-
Medical journals
- Career
Don't Hesitate to Refer a Patient to the MS Center: Time is Brain! Or What Recent Czech Research Has Shown?
17. 5. 2024
Time is crucial for every disease, but it is doubly true for diseases of the nervous system! Why is it important to diagnose and treat multiple sclerosis (MS) early? How to do it? And how are we doing with speed here in the Czech Republic?
Introduction: The First Meters are Decisive
Multiple sclerosis is a serious disease of the central nervous system. It is a chronic disease; its treatment is therefore a long-term process. However, the key in this process is the first meters! In the early stages of the disease, inflammatory activity prevails, which can now be very effectively therapeutically suppressed. Over time, however, neurodegeneration begins to dominate, which medicine is still unable to effectively influence. Moreover, inflammatory activity gets sealed off behind the blood-brain barrier, making it harder for medications to reach the pathological site.
There is already a substantial body of evidence confirming better clinical outcomes, fewer relapses, less disability, fewer inflammatory lesions on magnetic resonance imaging (MRI), and less atrophy in patients with early therapy. For this reason, many national and international recommendations set a period of 7−12 weeks between the first symptom and the diagnosis. How does the Czech Republic stand in fulfilling this time frame? And at what point does any delay usually occur?
What did the Czech observational study reveal?
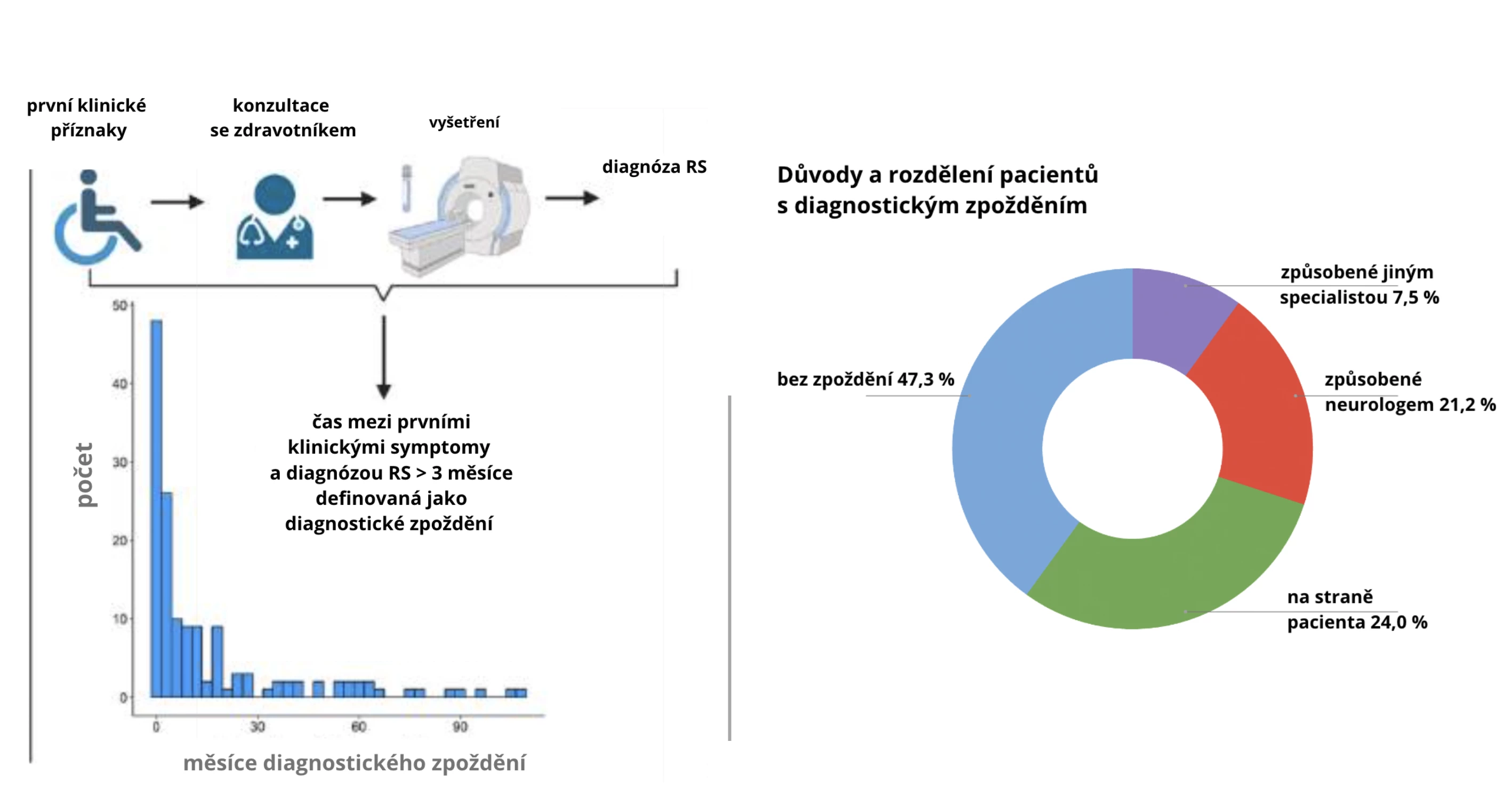
The frequency of diagnostic delays and their causes were the focus of Czech authors in their monocentric observational study. They evaluated diagnostic delays in 146 patients with relapsing-remitting MS (RRMS) newly diagnosed between November 2016 and February 2021. Diagnostic delay was defined as the time between the first symptom and the diagnosis being longer than 3 months. Information was gathered during initial examinations and supplemented by subsequent semi-structured telephone interviews.
Delay? For most!
Diagnostic delay was identified in 52.7% of patients. In 45.9% of cases, the delay was longer than 6 months, in 40.4% of cases, it was longer than 9 months, in 32.9% of cases longer than 12 months, and in 21.2% of cases, the delay was even longer than 2 years. This also relates to the fact that 43.2% of patients led to diagnosis only after at least a second attack.
Even more alarming is the fact that in 28.7% of respondents, the cause of the delay was on the side of healthcare providers (see table and chart). The most common cause was an incorrect diagnosis by a neurologist (22 cases) due to not completing the full diagnostic process or misinterpreting findings, often concluding the etiology as peripheral. In 4.7% of cases, the reason for the delay in the diagnostic process was long waits for paraclinical examinations or late referral to the MS center.
In most cases, however, the cause of the diagnostic delay lay on the patient's side, which suggests a need for better public awareness and shows that despite the perceived adequate information among the Czech public, the situation is far from satisfactory. Patients cited reasons such as minimal severity of symptoms (19 cases), attributing symptoms to stress (7 cases), and spontaneous resolution of symptoms (6 cases).
Fig. Study Layout
 Tab. Determinants of Diagnostic Delay
Tab. Determinants of Diagnostic Delay
Causes of Diagnostic Delay number (%)*, n = 77 Patient 35 (45.5%) − mild symptoms 19 (24.7%) − related to psychological stress 7 (9.1%) − full remission 6 (7.8%) − related to pregnancy 1 (1.3%) − related to migraine symptoms 1 (1.3%) − couldn't find time to visit a doctor 1 (1.3%) Doctor (or other healthcare provider) 42 (54.5%) − misdiagnosis by neurologist 22 (28.6%) − slow diagnostic process by neurologist (MRI > 2 months; referral to MS center > 2 months) 7 (9.1%) − misdiagnosis by ophthalmologist 6 (7.8%) − neurologist waiting for MRI to confirm diagnosis 2 (2.6%) − misdiagnosis by otolaryngologist 2 (2.6%) − misdiagnosis by general practitioner 1 (1.3%) − misdiagnosis by orthopedist 1 (1.3%) − misdiagnosis by physiotherapist 1 (1.3%) Note: *Share of group of 77 patients with diagnostic delay.Time Has Taken Its Toll
The fact that this is not just a theoretical problem was subsequently demonstrated by the authors in evaluating negative prognostic markers at the time of diagnosis. Diagnostic delay was associated with a trend of greater clinical disability assessed by the Kurtzke Expanded Disability Status Scale (EDSS), a greater total lesion volume, greater infratentorial lesion volume on MRI, and higher concentrations of light neurofilament chains in cerebrospinal fluid.
Better, but not enough
Diagnostic delay in the Czech cohort was comparable to delays published from various countries and regions worldwide. Compared to historical data, it was even shorter, likely due to the more sensitive McDonald diagnostic criteria published in 2017. Yet, there is no time to rest on our laurels. Although half of the patients diagnosed within 3 months may seem a good result to some, one-third of patients diagnosed after more than 1 year is truly alarming. How to address this?
Conclusion: Cooperation is Key
In addition to educating the Czech and broader professional community, it is also crucial to optimize procedures and cooperation between referring neurologists and MS centers. Ideally, patients suspected of multiple sclerosis should be referred for further examination at a facility experienced in diagnosing this disease and its associated MS center. This will enable early diagnosis as well as ensuring continuity and early initiation of therapy. It is also crucial to perform MRI examinations using a standardized protocol according to recently published national recommendations and ideally on a machine that will also be used for follow-up. Patients with radiologically isolated syndrome should also be referred to MS centers.
And most importantly, it is crucial to always keep in mind that treatment delay at the onset of the disease has a significant impact on the rest of the patient's life. The price of diagnostic delay is the loss of brain reserve and the window for the most effective therapeutic intervention. Simply put, the well-known statement that “time is brain” holds true without exception.
(dos)
Sources:
1. Uher T., Adzima A., Srpová B. et al. Diagnostic delay of multiple sclerosis: prevalence, determinants, and consequences. Mult Scler J 2023; 29 (11−12): 1437−1451, doi: 10.1177/13524585231197076
2. Vaněčková M., Horáková D., Šťastná D. et al. Standardization of MR utilization in the management of multiple sclerosis: Consensus of the Czech expert radiological-neurological panel. Česká a slovenská neurologie a neurochirurgie 2024; 87 (1): 69−78. doi: 10.48095/cccsnn202469.
3. Kubala Havrdová E. et al. Clinical recommended guideline for the diagnosis and treatment of multiple sclerosis and neuromyelitis optica spectrum disorder. version 3.0. Czech Neurological Society CLS JEP, December 2023. Available at: www.czech-neuro.cz/content/uploads/2023/12/standard_rs_a_nmosd_2023__v13.pdf
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Neurology
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


