-
Medical journals
- Career
Multiple neuroendocrine tumor of the small bowel: a case report and a review of literature
Authors: Lumír Kunovský 1,2; Milan Dastych 1; Oldrich Robek 2; Roman Svaton 2; Jakub Vlazny 3; Jakub Hustý 4; Michal Eid 5; Karolina Poredska 1; Petr Kysela 2; Zdeněk Kala 2
Authors‘ workplace: Department of Gastroenterology, University Hospital Brno Bohunice, Faculty of Medicine, MU, Brno 1; Department of Surgery, University Hospital Brno Bohunice, Faculty of Medicine, MU, Brno 2; Department of Pathology, University Hospital Brno Bohunice, Faculty of Medicine, MU, Brno 3; Department of Radiology, University Hospital Brno Bohunice, Faculty of Medicine, MU, Brno 4; Department of Hematology, Oncology and Internal medicine , University Hospital Brno Bohunice, Faculty of Medicine, MU, Brno 5
Published in: Vnitř Lék 2018; 64(10): 966-969
Category: Case Reports
Overview
Primary malignant tumors of small bowel constitute only about 1–2% of all gastrointestinal neoplasms. Although neuroendocrine tumors (NETs) are relatively rare, they still represent the second most common malignancy of the small bowel (after adenocarcinoma). Clinical manifestations include abdominal pain, bowel obstruction, diarrhea, weight loss and bleeding. The differential diagnosis of obscure gastrointestinal bleeding can sometimes be challenging for endoscopy as well as for radiology methods. We present the case of an 80-year-old man suffering from severe hypochromic anemia. Routine endoscopic methods did not show any appropriate pathology. Finally, a single ulcerative infiltration of the ileum was diagnosed by capsule endoscopy (CE). CT enterography did not reveal any other lesions. In accordance with a positive chromogranin A, endoscopic and radiologic methods, a suspicion of NET was expressed. During the surgery, 7 lesions were found and a resection of 120 cm of ileum was performed. The histology confirmed a diagnosis of NET grade 1, with a total number of 15 NET lesions in the specimen. The following octreotide scan did not show any residual infiltration. We present a patient with 15 NET lesions in the ileum diagnosed by CE and successfully cured by surgical resection of the ileum.
Key words:
capsule endoscopy – carcinoid syndrome – gastrointestinal carcinoids – neuroendocrine tumor – obscure gastrointestinal bleeding – small bowel – surgery
Introduction
Primary small bowel malignant tumours comprise only 1–2% of all gastrointestinal neoplasms. Neuroendocrine tumours (NETs) represent a relatively rare subgroup of malignant neoplasms. Despite this fact, NETs are the second most common malignant tumours of the small bowel [1–3]. NET can be often asymptomatic for a long time, sometimes can present with obscure gastrointestinal bleeding (OGIT) and the diagnostics can be challenging as for endoscopic as well as radiologic tools [4–7]. An increase of small bowel NETs incidence has been reported recently, not due to a real incidence rise but rather due to better diagnostic methods [6,8,9].
Case report
Our patient is an 80-year-old polymorbid man investigated for a severe anemia (hemoglobin level of 53 g/L). His case history includes chronic ischemic heart disease, heart attack, aortic valve replacement, cardiac rhythm disturbances, diabetes mellitus and prostatectomy for adenocarcinoma.
Esophagogastroduodenoscopy revealed just a mild erosive gastropathy. During colonoscopy, only diverticulosis of the sigmoid colon was diagnosed, and four small polyps were removed by endoscopic polypectomy (tubular adenomas).
Due to persistent anemia, the patient underwent enteroscopy, where no significant pathology was discovered. Subsequently, capsule endoscopy (CE) was performed, finding a 12 × 6 mm isolated ulceration in the ileum, with thickened edges giving the impression of an exulcerated submucosal formation of 2 cm in total (fig. 1a, 1b).
1. a, 1b. CE showing an ulceration with thickened edges of 2 cm in size 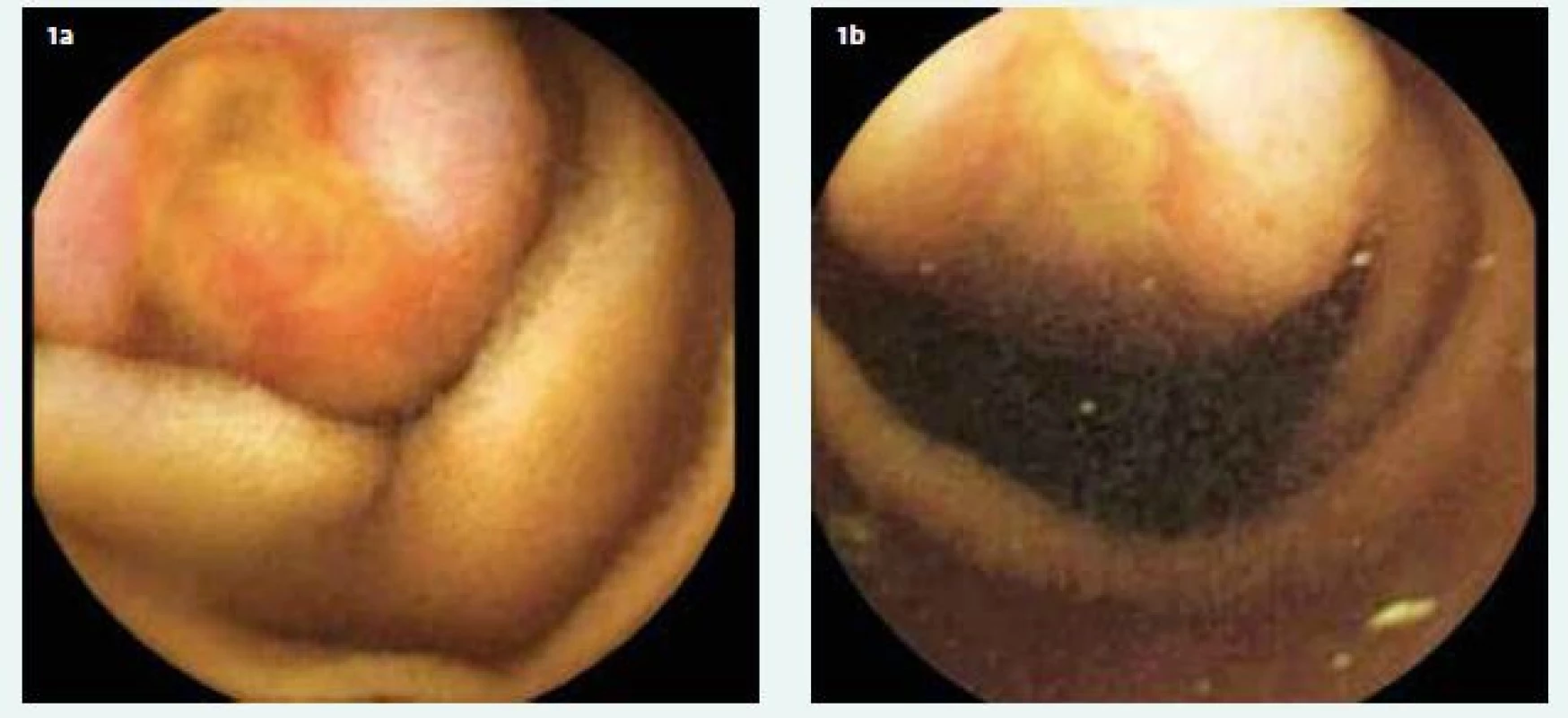
Due to the positive values of chromogranin A (207.3 µg/L, reference range < 50) and the findings of endoscopic and imaging methods – CT enterography (fig. 2a, 2b), we expressed a suspicion of a NET of the small intestine. During surgery (fig. 3), seven suspect rigid small intestine lesions were palpably detected, and a resection of 120 cm of the ileum was performed. According to definitive histology (fig. 4, 5, 6a, 6b), a total of 15 NET grade 1 lesions with the predominance of submucosa and muscularis propria (T3) were found. Metastases were present in 6 regional lymph nodes (total 12 examined lymph nodes). In the postoperative period, a following octreotide scan was performed without residual lesion finding. From an oncological point of view, only observation without subsequent adjuvant oncological treatment will be introduced.
2. a, 2b. Contrast enhanced CT: a (coronal scan) and b (transversal scan) hypervascularised lesion on ileal bowel loop (red arrow) 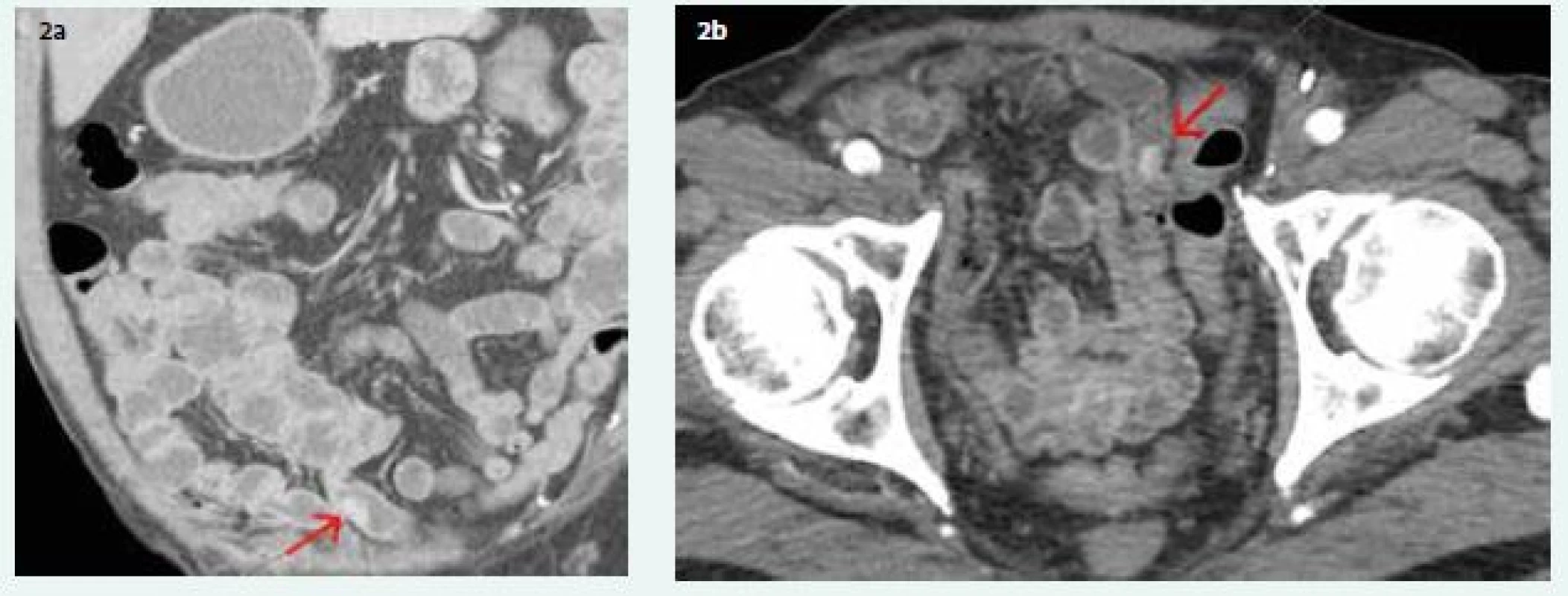
3. Peroperative view of 2 round-shaped lesions 
4. Specimen of ileum after fixation in formaldehyde. Lesions of NET marked by arrows 
5. Histological section: NET infiltrating submucosa of the small bowel wall, HE staining, 200× 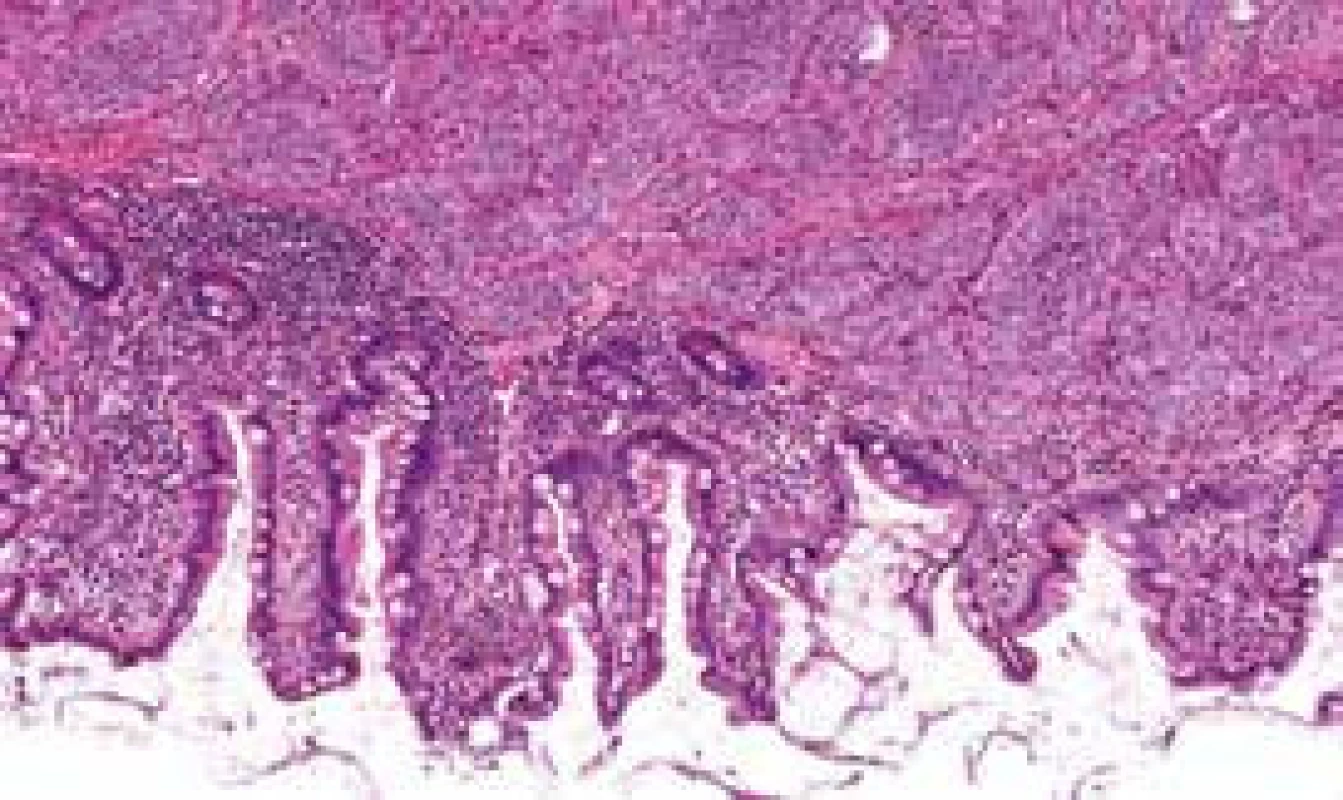
6. a. Histological section: Solid, insular masses of monotonous small round cells positive for chromogranin, immunohistochemical staining, 200× 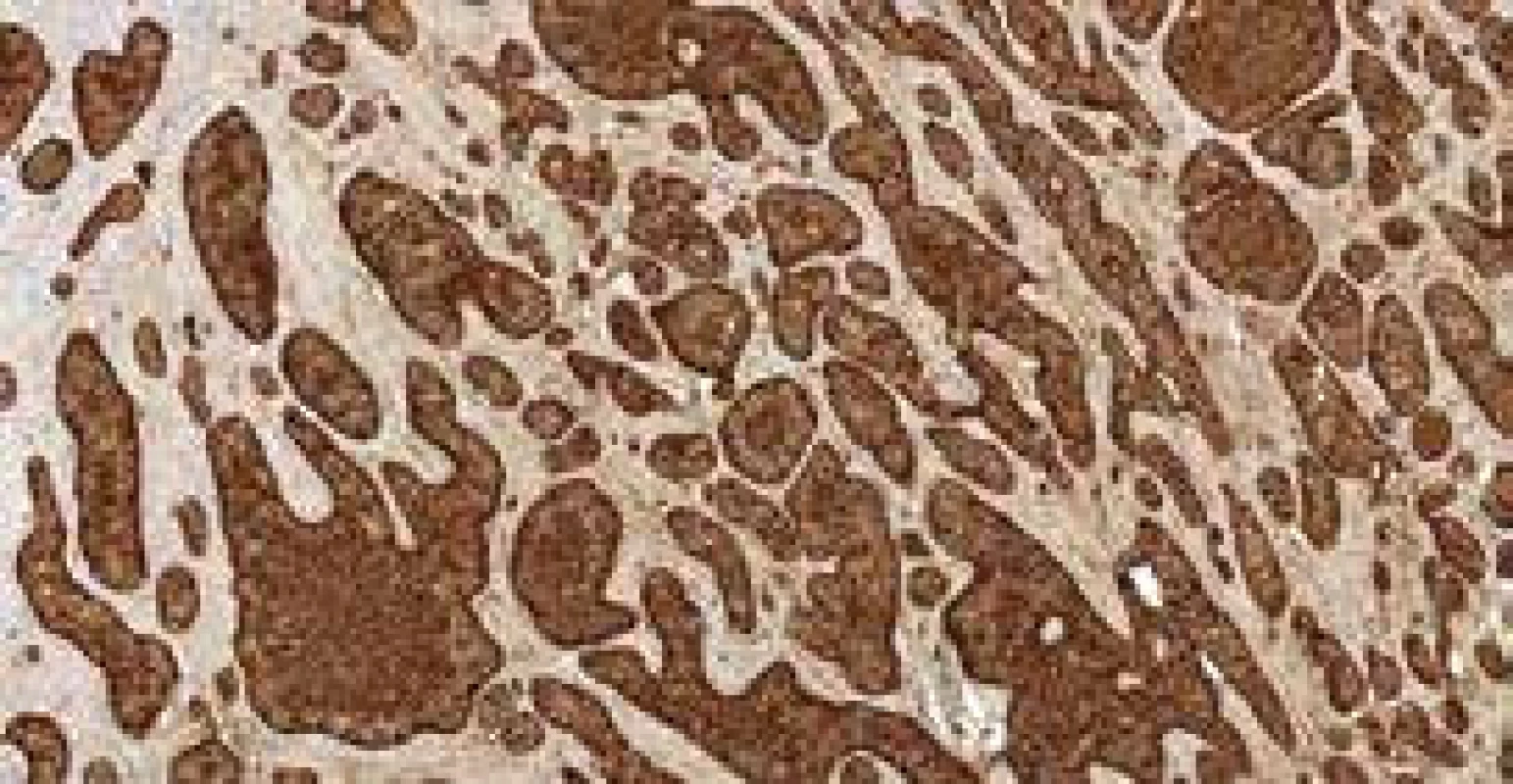
Fig. 6. b. Histological section: Proliferation Ki67 index is less than 2%, 1 mitoses/10 high-power fields, immunohistochemical staining, 200× 
Discussion
NETs located in the duodenum up to 1cm in size can be treated endoscopically and are mostly isolated lesions [10,11]. On the other hand, surgical treatment is recommended for NETs in the jejunoileum. They have a greater propensity to metastasize and NETs in this localization can even form more lesions [2,6,8]. Multiple lesions may be found in up to 40% of cases [8]. Small bowel NETs may initially behave asymptomatically, and even small tumors under 1 cm tend to form lymph node metastases relatively early (in 20–30% of cases). For NETs larger than 2 cm, the risk of metastatic involvement of regional lymph nodes increases to over 80%. With primary tumor size up to 2 cm, the incidence of liver metastases is reported in up to 20% of patients (for sizes greater than 2 cm in more than 40% of patients) [1,5]. The carcinoid syndrome, which occurs in 20–30% of patients with a NET of the small intestine, is almost always (around 95%) associated with the presence of liver metastases [4,6,8].
When diagnosing NETs, their tendency to extraluminal proliferation may be problematic. This was the case with our patient, most of whose lesions tended to infiltrate submucosa and muscularis propria. In the diagnosis of small intestine tumors, CE, double-ballon enteroscopy and CT enterography are usually compared. In comparative studies of these methods in the diagnosis of small intestine tumors, the yield appears to be similar (although in case of NETs, CE has slightly better results) [8,12–15].
On the other hand, a certain disadvantage of CE in the diagnosis of NETs may be their tendency toward extraluminal spreading [5]. The combination of these 3 methods in the diagnosis of OGIB and small intestine tumors [15–19] seems to be ideal. In our case, only one lesion was identically visible on CE and CT enterography. Other lesions were detected by palpation during surgery and from the definitive histology. The following octreotide scan did not reveal any other residual lesions. Therefore there is no indication of systemic treatment.
Even if in our patient one lesion of 2 cm in size and another 14 lesions occurred ranging in size from 0.5 cm to 2 cm, the carcinoide syndrome or liver metastasis were not present. Only positive regional lymph nodes metastases were evaluated in the specimen. There are no data for the adjuvant treatment.
5-year survival rate in patients with NET and the regional lymph node involvement reaches 70–90% after curative surgery with lymphadenectomy [1,4,20].
Conclusion
We present an 80-year-old man with OGIB. In our rare case, a patient with 15 lesions of NET in the ileum was diagnosed by CE and successfully cured by surgical resection of the ileum.
Supported by Ministry of Health, Czech Republic – conceptual development of research organization (FNBr, 65269705).
Petr Kysela, M.D., Ph.D.
Department of Surgery, University Hospital Brno Bohunice, Faculty of Medicine, Masaryk University
Sources
- Bonekamp D, Raman SP, Horton KM et al. Role of computed tomography angiography in detection and staging of small bowel carcinoid tumors. World J Radiol 2015; 7(9): 220–235. Dostupné z DOI: <http://dx.doi.org/10.4329/wjr.v7.i9.220>.
- Zonča P, Peteja M, Richter V et al. Primary malignant small bowel tumors. Rozhl Chir 2016; 95(9): 344–349.
- Němec L, Fabian P, Tomášek J et al. Malignant tumors of the small bowel. Rozhl Chir 2017; 96(6): 252–259.
- Niederle B, Pape UF, Costa F et al. ENETS Consensus Guidelines Update for Neuroendocrine Neoplasms of the Jejunum and Ileum. Neuroendocrinology 2016; 103(2): 125–438. Dostupné z DOI: <http://dx.doi.org/10.1159/000443170>.
- Johanssen S, Boivin M, Lochs H et al. The yield of wireless capsule endoscopy in the detection of neuroendocrine tumors in comparison with CT enteroclysis. Gastrointest Endosc 2006; 63(4): 660–665. Dostupné z DOI: <http://dx.doi.org/10.1016/j.gie.2005.11.055>.
- Scherübl H, Jensen RT, Cadiot G et al. Neuroendocrine tumors of the small bowels are on the rise: Early aspects and management. World J Gastrointest Endosc 2010; 2(10): 325–334. Dostupné z DOI: <http://dx.doi.org/10.4253/wjge.v2.i10.325>.
- Triester SL, Leighton JA, Leontiadis GI et al. A Meta-Analysis of the Yield of Capsule Endoscopy Compared to Other Diagnostic Modalities in Patients with Obscure Gastrointestinal Bleeding. Am J Gastroenterol 2005; 100(11): 2407–2418. Dostupné z DOI: <http://dx.doi.org/10.1111/j.1572–0241.2005.00274.x>.
- Xavier S, Rosa B, Cotter J. Small bowel neuroendocrine tumors: From pathophysiology to clinical approach. World J Gastrointest Pathophysiol 2016; 7(1): 117–124. Dostupné z DOI: <http://dx.doi.org/10.4291/wjgp.v7.i1.117>.
- Margonis GA, Samaha M, Kim Y et al. A Multi-institutional Analysis of Duodenal Neuroendocrine Tumors: Tumor Biology Rather than Extent of Resection Dictates Prognosis. J Gastrointest Surg 2016; 20(6): 1098–1105. Dostupné z DOI: <http://dx.doi.org/10.1007/s11605–016–3135-x>.
- Kim GH, Kim JI, Jeon SW et al. Endoscopic resection for duodenal carcinoid tumors: A multicenter, retrospective study. J Gastroenterol Hepatol 2014; 29(2): 318–324. Dostupné z DOI: <http://dx.doi.org/10.1111/jgh.12390>.
- Kimura T, Muguruma N, Goji T et al. Pedunculated duodenal carcinoid successfully removed by endoscopic resection with endoloop. J Dig Dis 2013; 14(7): 402–404. Dostupné z DOI: <http://dx.doi.org/10.1111/1751–2980.12033>.
- He B, Gong S, Hu C et al. Obscure gastrointestinal bleeding: diagnostic performance of 64-section multiphase CT enterography and CT angiography compared with capsule endoscopy. Br J Radiol 2014; 87(1043): 20140229. Dostupné z DOI: <http://dx.doi.org/10.1259/bjr.20140229>.
- Kysela S, Frajerová D, Hadraba L et al. Adenocarcinoma of the small intestine as an unusual source of hypochromic anemia. Gastroenterol Hepatol 2017; 71(4): 333–336.
- Friedman S. Comparison of capsule endoscopy to other modalities in small bowel. Gastrointest Endosc Clin N Am 2004; 14(1): 51–60. Dostupné z DOI: <http://dx.doi.org/10.1016/j.giec.2003.10.001>.
- Chu Y, Wu S, Qian Y et al. Complimentary Imaging Modalities for Investigating Obscure Gastrointestinal Bleeding: Capsule Endoscopy, Double-Balloon Enteroscopy, and Computed Tomographic Enterography. Gastroenterol Res Pract 2016; 2016 : 8367519. Dostupné z DOI: <http://dx.doi.org/10.1155/2016/8367519>.
- Zhang ZH, Qiu CH, Li Y. Different roles of capsule endoscopy and double-balloon enteroscopy in obscure small intestinal diseases. World J Gastroenterol 2015; 21(23): 7297–7304. Dostupné z DOI: <http://dx.doi.org/10.3748/wjg.v21.i23.7297>.
- Heo HM, Park CH, Lim JS et al. The role of capsule endoscopy after negative CT enterography in patients with obscure gastrointestinal bleeding. Eur Radiol 2012; 22(6): 1159–1166. Dostupné z DOI: <http://dx.doi.org/10.1007/s00330–011–2374–1>.
- Zhang Q, He Q, Liu J et al. Combined use of capsule endoscopy and double-balloon enteroscopy in the diagnosis of obscure gastrointestinal bleeding: meta-analysis and pooled analysis. Hepatogastroenterology 2013; 60(128): 1885–1891.
- Cellier C. Obscure gastrointestinal bleeding: Role of videocapsule and double-balloon enteroscopy. Best Pract Res Clin Gastroenterol 2008; 22(2): 329–340. Dostupné z DOI: <http://dx.doi.org/10.1016/j.bpg.2007.12.006>.
- Srirajaskanthan R, Ahmed A, Prachialias A et al. ENETS TNM Staging Predicts Prognosis in Small Bowel Neuroendocrine Tumours. ISRN Oncol 2013; 2013 : 420795. Dostupné z DOI: <http://dx.doi.org/10.1155/2013/420795>.
Labels
Diabetology Endocrinology Internal medicine
Article was published inInternal Medicine

2018 Issue 10-
All articles in this issue
- Is functional dyspepsia really that frequent?
- Does the time from symptoms onset to treatment impact further development of vein thrombosis in the leg?
- Transient elastography – role in the assessment of the liver disease development
- Some causes of poor adherence to long-term statin therapy and their solution
- Angiotensin-converting enzyme inhibitor-induced angioedema: epidemiology, pathogenesis and management
- Obstructive sleep apnea and dyslipidemia
- CD38 targeted treatment for multiple myeloma
- Fatty pancreas disease: clinical impact
- Treatment of polycythemia vera
- Weber-Christian disease: a case report
- Multiple neuroendocrine tumor of the small bowel: a case report and a review of literature
- Internal Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Fatty pancreas disease: clinical impact
- Treatment of polycythemia vera
- Weber-Christian disease: a case report
- Angiotensin-converting enzyme inhibitor-induced angioedema: epidemiology, pathogenesis and management
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

