-
Medical journals
- Career
Effective Treatment with Nivolumab in Patients with Negative PD-L1 Expression
11. 5. 2020
In the first case, it was a 62-year-old woman, former smoker, with a history of asthma and hypertension. The tumor disease first manifested with neurological problems in December 2014, with brain MRI showing two metastatic lesions temporally on the right and one infratentorially on the right in the cerebellar hemisphere. Stereotactic radiotherapy of the brain with a Leksell Gamma Knife was performed on January 20, 2015, with doses of 20 Gy to the cerebellar metastasis, 19 Gy to the temporal metastasis on the right, and 17 Gy to the area of the cystic metastasis on the left. The primary tumor origin was investigated, and the patient was diagnosed with primary lung adenocarcinoma. January 2015 CT showed a solid pathological formation approximately 65×60×50 mm in size, centrally located in the upper right lung lobe with post-contrast enhancement, involving the bronchus for the upper lung lobe, which it obstructed. The lesion extended with a desmoplastic reaction to the surrounding parenchyma, adhering to the ventral pleura and overgrowing through the interlobium. Bronchoscopy histologically verified primary lung adenocarcinoma, T3N0M1b, with genetic testing for EGFR and ALK being negative. Following brain RT, the patient remained clinically symptom-free; follow-up brain MRI showed regression. From March 2015 to January 2016, systemic chemotherapy was administered: 4 cycles of cisplatin + pemetrexed combination, followed by maintenance monochemotherapy with pemetrexed, with regular chest X-rays and chest CT every 3 months. Due to tumor progression with new metastatic involvement in the left lung, maintenance pemetrexed therapy was discontinued in January 2016 (Fig. 1), and the patient was started on regular nivolumab therapy in February 2016. Throughout the treatment, the patient experienced no side effects, receiving 50 cycles of nivolumab until February 2018 (2 years). The first chest CT (Fig. 2) after 3 months of nivolumab treatment showed regression of tumor involvement in the right lung where the primary tumor was located, as well as a reduction in metastatic involvement of the left lung. The patient was regularly monitored (monthly X-rays and CT every 4 months), and this treatment effect lasted for the mentioned 24 months. Retrospective analysis of the bronchoscopically obtained biopsy sample for PD-L1 expression determined it to be less than 1%. Despite this “negative” expression found in a limited biopsy sample, the patient benefited from the treatment without any side effects for 2 years, with clear partial regression evident in imaging studies. The patient is now undergoing further treatment but recently experienced worsened brain metastases, with external radiotherapy under reconsideration.
Image 1. CT scans with progressing tumor infiltration on the right and metastasis in the left lung after chemotherapy before the initiation of nivolumab 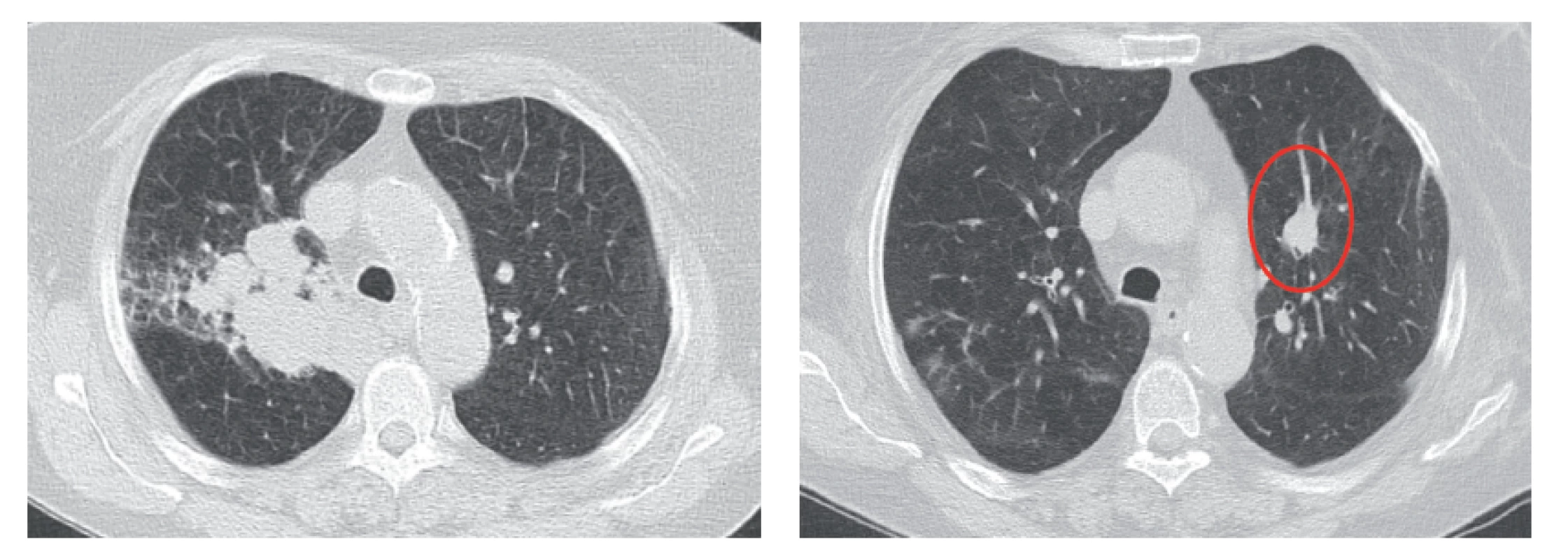
Image 2. CT scans showing regression of the original infiltration on the right, with only residual involvement in the hilum area, whereas in the upper lobe the findings have fully regressed and the metastasis on the left has reduced 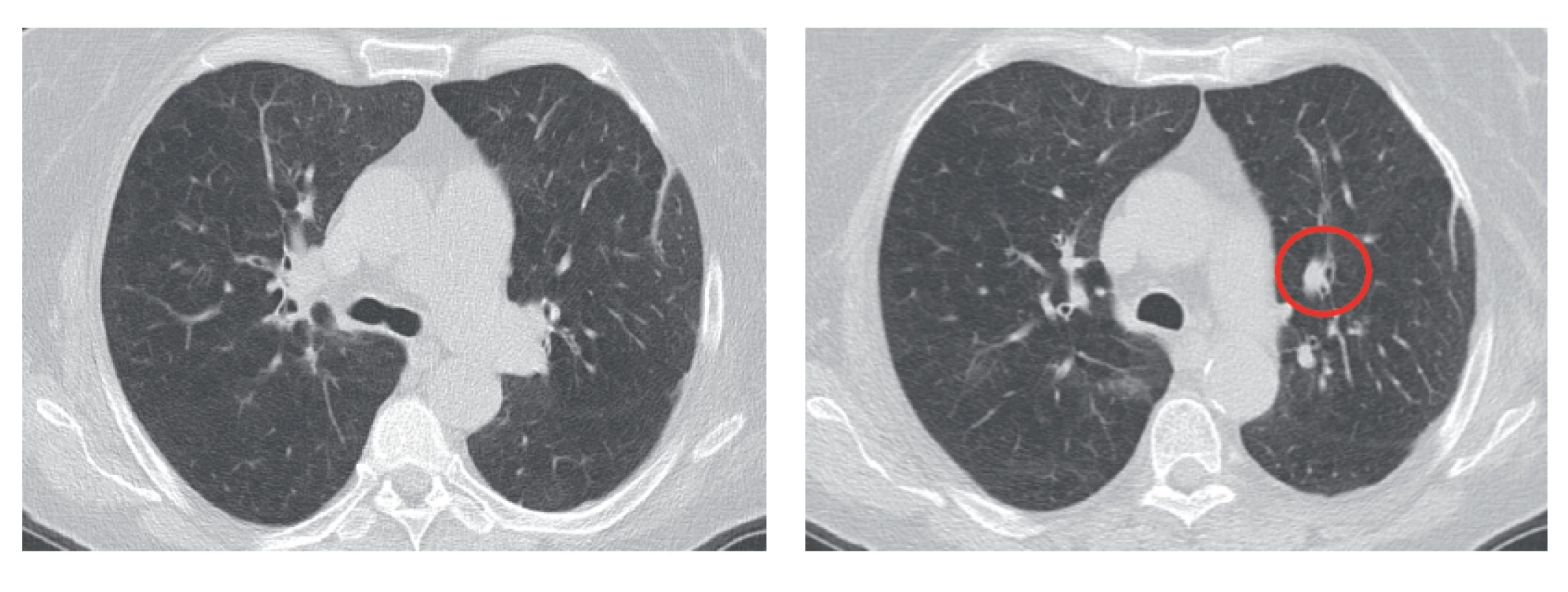
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Paediatric clinical oncology Clinical oncology
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


