-
Medical journals
- Career
Effect of Botulinum toxin A application in neuro-ophtalmologic indications on Schirmer’s test and tears osmolarity.
Authors: P. Žiak 1; J. Halička 1; K. Kapitánová 1; P. Mojžiš 2
Authors‘ workplace: Očná klinika, Jesseniova Lekárska fakulta v Martine, Univerzita Komenského v Bratislave, Slovenská Republika. Prednosta: MUDr. Peter Žiak, Ph. D. 1; Premium Clinic, Teplice, Česká republika Vedúci: MUDr. Peter Mojžiš, Ph. D., FEBO 2
Published in: Čes. a slov. Oftal., 75, 2019, No. 2, p. 74-77
Category: Original Article
doi: https://doi.org/10.31348/2019/2/3Overview
Botulinum toxin type A (BT-A) is used in the treatment of neuro-ophthalmologic disorders such as essential blepharospasm and facial hemispasm for more than 20 years. Although the long-term effect of repeated application of the BT-A was confirmed, the BT-A effect on tears production and retention is not clear. In our work we investigated whether applied BT-A in patients with blepharospasm and hemifacial spasm affect tears production. Tears quality was measured with Schirmer’s and tear osmolarity test during neuro-ophthalmologic diseases treatment, which was evaluated before and 14 days after application of BT-A (Botox inj, Allergan, Irvine, USA) into the orbicularis oculi muscle. BT-A doses of 16-18 U with unilateral and 32 to 36 U bilateral applications were used.
The mean tear production in Schirmer’s test before BT-A application was 8.38 ± 0.63 mm, and 2 weeks after BT-A application was 7.12 ± 0,6 mm (n = 50). Tear osmolarity was 305.4 ± 9.2 mOsm before BT-A application, and 2 weeks after BT-A application it was 305.2 ± 8,6 mOsm (n = 13).
We found significant difference between two groups in tear quantity (p < 0.012), but not quality (p > 0.05). Application of the BT-A reduced the amount of tears measured by Schirmer’s test. These results confirm rational basis of the empirical clinical experience where an artificial tears substitution is recommended for patients with neuro-ophthalmologic disorders treated by BT-A.
Keywords:
botulinum toxin – Schirmer’s test – Tear osmolarity – dry eye – blepharospasm – hemispasm
INTRODUCTION
Several studies confirm that patients with facial dystonias suffer from dry eye syndrome [1-3]. Botulinum toxin type A (BT-A) has been used in the treatment of essential blepharospasm and hemispasm for over 20 years. The long-term therapeutic effect of repeated applications of BT-A has been repeatedly confirmed, and the application of BT-A is considered the method of choice [4]. By contrast, opinions regarding the influence of BT-A of the production and retention of tears in the conjunctival sac are variable. The effect of BT-A may be generated partially by a blockade of parasympathetic innervation of the lachrymal gland (in the sense of reduced secretion), but also by an inhibiting influence on the muscle pump, thus causing a drainage of tears due to blockade of contraction of the orbicularis oculi muscle in the region of the eyelid, and dysfunction of the meibomian glands [5] (in the sense of increased tear retention). Some authors state improved parameters of the lachrymal film following application of BT-A [13]. An objective and the most widely available technique for measuring the production and simultaneously the retention of tears is the Schirmer’s test. Measurement of tear osmolarity is gradually finding application in clinical medicine, its main advantage is in particular the simplicity of the examination.
MATERIAL AND METHOD
The cohort comprised 27 patients (17 women, 10 men, average age 63.4 years) with essential blepharospasm (46 eyes of 23 patients) and hemispasm (4 eyes of 4 patients). All the patients had undergone repeated applications of BT-A for blepharospasm previously, none of them were BT-A naive patients. Before the application of BT-A, in 62% of patients (n=31) the Schirmer’s test was positive (< 10 mm in 5 minutes).
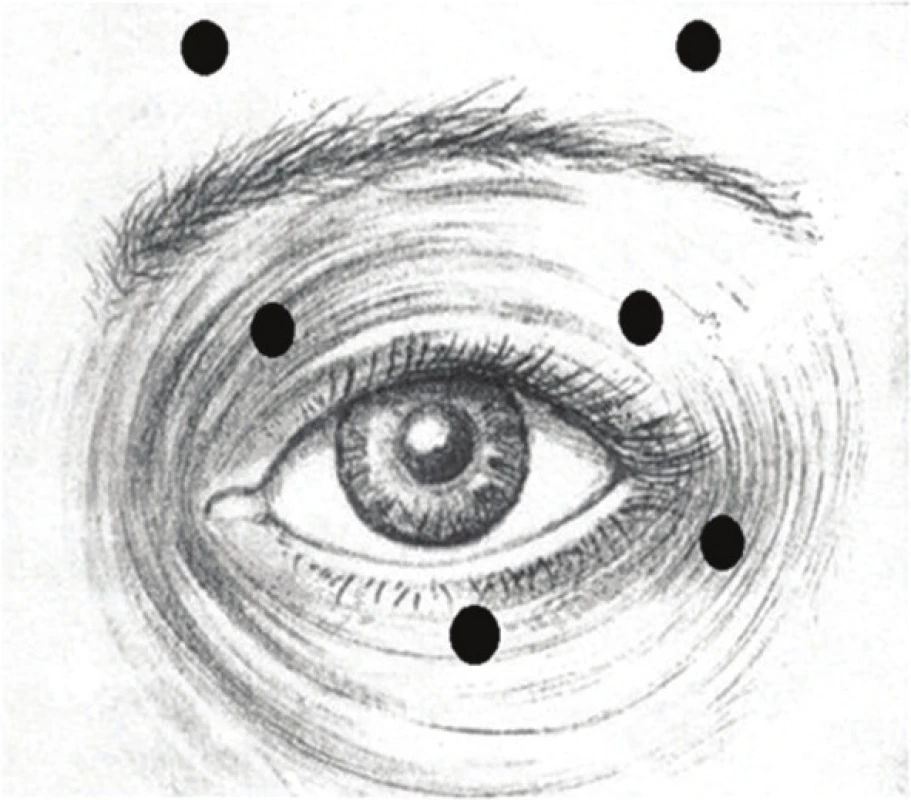
On all the patients we used the preparation BOTOX (Botox injection, Allergan, Irvine, USA) applied into 6 points of the orbicularis oculi muscle in a dose of 16 to 18 U/eye, in a dilution of 20U/ml of physiological solution. We used the recommended schema of application points (fig. 1).
We examined the patients treated with BT-A in neuro-ophthamlolgical indications using a Schirmer’s test (Schirmer I, duration 5 minutes, without the use of anaesthetic drops). Schirmer I examines basal and reflex tear production. On a number of the patients (n=13) we examined change of osmolarity (TearLab, USA), and as additional information we measured Schirmer II (n=10).
We performed the Schirmer’s test and examination of tear osmolarity immediately before the application of BT-A (in the absence of a therapeutic effect of the previous dose) and 14 days after the application of BT-A (when it was possible to expect the maximum therapeutic effect), without the use of anaesthetic drops.
With regard to the abnormal distribution of the values of the Schirmer’s test, determined with the aid of a Shapiro-Wilk test, for the statistical analysis we determined the difference in this parameter before and after the application of BT-A with the aid of a non-parametric Wilcoxon signed-rank test. For the statistical analysis of tear osmolarity before and after the application of BT-A we used a Student T-test.
RESULTS
We did not record any general or local complications following the application of BT-A.
The average value of the Schirmer’s test I before the application of BT-A was 8.38 ± 0.63 mm (n=50), in which 31 eyes (62 %) attained a value less than 10 mm in 5 minutes. The average value of the Schirmer’s test after the application of BT-A was 7.12 ± 0.6 mm (n=50), in which 39 eyes (78%) attained a value less than 10 mm in 5 minutes. We present the results in tables 1 and 2. The Schirmer’s test II before application was 5.58 ± 0.98 mm (n=10).
1. Results of Schirmer’s test before and after application of BT-A (average value ± SEM) 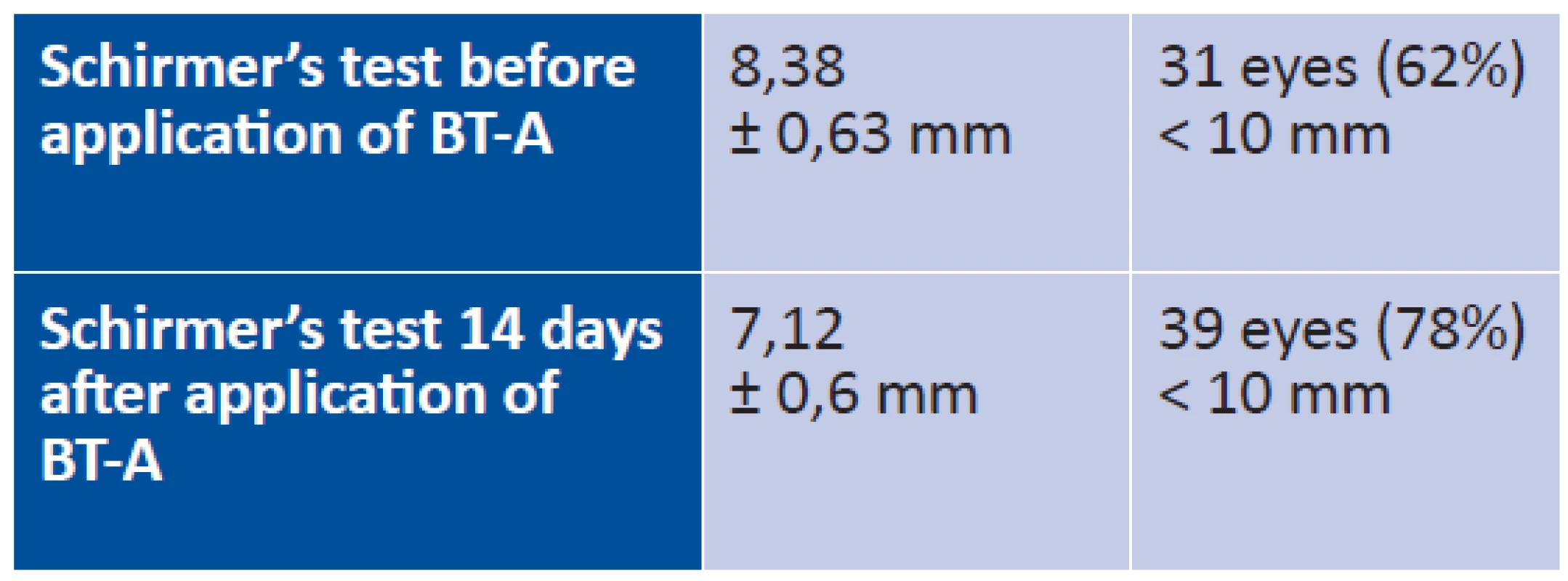
2. Values of tear secretion of all eyes (n = 50) 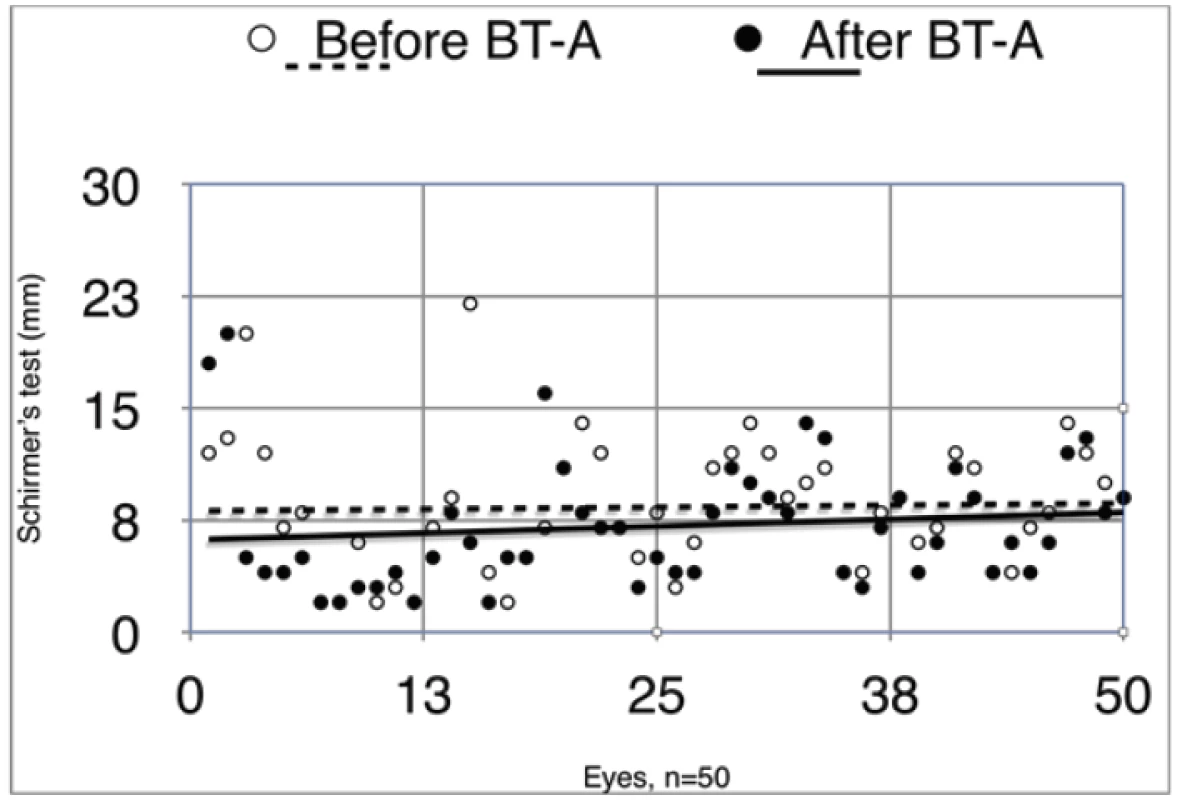
During the course of treatment there was a significant reduction in the value of the Schirmer’s test (p < 0.012, n=50). In 29 patients (58 %) there was a significant reduction of the value of tear secretion following the application of BT-A (p < 0.012). There was increased retention in 11 patients (22 %) and in 10 patients (20 %) there was no change.
Before the application of BT-A, tear osmolarity was 305.4 ± 9.2 mOsm (n=13), 14 days after application of BT-A tear osmolarity reached the level of 305.2 ± 8.6 mOsm (n=13), p > 0.05.
DISCUSSION
The basis of the therapeutic effect of BT-A is a blockade of the neuromuscular connections by means of a presynaptic blockade of release of vesicles containing the neurotransmitter acetylcholine. It acts on SNA (synaptosomal-associated protein), and it has been determined that it fragments the proteins necessary for the entry of secretory vesicles via the cell membrane into the acini of the lachrymal gland [6, 7]. An equivalent mechanism is responsible also for the regulation of secretion of the sweat glands, which is also used in practice [8, 9]. Despite the demonstrated effect of BT-A on tear secretion upon direct application to the lachrymal gland [10, 11], opinions regarding the effect of BT-A on tear retention in the conjunctival sac are not unified, but the application of BT-A itself close to the upper and lower lachrymal punctum may improve manifestations of dry eye syndrome [17]. The reason is the possible influence on BT-A on the muscle pump facilitating the drainage of tears from the conjunctival sac, which has also been demonstrated by dacryoscintigraphy [12]. This pump is formed by an anatomical arrangement of fibres of the orbicularis oculi muscle in relation to the horizontal section of the canaliculus lacrimalis and lateral wall of the lachrymal sac. In the usually used schemas of application of BT-A to the region of the orbicularis oculi muscle, BT-A is not applied to the region of the assumed muscle pump (internal third of the lower eyelid), and the effect of the applied BT-A should therefore be minimal. It is nevertheless impossible to exclude the possibility of diffusion of BT-A from the surrounding area. In our study we compared the effect of BT-A on the results of the Schirmer’s test in the sense of its reduction, which is in accordance with the literature [13]. Schirmer I examines basal and reflex tear production, the limitation of our study is that it does not distinguish change of basal and reflex lachrymation separately. According to the results of the Schirmer II test, our patients primarily suffered from dry eye syndrome.
Similarly to other authors, we did not record any difference in the osmolarity of the lachrymal film [16], the explanation shall evidently be the complexity of the condition and the chronically altered regulation of dry eye in patients with hemispasm or blepharospasm. The actual denervation of the lachymal gland by BT-A is evidently insufficient to alter osmolarity.
An equivalent decrease was observed following the application of BT-A for the correction of wrinkles [14]. Perhaps for this reason it is possible to assume that inhibition of secretion of the lachrymal gland predominates over any increased retention caused by the diffusion of BT-A into the region of the muscular lachrymal pump, and this applies for the classic method of application of BT-A, omitting the nasal point of application on the lower eyelid. Similarly as in other studies [15], in more than 60% of patients before application of BT-A we determined reduced values of the Schirmer’s test below 10 mm. The prevalence of dry eye syndrome in the population is 7.4 – 33.7 % [19], it occurs more frequently in women and the incidence increases with age, although precise data for our region is not available. The function of the lachrymal film is deteriorated by repeated application of BT-A [18], with the development of progressive atrophication of the surrounding tissue [20].
Blepharospasm and dry eye syndrome are two pathologies independent of one another, but may occur simultaneously. Although application of BT-A improves manifestations of blepharospasm, it does not restore normal lachrymation. By contrast, after application we may observe a worsening of the symptoms of dry eye syndrome. In the treatment of patients who suffer from blepharospasm in combination with dry eye syndrome, treatment of dry eye should be long-term, especially in patients following repeated applications.
CONCLUSION
Application of BT-A in a dose of 16-18 U/1 eye significantly reduces tear secretion and thereby also the results of the Schirmer’s test. In almost 60% of patients with a diagnosis of essential blepharospasm and hemispasm, there is a present detectable reduction of tear secretion even before application of BT-A. The use of tear substitution in patients with EB and HS before and especially after application of BT-A is suitable for rectifying the symptoms of dry eye syndrome, and its long-term application has a rational basis.
Received by the Editorial Department on: 14 June 2018
Accepted for printing on: 10 March 2019
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Peter Žiak, Ph.D.
Department of Ophthalmology, Jessenius Faculty of Medicine, Comenius University and Faculty Hospital in Martin
Kollárova ul. 2
036 59 Martin
Slovak Republic
E-mail: ocnesekr@unm.sk
Sources
1. Lu, R., Huang, R., Li, K., et al.: The influence of benign essential blepharospasm on dry eye disease and ocular inflammation. Amer J Ophthalmol, 157; 2014 : 591 – 597
2. Defazio, G., Abbruzzese, G., Aniella, MS., et al.: Eye symp - toms in relatives of patients with primary adult-onset dystonia. Movement Disord, 27; 2012 : 305–307.
3. Huang, XF., Wang, KY., Liang, ZH., et al.: Clinical analysis of patients with primary blepharospasm: A report of 100 cases in China. Euro Neurol, 73; 2015 : 337–341.
4. Ziak P.: [Results of long term treatment of essential blepharospasm and facial hemispasm with botulinum toxin A]. Cesk Slov Oftalmol, 60; 2004 : 37-44.
5. Call, CB., Wise, RJ., Hansen, MR., et al.: In vivo examination of meibomian gland morphology in patients with facial nerve palsy using infrared meibography. Ophthalm Plast Reconstruct Surg, 28(6); 2012 : 396–400.
6. Mense, S.: Neurobiological basis for the use of botulinum toxin in pain therapy. J Neuro, 251; 2004 : 11–17.
7. Wang, Y., Jerdeva, G., Yarber, FA., et al.: Cytoplasmic dynein participates in apically targeted stimulated secretory traffic in primary rabbit lacrimal acinar epithelial cells. J Cell Sci, 116; 2003 : 2051–2065.
8. Bushara, K., Park, D., Jones, J., et al.: Botulinum toxin-a possible new treatment for axillary hyperhidrosis. Clin Exp Dermatol, 21; 1996 : 276-278.
9. Naumann, M., Flachenecker, P., Bröcker, E., et al.: Botulinum toxin for palmar hyperhidrosis. The Lancet, 349; 1997 : 252.
10. Riemann, R., Pfennigsdorf, S., Riemann, E., et al.: Successful treatment of crocodile tears by injection of botulinum toxin into the lacrimal gland. Ophthalmology, 106; 999 : 2322-2324.
11. Suwan-Apichon, O., Rizen, M., Rangsing, R., et al.: Botulinum toxin B induced mouse model of keratokonjunctivitis sicca. Invest Ophthalmol Vis Sci, 47; 2006 : 133-139.
12. Park, D., Shin, H., Lee, S., et al.: Tear production and drainage after botulinum toxin A injection in patients with essential blepharospasm. Acta Ophthalmologica, 91; 2013: 108-112.
13. Gunes, A., Demirci, S., Koyuncuoglu, HR., et al.: Corneal and Tear Film Changes After Botulinum Toxin-A in Blepharospasm or Hemifacial Spasm. Cornea, 34; 2015 : 906 - 910.
14. Matarasso, S.: Decreased Tear Expression with an Abnormal Schirmerʼs Test Following Botulinum Toxin Type A for the Treatment of Lateral Canthal Rhytides. Dermatol Surg, 28; 2002: 149-152.
15. Price, J., O Day, J.: A Comparative Study of Tear Secretion in Blepharospasm and Hemifacial spasm Patients Treated with Botulinum Toxin. J Clin Neuro Opth, 13; 1993; 67-71.
16. Mali, YP., Schultze, RL., Wladis, EJ.: Evaluating the effects of Botulinum Toxin A on tear metrics in patients with hemifacial spasm. Orbit, 36; 2017 : 307-310.
17. Bukhari, AA.: Botulinum neurotoxin type A versus punctal plug insertion in the management of dry eye disease. Oman J Ophthalmol, 7; 2014 : 61-65.
18. Ainsworth, JR., Kraft, SP.: Long-term Changes in Duration of Relief with Botulinum Toxin Treatment of Essential Blepharospasm and Hemifacial Spasm. Ophthalmology, 102; 1995, 2036-2040.
19. Gayton, JL.: Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol, 2009; 405-12.
20. Krasný, J., Šach, J.: Aplikace Dysportu – možnost doprovodného vedlejšího efektu na postavení víček (klinicko-histologická studie). Cesk Slov Oftalmol, 68; 2012 : 216-220.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 2-
All articles in this issue
- Očná klinika Lekárskej fakulty Univerzity Komenského v Bratislave oslavuje 100-TÉ VÝROČIE činnosti – 1. časť
- Normal tension vs high tension glaucoma: an – overview
- Correction of myopia and myopic astigmatism by femtosecond laser in situ keratomileusis
- Effect of Botulinum toxin A application in neuro-ophtalmologic indications on Schirmer’s test and tears osmolarity.
- Peripheral exudative hemorrhagic chorioretinopathy
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Normal tension vs high tension glaucoma: an – overview
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Peripheral exudative hemorrhagic chorioretinopathy
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career