-
Medical journals
- Career
Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
Authors: T. Altschmiedová; M. Vaclová; M. Vráblík
Authors‘ workplace: Centrum preventivní kardiologie, III. interní klinika 1. LF UK a VFN
Published in: Čes. a slov. Oftal., 74, 2018, No. 4, p. 127-131
Category:
doi: https://doi.org/10.31348/2018/1/1-4-2018Overview
Familial hypercholesterolaemia (FH) is the most common congenital metabolic disorder characterised by the accumulation of lipid particles in the vascular wall thereby leading to premature development of atherosclerosis. It is a serious condition that, if left untreated, can lead to premature death in a cardiovascular event already in the third or fourth decade of life. According to recent studies, the frequency of heterozygotes in the general population is 1 : 250, suggesting that there may be up to 40,000 of these patients in the Czech Republic alone. In terms of capturing FH, the Czech Republic belongs to the most successful countries in the world; however, most patients remain undiagnosed. It is essential that these individuals be actively sought for and manifestation of cardiovascular disease (CVD) prevented. There is a therapeutic option that is effective, safe and affordable. The MedPed (Make early diagnosis to Prevent early deaths) project network and a large number of physicians involved in the project represent an effective approach to the diagnosis and treatment of patients with FH. Even though a large proportion of patients with FH are asymptomatic until the manifestation of CVD, it is possible to diagnose FH using a biochemical examination together with a family history. In some patients, it is also possible to identify clinical signs of the disease. Typical ophthalmologic findings include arcus lipoides corneae and xanthelasma palpebrarum. While these are non-specific symptoms, especially if they occur in patients under 50 years of age, they should prompt examination of lipid spectrum parameters. Every patient with (or suspected) familial hypercholesterolaemia should be referred to one of the workplaces of the MedPed project network.
Key words:
familial hypercholesterolaemia, MedPed, atherosclerosis, xanthelasma palpebrarum, arcus lipoides corneae
INTRODUCTION
Familial hypercholesterolaemia (FH) is the most common congenital metabolic disorder in humans, characterised by an accumulation of lipid particles in the vascular wall, thereby leading to the premature development of atherosclerosis. The estimated frequency of heterozygotes in the general population is 1 : 250, suggesting that there are approximately 40 000 affected individuals in the Czech Republic (1). However, the majority of patients are not diagnosed and correctly treated. An effective and safe treatment exists, which is available and should be commenced as soon as possible. In the opposite case, it is no exception that afflicted individuals may suffer the first myocardial infarction between the ages of 30 and 50 years of age (homozygotes even far earlier – usually before the age of 20 years), which results in a dramatic deterioration in quality of life and potentially even death. The disadvantage of this disorder is that it is frequently clinically asymptomatic. Hypercholesterolaemia is painless, the clinical symptoms are not often unequivocally expressed, and diagnosis of FH is thus unfortunately frequently not determined until the time when complications of the atherosclerotic process break out. The patient is referred for specialist care only in the stage of secondary prevention, following a myocardial infarction, in which case it is often impossible to return the patient's original condition and quality of life. As a result, the role played here by doctors upon first contact (in the case of FH, in addition to general practitioners and dermatologists this includes also ophthalmologists) is all the more important, since it is these professionals who have the possibility, if they take this disorder into consideration, to avert an adverse outcome for their patients.
DEFINITION OF FAMILIAL HYPERCHOLESTEROLAEMIA
Familial hypercholesterolaemia is an autosomal dominant (in exceptional cases also recessive) disorder. It is a genetic defect of one of three basic genes (gene for LDL receptor, for apolipoprotein B-100 and the gene for PCSK9 (pro-protein convertase subtilisin/kexin type 9)) applied in the metabolism of LDL cholesterol (LDL-c). The consequence of this disorder is a marked increase in the LDL-c level in the blood, which leads to an accumulation of lipid particles in the walls of the arteries, and thereby accelerates the development of atherosclerosis (3, 7, 16).
EPIDEMIOLOGY OF FAMILIAL HYPERCHOLESTEROLAEMIA
Familial hypercholesterolaemia appears in heterozygote or homozygote form. A Danish study from 2012 demonstrated a prevalence of approximately 1 : 250 (homozygotes 1 : 160 000 – 300 000), thus it is possible to estimate that there are approximately 40 000 patients with heterozygote form of FH in the Czech Republic (1). This prevalence makes FH the most common congenital metabolic disorder.
DIAGNOSIS OF FAMILIAL HYPERCHOLESTEROLAEMIA
FH is a disorder which is asymptomatic for a long period. Diagnosis is determined frequently either by chance (finding of high levels of total and LDL cholesterol in blood within the framework of a preventive check up), or a preliminary manifestation of atherosclerosis and its complications, or also, in the ideal case, by a targeted examination of an as yet asymptomatic relative of a patient with FH.
FH is characterised by isolated hypercholesterolaemia. A number of scoring systems are used for diagnosis (the most common is the Dutch Lipid Clinic Network Criteria), but for the regular practice of the doctor of first contact, it is sufficient to know that every patient with a concentration of LDL cholesterol above 5 mmol/l and/or total cholesterol above 8 mmol/l should be referred to a MedPed centre for a more in-depth examination.
However, we should consider FH immediately after recording the family anamnesis. With regard to the fact that this disorder is distinguished by an autosomal dominant type of heredity, we should, simply speaking, find a preliminary clinical manifestation of atherosclerosis and/or severe hypercholesterolaemia in one of the parents, grandparents, half of siblings or half of children.
CLINICAL SYMPTOMS OF FAMILIAL HYPERCHOLESTEROLAEMIA
Although the most characteristic clinical symptom in the case of FH is the presence of tendinous xanthomas (mainly Achilles tendons and tendons of the extensors primarily on the backs of the hands), there are also less specific symptoms which are nevertheless no less important, with which affected individuals may visit the surgery of an ophthalmologist, or which are a chance secondary finding here.
XANTHELASMA PALPEBRARUM
Xanthelasmas occur most frequently on the eyelids, in the proximity of the inner corners. They are flat or slightly raised deposits, manifesting a straw to orange-yellow colour (13). They represent areas containing lipids, but the precise mechanism of their origin is unknown (5).
Xanthelasmas have a tendency to progress, join together, and cause patients to seek medical attention for cosmetic reasons. This fact enables timely identification of the disorder, and should not be overlooked especially by dermatologists and ophthalmologists or plastic surgeons, to whom patients report first of all. Xanthelasmas should be an indication for laboratory examination of the lipid spectrum. This should certainly apply to patients in whom xanthelasmas have appeared before the age of 50, or in whom they have recurred following surgical removal. Because this constitutes an unspecific symptom, which may be present also in other forms of hyperlipidaemias, the best solution is to refer the patient to a lipidology clinic.
1. Family tree of family with familial hypercholesterolaemia (the proband is a patient from the Preventive Cardiology Centre in Prague) 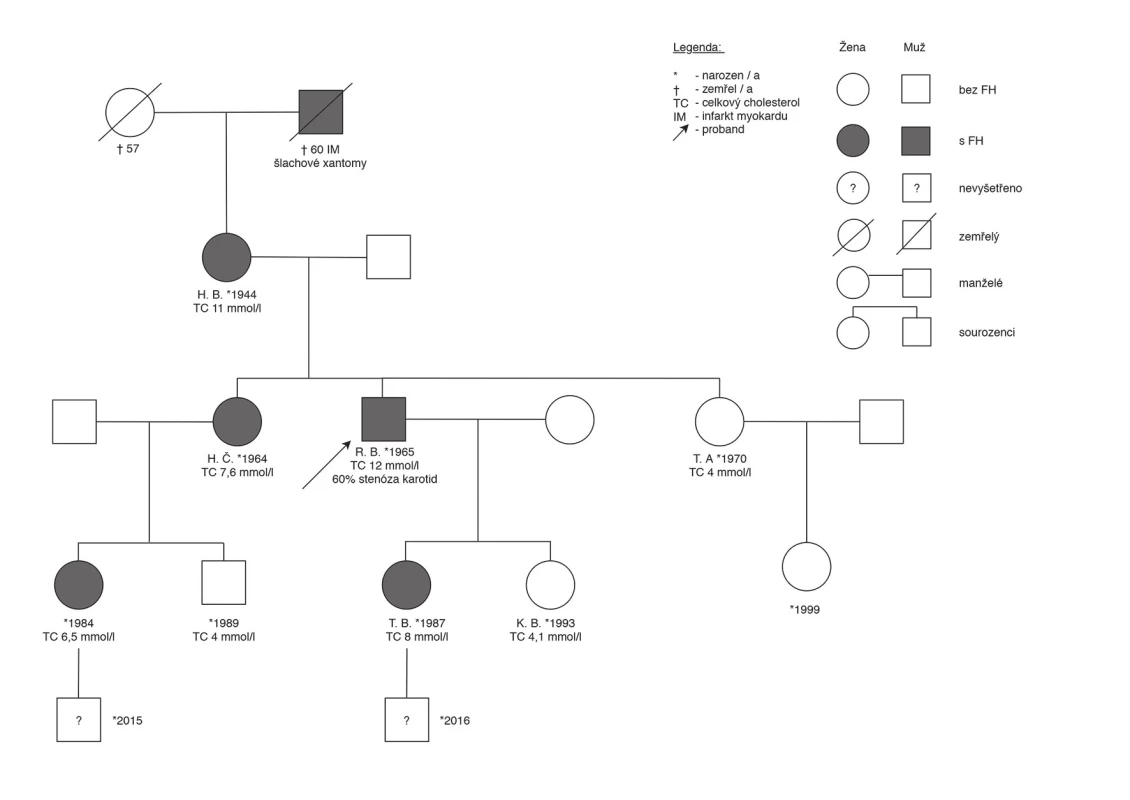
2. Xanthelasma palpebrarum of the upper and lower eyelid of both eyes (from the archive of the Preventive Cardiology Centre, 3rd Internal Clinic, General University Hospital Prague) 
3. Arcus lipoides corneae of both eyes (from the archive of the Preventive Cardiology Centre, 3rd Internal Clinic, General University Hospital Prague) 
ARCUS LIPOIDES CORNEAE
Other ocular symptoms of familial hypercholesterolaemia include arcus lipoides corneae (gerontoxon). This is a greyish-white, sometimes bluish ring on the limbus of the cornea, with a typical lucid interval, a width of approximately 1-1.5 mm, usually bilaterally. In some patients the arcus does not encircle the entire perimeter of the cornea, we then observe a line on the upper and lower perimeter of the cornea, but this never encroaches upon its centre (14). Arcus originates through an accumulation of lipids transported via the limbal capillaries to the corneal stroma. It never has any impact on visual acuity (13).
This represents a non-specific symptom. Accumulation of lipids in the cornea is a process which takes place progressively with age. However, if we observe it in persons aged younger than 50, it is advisable to examine the lipidogram parameters or refer the patient to a specialised centre.
All clinical manifestations depend on the level of cholesterol, as well as on the length of time during which the organism is exposed to the condition. For this reason, in children and young adults we generally do not find clinical symptoms, or they appear only in the case of very high lipidogram values, for example in homozygote forms of FH. In the case that clinical findings occur in a patient younger than 30 years, or even in a child, this represents a highly alarming situation. On the other hand, in patients with well configured therapy, clinical symptoms may be alleviated over time. Xanthelasmas in particular are reduced upon attaining the target values of LDL cholesterol, and in some patients are eradicated entirely (2).
At the Preventive Cardiology Centre we examined a cohort of 558 adult patients with familial hypercholesterolaemia. We determined xanthelasma palpebrarum in 6% of patients, and arcus lipoides corneae in 3% (3). From the above it ensues that these do not constitute frequent symptoms, which however does not in any way reduce their significance.
1. Estimate of the number of diagnosed FH worldwide in individual states at a frequency of 1:500. (Taken from the study by the authors B.G. Nordestgaard, M.J. Chapman, S.E. Humphries et al. and adjusted with the addition of data from the Czech Republic). 
Netherlands, Norway, Czech Republic, Iceland, Switzerland, United Kingdom, Spain, Belgium, Slovakia, Denmark, South Africa, Australia, Hong Kong, France, Taiwan, Italy, Oman, USA, Canada, Japan, Chile, Brazil, Mexico
THE MEDPED PROJECT IN THE CZECH REPUBLIC
In 1998 the Czech Republic joined the MedPed programme (Make early diagnosis to Prevent early deaths), which is under the auspices of the Czech Atherosclerosis Society (www.athero.cz). The main goal of this project is to actively seek out and provide long-term treatment to patients with FH, to diagnose their relatives and thereby reduce the number of untimely deaths due to cardiovascular complications of atherosclerosis. At present the network of the MedPed project comprises approximately 70 centres for children and adults. Within the framework of this programme there is a database of patients with FH, from which attending physicians can obtain valuable information not only about their own patients, but also about further family members. At present over 7 500 patients with familial hypercholesterolaemia are registered in the database, which ranks the Czech Republic in 3rd place in Europe and the world (after the Netherlands and Norway) (Graph 1). Within the framework of the MedPed project, the Czech Atherosclerosis Society also contributes to the organisation of a range of specialist and educational events, with the aim of increasing awareness about FH and thereby also the identification of the disorder in the presymptomatic stage (6, 10).
TREATMENT OF FAMILIAL HYPERCHOLESTEROLAEMIA
The situation of patients with FH fundamentally improved following the introduction of statins onto the market in 1987. A whole range of studies, including meta-analyses, have demonstrated that statins are safe drugs, which significantly reduce the concentration of LDL cholesterol in blood circulation, as well as the risk of cardiovascular ischaemic events and cardiovascular mortality (4, 9, 11). Treatment of an adult patient with FH is commenced immediately after determination of the diagnosis. It is lifelong, comprehensive and is entrusted to a specialist, ideally within the framework of the network of the MedPed project. In addition to lifestyle modifications, the drug of first choice is effective statins (in our conditions most commonly atorvastatin and rosuvastatin), and combination with pharmaceuticals from other groups (ezetimibe, or resin – ion exchanger) is frequently necessary. In the case of an increased level of triglycerides (which however does not primarily pertain to the image of FH), it is possible to add fibrates to the combination of treatment (15). In indicated cases a new, parenteral treatment is available in specialised centres, using monoclonal antibodies against the enzyme PCSK-9 (pro-protein convertase subtilisin kexin type 9), also referred to as PCSK-9 inhibitors, which have the capacity to increase the expression of the receptor for LDL-c, and in the final result reduce the concentration of LDL cholesterol by tens of percentage points. This new therapy is highly promising in the treatment of patients with severe or homozygote form of FH or statin intolerance, or in patients in whom other options for attaining the target level of LDL-c have been exhausted (15). In some centres a non-surgical machine cleaning method is also available – treatment by “LDL apheresis”.
HYPOLIPIDAEMIC THERAPY AND THE RISK OF INCIDENCE OF CATARACT
Studies exist which have observed an increase in the incidence of cataract upon statin therapy, as well as others which have not confirmed this assertion. Even a summary evaluation of the evidence from statin studies in a recent meta-analysis, numbering over 313 thousand patients, failed to demonstrate an increase of the risk upon therapy with these pharmaceuticals (17).
With regard to the new possibilities of further reduction of the level of LDL cholesterol provided by treatment with PCSK-9 inhibitors (alirocumab, evolocumab), investigations have been conducted as to whether such low levels of LDL-c themselves may correlate with the incidence of cataract. A summary analysis of 14 studies with alirocumab stated that upon attaining very low levels of serum LDL-c (<0.65 mmol/l), the incidence of cataract was approximately tripled. The cause of this has not been explained, but the study concluded that it was not connected with the application of PCSK-9 inhibitors (12). Similarly, nothing of this nature was confirmed in an analysis of persons with very low levels of LDL-c (<0.5 mmol/l) in the Fourier trial with evolocumab (8).
It is possible to conclude that the serum level of cholesterol may correlate with the risk of cataract, but in all cases the increased risk of cataract is not a reason for change of practice in the indication of hypolipidaemic therapy.
CONCLUSION
Familial hypercholesterolaemia is a very serious genetic disorder, which may relate to as many as 40 000 individuals in the Czech Republic. With regard to the fact that a large proportion of patients are asymptomatic, it may not be recognised until premature manifestation of cardiovascular disease or sudden cardiovascular death. Ophthalmologists may also provide assistance in the identification of new patients, by recognising clinical symptoms of FH and sending patients to a specialised centre. Thanks to screening in the family, one patient diagnosed with the condition may help reveal a number of similarly afflicted relatives. Treatment of FH is available, safe and effective, and it is more than desirable to seek out and treat these patients. Effective care for patients with FH is represented in its complex approach by the initiative of the Czech Atherosclerosis Society (MedPed project). More detailed information, including contacts, can be found on the website of the Czech Atherosclerosis Society (www.athero.cz).
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 25. 3. 2018
Accepted: 27. 8. 2018
Available on-line: 18. 3. 2019
MUDr. Tereza Altschmiedová
Centrum preventivní kardiologie,
III. interní klinika 1. LF UK a VFN
Fakultní poliklinika, Karlovo nám. 32, 128 08, Praha 2.
email: tereza.altschmiedova@vfn.cz; tereza@altschmiedova.cz
Sources
1. Benn, M., Watts, GF., Tybjaerg-Hansen, A. et al.: Familial hypercholesterolemia in the danish general population: prevalence, coronary artery disease, and cholesterol-lowering medication. J Clin Endocrinol Metab, 2012; 97 : 3956-3964. doi:10.1210/jc.2012-1563.
2. Civeira F., Perez-Calahorra S., Mateo-Gallego, R.: Rapid resolution of xanthelasmas after treatment with alirocumab. J Clin Lipidol, 2016; 10(5):1259-61.
3. Češka, R.: Familiární hypercholesterolemie, TRITON, 2015, Praha
4. de Vries, FM., Kolthof, J., Postma, MJ. et al.: Efficacy of standard and intensive statin treatment for the secondary prevention of cardiovascular and cerebrovascular events in diabetes patients: a meta-analysis. PLoS One, 2014;9(11):e111247.
5. Dey, A., Aggarwal, R., Dwivedi, S. et al.: Cardiovascular Profile of Xanthelasma Palpebrarum. Biomed Res Int, 2013; 2013 : 932863.
6. Freiberger, T., Vrablík, M.: Včasná diagnostika familiární hypercholesterolemie v České republice v rámci projektu MedPed. Vnitř Lék 2015; 61(11): 942-945.
7. Gidding, SS., Champagne, MA., de Ferranti, SD. et al.: The agenda for familial hypercholesterolemia: a scientific statement from the American Heart Association. Circulation, 2015; 132(22): 2167-92.
8. Giugliano, RP., Pedersen, TR., Park, JG. et al.: Clinical efficacy and safety of achieving very low LDL ‑ cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet 2017;390(10106):1962-1971.
9. Mihaylova, B., Emberson, J., Blackwell, L. et al.: Cholesterol Treatment Trialists’ (CTT) Collaborators: The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 2012;380(9841): 581-90.
10. Nordestgaard, BG., Chapman, MJ., Humphries, SE. et al.: European Atherosclerosis Society Consensus Panel: Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart, J 2013; 34(45):3478-90a.
11. Raal, FJ., Pilcher, GJ., Panz, VR. et al.: Reduction in mortality in subjects with homozygous familial hypercholesterolemia associated with advances in lipid-lowering therapy. Circulation 2011; 124(20):2202-7.
12. Robinson, JG., Rosensos, RS., Farnier, M. et al.: Safety of very low low-density lipoprotein cholesterol levels with alirocumab: Pooled data from randomized trials. J Am Coll Cardiol, 2017; 69(5):471-482.
13. Šobra, J.: Familiární hypercholesterolemická xanthomatosa. AVICENUM, 1970, Praha
14. Tůmová, E., Vrablík M.: Arcus lipoides corneae. Med. Praxi, 2013; 10(11–12): 395.
15. Vrablík, M.: Farmakoterapie dyslipidemie. Maxdorf, Praha, 2016, 123 str.
16. Watts, GF., Gidding, S., Wierzbicki, AS. et al.: Integrated guidance on the care of familial hypercholesterolemia from the International FH Foundation. Int J Cardiol, 2014; 171(3):309-25.
17. Yu, S., Chu, Y., Li, G. et al.: Statin use and the risk of cataracts: a systematic review and metaanalysis. J Am Heart Assoc, 2017; 6(3): e004180. doi: 10.1161/JAHA.116.004180.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 4-
All articles in this issue
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
- Digital Eye Strain in a Population of Young Subjects
- EFFECT OF MULTIPLE VARIABLES ON THE REFRACTIVE ERROR AFTER CATARACT SURGERY
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

