-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Motor Vehicle Crashes in Diabetic Patients with Tight Glycemic Control: A Population-based Case Control Analysis
Background:
Complications from diabetes mellitus can compromise a driver's ability to safely operate a motor vehicle, yet little is known about whether euglycemia predicts normal driving risks among adults with diabetes. We studied the association between glycosylated hemoglobin (HbA1c) and the risk of a motor vehicle crash using a population-based case control analysis.Methods and Findings:
We identified consecutive drivers reported to vehicle licensing authorities between January 1, 2005 to January 1, 2007 who had a diagnosis of diabetes mellitus and a HbA1c documented. The risk of a crash was calculated taking into account potential confounders including blood glucose monitoring, complications, and treatments. A total of 57 patients were involved in a crash and 738 were not involved in a crash. The mean HbA1c was lower for those in a crash than controls (7.4% versus 7.9%, unpaired t-test, p = 0.019), equal to a 26% increase in the relative risk of a crash for each 1% reduction in HbA1c (odds ratio = 1.26, 95% confidence interval 1.03–1.54). The trend was evident across the range of HbA1c values and persisted after adjustment for measured confounders (odds ratio = 1.25, 95% confidence interval 1.02–1.55). The two other significant risk factors for a crash were a history of severe hypoglycemia requiring outside assistance (odds ratio = 4.07, 95% confidence interval 2.35–7.04) and later age at diabetes diagnosis (odds ratio per decade = 1.29, 95% confidence interval 1.07–1.57).Conclusions:
In this selected population, tighter glycemic control, as measured by the HbA1c, is associated with an increased risk of a motor vehicle crash.
: Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 6(12): e32767. doi:10.1371/journal.pmed.1000192
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000192Summary
Background:
Complications from diabetes mellitus can compromise a driver's ability to safely operate a motor vehicle, yet little is known about whether euglycemia predicts normal driving risks among adults with diabetes. We studied the association between glycosylated hemoglobin (HbA1c) and the risk of a motor vehicle crash using a population-based case control analysis.Methods and Findings:
We identified consecutive drivers reported to vehicle licensing authorities between January 1, 2005 to January 1, 2007 who had a diagnosis of diabetes mellitus and a HbA1c documented. The risk of a crash was calculated taking into account potential confounders including blood glucose monitoring, complications, and treatments. A total of 57 patients were involved in a crash and 738 were not involved in a crash. The mean HbA1c was lower for those in a crash than controls (7.4% versus 7.9%, unpaired t-test, p = 0.019), equal to a 26% increase in the relative risk of a crash for each 1% reduction in HbA1c (odds ratio = 1.26, 95% confidence interval 1.03–1.54). The trend was evident across the range of HbA1c values and persisted after adjustment for measured confounders (odds ratio = 1.25, 95% confidence interval 1.02–1.55). The two other significant risk factors for a crash were a history of severe hypoglycemia requiring outside assistance (odds ratio = 4.07, 95% confidence interval 2.35–7.04) and later age at diabetes diagnosis (odds ratio per decade = 1.29, 95% confidence interval 1.07–1.57).Conclusions:
In this selected population, tighter glycemic control, as measured by the HbA1c, is associated with an increased risk of a motor vehicle crash.
: Please see later in the article for the Editors' SummaryIntroduction
Diabetic patients account for substantial amounts of driving. At a population disease prevalence of 5% to 7% for this diagnosis, general mobility statistics would suggest that diabetic patients drive about 250 million miles during the average day in the United States [1],[2]. Such distances are extraordinary—greater than traveling from the earth to the sun and back [3]. The exact figure could be either somewhat larger if diabetes correlates with a sedentary lifestyle that favors driving or somewhat smaller if diabetes is associated with incapacitating complications that leave the patient institutionalized [4]. The substantial driving distances are likely to continue into the future given societal reliance on road travel for work, recreation, leisure, and health care [5].
On average, a population with a large amount of driving tends to have a large number of crashes. If diabetic drivers were identical to average American adults, the baseline risk of a serious crash would be about one in 20 per year [6]. This number would amount to about five diabetic drivers killed and another 50 incapacitated each day from motor vehicle crashes in the United States. Even for individuals who crash without injuries, the event can disrupt the ideals of regular exercise, a prudent diet, work productivity, and other elements of lifestyle [7]. Impairments from retinopathy, neuropathy, and hypoglycemia might make the average diabetic driver more prone to crashing than the prevailing population average [8].
Governmental policies sometimes restrict the licenses of diabetic drivers on grounds that the disease makes the individual unfit to drive [9]. Different states in the US have different regulations, yet even permissive regions require drivers who hold commercial licenses to document glycemic control [10]–[15]. The laws are based on the theory that glycemic control predicts lower driving risk either by preventing retinopathy and other complications or by indirectly distinguishing persons who are innately conscientious [16],[17]. Guidelines in Canada state, for example, “In general, a patient is considered fit to drive if it can be demonstrated that he or she is fastidious and knowledgeable about controlling his or her blood glucose levels …” [18]. In this study we tested whether glycemic control, as measured by glycosylated hemoglobin (HbA1c), was associated with the risk of a motor vehicle crash.
Methods
Patient Selection
We selected all drivers reported to the Ontario Ministry of Transportation Medical Advisory Board who had an underlying diagnosis of diabetes mellitus. This population-based sampling strategy included all licensed drivers in Ontario with the accrual interval spanning from January 1, 2005 to January 1, 2007, representing all years available for analysis. Candidates were identified from mandatory annual reviews submitted by drivers who held commercial licenses or mandatory reports submitted in the aftermath of a documented motor vehicle crash. We also included all other diabetic patients reviewed for any other reason such as those appealing a license suspension or those with notifiable medical conditions reported by physicians [19]. Individuals were excluded if no HbA1c was available; otherwise, all drivers were analyzed. This study was approved by the Research Ethics Board of Sunnybrook Health Sciences Center and conducted using privacy safeguards at the Institute for Clinical Evaluative Sciences.
Crash Outcome
We classified each individual according to the manner through which they came to the attention of the licensing authority. Individuals involved in a motor vehicle crash were defined as cases. Such cases were identified by the authorities responsible for investigating a crash. All other individuals who were not involved in a motor vehicle crash were defined as controls. Such controls are not a random sample of the population because they come to attention by reports submitted by others or because of legal requirements for having a valid driver's license. Controls ought to include all diabetic drivers who developed diabetes or obtained a license during the study period, but do not because of noncompliance with legislation or other reasons.
Glycemic Control
We obtained the medical record of each person's diabetes care from available files. These records reflect submissions from community physicians corresponding to each patient; the accuracy of these reports has never been validated although each is submitted and signed by a licensed physician [20]. We used the hemoglobin HbA1c as the primary measure of long term blood glucose control since it reflects glycemic control over 2 to 3 mo, is widely available with a liquid chromatography assay, and is the objective standard for traffic policy decisions around the world [21],[22]. In secondary analyses we also examined the patients' degree of monitoring, total years since diagnosis of diabetes, and specific complications. These secondary analyses were conducted for exploratory purposes and did not involve statistical power calculations in advance.
Missing Data
Missing data were handled using methods blind to outcome status. The type of diabetes was not always recorded in available documents; instead, we classified individuals on the basis of whether they had started insulin treatment before or after age 20 y. The duration of diabetes was also gauged by categorizing patients who had been on insulin for 20 y or more. Data on specific complications, monitoring, and treatments were accepted as recorded under the assumption that not documented implied not present. Information on diet, exercise, weight, compliance, alcohol, lifestyle, age of first licensing, driving patterns, commercial licenses, past infractions, diabetic education, visual acuity, and at-fault analysis was not recorded and deemed not possible to impute from sources.
Statistical Analysis
Our primary analysis compared the mean HbA1c among cases involved in a crash to controls who were not involved in a crash using an unpaired t-test with two-tailed statistics. Logistic regression was used to quantify associations using odds ratios and adjusting for baseline confounders using a step-wise forward selection procedure (models constrained to 12 events per covariate to avoid overfitting and used the c-statistic to gauge overall accuracy) [23]. Odds ratios are good approximations of relative risk for low probability events (such as the annual risk of a crash) [24]. A nonparametric test for trend was also conducted using the Cochran-Armitage method [25]. Data validation was conducted blind to outcome to correct HbA1c values outside the plausible range (4.0%–16.0%) for magnitude anomalies (e.g., 6.5% reported as 0.65 or 0.065). The sample size was estimated to provide 80% power to detect a 0.5% difference in HbA1c between the two groups of patients.
Results
During the 2-y study interval a total of 3,900 individuals were reported to licensing authorities, of whom 795 were diabetic patients who had HbA1c values documented. Their mean age was 52 y, 84% were men, and the average patient had about a 20-y history of diabetes (Table 1). Most patients had end organ damage including retinopathy, nephropathy, and neuropathy. About 81% were treated with insulin, 27% with oral glucose-lowering medications, and 15% with neither insulin nor an oral medication. Overall, one in six lacked hypoglycemic awareness and one-third had a history of hypoglycemia that required outside assistance. The spread of HbA1c values was remarkable, ranging from 4.4% to 14.7%.
Tab. 1. Patient characteristics. 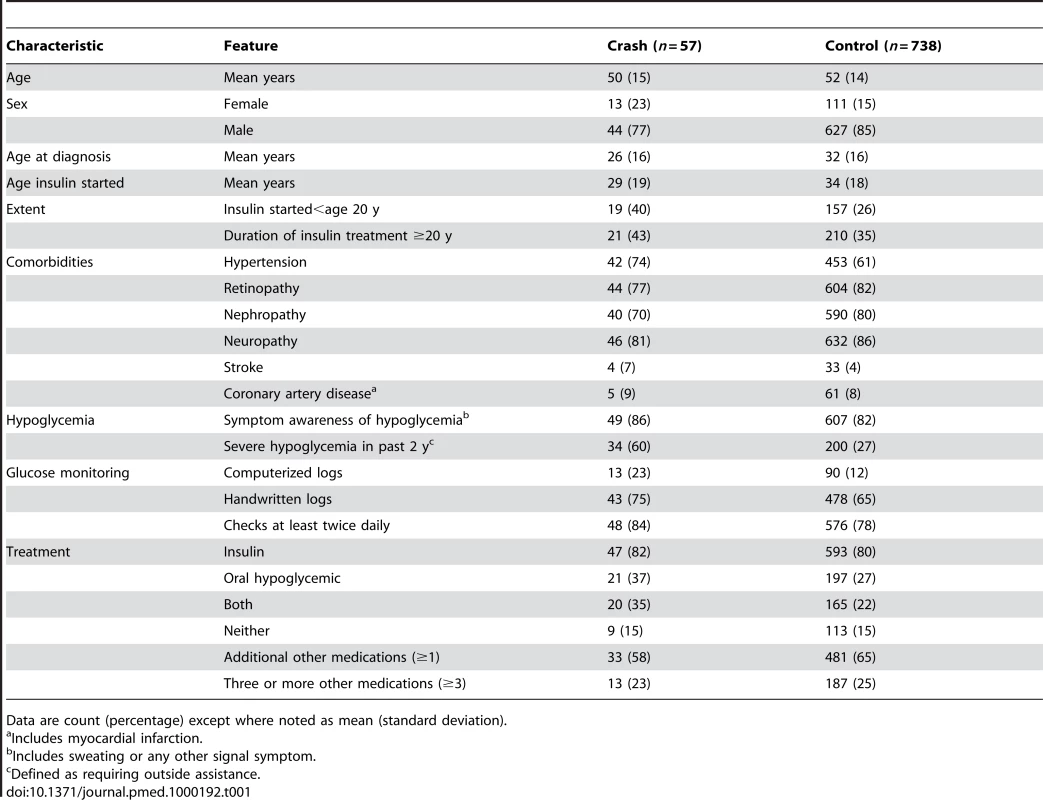
Data are count (percentage) except where noted as mean (standard deviation). Overall, 57 patients were involved in a crash (cases) and 738 were not involved in a crash (controls). In keeping with a potential adverse association, the mean HbA1c was lower among those who crashed than controls (7.4% versus 7.9%, p = 0.019). This association was equivalent to a 26% increase in the risk of a crash for each 1% reduction in HbA1c (odds ratio = 1.26, 95% confidence interval 1.03–1.54). The finding was evident across the range of HbA1c values and suggested that the risk of a crash in the bottom quartile was more than twice the risk in the top quartile (Figure 1). The absolute difference amounted to a net increase of 29 total crashes (95% confidence interval 16–46) had the risk in the highest quartile extended to all other quartiles.
Fig. 1. Glycemic control and risk of a motor vehicle crash. 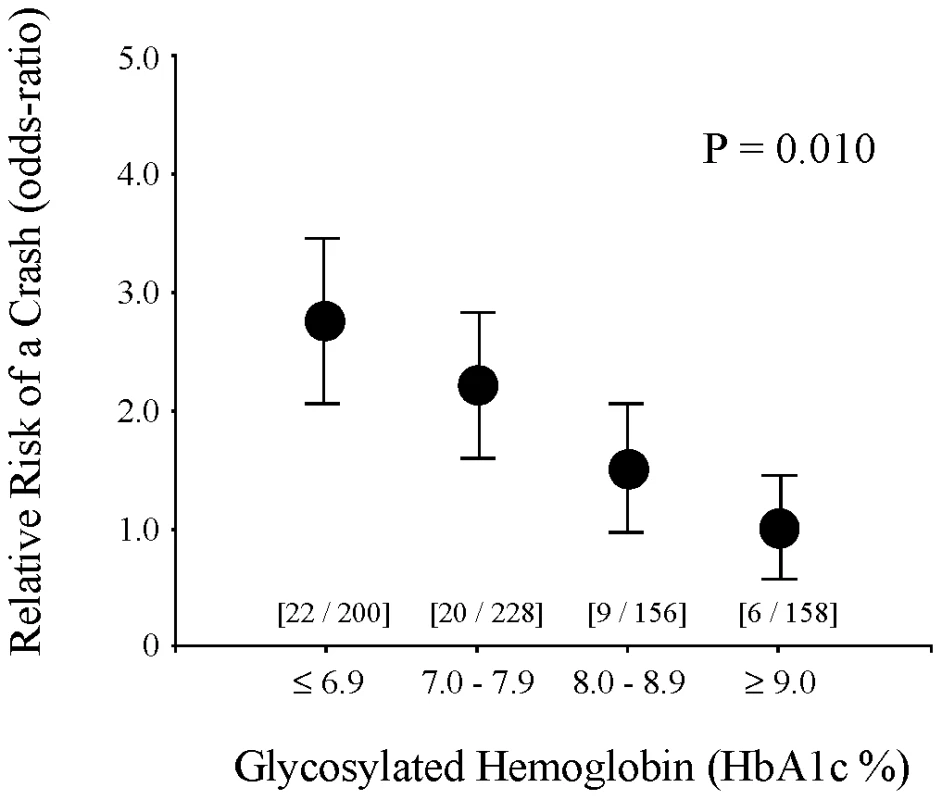
Relative risk of a motor vehicle crash for drivers at different levels of glycemic control. x-Axis shows glycemic control as measured by glycosylated hemoglobin concentration and grouped into approximate quartiles. Data in square brackets show individuals in each group as [number of cases/number of controls]. y-Axis shows relative risk of a crash expressed in odds-ratio calibrated using the top glycemic quartile as referent. Solid circles indicate point-estimates and vertical lines indicate standard error bars. p-Value tests for trend across all four quartiles. Overall results show a correlation between lower HbA1c levels and higher relative risk of a crash with no evidence of a U-shaped relationship. The observed association between low HbA1c values and increased crash risks tended to be consistent for patients with different characteristics (Figure 2). The risk was observed for patients with longer and shorter durations of diabetes, regardless of whether measured as time since diagnosis or time since starting insulin. Moreover, the risk was observed for those treated with insulin, oral hypoglycemics, both, or neither. In addition, the risk extended to those with no mention of severe hypoglycemia, hypoglycemic unawareness, or other specific chronic complications. The largest single anomaly (yet not statistically significant and overlapping the main analysis) was the subgroup not treated with insulin or oral hypoglycemic medications.
Fig. 2. Crash risk in different subgroups. 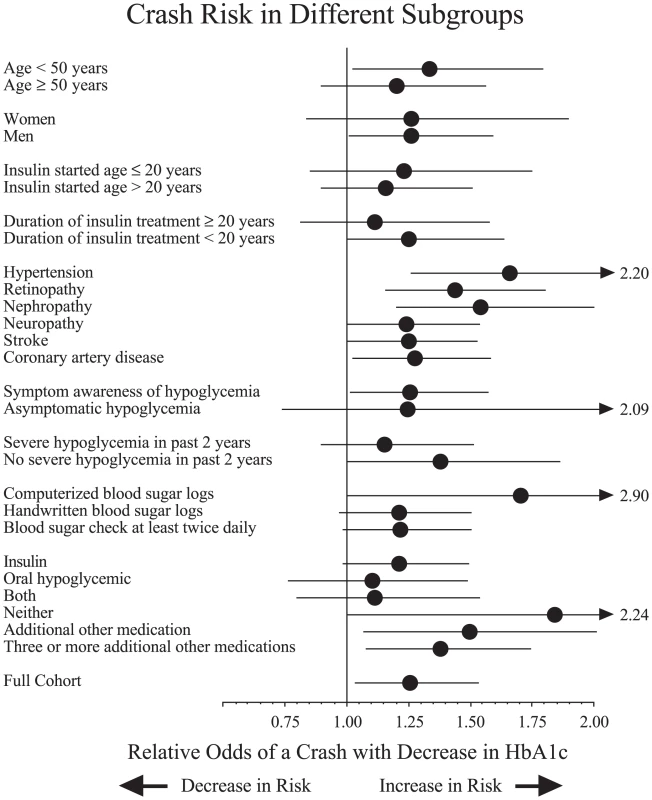
Each analysis examines correlation of lower HbA1c levels with higher risk of a crash. Results expressed as odds ratio (solid circle) and 95% confidence interval (horizontal line) per 1% point decrease in HbA1c. Analyses of chronic complication subgroups exclude patients reporting corresponding symptom. Results for full cohort appear at bottom and show an odds ratio of 1.26 with 95% confidence interval 1.03–1.54. The observed association between low HbA1c values and increased crash risks persisted when adjusted for potential confounders. Analyses adjusting for age yielded approximately the same increase in the relative risk of a crash for each 1% reduction in HbA1c (odds ratio = 1.27, 95% confidence interval 1.04–1.55). Similarly, analyses adjusting for age, age at diagnosis, and age when insulin started also yielded a comparable increase in the risk of a crash (odds ratio = 1.26, 95% confidence interval 1.00–1.58). Analyses adjusting for both age, gender, and each separate complication also yielded about a 25% increase in the risk of a crash for each 1% reduction in HbA1c (odds ratio range 1.20–1.30). None of the statistical models yielded a contrary result although results in some models were not statistically significant.
Two other patient characteristics were independent risk factors for a crash. A history of severe hypoglycemia that required outside help was associated with about a 4-fold increase in risk (odds ratio = 4.07, 95% confidence interval 2.35–7.04). In addition, older age of diabetes diagnosis (expressed as increase per decade) was also associated with an increase in risk (odds ratio = 1.29, 95% confidence interval 1.07–1.57). No other baseline characteristic (Table 1) was a significant predictor of risk in univariate analyses. Multivariate analysis that included both severe hypoglycemia requiring outside help and age at diabetes diagnosis had a mid-range overall accuracy (c-statistic = 0.65) and showed a persistent association of HbA1c with crash risk (odds ratio = 1.25, 95% confidence interval 1.02–1.55).
Discussion
We studied a selected sample of diabetic adults driving during a 2-y interval using a population-based approach. The main finding was that lower HbA1c levels were associated with an increased risk of a motor vehicle crash. The adverse association was observed across the range of HbA1c values, persisted after adjustment for independent confounders, yet was not as large as the relative risk associated with a history of severe hypoglycemia requiring outside assistance. The attributable risk was substantial, so that eliminating the association by extrapolating the risk observed at the highest HbA1c quartile to all drivers at all HbA1c quartiles would have eliminated about half of all observed crashes. These findings are difficult to explain with random chance, reverse-causality, or simple reporting bias.
A major limitation of our research relates to the nonrandomized design and sample selection. That is, adults with diabetes self-select how to control their glucose as well as how to drive a vehicle. One explanation for the association, therefore, could be that those who are stringent about controlling their blood glucose are paradoxically more careless about driving a vehicle. Another explanation could be that tightly controlled patients drive in more dangerous settings. A third explanation could be that unreported alcohol consumption influences both driving risk and glucose control (e.g., impaired liver glucogenesis). Many other biases are possible including Berkson's paradox, Neyman Bias, Hawthorn effects, restricted generalizability, imperfect compliance with the law, and spectrum bias [19],[26]. These limitations are unavoidable in trauma research except for studies that focus on volunteer samples, unnatural tasks, or hypothetical risks [27].
We have no data on baseline time spent driving, yet such data are unlikely to explain our findings. First, all individuals maintained valid licenses, remained active in the community, and were at risk for a crash. Second, no prior study shows diabetic adults drive substantially more than the prevailing average (or that small differences in HbA1c predict large differences in driving time) [28]. Third, research in other domains indicates time spent driving is a poor predictor of crash risk; for example, teenagers account for a large number of crashes despite a small amount of time spent driving and senior citizens have a heightened risk primarily explained by the very low distance drivers [29],[30]. No surprise, therefore, that license regulations account for fitness to drive but have no restrictions based on the amount of driving the person intends.
Our findings join a growing and contentious literature correlating low HbA1c values with adverse consequences in adults with diabetes mellitus. For example, three recent randomized trials found that intensive treatment regimens led to both lower HbA1c values and an increased incidence of severe hypoglycemia among diabetic patients [31]–[33]. These trials and our study do not prove that striving for a normal HbA1c is harmful; instead, the adverse association might indicate that customary treatments for achieving euglycemia are inexact and potentially hazardous to high level cognitive behavior [34]–[37]. Many patients, furthermore, are aware of their HbA1c results so that a double-blinded trial becomes unfeasible and susceptible to subtle confounders. Such behavioral factors are germane in clinical research since patients with a normalized HbA1c might develop a false sense of security whereas those with a high HbA1c might abandon their activities and ironically become protected from mobility related injury [38].
The basic implication of our study is to underscore the difficulty in judging fitness-to-drive in adults with severe diabetes mellitus [39]. This pitfall calls into question traffic laws that prevail in the United States, United Kingdom, Canada, Germany, Holland, Australia, and other countries that single out diabetic patients for specialized review. At a minimum, the data suggest that a patient's HbA1c level is neither necessary nor sufficient for determining fitness-to-drive. Whether a comprehensive medical review, functional performance assessment, formal driving test, detailed record of hypoglycemia episodes, or other measure could be more accurate and cost-effective remains a topic for future research. Unfortunately, most other measures of diabetes control are based on self-report that can be easily denied when applying for a driving license.
Zdroje
1. Fatality analysis reporting system encyclopedia Washington (D.C.) National Highway Traffic Safety Administration Available: http://www-fars.nhtsa.dot.gov/Main/index.aspx. Accessed 15 October 2009
2. Centers for Disease Control and Prevention 2005 National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Available: http://www.diabetes.org/uedocuments/NationalDiabetesFactSheetRev.pdf. Accessed 15 October 2009
3. Wikipedia, the Free Encyclopedia. Astronomical unit. Available: http://en.wikipedia.org/wiki/Astronomical_unit. Accessed 15 October 2009
4. EvansL
2004 Traffic safety Bloomfield Hills (Michigan) Science Serving Society 444
5. StegL
VlekC
SlotegraafG
2001 Instrumental-reasoned and symbolic-affective motives for using a motor car. Transportation Research Part F: Psychology and Behaviour 4 151 169
6. RedelmeierDA
WeinsteinMC
1999 Cost-effectiveness of regulations against using a cellular telephone while driving. Med Decis Making 19 1 8
7. WinstonFK
Kassam-AdamsN
Vivarelli-O'NeillC
FordJ
NewmanE
2002 Acute stress disorder symptoms in children and their parents after pediatric traffic injury. Pediatrics 109 e90
8. MarshallSC
2008 The role of reduced fitness to drive due to medical impairments in explaining crashes involving older drivers. Traffic Inj Prev 9 291 298
9. LangfordJ
BraitmanK
CharltonJ
EberhardJ
O'NeillD
2008 Licensing authorities' options for managing older driver safety—practical advice from the researchers. Traffic Inj Prev 9 278 281
10. DistillerLA
KramerBD
1996 Driving and diabetics on insulin therapy. S Afr Med J 86 1018 1020
11. FlanaganDE
WatsonJ
EverettJ
CavanD
KerrD
2000 Driving and insulin–consensus, conflict or confusion? Diabet Med 17 316 320
12. CundyT
DruryP
2000 Vocational driving, diabetes and insulin use. N Z Med J 113 317 318
13. PolakBC
van RijnLJ
KorverC
2003 Fitness to drive in people with diabetes mellitus; a recommendation from the Health Council of the Netherlands. Ned Tijdschr Geneeskd 147 1243
14. MarcinkiewiczA
SzoslandD
2007 Medical certification for diabetic drivers in the selected European Union member states. Med Pr 58 541 546
15. JornayvazFR
RagusoCA
PhilippeJ
2007 Diabetes mellitus and driving. Rev Med Suisse 3 1437 1438, 1440–1441
16. GillG
DurstonJ
JohnstonR
MacLeodK
WatkinsP
2002 Insulin-treated diabetes and driving in the UK. Diabet Med 19 435 439
17. American Diabetes Association 2004 Standards of medical care in diabetes. Diabetes Care 27 S15 S35
18. Canadian Medical Association 2006 Section 17: Endocrine and metabolic disorders. 74 81 Determining medical fitness to operate motor vehicles. CMA driver's guide, 7th edition Available: http://www.cma.ca/multimedia/CMA/Content_Images/Inside_cma/WhatWePublish/Drivers_Guide/Section17_e.pdf. Accessed 15 October 2009
19. RedelmeierDA
VenkateshV
StanbrookMB
2008 Mandatory reporting by physicians of patients potentially unfit to drive. Open Medicine 2 8 17
20. Ontario Ministry of Transportation Driver Improvement Office 2009 Medical review section. Available: http://www.mto.gov.on.ca/english/dandv/driver/medical-review/. Accessed 15 October 2009
21. CarpinelliA
MoscaA
BoniniP
1986 Evaluation of a new semi-automated high-performance liquid chromatography method for glycosylated haemoglobins. J Automat Chem 8 192 196
22. ManleyS
JohnWG
MarshallS
2004 Introduction of IFCC reference method for calibration of HbA1c: implications for clinical care. Diabetic Med 21 673 676
23. PeduzziP
ConcatoJ
KemperE
HolfordTR
FeinsteinAR
1996 A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49 1373 1379
24. HulleySB
CummingsSR
1988 Designing clinical research Baltimore Williams and Wilkins 250
25. NeuhauserM
HothornLA
1999 An exact Cochran-Armitage test for trend when dose-response shapes are a priori unknown. Comput Stat Data Anal 30 403 412
26. SackettDL
1979 Bias in analytic research. J Chron Dis 32 52 63
27. FildesBN
2008 Future directions for older driver research. Traffic Inj Prev 9 387 393
28. DanaeiG
DingEL
MozaffarianD
TaylorB
RehmJ
2009 The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 6 e1000058 doi:10.1371/journal.pmed.1000058
29. WilliamsAF
2009 Licensing age and teenage driver crashes: a review of the evidence. Traffic Inj Prev 10 9 15
30. EberhardJ
2008 Older drivers' “high per mile crash involvement”: the implications for licensing authorities. Traffic Inj Prev 9 284 290
31. Action to Control Cardiovascular Risk in Diabetes Study Group 2008 Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358 2545 2559
32. ADVANCE Collaborative Group 2008 Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358 2560 2572
33. DuckworthW
AbrairaC
MoritzT
RedaD
EmanueleN
2009 Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 360 129 139
34. WeingerK
KinsleyBT
LevyCJ
BajajM
SimonsonDC
1999 The perception of safe driving ability during hypoglycemia in patients with type 1 diabetes mellitus. Am J Med 107 246 253
35. ClarkeWL
CoxDJ
Gonder-FrederickLA
KovatchevB
1999 Hypoglycemia and the decision to drive a motor vehicle by persons with diabetes. JAMA 282 750 754
36. CoxDJ
Gonder-FrederickLA
KovatchevBP
JulianDM
ClarkeWL
2000 Progressive hypoglycemia's impact on driving simulation performance. Occurrence, awareness and correction. Diabetes Care 23 163 170
37. StorkAD
van HaeftenTW
VenemanTF
2007 The decision not to drive during hypoglycemia in patients with type 1 and type 2 diabetes according to hypoglycemia awareness. Diabetes Care 30 2822 2826
38. KennedyRL
HenryJ
ChapmanAJ
NayarR
GrantP
2002 Accidents in patients with insulin-treated diabetes: increased risk of low-impact falls but not motor vehicle crashes–a prospective register-based study. J Trauma 52 660 666
39. BeggIS
YaleJF
HouldenRL
RoweRC
McSherryJ
2003 Canadian Diabetes Association's clinical practice guidelines for diabetes and private and commercial driving. Can J Diabetes 27 128 148
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2009 Číslo 12- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Magnosolv a jeho využití v neurologii
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
Nejčtenější v tomto čísle- Motor Vehicle Crashes in Diabetic Patients with Tight Glycemic Control: A Population-based Case Control Analysis
- Sexual Inequality in Tuberculosis
- A New Year's Wish List for Authors, Reviewers, Readers—and Ourselves
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



