Perioperative Management in Patients with Atrial Fibrillation Treated with NOACs
The recommended procedures for perioperative management in patients using novel oral anticoagulants (NOACs) stem from the requirement to minimize treatment interruption before and after surgical procedures to reduce the risk of bleeding and thromboembolism. The safety of these regimens in patients with atrial fibrillation was examined in the prospective PAUSE study presented below.
Methodology and Study Progress
A total of 3007 patients (66.1% men; average age 72.5 years) with atrial fibrillation treated long-term with NOACs who needed treatment interruption for planned surgical intervention were included in the study from August 1, 2014, to July 31, 2018. Apixaban (5 mg or 2.5 mg twice daily) was used by 1257 (41.8%) patients, dabigatran (150 mg or 110 mg twice daily) was used by 668 (22.2%), and rivaroxaban (20 mg or 15 mg once daily) was used by 1082 (36.0%) patients. Exclusion criteria included:
- Creatinine clearance (CrCl) < 0.42 ml/s for patients using apixaban and < 0.50 ml/s for those treated with dabigatran or rivaroxaban;
- Cognitive impairment or psychiatric illness;
- > 1 planned surgical procedure in the next 30 days;
- Previous participation in the study.
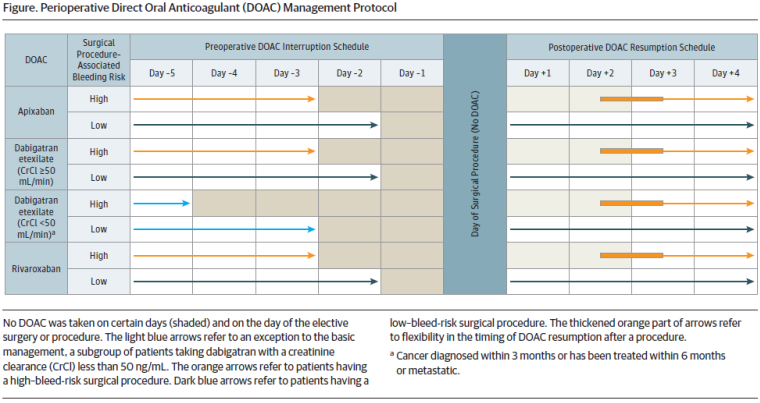
Based on recommended procedures, the timing for stopping and restarting NOACs was tailored according to low or high risk of perioperative bleeding and CrCl. A high risk of bleeding was identified in 1007 patients (at least one-third in each group). For low bleeding risk, NOACs were stopped 1 day before the procedure, and for high-risk, 2 days before (for patients using dabigatran with CrCl < 0.83 ml/s for high-risk procedures, even earlier), without heparin bridging. Blood samples were taken from patients just before the procedure to determine NOAC levels (xaban levels by anti-Xa activity and dabigatran by thrombin time).
For low-risk bleeding procedures, NOACs were resumed 1 day after, and for high-risk bleeding procedures, 2 to 3 days after. Patients at high risk of thromboembolism could receive a prophylactic dose of heparin post-operation.
Patients were monitored for 30 days from NOAC interruption. Primary parameters tracked included the proportion of patients with significant bleeding, thromboembolism (ischemic stroke, transient ischemic attack, or systemic embolism), and undetectable or minimal residual NOAC levels (< 50 ng/ml) during the procedure.
Results
Within 30 days of NOAC interruption before surgery, bleeding was observed in 1.35% of patients (95% confidence interval [CI] 0–2.00%) using apixaban, 0.90% (95% CI 0–1.73%) treated with dabigatran, and 1.85% (95% CI 0–2.65%) in the rivaroxaban group. Bleeding occurred on average 2 days after.
In the subgroups undergoing high-risk perioperative bleeding procedures, bleeding was reported in 2.96% (95% CI 0–4.68%) patients on apixaban, 0.88% (95% CI 0–2.62%) on dabigatran, and 2.95% (95% CI 0–4.76%) in the rivaroxaban group.
Arterial thromboembolism was diagnosed in 0.16% (95% CI 0–0.48%) patients on apixaban, 0.60% (95% CI 0–1.33%) on dabigatran, and 0.37% (95% CI 0–0.82%) on rivaroxaban. Thromboembolism also developed on average 2 days later.
NOAC levels before the surgical procedure were measured in 2541 patients (84.5%). High proportions of patients with undetectable or minimal residual drug levels were observed in all 3 groups: 90.5% in the apixaban group, 95.1% on dabigatran, and 96.8% on rivaroxaban.
Conclusion
The standard strategy of interrupting NOACs before planned surgical procedures without heparin bridging was associated with low rates of significant bleeding and arterial thromboembolism in atrial fibrillation patients. In high bleeding risk patients, a slightly higher bleeding rate was observed in the apixaban and rivaroxaban groups.
(mafi)
Source: Douketis J. D., Spyropoulos A. C., Duncan J. et al. Perioperative management of patients with atrial fibrillation receiving direct oral anticoagulant. JAMA Intern Med 2019; 179 (11): 1469–1478, doi: 10.1001/jamainternmed.2019.2431.
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
