-
Medical journals
- Career
The Role of Radiotherapy in Skull Metastasis of Thyroid Follicular Carcinoma
Authors: Benderli Yasemin Cihan 1; Ali Koc 2; Tursem Turgut Tokmak 2
Authors‘ workplace: Department of Radiation Oncology, Kayseri Education and Research Hospital, Turkey 1; Department of Radiology, Kayseri Education and Research Hospital, Turkey 2
Published in: Klin Onkol 2019; 32(4): 300-302
Category: Case Report
doi: https://doi.org/10.14735/amko2019300Overview
Introduction: Bone metastasis is seen in 2.3–12.7% of thyroid follicular carcinomas. Bone metastasis most commonly occurs in the vertebrae, costas and hip bones. In this report we discuss the diagnosis and treatment of a patient followed up due to skull metastasis of thyroid follicular carcinoma in light of literature. Case report: A 51-year-old female patient underwent surgery due a mass in the scalp. The histopathological examination was reported as metastasis of follicular thyroid carcinoma. No radiotherapy was indicated because of the total excision of the mass and the benign surgical margins. The patient, in whom fine needle aspiration biopsy showed the result of follicular carcinoma underwent a total bilateral thyroidectomy. Whole-body I-131 scintigraphy revealed diffuse activity involvement in the thyroid gland, and lung and bone (skull, sacrum, right acetabulum) metastasis. The patient was scheduled for radioactive iodine therapy. Conclusion: Total/near total thyroidectomy and metastasectomy should be the treatment of choice in skull metastasis. Postoperative radioactive iodine and radiotherapy should be offered. Radiotherapy should be reserved for inoperable and residual tumour cases.
Keywords:
radiotherapy – thyroid follicular carcinoma – skull metastasis
Introduction
Follicular thyroid carcinoma (FTC) accounts for 17% of all thyroid malignancies. Distant metastasis is reported in 4.5–15% in FTC [ 1]. It is often hematogenous. The most common metastasis occurs in the lungs, bones and liver [1,2]. Bone metastasis is not frequent in FTC with an incidence between 2.3% and 12.7%. Among bone metastases, skull metastasis is extremely rare [2,3]. The primary treatment of skull metastasis is surgery. Radiotherapy and radioactive iodine therapy are recommended for inoperable patients and residual tumours [1–4].
In this article, we discuss the clinical findings, imaging characteristics, the treatments administered and the prognosis of a patient followed up due to FTC, in light of literature.
Case report
A 51-year-old female patient was referred to the neurosurgery outpatient clinic with complaints of increasing swelling and pain in the scalp. The physical examination revealed a hard and immobile mass lesion of 4 × 4 cm in the parietal region at the level of the vertex. The patient had no known history of systemic disease. She had no history of smoking or alcohol abuse. Cranial computed tomography and magnetic resonance imaging showed an extra-axial localised mass lesion of 42 × 45 mm, which caused destruction in the bony structure in the right parietal and parasagittal areas, extending toward the superior and showing diffuse heterogeneous contrast enhancement on the postcontrast series (Fig. 1). Total excisional biopsy was performed. The pathological outcome was reported as follicular carcinoma metastasis. Radiotherapy was not indicated because of the benign surgical margins and total excision of the mass. On the neck and thyroid ultrasound of the patient, a multinodular heterogeneous thyroid gland was observed. The patient, in whom fine needle aspiration was reported as follicular carcinoma underwent a total bilateral thyroidectomy. Whole-body I-131 scintigraphy revealed diffuse activity involvement in the thyroid gland, and lung and bone (skull, sacrum, right acetabulum) metastasis. The patient was scheduled for radioactive iodine therapy.
1. Coronal T2-weighted fast spin echo and sagittal contrast enhanced T1-weighted MRI images show a calvarial expansile lytic lesion located at the right paramedian frontoparietal region with an intense heterogenous contrast enhancement. There is also compression and displacement of superior sagittal sinus without any finding of dural invasion. 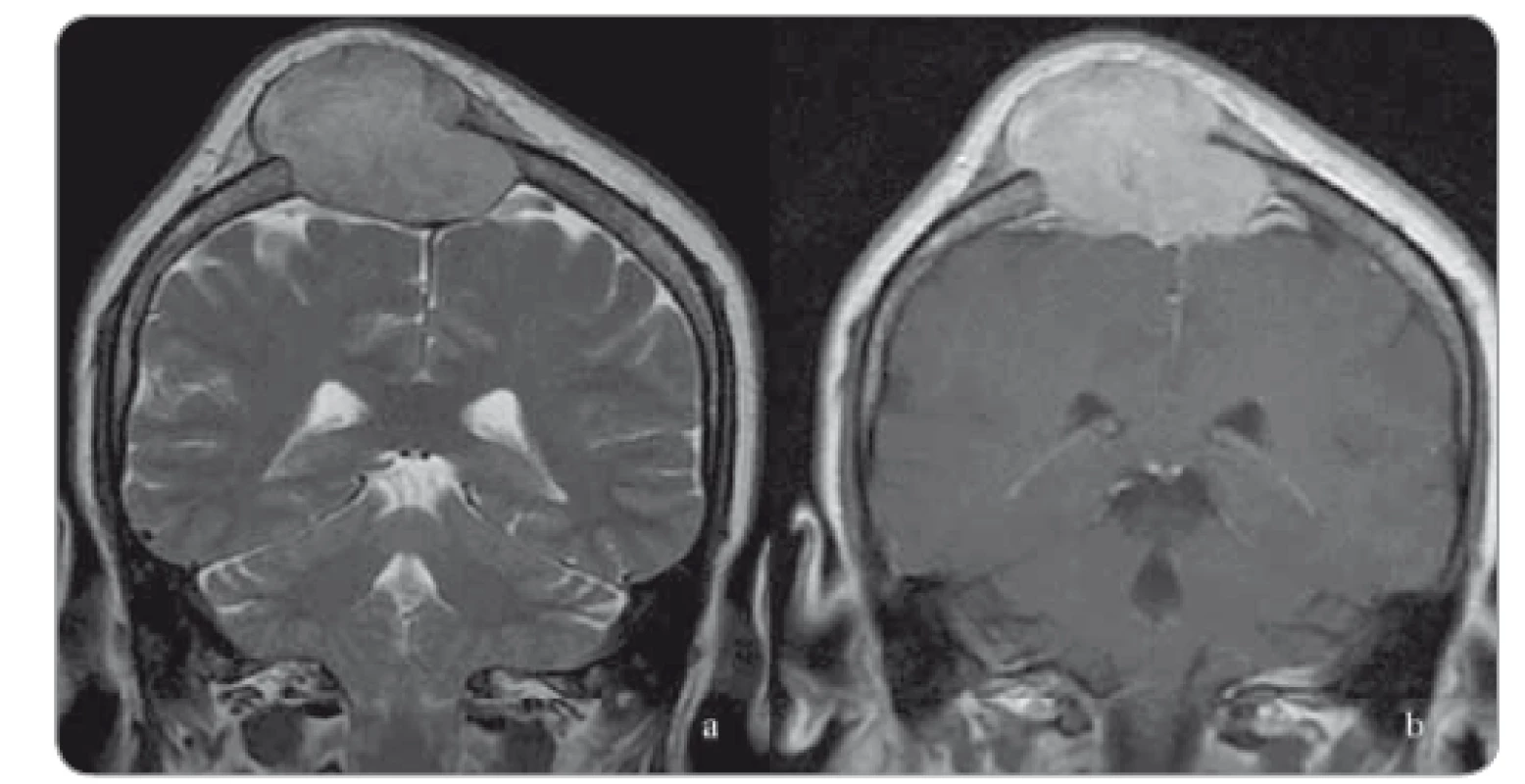
Discussion
Bone metastasis most commonly occurs in the vertebrae, costas and hip bones. Skull metastasis is extremely rare [1]. In a study by Nagamine et al. of 473 patients with thyroid cancer, skull metastasis was reported at 2.5% [2]. Anatomically, the lesions are more common in the middle line frontal and parietooccipital regions. Radiologically, the majority of the lesions seen in the scalp are typically single, hypervascular and osteolytic. The most common symptom is cranial nerve dysfunction [3,4].
The primary treatment of skull metastasis is surgery [4,5]. Studies have shown that the resection of skull metastasis in addition to total thyroidectomy increases survival [1]. Radioactive iodine and radiotherapy are applied for unresectable or residual tumours [2,5]. Besides, monoclonal antibodies targeting RANKL and bisphosphonates play an important role in the treatment of bone metastases of thyroid cancer [6]. Kotecha et al. reported that Gamma Knife surgery is an efficient treatment method in the calvarium bones and skull base metastases [7]. Screening the literature, timing a dose of the radiotherapy to be given, and the subgroup which will benefit from stereotactic radiosurgery have yet to be clarified. Vascular endothelial growth factor-specific receptor tyrosine kinase inhibitors have been shown to be useful in cases refractory to radioactive iodine therapy [8]. External-beam radiotherapy is recommended to improve locoregional control in cases resistant to radioactive iodine treatment [9]. The mean survival was reported as 4.5 years (5 months – 17 years) in thyroid cancers with skull metastasis. This duration has been found to be shorter in untreated patients [1,2,10,11].
In conclusion, no single standard postoperative treatment could be established in skull metastasis seen in thyroid cancer, because of its low incidence and lack of data from prospective studies. Total/near total thyroidectomy and metastasectomy should be the treatment of choice in skull metastasis. Postoperative radioactive iodine and radiotherapy should be offered.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE recommendation for biomedical papers
Yasemin Benderli Cihan, M.D.
Department of Radiation Oncology
Kayseri Education and Research Hospital
Sanayi District, Ataturk Boulevard
Hastane Street, No 78
38010 Kocasinan/Kayseri, Turkey
e-mail: cihany@erciyes.edu.tr
Submitted: 10. 2. 2019
Accepted: 22. 7. 2019
Sources
1. Lee HS, Yoo H, Lee SH et al. Clinical characteristics and follow-up of intracranial metastases from thyroid cancer. Acta Neurochir (Wien) 2015; 157 (12): 2185–2194. doi: 10.1007/s00701-015-2611-5.
2. Nagamine Y, Suzuki J, Katakura R et al. Skullmetastasis of thyroidcarcinoma. Study of 12 cases. J Neurosurg 1985; 63 (4): 526–531. doi: 10.3171/jns.1985.63.4.0526.
3. El Tazi M, Essadi I, Errihani H. Thyroid carcinoma presenting as a dural metastasis mimicking a meningioma: a case report. N Am J Med Sci 2011; 3 (1): 39–42. doi: 10.4297/najms.2011.339.
4. Shen J, Wang S, Zhao X et al. Skull metastasis from follicular thyroid carcinoma: report of three cases and review of literature. Int J Clin Exp Pathol 2015; 8 (11): 15285–15293.
5. Matsuno A, Katakami H, Okazaki R et al. Skull base metastasis from follicular thyroid carcinoma – two case reports. Neurol Med Chir (Tokyo) 2010; 50 (5): 421–425. doi: 10.2176/nmc.50.421.
6. Wexler JA. Approach to the thyroid cancer patient with bone metastases. J Clin Endocrinol Metab 2011; 96 (8): 2296–2307. doi: 10.1210/jc.2010-1996.
7. Kotecha R, Angelov L, Barnett GH et al. Calvarial and skull base metastases: expanding the clinical utility of Gamma Knifesurgery. J Neurosurg 2014; 121 (Suppl): 91–101. doi: 10.3171/2014.7.GKS141272.
8. Kloos RT, Ringel MD, Knopp MV et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol 2009; 27 (10): 1675–1684. doi: 10.1200/JCO.2008.18.2717.
9. Kiess AP, Agrawal N, Brierley JD et al. External-beam radiotherapy for differentiated thyroid cancer locoregional control: a statement of the American Head and Neck Society. Head Neck 2016; 38 (4): 493–498. doi: 10.1002/hed.24357.
10. Kalra R, Pawar R, Hasija S et al. Frontal bone metastasis from an occult follicular thyroid carcinoma: diagnosed by FNAC. J Cytol 2017; 34 (1): 59–61. doi: 10.4103/0970-9371.197623.
11. Califano I, Deutsch S, Löwenstein A et al. Outcomes of patients with bone metastases from differentiated thyroid cancer. Arch Endocrinol Metab 2018; 62 (1): 14–20. doi: 10.20945/2359-3997000000004.
Labels
Paediatric clinical oncology Surgery Clinical oncology
Article was published inClinical Oncology

2019 Issue 4-
All articles in this issue
- Current Perspective on HPV-Associated Oropharyngeal Carcinomas and the Role of p16 as a Surrogate Marker of High-Risk HPV
- Role of the Microbiome in the Formation and Development of Colorectal Cancer
- Methods of Classical and Molecular Cytogenetics Suitable for Biodosimetry of Persons with Professional Exposure to Carcinogens
- BMI and Odds of Endometrial Adenocarcinoma in Czech Women – a Case Control Study
- The Pharmacoeconomic Analysis of Cetuximab and Panitumumab in the 1st Line Treatment of mCRC in Real Clinical Practice in the Czech Republic
- Incidence and Risk Factors of Distant Metastases of Head and Neck Carcinoma
- Oncology Case Report – When Is the Appropriate Time to Integrate Palliative Care?
- Farmakoekonomické studie a procesy HTA při hodnocení nákladů a benefitů nákladné inovativní léčby u nás i ve světě
- Aplikovat jeden cyklus nebo jednu sérii chemoterapie?
- Zemřel prof. MUDr. Josef Koutecký, DrSc., zakladatel dětské onkologie
- Onkologie v obrazech Kožní toxicita při cílené léčbě generalizovaného melanomu
- P21-Associated ncRNA DNA Damage-Activated Expression in Bladder Cancer
- The Role of Radiotherapy in Skull Metastasis of Thyroid Follicular Carcinoma
- Urgent Surgical Treatment of GIST of Esophago-Gastric Junction in a Patient with Giant Hiatal Hernia
- Proposed Strategies for Improving Adherence to Tyrosine Kinase Inhibitors in Patients with Chronic Myeloid Leukaemia
- Clinical Oncology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Role of the Microbiome in the Formation and Development of Colorectal Cancer
- Current Perspective on HPV-Associated Oropharyngeal Carcinomas and the Role of p16 as a Surrogate Marker of High-Risk HPV
- Oncology Case Report – When Is the Appropriate Time to Integrate Palliative Care?
- Incidence and Risk Factors of Distant Metastases of Head and Neck Carcinoma
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

