-
Medical journals
- Career
VISUAL OUTCOMES, CONTRAST SENSITIVITY, AND SATISFACTION WITH MULTIFOCAL INTRAOCULAR LENS BLENDED TECHNIQUE: LATE MID-TERM RESULTS
Authors: NA. Blanco 1,2,3; A. Tello 1,2,4,5; V. Galvis 1,4,5; E. Mendoza Mogollón 2
Authors‘ workplace: Ophthalmology Foundation of Santander - Carlos Ardila Lulle (FOSCAL), Floridablanca, Colombia 1; Industrial University of Santander (UIS), Bucaramanga, Colombia 2; Santa Lucía Ophthalmology Clinic, Medellín, Colombia 3; Autonomous University of Bucaramanga (UNAB), Bucaramanga, Colombia 4; Virgilio Galvis Eye Center, Floridablanca, Colombia 5
Published in: Čes. a slov. Oftal., 79, 2023, No. 2, p. 80-85
Category: Original papers
doi: https://doi.org/10.31348/2023/13Overview
Purpose: To describe clinical visual outcomes, spectacle independence, and patient satisfaction after cataract surgery with blending implantation of ReSTOR (Alcon laboratories) multifocal intraocular lenses.
Material and Methods: A single-arm, non-randomized prospective study assessed patients undergoing cataract surgery with ReSTOR® +2.50 intraocular lens in the dominant eye and +3.00 add in the fellow eye between January 2015 to January 2020.
Results: In total, 47 patients (94 eyes) were enrolled, 28 women and 19 men. The average age at surgery time was 64 ±8 years, average postoperative follow-up was 45.4 ±7.0 months, with a minimum of 18.9 months. Postoperative binocular uncorrected distance visual acuity (UDVA) was on average 0.07 logMar (Snellen 20/24), uncorrected binocular intermediate visual acuity at 65 cm was 0.07 logMar (20/24), uncorrected binocular near visual acuity at 40 cm was 0.06 logMar (20/23). Contrast sensitivity under photopic and scotopic conditions, with and without glare, remained at the upper limit of normality. 98% of patients were quite satisfied or very satisfied. 87% did not require glasses for any activities, either at distant vision, nor at near vision.
Conclusions: Cataract surgery with ReSTOR® IOL blended vision showed medium-term satisfactory visual results, achieving spectacle independence and a high level of satisfaction.
Keywords:
Cataract surgery – intraocular lens – ReSTOR – blended vision – spectacle independence
INTRODUCTION
Cataract surgery is the most performed surgical procedure in developed countries, while in developing countries, cataracts are still the first cause of preventable and reversible blindness [1].
For the past 25 years, cataract treatment has moved on, due to surgical techniques’ improvements and the worldwide availability of intraocular lenses (IOLs), resulting in an increased rate of cataract surgery, and the number of people with pseudophakia in the world, although imbalances in cataract service providing are still evident between countries with high or low income [2,3].
Among IOL types, there are monofocal and multifocal, and more recently what are called “extended depth of focus” (EDOF) lenses. Monofocal IOLs (either spherical, aspherical or toric) show good outcomes in terms of uncorrected distance vision, but are limited in uncorrected near vision. Multifocal IOLs include bifocal and trifocal platforms. The former models allow near (around 40 cm) and distance vision to be corrected, and the latter have an additional focus for intermediate distance (around 65 cm). In addition, some bifocal models have lower addition power, in order to cover the intermediate distance, including the ReSTOR® +2.5 (Alcon laboratories, Fort Worth, TX, USA), which has an effective addition of around +1.75 D at corneal plane. EDOF IOLs are a newer alternative, which through various technologies extend focus and far vision to cover also the intermediate distance [4].
This study aimed to assess the binocular visual outcomes after ReSTOR® multifocal IOL implantation, +2.50 add in the dominant eye and +3.00 add in the fellow eye, as well as to evaluate patients’ level of satisfaction after surgery.
MATERIAL AND METHODS
A single-arm, non-randomized prospective study was performed to assess cataract surgery pre - and postsurgical changes with ReSTOR +2.50 multifocal non-toric IOL in the dominant eye and +3.00 add in the fellow eye, between January 2015 to January 2020, at Centro Oftalmológico Virgilio Galvis in Floridablanca, Colombia.
Patients who had intra - and postoperative complications were excluded. Likewise, those who had eye pathology other than cataracts, such as glaucoma, corneal or retinal diseases, which could influence visual outcomes, were excluded.
Postoperative evaluation, at least one month after surgery, included measurement of visual acuity, contrast sensitivity, satisfaction level and quality of vision, refractive results, as well as corrected visual acuity (distance, intermediate and near). Quality of vision was measured using a validated questionnaire [5].
A descriptive analysis was performed in Stata V 11.0 software, with a 5% significance level. Quantitative variables were summarized in absolute values and percentages, while qualitative variables were submitted graphically. Central tendency and data dispersion indicators were analyzed; mean, median, standard deviation, and range.
This study adhered to the tenets of the Declaration of Helsinki and was approved by the local Ethics Committee.
RESULTS
This study included a total of 47 patients (94 eyes), 28 women and 19 men. The average age at surgery time was 64 ±8 years, average postoperative follow-up was 45.4 ±7.0 months, with a minimum of 18.9 and a maximum of 63.1 months.
No patient had intraoperative or postoperative complications (2 presented transient corneal edema that resolved after 2 weeks). 6 patients were excluded from the study due to pre-existing co-morbidities: 4 had glaucoma, and 2 severe dry eye disease.
Postoperative binocular uncorrected distance visual acuity (UDVA) was on average 0.07 logMar (Snellen 20/24), uncorrected binocular intermediate visual acuity at 65 cm was 0.07 logMar (20/24), uncorrected binocular near visual acuity at 40 cm was 0.06 logMar (20/23).
Postoperative binocular uncorrected visual acuity of 20/25 or better was achieved in 38 out of 47 (81%) patients for distance vision, 38 out of 47 (81%) patients for intermediate vision, and 41 out of 47 (87%) patients for near vision.
The average of mean keratometry manual data, as well as pre - and postoperative keratometric cylinder are summarized in Table 1. There were no statistically significant differences among pre - and postoperative values of these measurements (p values 0.84 and 0.12, respectively).
1. Pre- and postoperative mean keratometry and keratometric astigmatism 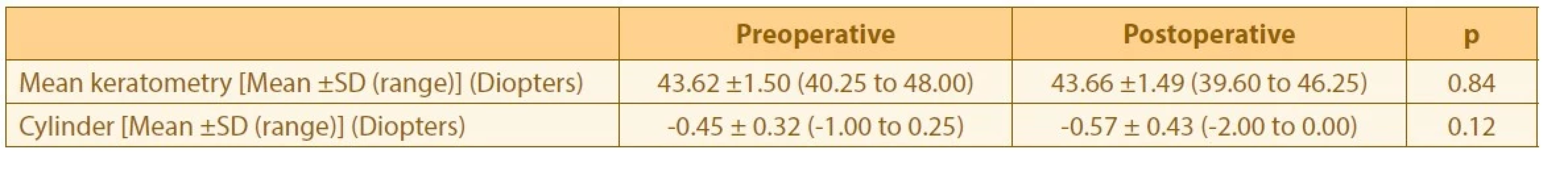
Incision-induced astigmatism centroid was 0.31 diopters (D) at 180 °, and the arithmetic mean of its magnitude was 0.57 ±0.44 D.
Regarding postoperative refraction, sphere showed an average of 0.20 ±0.40 diopters (D), and cylinder -0.34 ±0.48 D. Average spherical equivalent (SE) was 0.03 ±0.43 D, and defocus equivalent was 0.48 ±0.46 D. 89% of the eyes had a SE ±0.50 D and 71% of the eyes a cylinder ±0.50 D.
Contrast sensitivity levels under photopic and scotopic conditions, with and without glare, remained at the upper limit of normality (to ≥60 years old patients), or a little above normality average under scotopic conditions with glare for high spatial frequencies [6].
The satisfaction survey showed that 89% of patients felt very satisfied with their vision after surgery, and 98% of patients were quite satisfied or very satisfied. Only 2% reported being quite dissatisfied (1 patient), and none of the patients referred to being very dissatisfied (Graph 1). 88% considered that their postsurgical vision did not cause difficulties in their daily lives.
Graph 1. Satisfaction level with surgery 
After surgery, 87% of patients never wore glasses for any activity, either for distance vision, or for near vision. Graph 2 shows the results for postoperative spectacle use at both working distances.
Graph 2. Spectacles use after surgery for near and distance vision 
Satisfaction survey outcomes with the Catquest-9sf Questionnaire on difficulties with some specific activities are summarized in Graph 3.
Graph 3. Perceived difficulty in particular activities 
DISCUSSION
Bifocal intraocular lenses with additions around +3.00 D at the intraocular lens plane were designed to improve near vision, while maintaining a good distance vision period after cataract surgery. However, it is evident that people today have requirements for activities at intermediate vision. More recently, bifocal IOL with lower addition power were designed, in order to cover the need for focusing at distances around 60 or 70 cm of the eye (with a +2.50 D addition at intraocular lens plane, which corresponds approximately to between +1.75 and +1.90 D at spectacles’ plane).
In our Clinic, approximately 22% of patients that undergo cataract surgery are implanted with multifocal or EDOF IOLs. In our institution, in a previous group of 33 patients who had ReSTOR +3.00 Add IOLs bifocal implanted binocularly (unpublished results), although all reported being satisfied with the results, only 63.6% reported being very satisfied. Thus, we decided to use the blended vision alternative, hoping to increase the level of patient satisfaction.
Pedrotti et al. reported on ReSTOR +2.50 D y ReSTOR +3.00 D bilateral implantation and found that there was better intermediate vision and quality vision with the lower addition lens compared with the higher one. The multifocal +3.00 D lens showed the best near visual outcomes at a 40 cm distance. The multifocal +2.50 D lens and the extended view range lens (Tecnis Symfony) provided significantly better intermediate visual outcomes than the +3.00 D addition lens. A greater spectacle independence was evidenced with the +2.50 D addition multifocal lens and the extended viewing range lens (p < 0,001) [7].
The +2.50 D addition bifocal lenses provide good intermediate and near vision for patients, with less risk of visual symptoms such as halos and glare, more associated with the +3.00 D addition bifocal lens [8]. Using the +3.00 D ReSTOR lens in a group of patients, between 13% and 14% of them reported glare or “severe”’ glare, night vision problems, or halos’ vision [9]. However, some studies found that the lower addition lens did not offer a clear intermediate vision advantage, compared to the higher addition lens, in patients with binocular implantation of the same kind of lens [10,8].
An additional alternative that emerged with these types of lower addition intraocular lenses, was the combination of the two types of addition in the same patient, implanting a lens with the addition of +2.50 in the dominant eye and +3.00 in the non-dominant eye, to achieve the greater possibility of a spectacle independence at the three distances.
A Brazilian study analyzed the visual acuity outcomes, defocus curves, and contrast sensitivity in 20 patients, comparing ReSTOR +2.50 D and ReSTOR +3.00 D combination, versus the bilateral trifocal lens implantation (Panoptix). It obtained similar outcomes in both groups. Questionnaires about subjective quality vision did not find consistent differences between the two groups [11].
Blehm et al. recently reviewed the results of refraction, visual acuity, defocus curve, and subjective visual quality after trifocal toric IOL with a moderate addition (+2.50 D) in the dominant eye, and a higher addition (+3.00 D) to the non-dominant eye. 55% of patients expressed complete satisfaction with their vision. Residual refractive astigmatism was ≤ 0.50 D in 100% of the eyes. No subject had an uncorrected binocular visual acuity worse than 0.2 logMar (20/32 Snellen) at any distance. 75% of the subjects had an uncorrected binocular visual acuity of 0.10 logMar (20/25 Snellen) at all three distances. The majority of the subjects (22/29, 76%) reported that they were not bothered by any visual disturbances, like glare or halos. The authors concluded that the modality of combined bifocal lens seems to be well tolerated by subjects, with a good range of vision and minimal discomfort due to visual disturbances [12].
Podborączyńska-Jodko et al. published a study including 40 eyes of 20 patients with the blended technique. Three months after binocular surgery, binocular UIVA was logMar 0.08. Binocular UDVA was equal to logMar 0.1 or better in all cases. Binocular near visual acuity average was logMar 0.07, and all patients had a better near vision than logMar 0.3. [13]. These values were almost the same as the visual acuity values found in the present study.
Contrast sensitivity under photopic and scotopic conditions was at age-normal limits. All patients were spectacle independent [13]. This was also in very close agreement with the present study. In the present study, 87% of patients did not need spectacles for distance and near vision, 8.5% occasionally required them to read closely and 4.2% occasionally used them for distance vision.
In addition, the mean spherical equivalent was almost zero, and mean defocus equivalent was lower than 0.5 D, indicating good performance in terms of biometric calculations and refractive results.
The level of patient satisfaction in the present study was high. 89% answered that their vision after surgery did not cause any difficulty in their daily life. In addition, 85% of patients indicated that they felt very satisfied with their vision and 13% were quite satisfied.
In our study, with the +2.50 / +3.00 lens combination, a lower percentage (only 2%) of patients reported frequent spectacles’ use for near vision, compared to the 11% reported by Honavesian et al. The visual requirement differences of the two studied groups of patients (older adults at Colombia versus older adults in the United States) may be related to the lower spectacles’ need of the patients included in the present study [14].
The approach of combining different platforms (Mixand - Match) to add the advantages of them, have been used for a while, and is being explored. Lee et al. reported in 2021 that 37 patients underwent a combined vision approach, with an EDOF IOL implant (TECNIS Symfony) in the dominant eye and a bifocal IOL (TECNIS IOL +3.25 DMF) in the fellow eye. Mean uncorrected distance, intermediate, and near binocular visual acuities were 20/21, 20/22, and 20/27, respectively. 81.1% of the patients reported being more than satisfied with near vision, but 21.6 % complained of severe glare and halo. 91.9% of the patients achieved independence of near-vision glasses [15].
Furthermore, particularly with the EDOF platform, the approach of mini-monovision (with addition power for near between +0.50 and +0.75 D) has recently been used. Bala et al., in their multicenter study with the EDOF Vivity lens, performed a post hoc analysis comparing patients who ultimately had a result of mini-monovision (at least 0.50 D plus myopia in one eye, and with a spherical equivalent of at least -0.25 D or more myopia), compared with those who achieved bilateral emmetropia. They found that median binocular uncorrected intermediate visual acuity and uncorrected near visual acuity were better by almost 1 line in the mini-monovision patients. [16]
Newsom and Potvin published the results of 33 patients who underwent bilateral Vivity EDOF IOL implantation, with a target of emmetropia in the dominant eye and a myopic refraction of -0.75 D in the non-dominant eye. 88% of cases achieved an uncorrected binocular near acuity of 20/30 or better. Satisfaction with vision at all three distances was high. They found that the near vision was more than 1 line better than was reported in previous published studies where the target refraction was bilateral emmetropia, and also found higher rates of spectacle independence at near than for a comparative dataset from previous studies for the same EDOF IOL but without the monovision approach [17].
Van Amelsfort et al. recently reported the results of 22 patients targeted for mini-monovision with the Vivity EDOF IOL (calculated to be between -0.25 D and -0.50 D). Mean uncorrected distance, intermediate, and near binocular visual acuities were 20/24, 20/22, and 20/34, respectively. With regard to spectacle independence, 96% of the patients reported never or rarely using spectacles for distance vision, 68% for intermediate vision, but only 38% for near vision [18].
It is important to note that, although in recent years trifocal IOL have gained popularity, in a recent meta-analysis the authors concluded that there is evidence, but of a low level, that, compared to bifocal IOL, the implantation of trifocal lenses may improve uncorrected intermediate visual acuity. However, there is no evidence of a difference between trifocal and bifocal lenses for UDVA and UNVA [19]. Recent studies, however, suggested that PanOptix trifocal IOLs may lead to higher total independence of eyeglasses [20,21]. Further studies on this topic are warranted, particularly using combined approaches (Mix-and-Match), or blended vision.
CONCLUSION
Cataract surgery with the ReSTOR ® IOL blended technique showed satisfactory visual outcomes in the medium term, achieving independence of spectacles and a high level of satisfaction. Therefore, this approach could still be maintained as an alternative option to trifocal intraocular lenses in patients who seek complete independence from glasses for the different distances.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceutical company.
Received: November 16, 2022
Accepted: January 20, 2023
Available on-line: March 30, 2023
Nicolás Alberto Blanco, MD
Clínica de Oftalmología Santa Lucía
Carrera 43.ª #14-72
Medellín
Colombia
E-mail: nblancogarcia@gmail.com
Sources
1. Wang W, Yan W, Fotis K, et al. Cataract Surgical Rate and Socioeconomics: A Global Study. Invest Ophthalmol Vis Sci. 2016 Nov1;57(14):5872-5881.
2. Foster A, Gilbert C, Johnson G. Changing patterns in global blindness: 1988-2008. Community Eye Health. 2008;21(67):37-39.
3. Yan W, Wang W, van Wijngaarden P, Mueller A, He M. Longitudinal changes in global cataract surgery rate inequality and associations with socioeconomic indices. Clin Experiment Ophthalmol. 2019 May;47(4):453-460.
4. Breyer DRH, Beckers L, Ax T, Kaymak H, Klabe K, Kretz FTA. [Current Review: Multifocal Intraocular Lenses and Extended Depth of Focus Intraocular Lenses]. Klin Monbl Augenheilkd. 2020 Aug;237(8):943-957.
5. Lundström M, Llovet F, Llovet A, et al. Validation of the Spanish Catquest-9SF in patients with a monofocal or trifocal intraocular lens. J Cataract Refract Surg. 2016 Dec;42(12):1791-1796.
6. Hohberger B, Laemmer R, Adler W, Juenemann AGM, Horn FK. Measuring contrast sensitivity in normal subjects with OPTEC® 6500: influence of age and glare. Graefes Arch Clin Exp Ophthalmol. 2007 Dec;245(12):1805-1814.
7. Pedrotti E, Carones F, Aiello F, et al. Comparative analysis of visual outcomes with 4 intraocular lenses: Monofocal, multifocal, and extended range of vision. J Cataract Refract Surg. 2018 Feb;44(2):156-167.
8. Gundersen KG, Potvin R. Comparative visual performance with monofocal and multifocal intraocular lenses. Clin Ophthalmol. 2013 Oct;7 : 1979-1985. doi:10.2147/OPTH.S52922
9. Hovanesian JA. Patient-reported outcomes of multifocal and accommodating intraocular lenses: analysis of 117 patients 2-10 years after surgery. Clin Ophthalmol. 2018 Nov;12 : 2297-2304. doi: 10.2147/OPTH.S182943
10. Vingolo EM, Carnevale C, Fragiotta S, Rigoni E, Iacobelli L. Visual Outcomes and Contrast Sensitivity after Bilateral Implantation of Multifocal Intraocular Lenses with +2.50 or +3.0 Diopter Addition: 12-Month Follow-Up. Semin Ophthalmol. 2017;32(5):588-592.
11. Vilar C, Hida WT, de Medeiros AL, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol. 2017 Aug;11 : 1393-1397. doi: 10.2147/OPTH.S139909
12. Blehm C, Potvin R. Evaluating Refractive and Visual Outcomes After Bilateral Implantation of an Apodized Diffractive Multifocal Toric Intraocular Lens with a Moderate Add in the Dominant Eye and a Higher Add in the Fellow Eye. Clin Ophthalmol. 2020 Apr;14 : 1035-1041. doi: 10.2147/OPTH.S246271
13. Podborączyńska-Jodko K, Lubiński W, Post M. Intermediate vision and other visual function parameters in patients after uneventful cataract surgery with implantation of diffractive intraocular lenses using the blending procedure. Klin Oczna. 2020;122(2):49-53.
14. Hovanesian JA, Lane SS, Allen QB, Jones M. Patient-Reported Outcomes/ Satisfaction and Spectacle Independence with Blended or Bilateral Multifocal Intraocular Lenses in Cataract Surgery. Clin Ophthalmol. 2019 Dec;13 : 2591-2598. doi: 10.2147/OPTH.S227629
15. Lee JH, Chung HS, Moon SY, et al. Clinical Outcomes after Mixand - Match Implantation of Extended Depth of Focus and Diffractive Multifocal Intraocular Lenses. J Ophthalmol. 2021 Aug;2021 : 8881794. doi:10.1155/2021/8881794
16. Bala C, Poyales F, Guarro M, et al. Multicountry clinical outcomes of a new nondiffractive presbyopia-correcting IOL. J Cataract Refract Surg. 2022;48(2):136-143. doi:10.1097/j.jcrs.0000000000000712
17. Newsom TH, Potvin R. Evaluation of Quality of Vision and Visual Outcomes with Bilateral Implantation of a Non-Diffractive Extended Vision Intraocular Lens with a Target of Slight Myopia in the Non-Dominant Eye. Clin Ophthalmol. 2022 Jan;16 : 183-190. doi:10.2147/OPTH.S350850
18. Amelsfort T, Webers VSC, Bauer NJC, Clement LHH, van den Biggelaar FJHM, Nuijts RMMA. Visual outcomes of a new nondiffractive extended depth-of-focus intraocular lens targeted for minimonovision: 3-month results of a prospective cohort study. J Cataract Refract Surg. 2022;48(2):151-156. doi:10.1097/j. jcrs.0000000000000825
19. Zamora-de La Cruz D, Zúñiga-Posselt K, Bartlett J, Gutierrez M, Abariga SA. Trifocal intraocular lenses versus bifocal intraocular lenses after cataract extraction among participants with presbyopia. Cochrane Database Syst Rev. 2020 Jun;6(6):CD012648.
20. Hovanesian JA, Jones M, Allen Q. The PanOptix Trifocal IOL vs the ReSTOR 2.5 Active Focus and ReSTOR 3.0-Add Multifocal Lenses: A Study of Patient Satisfaction, Visual Disturbances, and Uncorrected Visual Performance. Clin Ophthalmol. 2021 Mar;15 : 983 - 990. doi: 10.2147/OPTH.S285628
21. Galvis V, Escaf LC, Escaf LJ, et al. Visual and satisfaction results with implantation of the trifocal Panoptix® intraocular lens in cataract surgery. J Optom. 2022 Jul-Sep;15(3):219-227.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2023 Issue 2-
All articles in this issue
- Zprávy
- TRAUMA-RELATED ACUTE MACULAR NEURORETINOPATHY. A CASE REPORT
- FORMS OF OCULAR LARVAL TOXOCARIASIS IN CHILDHOOD. A REVIEW
- CENTRAL CORNEAL THICKNESS AND INTRAOCULAR PRESSURE CHANGES POST- PHACOEMULSIFICATION SURGERY IN GLAUCOMA PATIENTS WITH CATARACT
- VISUAL OUTCOMES, CONTRAST SENSITIVITY, AND SATISFACTION WITH MULTIFOCAL INTRAOCULAR LENS BLENDED TECHNIQUE: LATE MID-TERM RESULTS
- CHANGE OF SURGICALLY INDUCED CORNEAL ASTIGMATISM AND POSITION OF ARTIFICIAL INTRAOCULAR LENS OVER TIME
- SEVERE NEAR REFLEX SPASM IN A HEALTHY TEENAGER. A CASE REPORT
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- FORMS OF OCULAR LARVAL TOXOCARIASIS IN CHILDHOOD. A REVIEW
- CHANGE OF SURGICALLY INDUCED CORNEAL ASTIGMATISM AND POSITION OF ARTIFICIAL INTRAOCULAR LENS OVER TIME
- VISUAL OUTCOMES, CONTRAST SENSITIVITY, AND SATISFACTION WITH MULTIFOCAL INTRAOCULAR LENS BLENDED TECHNIQUE: LATE MID-TERM RESULTS
- CENTRAL CORNEAL THICKNESS AND INTRAOCULAR PRESSURE CHANGES POST- PHACOEMULSIFICATION SURGERY IN GLAUCOMA PATIENTS WITH CATARACT
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

