-
Medical journals
- Career
The effectiveness of hyperbaric oxygen therapy comparing to pharmacological treatment in the patients with complex regional pain syndrome: a systematic review protocol
Authors: D. Tučková 1,3; M. Klugar 1,2,4; M. Hájek 5,6; J. Klugarová 1,2; D. Chmelař 6,7
Authors‘ workplace: The Czech Republic (Middle European) Centre for Evidence-Based Healthcare: The Joanna Briggs Institute Centre of Excellence, Czech National Centre for Evidence-Based Healthcare and Knowledge Translation, Institute of Biostatistics and Analyses, Faculty of 1; Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, Brno, Director doc. RNDr. Ladislav Dušek, Ph. D. 2; Department of Public Health, Faculty of Medicine and Dentistry, Palacký University Olomouc, Head doc. MUDr. Helena Kollárová, Ph. D. 3; Centre for Evidence-Based Healthcare, Library, Faculty of Medicine and Dentistry, Palacký University Olomouc, Director PhDr. Miloslav Klugar, Ph. D. 4; Centre for hyperbaric medicine, City hospital in Ostrava, Head MUDr. Michal Hájek, Ph. D. 5; Department of Biomedical Sciences, Institute of Microbiology and Immunology, Medical Faculty, Ostrava, Head doc. RNDr. Kristian Šafarčík, Ph. D. 6; Czech Anaerobic Bacteria Reference Laboratory, Medical Faculty, University of Ostrava, Head doc. RNDr. Dittmar Chmelař, Ph. D. 7
Published in: Pracov. Lék., 70, 2018, No. 3-4, s. 146-153.
Category:
Overview
The protocol of the systematic review is focused on the effectiveness of hyperbaric oxygen therapy comparing to pharmacological treatment in the patients with complex regional pain syndrome type I. and type II. in the inflammatory and dystrophy phase of the disease. The review question was developed using the PICO acronyme where P stands for patients suffer from the CRPS, I stands for hyperbaric oxygen therapy for 30 to 120 minutes at the 1,5 ATA to 3 ATA. This will be compared with standard/convention care regimens (C) including rehabilitation therapy, psychotherapy, topical pharmacotherapy, blocking of sympathetic nervous system and medications. O as an outcome will consider a level of pain (mild, moderate, severe – according to the Numeric Rating Scale (NRS), visual analogue scale (VAS) or Likert scale), function limitation, extension of ability to move measured by standardized scale, osteoporosis remission measured with X-ray or CT scan, ligament, muscle and bone dystrophy using standardized screening techniques before and after HBO. The search strategy used in this systematic review will include three steps according to Joanna Briggs Institute (JBI) methodology. Initial search will be done in MedLine, Cinahl, and Embase database. Studies, which will be found, will be assessed by two independent reviewers. Standardized critical appraisal tools of JBI will be used.
Keywords:
hyperbaric oxygen therapy – complex regional pain syndrome – effectiveness – systematic review
REVIEW QUESTION/OBJECTIVE
The objectives of this review are to identify the effectiveness of hyperbaric oxygen therapy (HBO) comparing to pharmacological treatment on level of pain, function limitation, extension of ability to move, osteoporosis remission, ligament, muscle and bone dystrophy in patient with the complex regional pain syndrome (CRPS) type I. and type II. in the inflammatory and dystrophy phase of the disease.
BACKGROUND
Complex regional pain syndrome (hereinafter CRPS) is a chronic pain condition characterized by spontaneous and evoked regional pain, usually beginning in a distal extremity, that is disproportionate in a magnitude or duration to the typical course of pain after similar tissue trauma [1]. It remains a poorly understood chronic pain condition with regards to pathophysiology and treatment [2–4]. The CRPS was first described in the 17th century and various names have been used since then to describe name this disease: causalgia, algodystrophy, reflex symphatetic dystrophy, shoulder-hand syndrome, and/or Sudeck syndrome [5]. Although the CRPS is known for more than one century, the pathogenesis has not been definitely clarified.
The CRPS develops as a localized pain disorder within 4–6 weeks following trauma when there are present clinical symptoms that can no longer be explained by the initial trauma [6]. According to the official International Association for the Study of Pain (hereinafter IASP), the symptoms of the CRPS affect the distal externity, go beyond the trauma territory and beyond nerve/nerve root innervation territories. Other diseases are vigorously excluded [6].
It can be distinguished two types of the CRPS – type I. (known as reflex sympathetic dystrophy) and type II. (known as causalgia) [1–3, 5, 7, 8]. The CRPS type I. is characterized by spontaneous pain, allodynia and hyperalgesia [4] and it is the most common [9]. It occurs after an effect causing a damaging causes or without any obvious cause [10–12], usually after an illness or injury that has not directly damaged a nerve in the affected area [13]. It can be defined as an articular and periarticular pain syndrome with vasomotor deregulation triggered by various stresses with no relationship between the identity of the initial injury and severity of the continuing pain [5]. The CRPS type II. includes all of foregoing features and occurs after a peripheral nerve lesion either isolated or in connection with an injury of the tissues around [3, 6]. The spontaneous pain and an allodynia or hyperalgesia that does not have to be bordered on the area of damaged/affected nerve is present [14]. Except of the presence or absence the nerve injury, different clinical findings of the CRPS can be distinguished with the skin temperature, when approximately 70% patients with CRPS have “warm” affected limbs and 30% have “cold” affected limbs [150]. Although the CRPS can be subclassified into these two diagnostic subtypes, the distinction is not always easily made [16].
There are three stages in the development of the CRPS:
- acute (stage I),
- dystrophic (stage II), and
- atrophic (stage III).
In the acute (or “inflammatory”) stage, due to decreased activity of symphaticus is the temperature of the limb increased compared to original state after the trauma. Other features are: hyperaemia, oedema, glossy, reddish and tighten skin, accelerated growth of nails and hair, burning deep pain during rest (especially during the night), movement disorder, respectively functional failure (especially because of the pain). It can be recognized a difference in a perspiration (it is increased on the affected limb). The symptoms occur after 1–12 weeks (the first three months) after the trauma. The time of treatment of this stage is usually considered for 3 months [17]. The dystrophic stage is proposed to occur 3–6 months after onset, and it is characterized by more marked pain/sensory dysfunction, continued evidence of vasomotor/trophic changes [18]. A healing is usually incomplete. The symptoms are an oedema regression, spontaneous pain regression (but pain still persists in a movement or in a load), pale and glossy, cold skin, decrease temperature of a limb on the affected side, soft tissue atrophy, limitation of movement of affected limb area, slowing of the hair and nails growth, beginning of a joint stiffness [17, 19]. The atrophic stage is irreversible and is characterized by stiffness and flexion contractures of the limb. The injury progresses into the III. stage around the sixth month after the trauma [5]. The patient complains of vasomotor pain and the trophic changes in the skin, muscles and skeleton are permanent and progressively worsen until there is ankyloses and complete loss of function [20].
The incidence of the CRSP states that 45–65% is early or late trauma complication (including the fractures), 20% occurs as a complication after a surgery intervention, 12–20% is noticed in the patients with hemiphlegia, 10% of cases has unclear onset [11, 12]. In the general population, the CRPS seems to occur most often after the fractures (> 40 % of CRPS cases in two population based studies [1]). De Mos, Bruijn et al. (2006) in their population-based study stated that the CRSP occurs the most in patient after a fracture (in 44.1 %, especially fracture of calcaneus, talus, wrist bone (especially os scaphoideum), and lower and upper ends of the tibia), after a sprain (in 17.6 %), and after an elective surgery (in 12.2 %, e.g. 2–4% after Carpal tunnel surgery [5, 21].
The overall incidence of the CRPS is difficult to evaluate. It is estimated that the incidence is between 5 and 25 per 100,000 people/year, with the frequency being higher with age [5]. Women are more frequently affected than men with the ration of 4 : 1 and average age in the CRPS patient is 46.5 for males and 47.7 for females [22]. The CRPS affects more commonly the upper limbs and peaks of incidence is at 50–70 years of age [21]. In a study conducted in 1990 in the USA, incidence rates of the CRPS type I and II were reported as 5.46 per 100,000 persons a year. In the retrospective study (1996–2005) in population in the Netherlands, there was reported incidence of 26.2 cases per 100,000 person a year [1]. In Sweden in 1990, 67 cases of the CRSP were reposted while in 1993 it was 2,458 cases [3]. Thus the trend of the CRPS occurrence is increasing [1, 3, 21, 22].
The CRPS is more likely to respond to comprehensive, integrated multidisciplinary treatment that includes medical, psychological, and physical and occupational therapy components [1].
Medical therapy includes administration of:
- Anti-inflammatory drugs and immunomodulators/immunoglobulins, including non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids (especially in acute stage), cyclooxygenase-2 (Cox-2) inhibitors, free radical scavengers (e.g. vitamin C) and biologics (e.g. tumour necrosis factor-α (TNF - α inhibitors) [23] and glucocorticoids [6] successfully administered in initial dose of 100 mg prednisolone per day with a 25 %; reduction of every 4 days; an improvement for the patients with the CRPS has been reported by Tran, Duong et al. (2010) [24];
- Anticonvulsants, neuromodulators – pain medication (e.g. carbamazepine, gabapentin or neurontin® [5]); a clear benefit has not been reported with gabapentin by Tran, Duong et al. (2010) [24]; van de Vusse, Stomp-van den Berg et al. (2004) stated a mild effect of gabapentin in the patient with CRPS I. [25];
- Antidepressants and anxiolytics (e.g. amitriptyline, doxepin) effects have not been proven by any conducted RCT focused specifically on the patients with the CRPS [1];
- Opioids have showed that extended-release morphine did not significantly reduce pain beyond eight days although the findings may have been affected by the maximum titrated dose of morphine allowed [5] but no controlled studies of opioid use in the CRPS exist [3].
- N-methyl-aspartate (NMDA) antagonists (e.g. ketamine, dextromethorphan); Various ketamine dosage schemes have been tested, from transcutaneous application to a ketamine-induced coma and although the lowest doses seems to provide the best results, the lack of regulatory approval in this indication and various side effects limit the use of ketamine in current practice [5];
- Antihypertensives and α-adrenergic antagocists (e.g. clonidine, phentolamine).
- Bisphosphonates (e.g. alendronate) inhibit the activity of osteoclasts and show uniformly positive effects. Whether bisphosphonates are preferable in acute or chronic CRPS remains unclear [6];
- Calcitonin was formerly used for its inhibit effect in the second and third stage of the CRPS. But it quit to be used because of a suspicion of an increased occurrence of the oncological diseases [26].
Not all the patients need pharmacological therapy. Therefore, it can be used other non-pharmacological options how to manage the CRPS.
Topical pharmacotherapy includes drug treatments and creams, e.g. lidocaine patches and mixed local anaesthetic creams, capsaicin and dimethyl sulfoxide [23] (DMSO 50% in a grease-based cream [6]). Topical dimethyl sulfoxide seems to have a positive effect on pain and the symptoms in patients with “primarily warm” CRPS [6]. Topical capsaicin application leads to a reversible depletion of peptides including substance P and calcitonin gene-related peptide from the C-fiber nerve terminals, resulting in activation and subsequent reversal of C-fiber function [3].
Psychological therapies primarily aim to improve function and disability, rather than pain, by patient education [23]. Psychotherapy or psychological therapies can include cognitive-behavioural therapy (CBT), operant conditioning (OC), counselling, pain education, relaxation techniques [23]. Psychological pain management (especially using behavioural modification therapy) can significantly reduce chronic pain. Although there are not enough controlled trials on this topic, experts believe this is the most important treatment modality for CRPS patients [5]. Given the psychological complexity of the CRPS, it is generally agreed that inclusion of pain focused CBT is beneficial as a part of standard care of chronic CRPS [1, 27].
Rehabilitation therapy (occupational and physiotherapy rehabilitation) are frequently used to treat the CRPS, usually in a multi-modal way (manual therapy, electrotherapy, massage, therapeutic exercise [23], desensitization, isometric muscle work, muscular release, orthoses, and active mobilisation within the non-painful range of motion, or mirror therapy [50]. Rehabilitation approached typically include exercise regimes as well as passive techniques to improve range of movement (hereinafter ROM) and the strength and function in the joints of affected body part [23]. Rehabilitation therapy includes a progressive-loading physical exercise program based on the pain-exposure physical therapy (PEPT) and graded exposure in vivo (GEXP). However, confirmation of the effectiveness of these programs are lacking [6]. Mirror therapy has recently been successfully managing for the CRPS, both in terms joint range of motion and pain [5]. This rehabilitation method consists of stimulating the visual proprioceptive pathway by asking the subject to look at the movement performed by the healthy limb in a mirror; this gives a visual illusion of the movement being performed with the affected limb [5]. The mirror therapy is the most effective in patients with acute CRPS [6].
Blocking of sympathetic nervous system (hereinafter SNS) is an invasive treatment using administration of the injection directly into sympathetic neural structures such as the stellate ganglion or lumbar sympathetic chain (administering poisonous agents such as phenol or using surgical methods e.g. surgical excision or electrocoagulation) [23]. There was no proof of sympathetic blocks efficacy but clinical experience and some small RCT (n = 7) suggest that in some patients they may provide additional pain relief [1, 5]. However, blocking the SNS is no longer considered a first-line therapy [6].
In 2013, O’Connell, Wand et al. published an overview of systematic review within the Cochrane collaboration saying that there is a lack of high quality evidence for the effectiveness of most therapies for the CRPS. The low evidence for the efficacy of bisphosphonates, calcitonin, subanesthetic intravenous ketamine, graded motor imagery (GMI) programmes and mirror therapy (specific physical therapy interventions, with mirror therapy effective particularly in acute post-stroke CRPS), and CRPS focused on the physical and occupational therapy was found [1, 23].
Hyperbaric oxygen therapy (HBOT) can be defined as an intervention in which an individual breathes near 100% oxygen intermittently while inside a hyperbaric chamber that is pressurized to greater than sea level pressure (1 atmosphere absolute [ATA], which converts to 101.325 kilopascals [kPa]). For clinical purposes, the pressure must equal or exceed 1.4 ATA (141.86 kPA) while breathing near 100% oxygen [28]. The physiological effect of HBOT is to increase the oxygen level in plasma from 0.3 to 6 mL/dL at 3 ATA [29-31]. But the range of pressure used for HBOT can be between 1.5 ATA and 3 ATA for 30 to 120 minutes [32]. HBOT greatly increases the oxygen concentration in plasma, reducing the need for haemoglobin in blood oxygen transport and has bacteriostatic or bactericidal effects, and has positive effects on the physiology of tissue rendered ischaemic by trauma or infection [30]. Due to the effect of HBOT it has been used worldwide to treat many diseases. The increased concentration and the partial pressure of oxygen increase oxygenation of the whole body. The increased tissue oxygen enhances the growth of fibroblasts, formation of collagen, angiogenesis and the phagocytic capabilities of the hypoxic leukocytes [20, 32] and it can reduce in oedema and healing damaged tissues [29]. The hyperbaric oxygen therapy can significantly help in the treatment of patients suffering from the CRPS type I. and II. With HBOT, the hypoxia forming in the body leads to vasoconstriction, lowers oedema, and raises tissue partial oxygen pressure and it stimulates the depressed osteoblast activity and reduces the formation of fibrous tissues [31].
Krásová (1995) described 66 patients treated in 1988–1991 with the CRPS (45 of patients with disability of lower limb, 21 with disability of upper limb) in the second stage of disease (mean time of onset of symptoms 138th day). 72% of cases was caused by trauma, 79% of the limbs were fixed with plaster or a splint, all patients were suffering from the oedema and pain. All patients were treated by HBOT at 3 ATA for 90 minutes, 20 exposures in average. 8% of cases were cured, 65% were improved, 15% stayed without any change and 12% could not be evaluated from different reasons. The same cohort of patients was invited for the checking up in 1995 (which means 4–7 years after the CRPS onset). Only 36 patients have appeared, but 30 (83%) of them returned back to work or got retired without any severe health issues related to the CRPS [33].
Hájek (2017) referred 603 patients with CRPS out of total 13.608 patients treated during 1965–2004 (4.5%) in Centre of hyperbaric medicine of Ostrava. During 2000–2004 total of 33 patients were treated with HBOT. After HBOT it was finished, 64% of cases had a mild improvement, 21% had a significant improvement, 3 patients had no healing effect and 6% could not be evaluated [38]. During last decade 10–15 patients per year have been treated in the same centre, most of them in 2005 (16 patients, 10 males and 6 females) and 2015 (15 patients, 3 males, 12 females). Majority of patients have been referred from surgical and orthopaedics ambulances of all Moravia-Silesian region [38].
Kiralp, Yilidiz et al. (2016) referred in a double-blind randomized placebo controlled study, of the 71 patients in I. or II. stage of the CRPS, 37 of them were allocated to the HBO group receiving 15 90minutes therapy sessions with 2.4 ATA on 5 days of the week (1 session per day). When comparing with placebo it showed significant differences after the 15th therapy regarding to decreasing of pain and oedema and increasing of the range of motion [20].
Tuter, Danilov et al. (1996) used the HBO therapy in 20 of 35 patients with the CRPS. They observed a significant decrease of pain in all patients after the treatment sessions and the effect of HBO therapy persisted during 6 months in 87% of the patients. There was also found the tendency to normalization of evoked skin potentials [34].
Peach (1995) used the HBO therapy in a female patient suffering from acute smoke inhalation with the medical history of the CRPS who was allergic to steroid, non-steroidal anti-inflammation agents, and all narcotics. She was referred for hyperbaric oxygen therapy for 46 min at 60 feet of sea water (hereinafter fsw). Then she was offered treatment at 33 fsw for 90minutes session and the following week at 45 fws for 30 minutes. After the HBO therapy, it was significant that her pain was relieved after initiation of the therapy [35].
The HBO therapy is not standardized in the CRPS management but it is promising solution in both acute and chronic treatment of the disease. Because of symptoms that limit the patients in everyday life the early diagnostics and active treatment approach directly after an onset of the CRPS are crucial factors improving patient’s prognosis.
A preliminary search performed in February 2017 of the Cochrane Database of Systematic Reviews, JBI Database of Systematic Reviews and Implementation Reports, PROSPERO, EMBASE and MEDLINE located no systematic reviews that have evaluated the effectiveness of HBO therapy in patients with CRPS.
INCLUSION CRITERIA
Types of participants
This review will consider studies that include patients (both genders) suffering from the complex regional pain syndrome (CRPS) type I. and type II. in the inflammatory and dystrophy phase of the disease.
Types of intervention(s)/phenomena of interest
This review will consider studies that evaluate the effect of hyperbaric oxygen therapy for 30 to 120 minutes at the 1.5 ATA to 3 ATA.
The effect of hyperbaric oxygen therapy will be compared with normobaric (normal) oxygen and/or with standard/convention care regimens, including: rehabilitation therapy (exercise of the painful limb or body part, including transcutaneous electrical nerve stimulation (TENS), massage, therapeutic exercise), psychotherapy (including cognitive-behavioural therapy (CBT) mirror therapy, operant conditioning (CO) counselling pain education and relaxation techniques [1], topical pharmacotherapy (e.g. lidocaine patches and anaesthetic creams, capsaicin and dimethyl sulphoxide (DMSO), blocking of sympathetic nervous system (i.e. cervicothoracic (stellate) ganglion blocks) and medications (which is described in details in the background).
Types of outcomes
This review will consider studies that include the following outcome measures: level of pain (mild, moderate, severe – according to the Numeric Rating Scale (NRS), visual analogue scale (VAS) or Likert scale), function limitation, extention of ability to move measured by standardized scale, osteoporosis remission measured with X-ray or CT scan, ligament, muscle and bone dystrophy using standardized screening techniques before and after HBO.
Exclusion criteria will be:
Patients with the CRPS type I. or II. in the atrophic phase of the disease
TYPES OF STUDIES
This review will consider primarily experimental study designs, including parallel and crossover RCTs and quasi-experimental studies. If non-experimental study designs are found, the review will also consider for inclusion epidemiological study designs, including prospective and retrospective cohort studies, case control studies, and analytical cross-sectional studies.
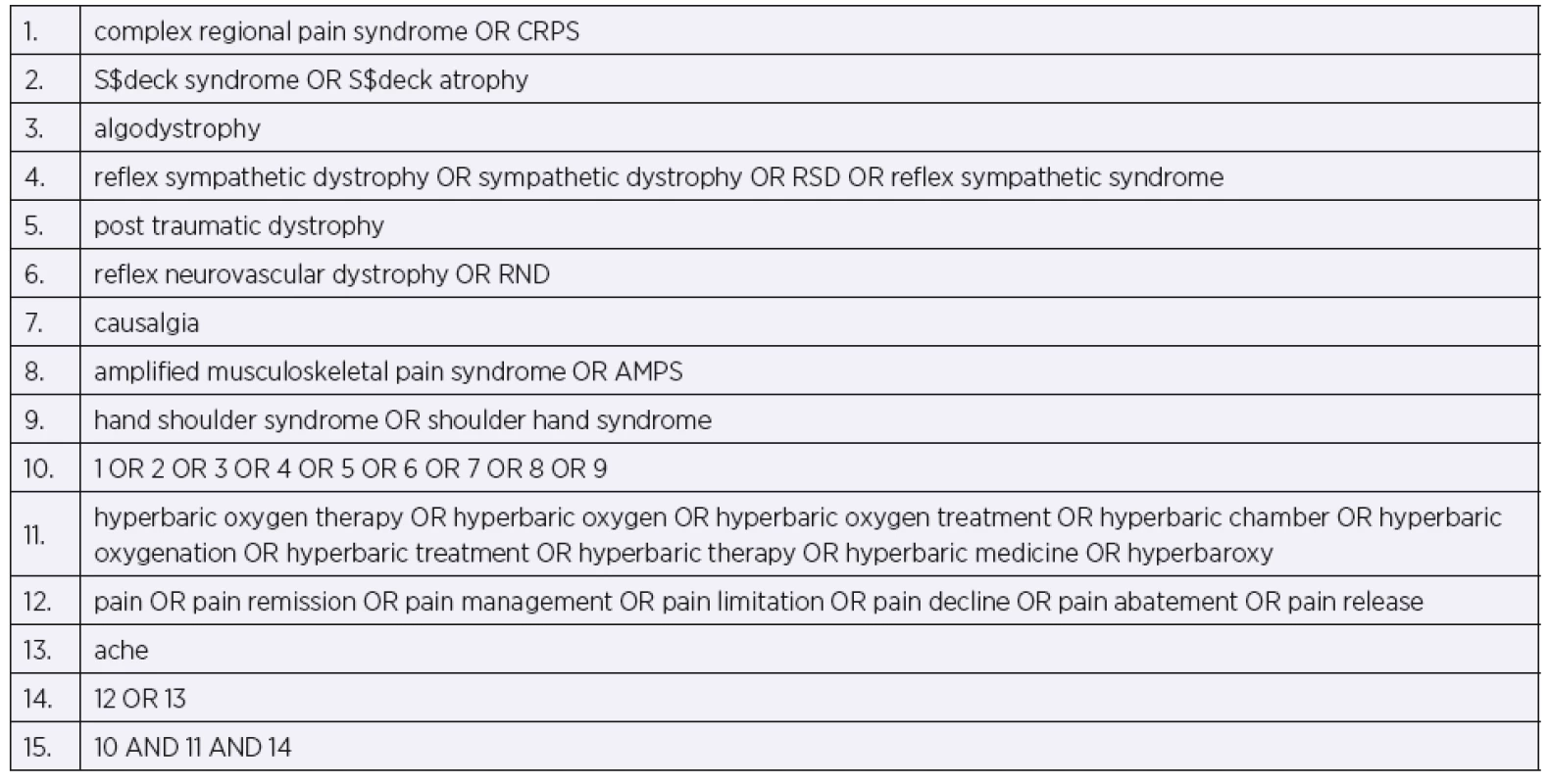
SEARCH STRATEGY
The search strategy aims to find both published and unpublished studies. A three-step search strategy will be utilised in this review. An initial limited search of MEDLINE, Cinahl and EMBASE will be undertaken followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe article. A second search using all identified keywords and index terms will then be undertaken across all included databases. Thirdly, the reference list of all identified reports and articles will be searched for additional studies. Studies published in all possible languages, if they have a title and an abstract in English, will be considered for inclusion in this review. Studies published with no time restriction will be considered for inclusion in this review.
The databases to be searched include: MedLine@Ovid MEDRLINE(R), Biomedica Czechoslovaca, Pedro, EMBASE, Cochrane Central Register of Controlled Trials, Cinahl, Web of Science, Google Scholar, and Scopus
The search for unpublished studies will include: Open Grey, Current Controlled Trials, MedNar, ClinicalTrials.gov., Cos Conference Papers Index
SELECTION PROCESS
In order to select studies for inclusion, two reviewers (DT, MH) will review the literature search results independently in a two-step process. In the first step, the titles and abstracts will be reviewed for eligibility against the inclusion criteria. In the second, the full text of the articles will be obtained and reviewed for consideration of inclusion. A record will be kept of the reason for exclusion against each study. Any disagreements that arise between the reviewers will be resolved through discussion or with a third reviewer (MK) where appropriate. Study authors will be contacted should additional information be required.
ASSESSMENT OF METHODOLOGICAL QUALITY
Papers selected for retrieval will be assessed by two independent reviewers (DT, JK) for methodological validity prior to inclusion in the review using standardized critical appraisal instruments from the Joanna Briggs Institute Meta Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) [36]. Any disagreements that arise between the reviewers will be resolved through discussion, or with a third reviewer (MK). Studies will be not excluded based on the assessment of methodological quality; however, analysis of sensitivity will be performed to evaluate the quality impact.
DATA COLLECTION
Data will be extracted from papers included in the review using the standardized data extraction tool from JBI-MAStARI [36]. The data extracted will include specific details about the interventions, populations, study methods and outcomes of significance to the review question and specific objectives. If there are data missing or incomplete, the reviewers will contact the authors of the primary studies. Two reviewers (DT, JM) will extract data independently. If there is disagreement, a third reviewer (MK) will be involved.
DATA SYNTHESIS
Quantitative data will, where possible, be pooled in statistical meta-analysis using JBI-MAStARI. Effect sizes expressed as odds ratio (for categorical data) or weighted mean differences (for continuous data) and their 95% confidence intervals will be calculated for analysis. If we retrieve homogeneous RCTs, we will not include any other study design, and we will then perform fixed-effects meta-analyses to synthesize the data by pooling the results of included studies. If we do not retrieve homogeneous RCTs, or have to include other study designs, we will perform random-effects meta-analyses. We will pool studies with similar designs, for example, the data from RCTs will not be pooled with data from quasi-randomized trials or non-randomized trials. Initially, clinical heterogeneity will be assessed by determining whether the studies are sufficiently similar to pool in terms of inclusion criteria. If they are clinically homogeneous, statistical heterogeneity will be assessed using the standard x2 test (significance level: 0.1) and I2 statistic, with a value of I2 ≥ 50% indicating significant heterogeneity. If statistical heterogeneity is found, it will be assessed by sensitivity and subgroup analyses. Where statistical pooling is not possible, the findings will be presented in narrative form, including tables and figures to aid in data presentation where appropriate. Where statistical pooling is not possible the findings will be presented in narrative form including tables and figures to aid in data presentation where appropriate.
SUBGROUP ANALYSIS
1. Subgroup analysis will be used for type I. and type II. of the complex regional pain syndrome.
2. Other subgroup analysis will be done for different phase of the disease – inflammatory or dystrophic.
3. Another subgroup analysis will be done for number of exposures:
- 0–10 exposures;
- 11–20 exposures;
- 21 – more.
4. Another subgroup analysis will be used for a different intervention:
- Hyperbaric oxygen therapy versus pharmacological therapy;
- Hyperbaric oxygen therapy versus normal air therapy (placebo).
5. Another subgroup analysis will be used for the age:
- Patients aged 0–18 years;
- Patients aged over 18 years;
- Patients aged over 65 years.
Based on the results and quality of evidence, the tool known as ‘Grading of Recommendation Assessment, Development and Evaluation’ (GRADE) [37] will be used. The quality of evidence will be assessed across the domains of risk of bias, consistency, directness, precision and publication bias. Quality will be assessed as high (further research is very unlikely to change our confidence in the estimate of effect) or moderate (further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate) or low (further research is very likely to have an impact on our confidence in the estimate of effect and is likely to change the estimate) or very low (very uncertain about the estimate of effect).
Conflicts of interest
All the reviewers have no potential conflicts of interest to declare.
Acknowledgements
The project was supported by the institutional support RVO: 61989592.
Do redakce došlo dne 28. 8. 2018.
Do tisku přijato dne 7. 9. 2018.
Adresa pro korespondenci:
PaedDr. Dagmar Tučková, Ph.D.
Ústav veřejného zdravotnictví
Hněvotínská 3
775 15 Olomouc
e-mail: tuckova.dagmar@seznam.cz
Sources
1. Bruehl, S. Complex regional pain syndrome. BMJ, 2015, 351, p. h2730.
2. Allen, G., Galer, B. S., Schwartz, L. Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients. Pain, 1999, 80, 3, p. 539–544.
3. Stanton-Hicks, M., Baron, R., Boas, R., Gordh, T., Harden, N., Hendler, N. et al. Complex Regional Pain Syndromes: guidelines for therapy. The Clinical journal of pain, 1998, 14, 2, p. 155–166.
4. Huygen, F. J., De Bruijn, A. G., De Bruin, M. T., Groeneweg, J. G., Klein, J., Zijlstra, F. J. Evidence for local inflammation in complex regional pain syndrome type 1. Mediators of inflammation, 2002, 11, 1, p. 47–51.
5. Gay, A.-M., Béréni, N., Legré, R. Type I complex regional pain syndrome. Chirurgie de la main, 2013, 32, 5, p. 269–280.
6. Birklein, F. Complex regional pain syndrome. J. neurol., 2005, 252, 2, p. 131–138.
7. Harden, R., Bruehl, S. Introduction and diagnostic conside-rations. Reflex Sympathetic Dystrophy Syndrome Association (RSDSA) Complex Regional Pain Syndrome: treatment guidelines RSDSA Press Milford (CT) 2006, p. 1–11.
8. Mahajan, A., Suri, P., Bardi, G. H., Singh, J., Gandotra, D., Gupta, V. Reflex sympathetic dystrophy syndrome. 2004.
9. De Mos, M., Sturkenboom, M. C., Huygen, F. J. Current understandings on complex regional pain syndrome. Pain Practice, 2009, 9, 2, p. 86–99.
10. Černý, R., Kozák, J. Komplexní regionální bolestivý syndrom. Postgraduální medicína – příloha. Praha, 2005.
11. Köck, F., Borisch, N., Koester, B., Grifka, J. Complex regional pain syndrome type I (CRPS I). Pathophysiology, diagnostics, and therapy. Der Orthopade, 2003, 32, 5, p. 418–431.
12. Emmerová, M., Růžička, J., Hadravský, M., Koudelová, J., Kreuzberg, B., Koudela, K. Příspěvek k problematice Sudeckova syndromu. Intern med pro praxi, 2006, 12, p. 520–530.
13. Giannoudis, P. V., Lasanianos, N. G. Reflex Sympathetic Dystrophy Syndrome. Trauma and Orthopaedic Classifications: Springer; 2015. pp. 533–535.
14. Wong, G. Y., Wilson, P. R. Classification of complex regional pain syndromes. New concepts. Hand clinics, 1997, 13, 3, p. 319–325.
15. Eberle, T., Doganci, B., Krämer, H., Geber, C., Fechir, M., Magerl, W. et al. Warm and cold complex regional pain syndromes Differences beyond skin temperature? Neurology, 2009, 72, 6, p. 505–512.
16. Harden, R. N., Oaklander, A. L., Burton, A. W., Perez, R. S., Richardson, K., Swan, M. et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines. Pain medicine, 2013, 14, 2, p. 180–229.
17. Stašek, M., Řezáč, T., Bébarová, L., Tüdös, Z., Prášil, P., Gabrhelík, T. Komplexní regionální bolestivý syndrom při léčbě ran. Hojení ran, 2013, 7, 2, p. 21–24.
18. Bruehl, S., Harden, R. N., Galer, B. S., Saltz, S., Backonja, M., Stanton-Hicks, M. Complex regional pain syndrome: are there distinct subtypes and sequential stages of the syndrome? Pain, 2002, 95, 1, p. 119–124.
19. Stica, P. Využití hyperbarické oxygenoterapie v léčbě komplexního regionálního bolestivého syndrome I. typu. 18 kongres ČSHLM. Plzeň, 2009.
20. Kiralp, M., Yildiz, Ş., Vural, D., Keskin, I., Ay, H., Dursun, H. Effectiveness of hyperbaric oxygen therapy in the treatment of complex regional pain syndrome. Journal of international medical research, 2004, 32, 3, p. 258–262.
21. De Mos, M., De Bruijn, A., Huygen, F., Dieleman, J., Stricker, B. C., Sturkenboom, M. The incidence of complex regional pain syndrome: a population-based study. Pain, 2007, 129, 1, p. 12–20.
22. Sandroni, P., Benrud-Larson, L. M., McClelland, R. L., Low, P. A. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain, 2003, 103, 1, p. 199–207.
23. O’Connell, N. E., Wand, B. M., McAuley, J., Marston, L., Moseley, G. L. Interventions for treating pain and disability in adults with complex regional pain syndrome an overview of systematic reviews. The Cochrane Library, 2013.
24. Tran, D. Q., Duong, S., Bertini, P., Finlayson, R. J. Treatment of complex regional pain syndrome: a review of the evidence. Canadian Journal of Anesthesia/Journal canadien d’anesthésie, 2010, 57, 2, p. 149–166.
25. Van de Vusse, A. C., Stomp-van den Berg, S. G., Kessels, A. H., Weber, W. E. Randomised controlled trial of gabapentin in Complex Regional Pain Syndrome type 1 [ISRCTN84121379]. BMC neurology, 2004, 4, 1, p. 13.
26. SÚKL Kalcitonin – omezení indikací pro použití. In: léčiv Súpk editor. Kalcitonin – omezení indikací pro použití. Praha: Státní ústav pro kontrolu léčiv, 2011.
27. Bruehl, S., Chung, O. Y. Psychological and behavioral aspects of complex regional pain syndrome management. The Clinical journal of pain, 2006, 22, 5, p. 430–437.
28. Weaver, L. Hyperbaric Oxygen Therapy Indications. North Palm Beach, Florida, USA: Undersea and Hyperbaric Medical Society, 2014.
29. Danesh-Sani, S. A., Shariati-Sarabi, Z., Feiz, M. R. Comprehensive review of hyperbaric oxygen therapy. Journal of Craniofacial Surgery, 2012, 23, 5, p. e483–e491.
30. Sharkey, S. Current indications for hyperbaric oxygen therapy. Adf health, 2000, 1, 2, p. 64–72.
31. Yildiz, S., Uzun, G., Kiralp, M. Z. Hyperbaric oxygen therapy in chronic pain management. Current pain and headache reports, 2006, 10, 2, p. 95–100.
32. Jain, K. K. Textbook of hyperbaric medicine. Springer, 2016.
33. Z K. Sudeckův syndrom. XII konference o hyperbaroxii a potápění. Ostrava1995. pp. 30–33.
34. Tuter, N., Danilov, A., Poliakova, L. The treatment of a complex regional pain syndrome. Zhurnal nevrologii i psikhiatrii imeni SS Korsakova, 1996, 97, 11, p. 33–35.
35. Peach, G. Hyperbaric oxygen and the reflex sympathetic dystrophy syndrome: a case report. Undersea & hyperbaric medicine: journal of the Undersea and Hyperbaric Medical Society, Inc, 1995, 22, 4, p. 407–408.
36. Institute TJB Joanna Briggs Institute Reviewers´Manual: 2014 edition. Adelaide, Australia: The Joanna Briggs Institute, 2014.
37. Munn, Z., Porritt, K., Aromataris, E., Lockwood, C., Peters, M.Summary of Findings Tables for Joanna Briggs Institute Systematic Reviews. Joanna Briggs Institute Reviewers´ Manual: 2014 edition. Adelaide, Australia: The Joanna Briggs Institute, 2016.
38. Hájek, M. Komplexní regionální bolestivý syndrom. In: Hyperbarická medicína. Mladá Fronta 2017, s. 390–399.
Labels
Hygiene and epidemiology Hyperbaric medicine Occupational medicine
Article was published inOccupational Medicine

2018 Issue 3-4-
All articles in this issue
- Eczema of the hands
- Trend in smoking prevalence and providing brief interventions in employees of the Královské Vinohrady Teaching Hospital and Third Faculty of Medicine of Charles University
- Effect of night work on occurrence of cardiovascular diseases in health professionals
- Real effectiveness of respirators in protecting airways
- Risk assessment for employees exposed to vibrations at work in manipulation – expedition storage – Part 1 – Scientific background
- Risk assessment for employees exposed to vibrations at work in manipulation – expedition storage – Part 2 – Results of the study
- Changes in pulmonary fibroblasts respiration in vitro after repeated short-term hyperoxic exposure
- Actual research evidence in effectiveness of hyperbaric oxygen therapy in available chronical indications: overview of systematic reviews
- Lung squeeze and freediving
- Development of an in vitro model to study the effect of hyperbaric oxygen therapy on the antimicrobial effects of selected antibiotics
- Night shift work and cardiovascular diseases
- Telemetric measurement of rats during experimental dives in a hyperbaric chamber – a pilot study
- The effectiveness of hyperbaric oxygen therapy comparing to pharmacological treatment in the patients with complex regional pain syndrome: a systematic review protocol
- Occupational Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Real effectiveness of respirators in protecting airways
- Lung squeeze and freediving
- Eczema of the hands
- Risk assessment for employees exposed to vibrations at work in manipulation – expedition storage – Part 1 – Scientific background
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career