-
Medical journals
- Career
Current Recommendations of the International League Against Epilepsy for the Treatment of Seizures in Newborns
21. 5. 2024
In 2023, a team of experts in neurology, neonatology, and pediatrics, along with representatives of parents, published recommendations for the treatment of epileptic seizures in newborns. These were developed based on a systematic literature review (and in cases of insufficient evidence, based on consensus achieved using the Delphi method) and include first and second choice pharmacotherapy, dosing, duration of treatment, effects of therapeutic hypothermia, and the use of pyridoxine. We offer their summary in a nutshell (and always indicate the strength of the recommendation in parentheses).
Recommendations
- For newborns with seizures requiring anti-seizure medication (ASM), phenobarbital should be the first choice. (moderate, literature-based recommendation)
- Phenobarbital should be administered as the first-line treatment regardless of seizure etiology (hypoxic-ischemic encephalopathy /HIE/, stroke, hemorrhage). (high, consensus-based recommendation)
- If channelopathy is a probable cause of the seizure based on family history, the first-choice ASM may be phenytoin or carbamazepine (sodium channel blocker). (high, consensus-based recommendation)
- If the newborn does not respond to the first-line ASM, phenytoin or levetiracetam may be used as second-line for most etiological causes (HIE, stroke, hemorrhage). Another option is midazolam or lidocaine. (moderate, consensus-based recommendation)
- If channelopathy is suspected based on clinical or EEG characteristics, a sodium channel blocker like phenytoin or carbamazepine based on clinical status (critically ill or otherwise well) and local ASM availability can be used as a second-line ASM. (high, consensus-based recommendation)
- For newborns with heart disease, levetiracetam may be preferred as second-line. (moderate, consensus-based recommendation)
- If acute provoked seizures (electroclinical or electrographic) resolve without evidence of neonatal epilepsy, ASM can be discontinued before discharge regardless of MRI or EEG findings. (high, consensus-based recommendation)
- Therapeutic hypothermia may reduce seizure occurrence in term newborns with HIE. The impact of therapeutic hypothermia as a specific anti-seizure treatment, however, has not been evaluated. (weak, literature-based recommendation)
- Therapeutic hypothermia can reduce seizure incidence in newborns with HIE. (high, consensus-based recommendation)
- Treating neonatal seizures (including electrographic-only seizures) to achieve reduced seizure occurrence can be associated with better neurological development and reduced risk of subsequent epilepsy. (moderate, consensus-based recommendation)
- For newborns with clinical or EEG signs indicative of pyridoxine-dependent epilepsy, and those who do not respond to second-line ASM and have undetermined seizure etiology, adding pyridoxine to ASM can be tried. (high, consensus-based recommendation)
- Each neonatal unit should have a standard protocol for managing neonatal seizures. (high, consensus-based recommendation)
- Parents/caregivers of newborns with seizures should be informed about the condition, including possible causes and initial treatment options. Subsequent discussions should be guided by the newborn's condition. (high, consensus-based recommendation)
Fig. Algorithm for the treatment of seizures in newborns
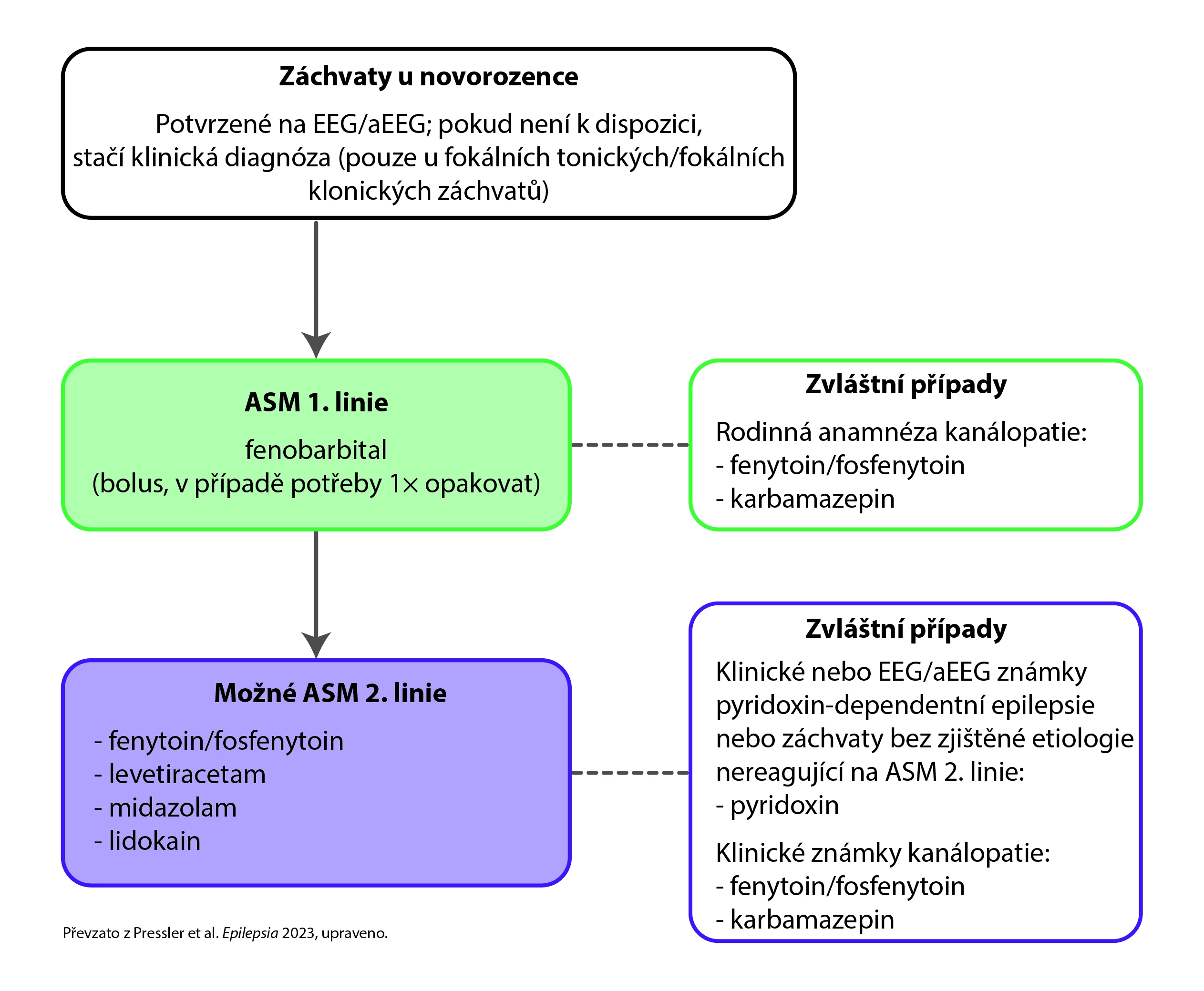
Table. Dosing of anti-seizure medications in newborns
Phenobarbital
- Loading dose 20 mg/kg IV
- If needed, second loading dose 10–20 mg/kg IV
- Maintenance dose 5 mg/kg/day PO in a single dose
Phenytoin/Fosphenytoin
- Loading dose 20 mg/kg IV over 30 minutes
- Maintenance dose 5 mg/kg/day IV or PO in 2 doses, adjusted by plasma concentration up to 7.5 mg/kg/dose
- Target level 10–20 µg/ml
Levetiracetam
- Loading dose 40 mg/kg IV
- If needed, second loading dose 20 mg/kg IV
- Maintenance dose 40–60 mg/kg/day IV or PO in 3 doses
Lidocaine
- Loading dose 2 mg/kg IV over 10 minutes
- Maintenance dose 7 mg/kg/hour IV for 4 hours, then 3.5 mg/kg/hour for 12 hours, then 1.75 mg/kg/hour for 12 hours, then stop
- Adjust dose according to birth weight, gestational age, and therapeutic hypothermia
Midazolam
- Loading dose 0.05–0.15 mg/kg
- Maintenance dose 60 µg/kg/hour in continuous infusion, titrating gradually by 1 µg/kg/min up to 5 µg/kg/min (= 300 µg/kg/hour)
Carbamazepine
- 10 mg/kg/day PO in 2 doses
Pyridoxine Hydrochloride
- Loading dose 100 mg IV or PO, then 30 mg/kg/day IV or PO in 2 doses for 3–5 days
(zza)
Source: Pressler R. M. et al. Treatment of seizures in the neonate: Guidelines and consensus-based recommendations-Special report from the ILAE Task Force on Neonatal Seizures. Epilepsia 2023 Oct; 64 (10): 2550−2570, doi: 10.1111/epi.17745.
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Neurology Paediatrics General practitioner for children and adolescents
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


