associated with lower lid mechanical ptosis without cutaneous changes was apparent. On closer examination under a bright light, 2 vertical and engorged subcutaneous small vessels could be detected over the lesion. On palpation, a subcutaneous oval-shaped mass with a firm consistency and measuring about 2cm was noted. The lesion was non-tender, but mobile in both the horizontal and vertical directions. The sensation of the lower lid was intact. The uncorrected visual acuities of the patient were 20/20 (by Snellen chart) bilaterally, and the examinations of the anterior and posterior segments of both eyes were unremarkable. Moreover, relative apparent pupillary deficit (RAPD) was negative and eye movements were unlimited. On the orbital Computed Tomography (CT) scan of the patient, a solitary and homogenous solid globular mass, with the same density of the brain tissue overlying the right lower orbital rim, with extension toward the anterior face of the lower lid tarsus and margin was evident, lacking bone invasion or extension toward the orbital space (Figure 1).
The patient underwent excisional surgery with local sedation. A horizontal 2.5 cm incision was made with a 15.0 blade over the lesion. Subcutaneous dissection and hemostasis were performed by scissors and cauterization. An encapsulated smooth lesion was excised totally and sent for pathological investigation (Figure 2). The macroscopic evaluation of the lesion reported an encapsulated round gray mass, measuring 2×1.5×1.5 cm in cut sections, with an apparent homogenous grayish pattern with some foci of hemorrhage. On microscopic assessment of the lesion, a biphasic hypercellular area (Antoni A) and myxoid hypocellular areas (Antoni B), containing narrow, elongated and wavy cells with tapered ends interspersed with collagen fibers were obvious (Figure 3). In addition, some foci of nuclear palisading around the fibrillary process (Verocay bodies) could frequently be seen in highly cellular areas (Figure 4). Several sections of blood-filled small vessels were also evident. Fortunately, the post-op period of the patient was uneventful and no recurrences occurred after 1-year follow-up.
1. Spiral orbital CT scan (without contrast) in axial (A) and saggital (B) views showing a homogenous, well-defined solid mass in the right lower lid 
2. The patient’s right lower eyelid appearance immediately before the surgery (A) and the Excised lesion (B) 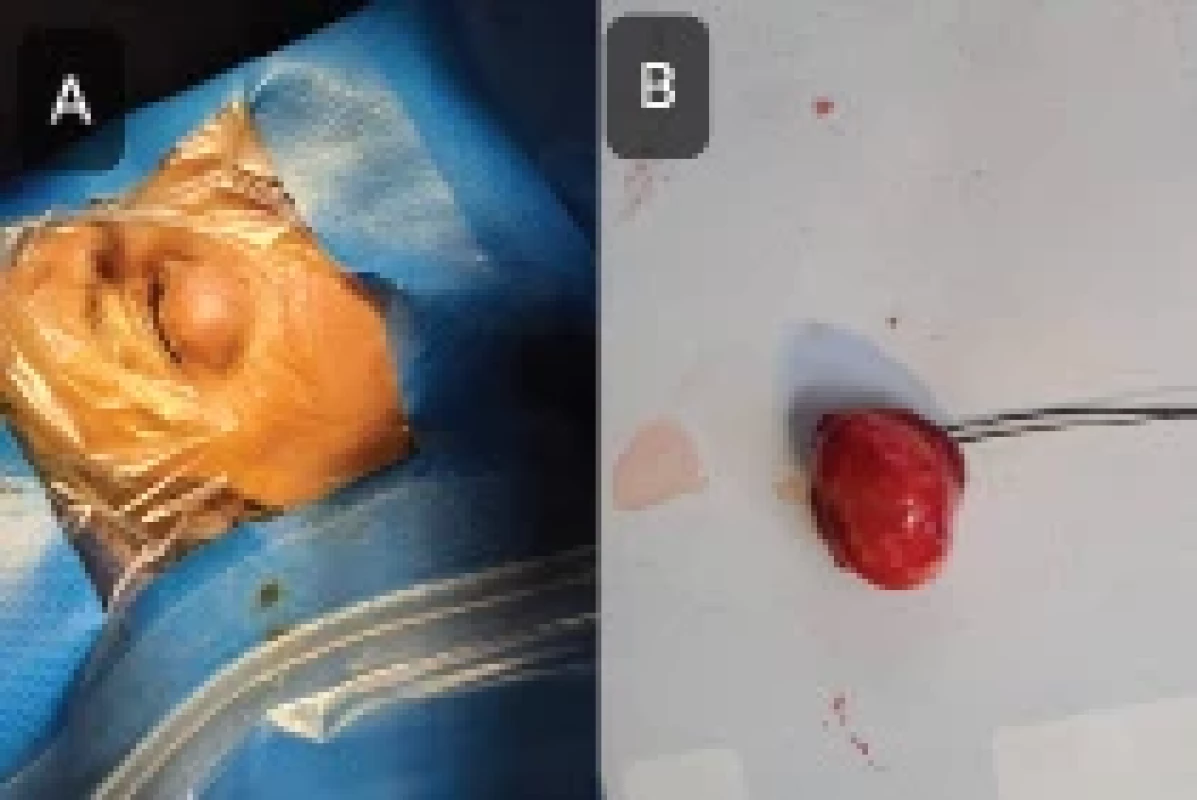
3. Low (left) and high (right) microscopic magnification of the lesion showing a biphasic pattern of hypercellular (Antony A) and hypocellular (Antony B) areas with a surrounding capsule (C). H & E: Hematoxillin and Eosin 
4. This image shows verocay bodies including the palisading of the schwann cells nuclei with an arrangement in rows and separated by pinkish fibrillary processes. H & E: Hematoxillin and Eosin 
DISCUSSION
Schwannomas are most often characterized as encapsulated benign tumors, which have been reported as isolated tumors in the orbit, uvea, sclera and conjunctiva. However, they extremely rarely occur in the eyelids. These lesions usually arise sporadically and as a solitary, eccentric lesion from the related nerve in the 5th and 6th decades. Nonetheless, they can form in children as well, and involve both genders equally [4,7,10] The incidence of multiple tumors, either in the same location or different regions of the body, needs a systemic evaluation to assess precipitating genetic disorders, such as neurofibromatosis [5–12].
In the clinical appearance of eyelid schwannomas, the firm consistency due to a solid fibro-cellular content accompanied by smooth borders, owing to the capsular coverage, along with a gradual growth are the main diagnostic clues of these tumors. Nevertheless, there are some reports of small lid margin schwannomas which may mimic an eyelid papilloma or hydrocystoma in appearance [13–18]. Regarding the imaging features on CT scan, a well circumscribed and usually homogenous lesion without bony erosion is seen, as in our case. The lesions also show intense enhancement, which may be heterogeneous in larger ones. Adjacent bone remodeling may be present in some long-lasting cases. In magnetic resonance imaging (MRI), the lesions are isointense or hypointense in T1 and hyperintense in T2. Again, in MRI, with contrast, they enhance strongly, especially more in the periphery and less centrally [19].
Complications of eyelid schwannomas are usually related to mechanical ptosis, cosmetic effects and maybe visual obstruction [6–17]. Total excision of the tumor via surgery and, preferably with sparing of the capsular integration, is the mainstay of treatment. In terms of the microscopic appearance, alternative areas of high and low density of spindle-shaped cells are evident, which correspond to the histopathological terms of Antoni type A and Antoni type B, respectively (Figure 3). Furthermore, Verocay bodies constitute a characteristic finding, in which palisading of several nuclei are demonstrated around an acellular area (Figure 4). In cases with atypical microscopy, immunohistochemical staining for S-100 antigen will be addressed, which would be strongly stained positive in schwannomas.
In conclusion, we suggest that eyelid schwannoma be considered as an element of the differential diagnoses list for subcutaneous lesions of the eyelid.
Ethics
The patient's consent for the anonymous reporting of her clinical information in the paper was obtained.
Sima Sheikhghomi MD.
Department of Ophthalmology, Faculty of Medicine,
Alborz University of Medical Sciences
Karaj
3149779453 Iran
E-mail: sshaikhghomi@yahoo.comThe authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceutical company. The study has not been submitted to another journal and is not printed elsewhere, with the exception of congress summaries and recommended procedures.
Received: March 18, 2023
Accepted: June 15, 2023
Sources
- Mirsky R, Jessen KR. The neurobiology of Schwann cells. Brain pathol 1999;9(2):293-311. https://doi.org/10.1111/j.1750-3639.1999.tb00228.x
- Pandey S, Mudgal J. A review on the role of endogenous neurotrophins and schwann cells in axonal regeneration. J Neuroimmune Pharmacol. 2021;1-11. https://doi.org/10.1007/s11481-021-10034-3
- Gupta TKD, Brasfield RD, Elliot WS, Hajdu SI. Benign solitary schwannomas (neurilemomas). Cancer. 1969;24(2):355-366. https://doi.org/10.1053/j.jfas.2016.12.003
- Onaran Z, Ornek K, Yilmazbas P, Bozdogan O. Schwannoma of the lower eyelid in a 13-year-old girl. Ophthalmic Plast Reconstr Surg. 2009;25(1):50-52. http://doi: 10.1097/IOP.0b013e3181936826
- Brown-joel Z, Esmaili N, Hong S, Young K, Wanat K. Eyelid schwannomas with associated neoplasms: A report of 2 cases. JAAD Case Rep. 2022;30 : 56-58. https://doi.org/10.1016/j.jdcr.2022.10.004
- Shibata N, Kitagawa K, Noda M, Sasaki H. Solitary neurofibroma without neurofibromatosis in the superior tarsal plate simulating a chalazion. Ger J Ophthalmol. 2012;250(2):309. http://doi:10.1007/s00417-010-1593-5
- Ittarat M, Srihachai P, Chansangpetch S. Case report of eyelid schwannoma: A rare presentation in a child. Am J Ophthalmol Case Rep. 2019;13 : 56-58. https://doi.org/10.1016/j.ajoc.2018.12.005
- Touzri RA, Errais K, Zermani R, Benjilani S, Ouertani A. Schwannoma of the eyelid: apropos of two cases. Indian J Ophthalmol Case Rep. 2009;57(4):318.
- López-Tizón E, Mencía-Gutiérrez E, Gutiérrez-Díaz E, Ricoy JR. Schwannoma of the eyelid: report of two cases. JAMA Dermatol. 2007;13(2). https://doi.org/10.5070/D33s09x4kn
- Kimura K, Tanaka T, Edagawa H, Goto H. A case of eyelid schwannoma in a child. Jpn J Ophthalmol. 2010;54 : 635-636. http://doi.org/10.1007/s10384-010-0880-3
- Ho DK-Hong, Shah V, Obi EE. Giant eyelid schwannoma. Digit J Ophthalmol. 2018;1(11) http://djo.harvard.edu/index.php/djo/article/view/274
- Singh S, Saraf S, Goswami D, Singh S. Case Report of Isolated Schwannoma - A Rare Eyelid Tumor. Ocul Oncol Pathol. 2014;7(2):143-145. http://doi.org/10.17925/USOR.2014.07.02.143
- Morsi NH, Almansouri OS, Almansour EM. Isolated eyelid Schwannoma: A rare differential diagnosis of lid tumor. Saudi J Ophthalmol. 2017;31(2):112-114. https://doi.org/10.1016/j.sjopt.2017.02.005
- Magdum RM, Paranjpe R, Kotecha M, Pallavi P. Solitary eyelid schwannoma. Med J DY Patil Vidyapeeth. 2014;7(4):502. http://doi.org/10.4103/0975-2870.135286
- Lee KW, Lee MJ, Kim NJ, Choung HK, Wook K, et al. A Case of Eyelid Schwannoma. J Korean Ophthalmol Soc.2009;50(2):290-293. https://doi.org/10.3341/jkos.2009.50.2.290
- Cheng KH, Karres J, Kross Jm, Kijlstra J, Dekken V, Herman. Cyst-like schwannoma on the eyelid margin. J Craniofac Surg. 2012;23(4):1215-1216. http://doi: 10.1097/SCS.0b013e3182564ace
- Siddiqui MA, Leslie T, Scott C, Mackenzie J. Eyelid schwannoma in a male adult. J Clin Exp Ophthalmol. 2005;33(4):412-413. https://doi.org/10.1111/j.1442-9071.2005.01035.x
- Mun YS, Kim N, Choung Ho K, Khwarg SI. Eyelid Schwannoma Mimicking Eyelid Amelanotic Nevus. Korean J Ophthalmol. 2019;33(5):478-480. https://doi.org/10.3341/kjo.2018.0123
- Skolnik AD, Loevner LA, Sampathu DM et-al. Cranial Nerve Schwannomas: Diagnostic Imaging Approach. Radiographics. 2016;36(5):150199. http://doi:10.1148/rg.2016150199
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2023 Issue Ahead of Print-
All articles in this issue
- CURRENT VIEW OF THE SPECTRUM OF PACHYCHOROID DISEASES. A REVIEW
- ULTRASOUND EXAMINATION OF THE ORBIT IN PATIENTS WITH THYROIDASSOCIATED ORBITOPATHY – EXAMINATION GUIDE AND RECOMMENDATIONS FOR EVERYDAY PRACTICE. A REVIEW
- COMPUTER TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING OF THE ORBIT IN THE DIAGNOSIS AND TREATMENT OF THYROID-ASSOCIATED ORBITOPATHY – EXPERIENCE FROM PRACTICE. A REVIEW
- DETERMINATION OF CORNEAL POWER AFTER REFRACTIVE SURGERY WITH EXCIMER LASER: A CONCISE REVIEW
- Eyelid Schwannoma. A Case Report
- The Current State of Artificial Intelligence in Neuro-Ophthalmology. A Review
- Central Serous Chorioretinopathy. A Review
- Therapy for Vitreous Seeding Caused by Retinoblastoma. A Review
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Central Serous Chorioretinopathy. A Review
- ULTRASOUND EXAMINATION OF THE ORBIT IN PATIENTS WITH THYROIDASSOCIATED ORBITOPATHY – EXAMINATION GUIDE AND RECOMMENDATIONS FOR EVERYDAY PRACTICE. A REVIEW
- CURRENT VIEW OF THE SPECTRUM OF PACHYCHOROID DISEASES. A REVIEW
- COMPUTER TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING OF THE ORBIT IN THE DIAGNOSIS AND TREATMENT OF THYROID-ASSOCIATED ORBITOPATHY – EXPERIENCE FROM PRACTICE. A REVIEW
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

