-
Medical journals
- Career
THE NASOLABIAL FLAP: THE MOST VERSATILE METHOD IN FACIAL RECONSTRUCTION
Authors: J. Bayer; K. Schwarzmannová; M. Dušková; K. Novotná; J. Kníže; A. Sukop
Authors‘ workplace: Department of Plastic Surgery, 3rd Faculty of Medicine, Charles University, University Hospital Královské Vinohrady, Prague, Czech Republic
Published in: ACTA CHIRURGIAE PLASTICAE, 59, 3-4, 2017, pp. 135-141
INTRODUCTION
The nasolabial (also called melolabial) flap was one of the first local flaps used for closure of defects in the midfacial area. It was described in 1846 by a German surgeon, Johann Friedrich Dieffenbach, and still remains the most useful option for reconstruction in the area of facial triangle due to its versatility and effectiveness.1, 2 Over 560 articles were found in PubMed search for nasolabial flap between 1960 and 2016.3
This flap may be either superiorly or inferiorly based. The most commonly used superiorly based flap is useful for defects of the central and lateral nasal dorsum as well as the nasal tip and ala. This technique allows harvesting a huge flap along the whole length of nasolabial fold down to the border of the chin and in the width determined by the amount of natural excess of tissue at the nasolabial crease and its extensibility. The inferiorly based flap is useful for upper and lower lip defects, the floor of the nose and reconstruction of the columella.4, 5 (Fig. 1, 2.)
1. Nasolabial flap with superior pedicle 
2. Nasolabial flap with inferior pedicle 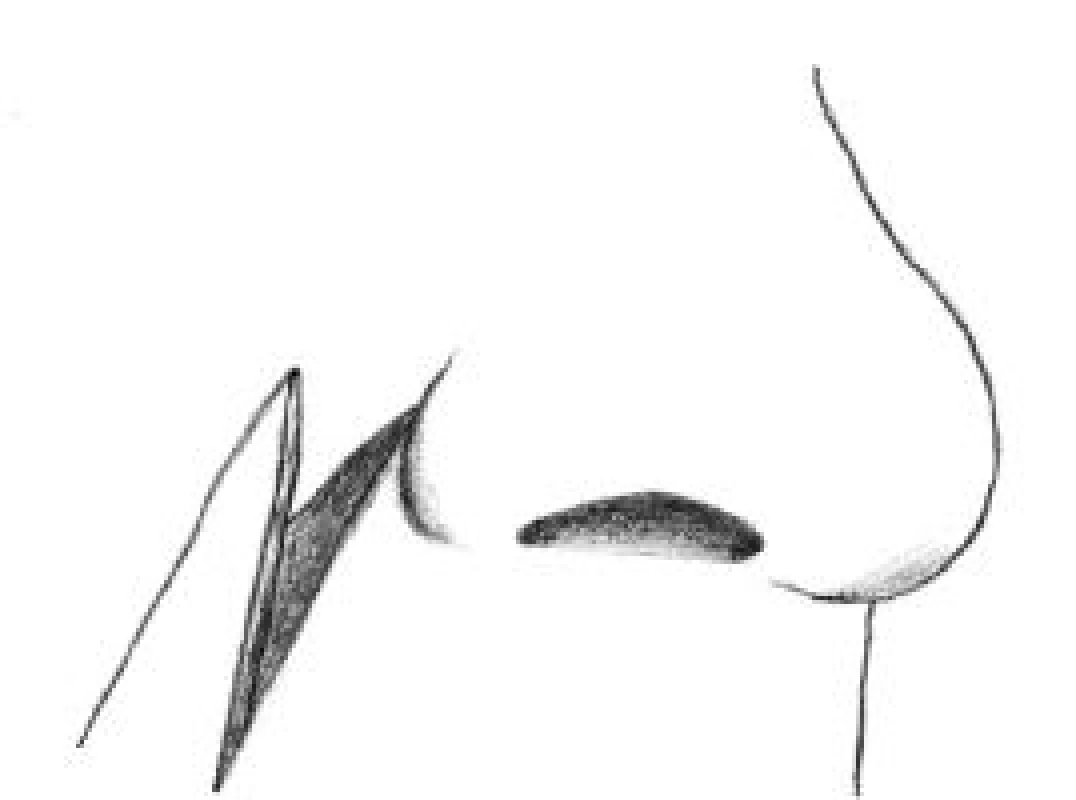
ANATOMY OF THE VASCULAR SUPPLY
The paranasal cheek area is supplied medially by the angular artery and its perforating branches. The central cheek is supplied by the perforating branches from the internal maxillary artery as well as by extensions of the transverse facial branch from the superficial temporal artery. The nasolabial flap can be used as a random pattern type or it can be lifted as an axial pattern flap. The vascular supply to random flaps arises from the subdermal vascular plexus and dermal plexus, which are ultimately supplied by musculocutaneous arteries. Thus, the appropriate plane of dissection is subcutaneous fat. 6
NASOLABIAL FLAP MODALITIES
Transposition flap
This technique, usually based on the superior pedicle, allows the use of the cheek tissue adjacent to the upper lip from which a larger flap can be harvested. The flap is raised and transferred as a single stage procedure to an immediately adjacent defect. With the paramedian forehead flap, this technique is the most suitable method for reconstruction of the nasal lobule.
When the defect is on the lateral nasal lobule and does not cross the midline, the flap may be based only on dermal blood supply.
The medial border of the flap should be drawn from the tangent at the edge of the defect so as to leave the lateral alar crease intact. The flap is then back-cut to approximately the same level and a Burrow´s triangle is removed from the upper lateral nasal skin. The cheek skin over the malar and buccal areas is then elevated in a subcutaneous plane, so that the transposition flap becomes a secondary extension from the edge of the cheek advancement flap. The nasolabial transposition flap should be defatted to the appropriate thickness at the time of transfer so that a secondary revision should be unnecessary. The flap could also be folded upon itself for nasal lining or extended past the midline. In this case, consideration may be given either to delay the flap or to maintain a direct communication with the subcutaneous portion of the pedicle and its branches from the angular artery.6, 7 (Fig. 3, 4.)
3. Tumorous infiltration of the nasal ala 
4. Transposition nasolabial flap 
Transposition nasolabial flaps are very often used for reconstruction of complex nasal defects especially in the alar and tip regions. The flap could be folded upon itself to restore nasal lining usually in combination with other flaps such as forehead or contralateral nasolabial flaps.8, 9, 17, 24 (Fig. 5.)
5. A–F. Sequence of nasal lining reconstruction with transposition nasolabial flap 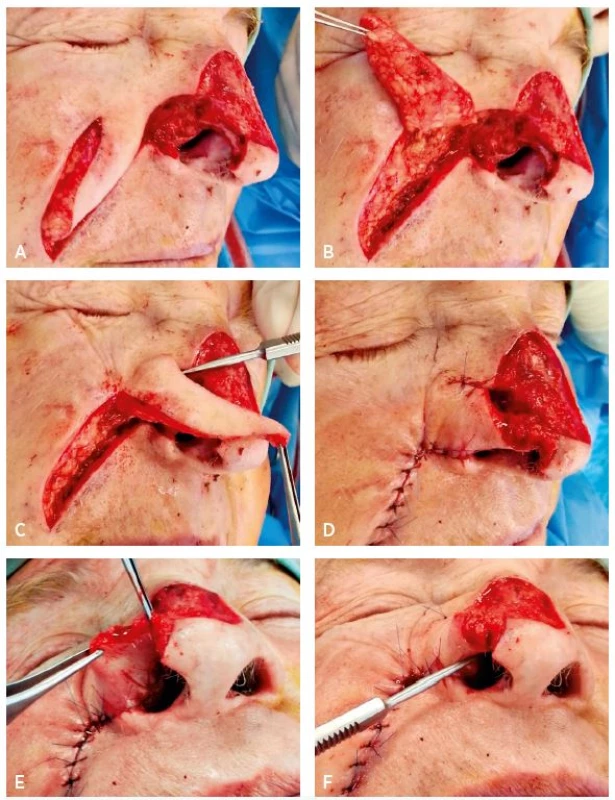
Interpolation flap
Interpolation flaps are similar to transposition flaps with the difference that the interpolation flap is lifted over an area of normal skin to reach the defect. The base of the flap is not immediately adjacent to the recipient site. This arrangement results in a bridge of tissue, or pedicle, between the flap base and the surgical defect. These flaps are used when insufficient tissue or mobility in nearby skin prevents coverage of a surgical defect with primary closure or an adjacent flap. An interpolation flap is a two-stage surgery. The bridge must be disconnected in a second stage when the new vascular supply is established between the wound and the flap (usually after 3 weeks).7, 10, 11 (Fig. 6 A–D.)
6. A–D. Sequence of nasal ala defect reconstruction with interpolation nasolabial flap 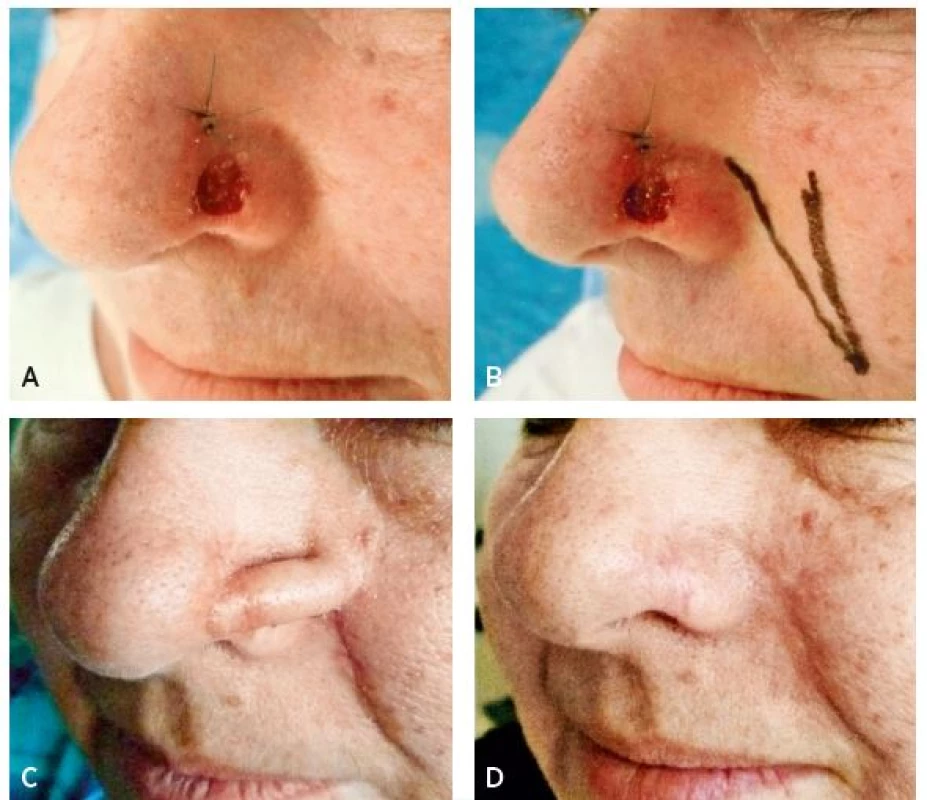
This method is very suitable for nasal tip or columella reconstruction. Often in combination with cartilaginous grafts, mucosal flaps or skin grafts, it could be used for rconstruction of penetrating (complex) nasal defects.10, 11 (Fig. 7A–D.)
7. A–D. Sequence of reconstruction of a penetrating defect of the nasal tip with interpolation nasolabial flap in combination with nasal mucosal advancement 
Advancement flap – V-Y flap
A sliding flap from the nasolabial fold in a V-Y manner is well suited for reconstructing the area where the lower or middle third of the nose meets the cheek. Like the island flap, the sliding flap is generally slid into the defect on a subcutaneous pedicle.7, 12 (Fig. 8A–D.)
8. A–D. Sequence of reconstruction of defect on the nasal-cheek border with V-Y advancement nasolabial flap 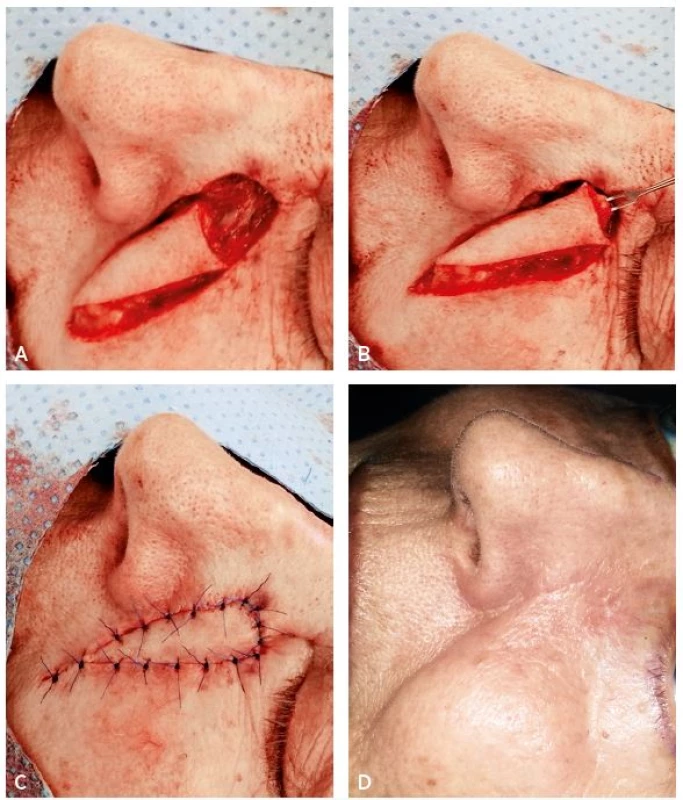
Subcutaneously pedicled island flap
This method popularized by Bouisson (1864) is also useful for reconstructing small defects in the nasal flank area. The flap may be based on the facial artery or be designed with a subcutaneous pedicle that has an inferolateral or superolateral position in relation to the flap. The skin between the flap and the defect is undermined, and the pedicle is pulled through. Care is taken not to place excessive torsion or pressure on the flap pedicle. Because the subcutaneous pedicle often creates fullness at the pull-through site, this is not one of the most favourite flaps. The cheek must be mobilized somewhat more widely than with other flaps to avoid distorting the upper lip.4, 6, 7, 13
Facial artery perforator based nasolabial flap
The facial artery perforator-based nasolabial flap is supported by the study of angiosomes of the facial region and is usually based on the superior labial artery perforator, including the facial artery perforator. These flaps are designed as rotation propeller flaps. The term “propeller flap” is an island flap that reaches the recipient site by axial rotation. This technique allows greater freedom in rotation, mobility, and flap design for the reconstruction of perinasal defects. Possible negative aspect of this method is the time required. Perforator dissection is a more difficult procedure than the use of other local flaps that do not require perforator dissection.14, 15
Nasolabial free flap
A nasolabial free flap consisting of a part of the risorius and buccinator muscles, buccal mucosa, and nasolabial skin is rarely used for reconstruction of full-thickness lower eyelid defects. This flap, supported by the facial vessels, is transported via microvascular anastomosis to the superficial temporal vessels.16
DISCUSSION
When choosing the method of facial reconstruction, it is necessary to carefully consider surgical stress on the patient, the technical demand of the approach, and the type of anaesthesia. These circumstances must meet the expected benefit of the surgery. The surgery must be undergone in a disease free terrain, however, it is necessary to maintain good function and an acceptable appearance. The need of functional and aesthetic effects may be different according to each individual personality. The simplest method for closure of facial defects is a skin graft. It can be used only in superficial defects with a suitable vascular bed.11, 21, 22
The cosmetic outcome of skin grafts may be poor due to the colour and texture mismatch. Especially in nasal reconstruction, local flaps such as nasolabial or dorsal nasal flap have better results. Bilobed flaps are now largely abandoned in nasal reconstruction because they almost violate the subunit principle either at the donor site or at the recipient site.19 Dorsal nasal flaps are often linked with apparent scars and are insufficient for large tip defects.1
In deep and large defects of the nose and the centrofacial region, only nasolabial and forehead flaps can be used. The forehead flap, which is more suitable for larger defects of the nasal dorsum and tip, represents more encumbering two-stage surgery, which requires general anaesthesia and results in a more visible scar at the donor area18. Postoperative morbidity can be considerably higher for forehead flaps than for nasolabial flaps.1, 18, 19, 23, 25
The nasolabial flap perfectly matches the requirements of complex reconstruction of small and middle size defects including the possibility to combine it with a cartilage graft or a contralateral flap. Technically, it is an easy surgery performed in local anaesthesia with minimal donor site morbidity. Disadvantages of this procedure are the risk of transferring hairy skin onto the nose and two-stage procedure in the interpolation variant of this flap.20, 21, 22, 23, 25
CONCLUSION
The nasolabial flap is an easy, quick and effective approach for treatment of smaller and middle-sized defects of the midfacial area. This technique allows harvesting a wide and rich vascularized flap along the whole length of the nasolabial fold. In combination with the wide arc of rotation, the flap could reach almost any site of centrofacial area. The flap perfectly matches the requirements of complex reconstruction including the possibility to combine it with cartilage graft. It produces a good functional and aesthetic outcome with minimal donor site morbidity and overall stress for the patient. Therefore, it is suitable for patients with higher expectations even in cases that they are old and polymorbid. Due to its versatility and effectiveness, the nasolabial flap still remains the most useful option for reconstruction in the area of facial triangle.
Corresponding author:
Jiří Bayer, M.D.
Department of Plastic Surgery, 3rd Faculty of Medicine, Charles University
and University Hospital Královské Vinohrady
Šrobárova 50, 100 34 Prague 10, Czech Republic
E-mail: bayer01@seznam.cz
Sources
1. Thornton JF, Weathers WM. Nasolabial flap for nasal tip reconstruction. Plast Reconstr Surg. 2008 Sep;122(3):775-81.
2. Rao JK, Shende KS. Overview of Local Flaps of the Face for Reconstruction of Cutaneous Malignancies: Single Institutional Experience of Seventy Cases. J Cutan Aesthet Surg. 2016 Oct-Dec;9(4):220-225.
3. Rahpeyma A, Khajehahmadi S. The place of nasolabial flap in oro-facial reconstruction: A review. Ann Med Surg (Lond). 2016 Nov 23;12 : 79-87.
4. Rudkin GH, Carlsen BT, Miller TA. Nasolabial flap reconstruction of large defects of the lower lip. Plast Reconstr Surg. 2003 Feb;111(2):810-7.
5. Yanai A, Nagata S, Tanaka H. Reconstruction of the columella with bilateral nasolabial flaps. Plast Reconstr Surg. 1986 Jan;77(1):129-32.
6. Ohtsuka H, Shioya N, Asano T. Clinical experience with nasolabial flaps. Ann Plast Surg. 1981 Mar;6(3):207-12.
7. Weerda, Hilko. Reconstructive facial plastic surgery: a problem-solving manual. Univ of California Press, 2001.pPg. 36-46, 62
8. Zelken JA, Reddy SK, Chang CS et al. Nasolabial and forehead flap reconstruction of contiguous alar-upper lip defects. J Plast Reconstr Aesthet Surg. 2017 Mar;70(3):330-335.
9. Sukop A, Tvrdek M, Duskova M, Hýza P, Haas M, Bayer J. Nasal reconstruction in children with the combination of nasolabial and island flaps. Acta Chir Plast. 2010;52(1):3-6.
10. Smith JW et al. Grabb and Smith’s plastic surgery. Lippincott-Raven, 1997. pg. 392.
11. McGregor, Ian A., and Alan D. McGregor. Fundamental techniques of plastic surgery: and their surgical applications. Churchill Livingstone, 2000. pg. 178-9.
12. Rose EH. One-stage arterialized nasolabial island flap for floor of mouth reconstruction. Ann Plast Surg. 1981 Jan;6(1):71-5.
13. Turan A, Kul Z, Türkaslan T, Ozyiğit T, Ozsoy Z. Reconstruction of lower half defects of the nose with the lateral nasal artery pedicle nasolabial island flap. Plast Reconstr Surg. 2007 May;119(6):1767-72.
14. Yoon TH, Yun IS, Rha DK, Lee WJ. Reconstruction of various perinasal defects using facial artery perforator-based nasolabial island flaps. Arch Plast Surg. 2013 Nov;40(6):754-60.
15. Durgun M, Özakpınar HR, Selçuk CT, Sari E, Seven E, İnözü E. Repair of Full-Thickness Nasal Alar Defects Using Nasolabial Perforator Flaps. Ann Plast Surg. 2015 Oct;75(4):414-7.
16. Sasaki K, Nozaki M, Katahira J, Kikuchi Y. A nasolabial composite free flap with buccal mucosa: reconstruction of full-thickness lower eyelid defects. Plast Reconstr Surg. 1998 Aug;102(2):464-72.
17. Takeda A, Akimoto M, Park K et al. Single-stage reconstruction of a full-thickness alar defect using a folded nasolabial flap combined with a redundant skin turnover flap. J Craniofac Surg. 2014 Nov;25(6):2144-6.
18. Uchinuma E, Matsui K, Shimakura Y, Murashita K, Shioya N. Evaluation of the median forehead flap and the nasolabial flap in nasal reconstruction. Aesthetic Plast Surg. 1997 Mar-Apr;21(2):86-9.
19. Lindsay KJ, Morton JD. Flap or graft: The best of both in nasal ala reconstruction. J Plast Reconstr Aesthet Surg. 2015 Oct;68(10):1352-7.
20. Weathers WM, Wolfswinkel EM, Nguyen H, Thornton JF. Expanded uses for the nasolabial flap. Semin Plast Surg. 2013 May;27(2):104-9.
21. Lunatschek C, Schwipper V, Scheithauer M. Soft tissue reconstruction of the nose. Facial Plast Surg. 2011 Jun;27(3):249-57.
22. Menick FJ. Practical details of nasal reconstruction. Plast Reconstr Surg. 2013 Apr;131(4):613e-30e.
23. Konofaos P, Alvarez S, McKinnie JE, Wallace RD. Nasal Reconstruction: A Simplified Approach Based on 419 Operated Cases. Aesthetic Plast Surg. 2015 Feb;39(1):91-9.
24. Rohrich RJ, Conrad MH. The superiorly based nasolabial flap for simultaneous alar and cheek reconstruction. Plast Reconstr Surg. 2001 Nov;108(6):1727-30.
25. Thornton JF, Griffin JR, Constantine FC. Nasal reconstruction: an overview and nuances. Semin Plast Surg. 2008 Nov;22(4):257-68.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2017 Issue 3-4-
All articles in this issue
- Editorial
- PATIENT SATISFACTION AFTER BREAST RECONSTRUCTION: IMPLANTS VS. AUTOLOGOUS TISSUES
- OLEOGEL-S10 TO ACCELERATE HEALING OF DONOR SITES: MONOCENTRIC RESULTS OF PHASE III CLINICAL TRIAL
- THE NASOLABIAL FLAP: THE MOST VERSATILE METHOD IN FACIAL RECONSTRUCTION
- CURRENT TREATMENT OPTIONS OF DUPUYTREN´S DISEASE
- SURGICAL TREATMENT OF MELANOMA
- POSTOPERATIVE FIXATION AFTER REPOSITIONING OF PREMAXILLA IN A PATIENT WITH BILATERAL CLEFT LIP AND PALATE – CASE REPORT
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- THE NASOLABIAL FLAP: THE MOST VERSATILE METHOD IN FACIAL RECONSTRUCTION
- CURRENT TREATMENT OPTIONS OF DUPUYTREN´S DISEASE
- PATIENT SATISFACTION AFTER BREAST RECONSTRUCTION: IMPLANTS VS. AUTOLOGOUS TISSUES
- OLEOGEL-S10 TO ACCELERATE HEALING OF DONOR SITES: MONOCENTRIC RESULTS OF PHASE III CLINICAL TRIAL
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

