-
Medical journals
- Career
Quality of life after bowel resection for Crohn´s disease – first results
Authors: L. Kunovsky 1; Z. Kala 1; L. Mitas 1; Jiří Dolina 2; V. Can 1; L. Kucerova 2; V. Jadczakova 3; I. Penka 1
Authors‘ workplace: Department of Surgery, University Hospital Brno Bohunice, Faculty of Medicine, Masaryk University Head of Department: prof. Z. Kala, M. D., Ph. D. 1; Department of Gastroenterology, University Hospital Brno Bohunice, Faculty of Medicine, Masaryk University Head of Department: prof. A. Hep, M. D., Ph. D. 2; Department of Applied Statistics and Demography, Faculty of International Development and International Studies Mendel University in Brno Head of Department: assoc. prof. Ing. K. Somerlikova, Ph. D. 3
Published in: Rozhl. Chir., 2016, roč. 95, č. 12, s. 444-448.
Category: Original articles
Overview
Introduction:
Crohn´s disease (CD) highly affects a patient´s quality of life. The aim of the study was to find out the impact of surgery on the quality of life (QoL) in CD patients and factors affecting their postoperative QoL.Methods:
90 patients with CD who underwent surgery (bowel resection) filled out an EORTC QLQ-CR29 questionnaire preoperatively and again after the surgical procedure.Results:
77% of the patients experienced a positive change (p<0.001), 22% negative and 11% no change.Conclusion:
In this cohort, we proved that surgical treatment improves the overall QoL in patients with CD. To determine factors which affect postoperative QoL, more patients need to be enrolled in future studies.Key words:
Crohn´s disease – quality of life – surgery – bowel resection – Czech cohortIntroduction
Being a chronic disorder, Crohn´s disease (CD) highly affects the quality of life (QoL) of patients suffering from this disease and is characterized by periods of remission and disease relapses.
Some of the symptoms that may alter QoL include abdominal pain, frequent stool, bowel obstruction, weight loss, malnutrition and extraintestinal manifestations.
Population-based studies showed that patients with inflammatory bowel disease (IBD) have significant impairment of QoL compared to the general healthy population [1,2]. Studies proved that QoL in IBD individuals responds to disease activity and it seems that remission has the strongest impact that contributes to the improvement of their QoL [2–4].
Manifestation of CD occurs most often at a younger age [5–7]. The incidence shows a current increase [8–11], the highest number of patients being in North America, Australia and Western Europe [8–13].
Despite all the possibilities of conservative therapy, approximately 80% of patients with CD have to undergo a surgical procedure during their lives [14–18]. The aim of the study was to compare the QoL before and after surgical treatment of CD in a Czech cohort.
Methods
During the years 2010–2014, patients with CD consecutively filled out a questionnaire preoperatively and again after a surgical procedure (bowel resection) related to CD.
The patients with perianal CD that were indicated for surgery due to perianal disease were excluded from the study (abscess, fistula, etc.). Patients that were indicated for intestinal resection filled out the questionnaire in the 6 week period prior to the operation. The same questionnaire was filled out 2 months after the surgical procedure. The period of 2 months after the operation was set as a sufficient time for healing and reconvalescence, and conversely a short time for CD recurrent activity after surgery.
Questionnaire
A routinely used questionnaire for assessing QoL in IBD patients is IBDQ-32 [19]. For a better evaluation of QoL related to surgery, we decided to use QLQ-CR 29, a module for colorectal disorders, which can better reflect the postoperative outcome.
The European Organisation for Research and Treatment of Cancer (EORTC) has a working group on QoL and has created a combined system for QoL assessment using a generic core (EORTC QLQ-C30) [20] and a supplementary module for a specific disease. QoL was evaluated using validated questionnaire module QLQ-CR 29 developed by EORTC [21,22]. Purely oncologically focused questions were excluded and the questionnaire was modified and validated in cooperation with a statistician. The content validity of the questionnaire was discussed with gastroenterologists who specialize in CD at the University Hospital Brno and a psychometrician.
The questionnaire included questions about abdominal pain and discomfort, urinary and sexual functions, stool, quality of defecation, physical functioning and body image. Questions about stool were focused on frequency, admixture of blood or mucus in the stool. In the quality of defecation, parameters such as flatulence, faecal incontinence and perianal skin discomfort were measured.
Patients rated all items of the EORTC QLQ-CR29 questionnaire on a 7-point scale which was linearly transformed to give a score ranging from 0 to 100 according to the formula suggested by developers. In doing so, a high score indicated a high (“worse”) level of symptomology (or problems), and thus a lower level of quality of life, and vice versa. The score for overall QoL was calculated as a summated scale by averaging items compromising it.
Statistics
A total of 90 patients was subjected to the analysis. Due to the ordinal nature of the data and non-Gaussian distributions, the level and variation of quality of life components was presented as median and interquartile range and nonparametric analysis was used to examine the effects in the sample. Specifically, Wilcoxon signed-rank test was performed to assess the difference between preoperative and postoperative components of the quality of life. The Mann-Whitney U test or Kruskal-Wallis one-way ANOVA for k samples was used to assess the association between the overall QoL and selected demographic and clinical characteristics. To treat the effect of multiple comparisons, the Bonferroni correction or multivariate canonical analysis was applied. In doing so, if not specified otherwise, the p <0.05 was considered statistically significant for all analyses.
Results
We recruited 90 patients with CD who underwent intestinal resection. Basic characteristics of the patients can be seen in Tab. 1. In our group, we had 51 females and 39 males, the mean age at the time of the surgical procedure was 33.5±10.7 years. 49 patients (54.4%) were smokers and 33 patients (36.7%) had at least one previous abdominal surgical procedure.
1. Basic characteristics of patients 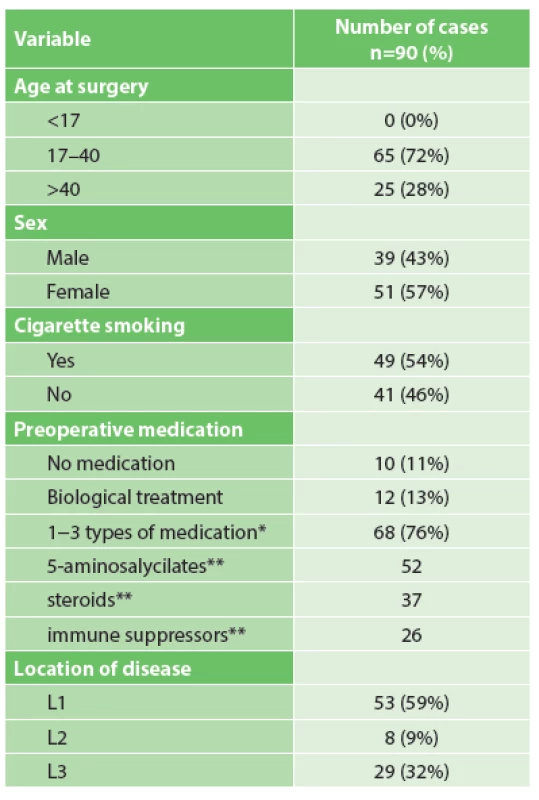
* 5-aminosalycilates, steroids, immune suppressors or combination ** counted independently In 25 cases, the laparoscopic approach (27.8%) was chosen, in 65 cases the surgery was done by open approach (72.2%). The spectrum of all surgical procedures is mentioned in Tab. 2. The most frequent procedure was ileocecal resection in 61 patients (67.8%). The 30-day postoperative complications were also recorded. The most frequent complications were surgical site infections or wound hematoma in 17 patients (18.9%). Severe complications such as anastomotic leakage were reported in 3 patients (3.3%), bowel obstruction in 3 patients (3.3%), intraabdominal abscess in 5 patients (5.6%) and postoperative bleeding in 2 patients (2.2%). Other complications can be seen in Tab. 3. The assessment of the surgical approach and complications as postoperative QoL predictors are listed in Tab. 4.
2. Summary of surgical procedures 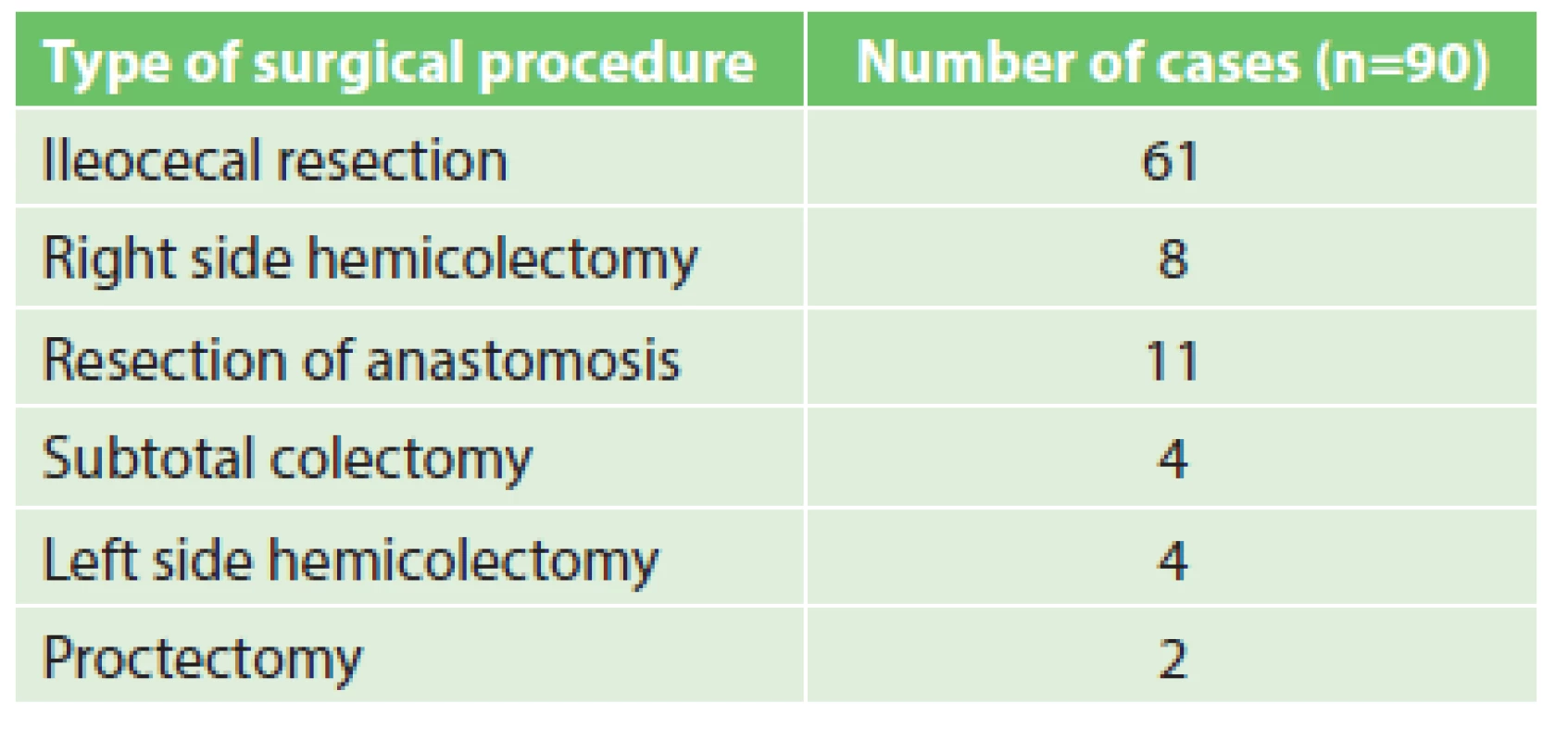
3. Summary of complications within 30 days 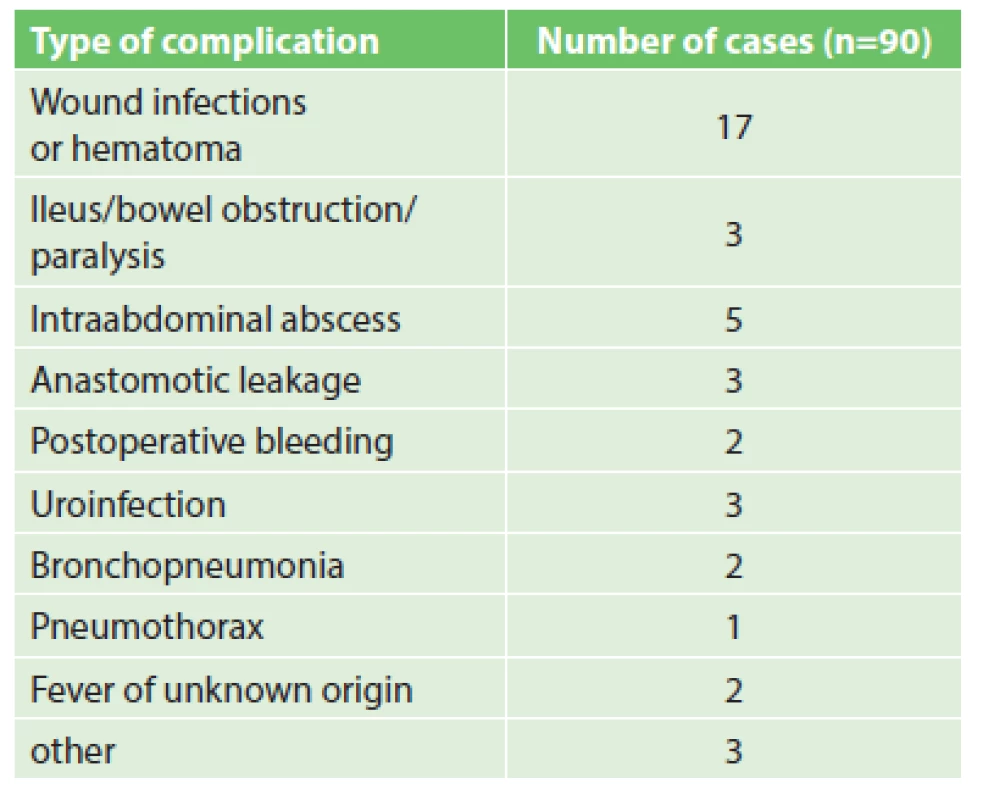
4. Analysis of factors affecting overall postoperative QoL 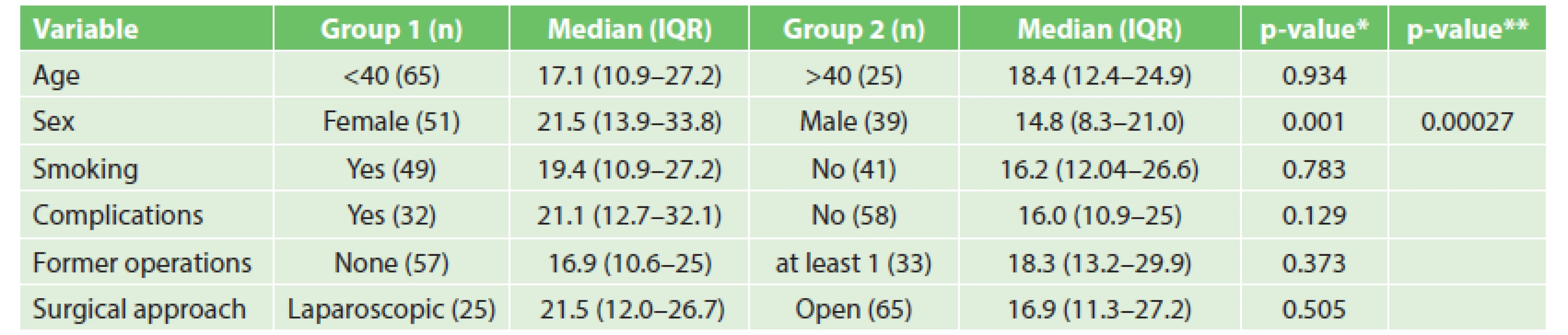
*Mann-Whitney U test (significant p-value <0.05) ** Canonical analysis (significant p-value <0.05) IQR: Inter-quartile-range; QoL: Quality of life At the time of surgery, most of the patients were on 5-aminosalicylates, steroids, immune suppressors or any combination of these medications. 12 patients were treated by biological therapy and 10 were not using any pharmacotherapy for CD. The location of the disease was classified by the Montreal classification [23] (L1 in 53 patients, L2 in 8 and L3 in 29). The evaluation of pharmacotherapy and location of the disease as postoperative QoL predictors are mentioned in Tab. 5.
5. Analysis of factors affecting overall postoperative QoL 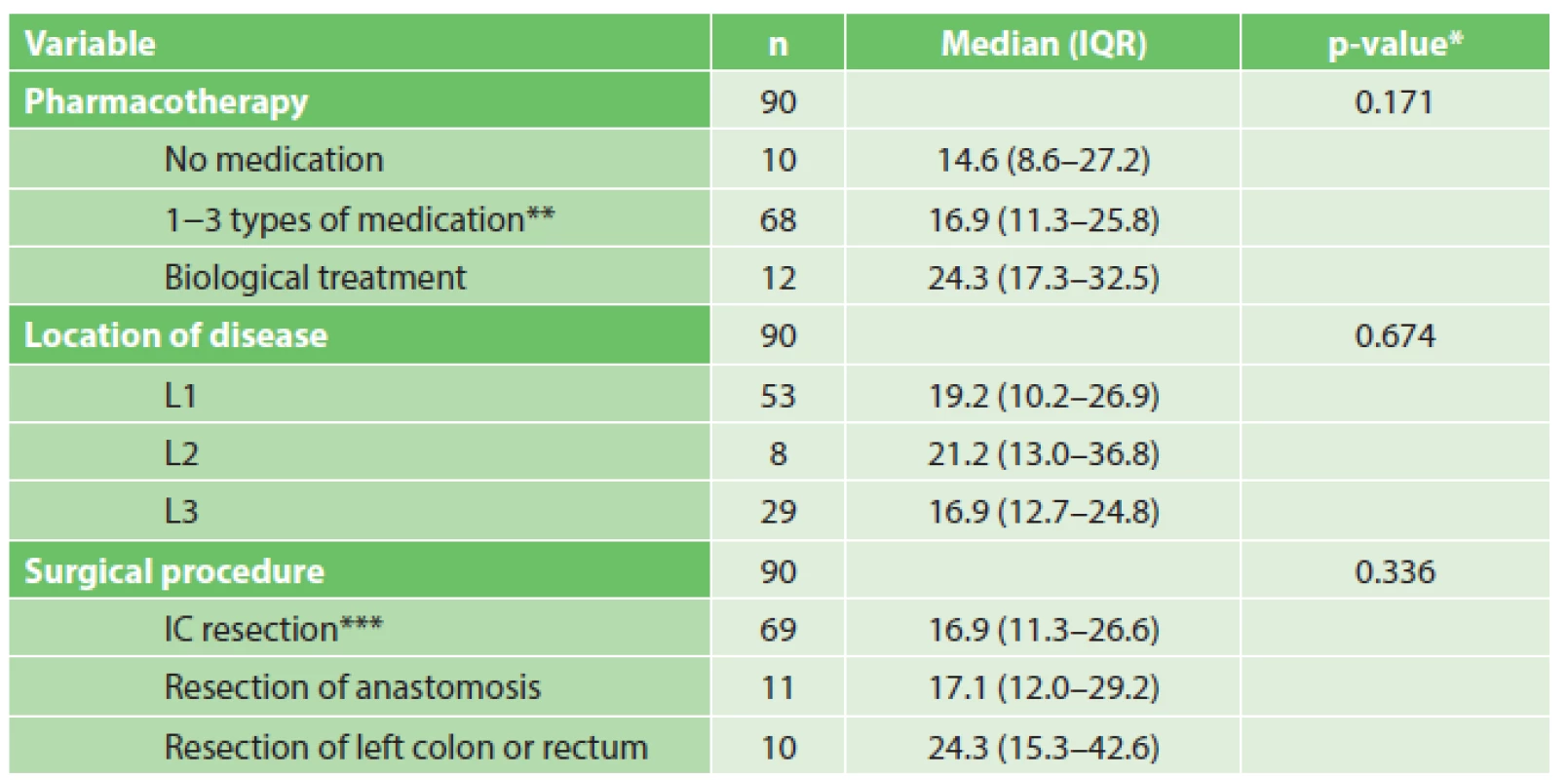
*Kruskal-Wallis one-way ANOVA for k samples (significant p-value <0.017, Bonferroni p-value threshold) ** 5-aminosalycilates, steroids, immune suppressors or combination *** Right side hemicolectomy was evaluated together with IC resection In our first results, we proved that the short-term QoL measured 2 months after surgery improved. The postoperative overall QoL improved statistically significantly (77% patients experienced a positive change, 22% negative and 11% no change), further improvement of QoL comprised a reduction of abdominal pain and discomfort, reduced frequency of stool, etc. Except for urinary functions, where there was no impact of surgery on QoL, all variables were evaluated with a significant postoperative improvement of QoL. All data are summarized in Tab. 6.
6. Preoperative and postoperative changes of QoL in patients after bowel resection for Crohn´s disease 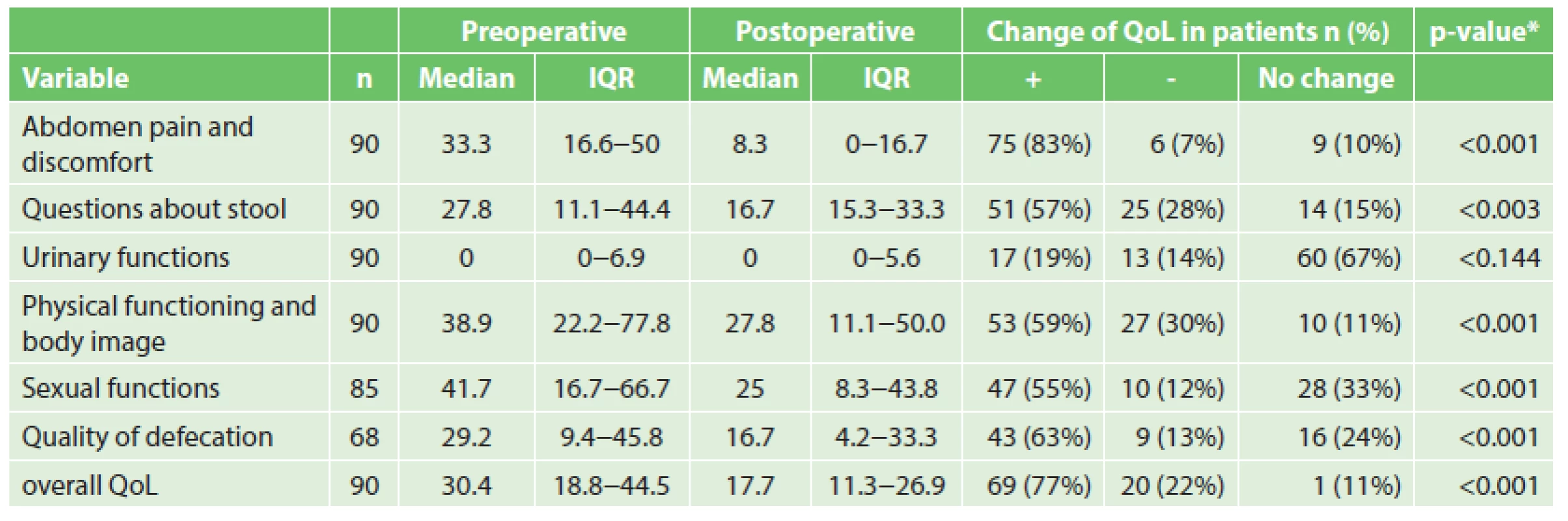
* Wilcoxon signed-rank test (significant p-value <0.008, Bonferroni p-value threshold) IQR: Inter-quartile-range; QoL: Quality of life Discussion
Even though there is a possibility of biological treatment, the majority of patients with CD still has to undergo a surgical procedure during their lifetime. In our group of patients, we proved that surgical treatment improves the QoL in the short-term period after surgery. Except for urinary functions, the QoL was assessed as significantly better postoperatively in all the observed parameters. In 2003, Delaney et al. [24], also published evidence of improvement of QoL measured 30 days after surgery for CD. However, the duration of this level of quality of life is still uncertain, as the clinical recurrence after surgery is about 55−65% in 5 years [14,17,25].
In our analysis, male gender was evaluated as a statistically significant factor of postoperative improvement of QoL (p=0.00027). Tabibian et al. [26] published an article in 2015 about predictors of impaired QoL in patients with inflammatory bowel disease. In his work, female gender was described as a statistically significant predictor of lower QoL among CD patients. Casellas et al. [4] obtained similar results where bowel symptoms were perceived as worse by women patients suffering from CD, although in other domains gender was not crucial for QoL.
Some variables from our analysis indicated predictive value of postoperative QoL, but they did not reach statistically significant values (e.g. complications, pharmacotherapy). Complications within 30 days after surgery are associated with impaired QoL as published by Delaney et al. [24]. In our study, patients with postoperative complications also had reduced QoL, but the results were not statistically significant (p=0.129). Concerning the impact of pharmacotherapy on postoperative QoL, it was most enhanced in patients without medication. Patients on biological treatment had the lowest QoL. However, the factor of pharmacotherapy was not at a statistically significant level (p=0.171).
Other factors in the analysis were not statistically significant or could be misleading due to the total number of patients (e.g. surgery approach, surgical procedure). In previous studies, when laparoscopic approach was compared to open surgery, it was associated with a shortened hospital stay and better effects on body image and cosmetic results, although the overall improvement in QoL was not observed [27]. In our analysis, the laparoscopic approach also did not enhance overall postoperative QoL (p=0.505).
In this article, we publish our first results of the study analysing QoL after bowel resection in patients with CD. For more significant results of factors affecting postoperative QoL, more patients should be enrolled. A control group of a healthy cohort could also be established to reveal the differences in QoL (as presented in table 6) between a healthy cohort and patients with CD after surgery. Another control group of patients with CD who do not need surgery yet could be used for comparison as well.
Conclusion
In this cohort, we proved that surgical treatment (bowel resection) improves the overall QoL in patients with CD. However, to determine factors which affect postoperative QoL, more patients need to be enrolled in future studies.
Abbreviations:
CD - Crohn´s disease
QoL - quality of life
IBD - inflammatory bowel disease
IBDQ-32 - Inflammatory bowel disease questionnaire-32
EORTC - The European Organisation for Research and Treatment of Cancer
QLQ-CR 29 - Quality of life questionnaire-colorectal 29
Conflict of Interests
The authors declare that they have not conflict of interest in connection with the emergence of and that the article was not published in any other journal.
Lumir Kunovsky, M.D.
Department of Surgery, University Hospital Brno Bohunice,
Faculty of Medicine, Masaryk University
Jihlavska 20
625 00 Brno
e-mail: kunovsky.lumir@fnbrno.cz
Sources
1. Mikocka-Walus AA, Turnbull DA, Andrews JM, et al. Psychological problems in gastroenterology outpatients: A South Australian experience. Psychological co-morbidity in IBD, IBS and hepatitis C. Clin Pract Epidemiol Ment Health 2008;4 : 15.
2. Gavrilescu O, Mihai C, Anton-Paduraru DT, et al. Impact of inflammatory bowel diseases on quality of life. Revista de Cercetare si Interventie Sociala 2015;50 : 80–95.
3. Lix L, Graff L, Walker J, et al. Longitudinal study of quality of life and psychological functioning for active, fluctuating, and inactive disease patterns in inflammatory bowel disease. Inflamm Bowel Dis 2008;14 : 1575–84.
4. Casellas F, López-Vivancos J, Badia X, et al. Impact of surgery for Crohn’s disease on health-related quality of life. Am J Gastroenterol 2000;95 : 177–82.
5. Julsgaard M, Nørgaard M, Hvas CL, et al. Influence of medical treatment, smoking and disease activity on pregnancy outcomes in Crohn’s disease. Scand J Gastroenterol 2014;49 : 302–8.
6. Pedersen N, Munkholm P, Bortoli A, et al. The course of inflammatory bowel disease during pregnancy and postpartum: A prospective European ECCO-EpiCom Study of 209 pregnant women. Aliment Pharmacol Ther 2013;38 : 501–12.
7. Nørgård B, Hundborg H, Jacobsen B, et al. Disease activity in pregnant women with crohn’s disease and birth outcomes: A regional Danish cohort study. Am J Gastroenterol 2007;102 : 1947–54.
8. Nørgård BM, Nielsen J, Fonager K, et al. The incidence of ulcerative colitis (1995–2011) and Crohn’s disease (1995−2012) − Based on nationwide Danish registry data. J Crohns Colitis 2014;8 : 1274–80.
9. Wilson J, Bell S, Kamm M, et al. High incidence of inflammatory bowel disease in Australia: A prospective population-based Australian incidence study. Inflamm Bowel Dis 2010;16 : 1550–6.
10. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142 : 46–54.e42.
11. Kunovsky L, Hemmelova B, Kala Z, et al. Crohn disease and pregnancy: a case report of an acute abdomen. Int J Colorectal Dis 2016;31 : 1493–4.
12. Vegh Z, Burisch J, Pedersen N, et al. Incidence and initial disease course of inflammatory bowel diseases in 2011 in Europe and Australia: Results of the 2011 ECCO-EpiCom inception cohort. J Crohns Colitis 2014;8 : 1506–15.
13. Lowe A-M, Roy P-O, Poulin M-B, et al. Epidemiology of Crohn's disease in QuéBec, Canada. Inflamm Bowel Dis 2009;15 : 429–35.
14. Aratari A, Papi C, Leandro G, et al. Early versus late surgery for ileo-caecal Crohn’s disease. Aliment Pharmacol Ther 2007;26 : 1303–12.
15. De Cruz P, Kamm MA, Hamilton AL, et al. Crohn’s disease management after intestinal resection: a randomised trial. The Lancet 2015;385 : 1406–17.
16. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg 2000;231 : 38–45.
17. Bobanga I, Bai S, Swanson M, et al. Factors influencing disease recurrence after ileocolic resection in adult and pediatric onset Crohn’s disease. Am J Surg 2014;208 : 591–6.
18. Fornaro R, Caratto E, Caratto M, et al. Post-operative recurrence in Crohn’s disease. Critical analysis of potential risk factors. An update. The Surgeon 2015;13 : 330–47.
19. Guyatt G, Mitchell A, Irvine EJ, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 1989;96 : 804–10.
20. Aaronson N, Ahinedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85 : 365–76.
21. Whistance RN, Conroy T, Chie W, et al. Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer 2009;45 : 3017–26.
22. Gujral S, Conroy T, Fleissner C, et al. Assessing quality of life in patients with colorectal cancer: An update of the EORTC quality of life questionnaire. Eur J Cancer 2007;43 : 1564–73.
23. Satsangi J, Silverberg MS, Vermeire S, et al. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 2006;55 : 749–53.
24. Delaney CP, Kiran RP, Senagore AJ, et al. Quality of life improves within 30 days of surgery for Crohn’s disease. J Am Coll Surg 2003;196 : 714–21.
25. Achkar JP, Hanauer SB. Medical therapy to reduce postoperative Crohn’s disease recurrence. Am J Gastroenterol 2000;95 : 1139–46.
26. Tabibian A, Tabibian JH, Beckman LJ, et al. Predictors of health-related quality of life and adherence in Crohn’s disease and ulcerative colitis: implications for clinical management. Dig Dis Sci 2015;60 : 1366–74.
27. Scarpa M, Ruffolo C, Bassi D, et al. Intestinal surgery for Crohn’s disease: Predictors of recovery, quality of life, and costs. J Gastrointest Surg 2009;13 : 2128−35.
Labels
Surgery Orthopaedics Trauma surgery
Article was published inPerspectives in Surgery

2016 Issue 12-
All articles in this issue
- 10 years of sleeve gastrectomy in the Czech Republic in terms of the surgical procedure
- Tumor cells transfer between the patient and laboratory animal as a basic methodological approach to the study of cancerogenesis and identification of biomarkers
- Proximal gastrectomy for adenocarcinoma of the gastroesophageal junction in a selected set of patients − immediate and long-term results
- Purtscher-like retinopathy as a complication of acute pancreatitis
- Rare case of a giant parathyroid adenoma
- Quality of life after bowel resection for Crohn´s disease – first results
- Castleman’s disease - surgical treatment, case reports
- Perspectives in Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Rare case of a giant parathyroid adenoma
- 10 years of sleeve gastrectomy in the Czech Republic in terms of the surgical procedure
- Purtscher-like retinopathy as a complication of acute pancreatitis
- Proximal gastrectomy for adenocarcinoma of the gastroesophageal junction in a selected set of patients − immediate and long-term results
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

