-
Medical journals
- Career
Updated Recommendations of the European Society of Cardiology for the Treatment of HCM
28. 4. 2024
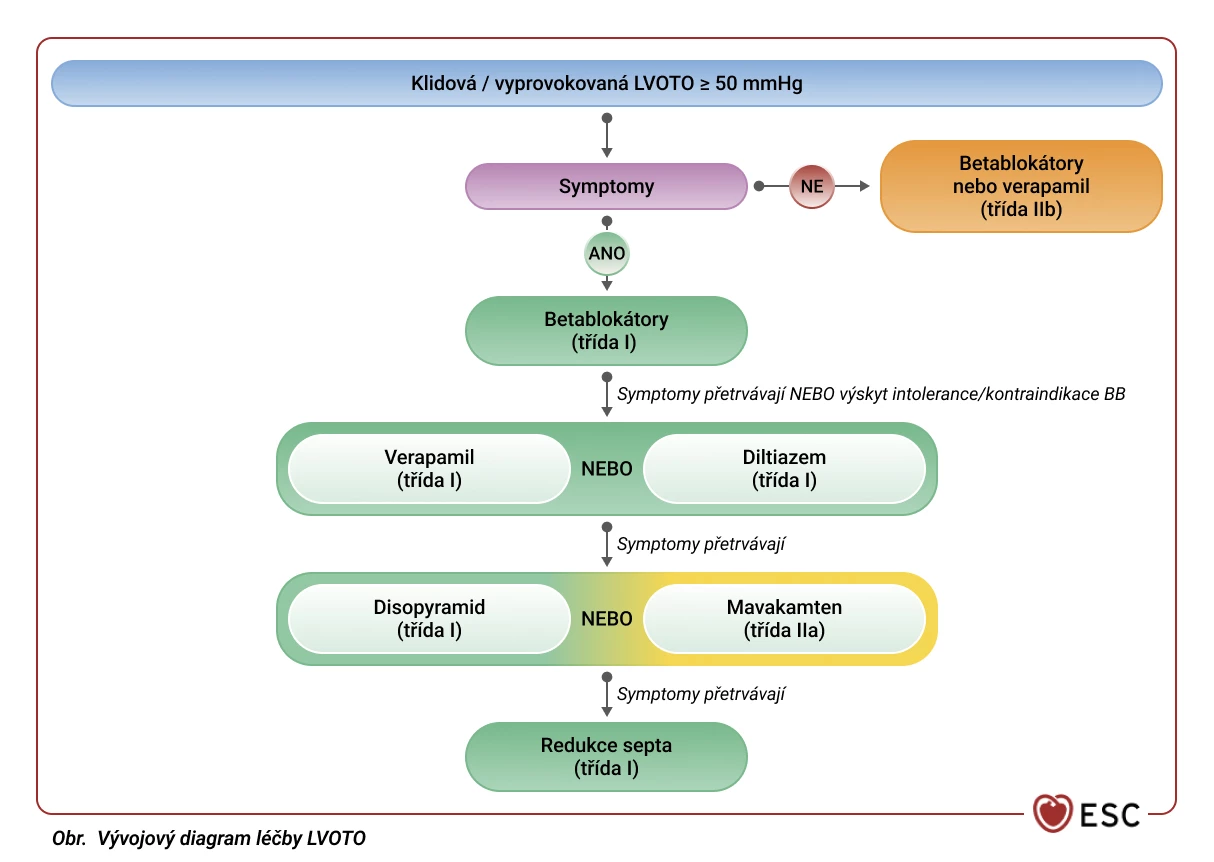
Newly published guidelines by the European Society of Cardiology (ESC) bring several updates in the care of patients with cardiomyopathies. In the following excerpt, we focus on new recommendations for the pharmacotherapy of hypertrophic cardiomyopathy (HCM) in the case of left ventricular outflow tract obstruction (LVOTO).
Definition of HCM and LVOTO
In adults, hypertrophic cardiomyopathy is defined by a left ventricular wall thickness of ≥ 15 mm in any myocardial segment, which cannot be justified by its loading. A smaller degree of wall thickening (13–14 mm) requires further evaluation, including family history, genetic testing, and ECG abnormalities.
Hypertrophic cardiomyopathy often leads to obstruction of the left ventricular outflow tract (LVOTO). It is important to identify LVOTO in HCM patients to address disease symptoms and assess the risk of sudden cardiac death. All HCM patients should have transthoracic 2D and Doppler echocardiography at rest and during the Valsalva maneuver in sitting and semi-recumbent positions at their initial evaluation, and if no gradient is detected, also while standing to detect LVOTO.
LVOTO is defined as a peak instantaneous gradient in the left ventricular outflow tract at Doppler examination of ≥ 30 mmHg. The threshold for invasive treatment is usually a gradient of ≥ 50 mmHg.
General Recommendations for LVOTO
Patients with LVOTO should avoid dehydration and excessive alcohol use, while weight loss is desirable and should be encouraged by physicians. To prevent potential exacerbation of LVOTO, the administration of vasodilators, including nitrates and phosphodiesterase 5 inhibitors (PDE5i), is discouraged. The use of digoxin is also advised against.
Newly diagnosed or poorly controlled atrial fibrillation can worsen LVOTO symptoms, which is why efforts should be made to quickly restore sinus rhythm or control ventricular rate.
Pharmacotherapy for LVOTO
Most patients with a resting or provocable LVOT gradient of < 50 mmHg should be treated according to recommendations for non-obstructive HCM. In a small number of cases with a gradient of 30–50 mmHg without an obvious cause, intervention to reduce the gradient may be considered, although data on this group are insufficient. Most asymptomatic LVOTO patients do not require treatment; however, pharmacological treatment to reduce left ventricular pressures may be considered in selected cases.
Diagram. LVOTO Treatment Flowchart
Note:
Provocable LVOT obstruction is defined as LVOTO provoked by the Valsalva maneuver, upright exercise, or nitrates (if exercise is not possible).
During the titration of disopyramide, the QT interval should be monitored, and if it extends beyond 500 ms, the disopyramide dose should be reduced.The latest pharmacotherapy recommendations for LVOTO are divided by the strength of recommendation, with class I recommendations representing the strongest scientific evidence for a given finding.
Class I Recommendations, Level B
For patients with resting or provocable LVOTO, first-line treatment should be non-vasodilating beta-blockers (BB), titrated to the maximum tolerated dose. If symptoms persist or in cases of intolerance or contraindication to BB, verapamil or diltiazem titrated to the maximum tolerated dose can be used.
As (additional) add-on therapy, disopyramide can be titrated to the maximum dose in combination with BB or verapamil or diltiazem.
Class IIa Recommendations, Level A
In addition to BB or verapamil or diltiazem, the heart myosin-ATPase inhibitor mavacamten titrated to the maximum tolerated dose based on monitoring left ventricular ejection fraction with echocardiographic examination can be considered.
Class IIa Recommendations, Level B
In cases of intolerance or contraindication to BB, verapamil/diltiazem, or disopyramide, mavacamten can be indicated as monotherapy for symptomatic patients.
Class IIa Recommendations, Level C
In patients with severe provocable LVOTO with hypotension and acute pulmonary edema who do not respond to fluid administration, BB (orally or intravenously) and vasoconstrictors should be considered.
Class IIb Recommendations, Level C
For symptomatic patients who cannot be treated with BB, verapamil, or diltiazem, disopyramide titrated to the maximum tolerated dose can be indicated as monotherapy. Low doses of diuretics can be cautiously considered to improve exertional dyspnea in symptomatic patients. In selected asymptomatic patients, BB or verapamil may be used to reduce left ventricular pressures.
Conclusion
In addition to traditionally indicated medications used in the treatment of LVOTO in HCM patients, such as beta-blockers or verapamil or diltiazem, the ESC guidelines also introduce the relatively newly registered drug mavacamten. First-line therapy continues to be BB, verapamil, or diltiazem, possibly supplemented by disopyramide. Therapeutic options are expanded with the myosin-ATPase inhibitor mavacamten, both in combination with basic therapy and as monotherapy in cases of intolerance or contraindication to other drugs. Gradual titration of medications to the maximum tolerated dose evaluated by echocardiographic examination is essential.
(lexi)
Sources:
1. Arbelo E., Protonotarios A., Gimeno J. R. et al. 2023 ESC Guidelines for the management of cardiomyopathies Developed by the task force on the management of cardiomyopathies of the European Society of Cardiology (ESC). Eur Heart J 2023 Oct 1; 44 (37): 3503–3626, doi: 10.1093/eurheartj/ehad194.
2. Veselka J. Therapeutic options for hypertrophic obstructive cardiomyopathy with a focus on interventional treatment. Cor et Vasa 2012; 54 (1): e39–e44, doi: 10.1016/j.crvasa.2011.12.003.3500-CZ-2400014
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Internal medicine Cardiology
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


