-
Medical journals
- Career
Biologic therapy does not affect results of endoscopic balloon dilations in Crohn’s disease patients
Authors: I. Romanko 1,2; M. Bortlík 1,3; D. Ďuricová 1,4; M. Lukáš Jr 1; N. Machková 1; V. Hrubá 1; K. Mitrová 1; M. Lukáš 1,5
Authors‘ workplace: Klinické a výzkumné centrum pro střevní záněty ISCARE I. V. F. a. s., Praha 1; III. interní klinika 1. LF UK a VFN v Praze 2; Interní klinika 1. LF UK a ÚVN Praha 3; Ústav farmakologie, 1. LF UK, Praha 4; Ústav lékařské bio chemie a laboratorní diagnostiky, 1. LF UK v Praze 5
Published in: Gastroent Hepatol 2015; 69(1): 33-37
Category: IDB: Original Article
doi: https://doi.org/10.14735/amgh201533Overview
Patients with Crohn’s disease are at substantial risk of recurrent stenotic complications even after they have been operated on. Endoscopic balloon dilation is an acceptable alternative to surgical therapy in selected cases.
Methods:
We performed a retrospective analysis of results of endoscopic balloon dilations in patients with Crohn’s disease treated in our center. The aim was to assess the efficacy and safety of the balloon dilation as well as the influence of biologic therapy and other factors on results of dilation therapy.Results:
Between May 2007 and December 2013 we performed 220 balloon dilations on 109 Crohn’s disease patients. Technical success (passage through the stricture after dilation) was achieved in 77% and clinical efficacy in 75% of cases. Technical success was associated with significantly longer duration of clinical effect (10 months vs 4.5 months, p < 0.001), and lower risk of surgery (14% vs 29%; p = 0.02). Dilation of anastomotic strictures was also associated with more favorable outcome with respect to the risk of surgery as compared with primary stenosis (11% vs 42%; p < 0.001). Concomitant biologic therapy did not have any effect on clinical effect of dilation and the risk of surgery was also not affected by this treatment. Serious complications were observed in 2% of cases (three cases of bleeding and one perforation).Conclusion:
Balloon dilation is an effective and safe therapeutic method especially in patients with anastomotic strictures. Technical success prolongs clinical efficacy and decreases the risk of surgery. Biological therapy has no effect on the results of dilation therapy.Key words:
Crohn‘s disease – balloon dilation – stenosis – biological therapy
Crohn`s disease (CD) is a chronic inflammatory bowel disease affecting any part of the gut, most frequently an ileocaecal area. In 80% of patients CD evolves into stenosing or perforating type [1,2]. Up to 40 – 55 % of patients have to undergo an intestinal resection within ten years from diagnosis and nearly half of them require repeated surgery within 15 years after the first operation [3].
Endoscopic balloon dilation (EBD) represents an alternative to surgery in selected cases, and currently belongs to one of the most frequently used therapeutic methods in patients with CD. It can be used especially in patients with secondary anastomotic stenoses, however it is also suitable for some primary small or large bowel stenoses [4,5]. On the contrary, terminal ileum or ileocaecal valve stenosis is not an optimal indication for EBD and in these cases the surgical resection should be the method of choice.
For EBD we use balloons introduced through the working channel of the endoscope (through ‑ the ‑ scope or TTS balloon). Stenoses suitable for EBD should not be longer than 4 – 5 cm, with no fistula and/ or abscess [6]. Procedure of dilation, diameter of the balloon, pressure used for dilation, as well as number of dilations during one session vary between authors and depend mainly on actual endoscopic finding (stenosis diameter, presence of inflammatory changes and ulcers, etc.) and experience of the endoscopist. EBD is considered successful when the post‑dilation diameter allows the scope to pass through the stenosis [2,7].
Effect of medical therapy on the efficacy of EBD still remains questionable [8]. Although biological therapy decreases the risk of hospitalization and surgery in CD patients, we are missing a clear proof of positive effect of anti‑TNF antibodies on EBD outcome [9]. Previous study of our group on the cohort of 53 CD (19 treated with biologicals) patients have not shown any positive influence of biological therapy on the duration of clinical effect of EBD. Moreover, patients treated with biologicals in our study had significantly shorter median of symptom relief after EBD as compared to patients treated with conventional medical therapy [10].
The aim of this study was therefore: 1. to assess the short ‑ as well as long‑term effect and safety of EBD; 2. to assess the effect of concomitant biological therapy on EBD outcome; 3. to evaluate the influence of other factors (smoking, localization of stenosis, type of anastomosis, technical success of dilation, etc.) on EBD outcome.
Patients and methods
We retrospectively analyzed efficacy and safety of EBD performed in CD patients at IBD center ISCARE between May 2007 and December 2013. Patients with both anastomotic stenosis and primary – not anastomotic stenosis were included. The medical records were retrieved and the following data were extracted: patients’ demographic characteristics, disease behaviour, details on anti‑TNFa therapy, number and type of previous surgeries and characteristics of stenosis. Furthermore, details on EBD procedure, efficacy and complications were recorded.
Procedure
In our centre EBD is performed either in patients with clinical obstructive symptoms, or because of incidental findings of significant stenosis (inability to pass the scope through the stenosis) during endoscopic examination. Elective EBD is performed after CT or MR enterography was done to evaluate the shape and length of the stricture. We use TTS balloons from Olympus or Boston Scientific Microvasive. Deep sedation using propofol with the assistance of anaesthesiologist is given to all patients. Length of dilation procedure takes from 0.5 to 2 minutes, and can be repeated several times. Maximal balloon pressure depends on the diameter of stenosis and presence of ulcers. EBD is considered technically successful when the scope can be passed through the dilated stricture. Duration of clinical effect (partial or complete relief from obstructive symptoms) is measured until symptoms recur, or surgery is required (strictureplasty, resection).
Statistical analysis
For cohort characteristics we used descriptive statistics for continuous and categorical variables (mean, standard deviation, median, range). To assess effects of various factors on outcome of EBD we used Chi ‑ square test and Fischer`s exact test. For comparison of variables between two groups we used Mann‑Whitney test.
Results
Characteristics of the cohort
We included 109 patients (60 men, 49 women) who had undergone 220 dilations (range 1 – 8). Median age at the time of dilation was 38 years (13 – 75), 53% of patients had obstructive symptoms prior to procedure. Majority of patients had ileal (63%) or ileocolonic (27%) localization. Nineteen percent were treated with biological therapy at the time of EBD. The most common type of anastomosis was end‑to ‑ end anastomosis (59%). Detailed information provided in tab. 1.
1. Characteristics of the cohort. Tab. 1. Charakterisktika souboru pacientů. 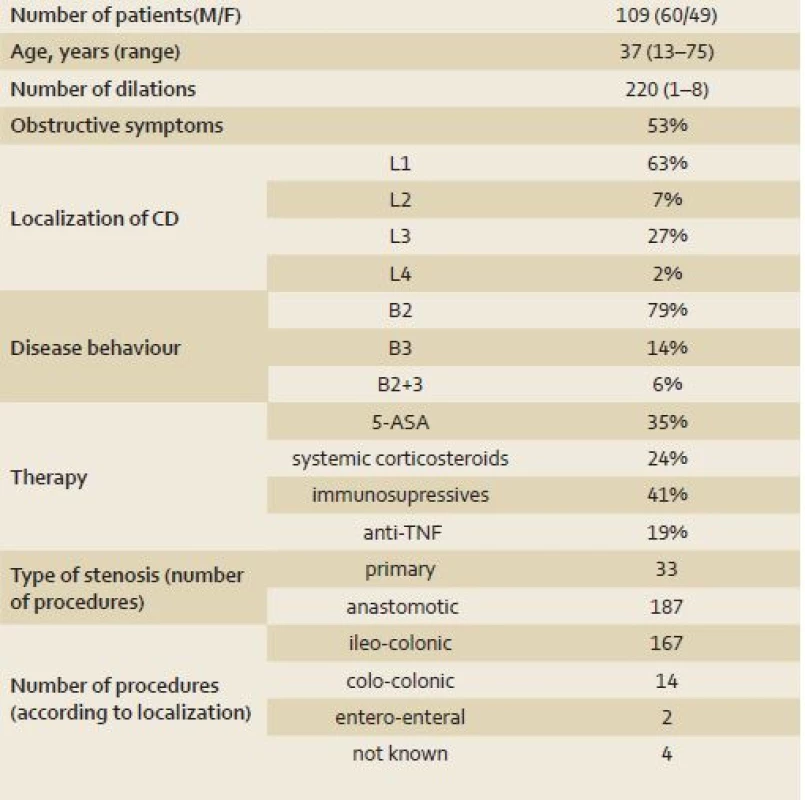
5-ASA – 5-aminosalicylic acid; M – male; F – female; CD – Crohn´s disease. Disease localization and behaviour was classified according to Montreal classification. Efficacy and safety of balloon dilation
Technical success was achieved in 77% of procedures (tab. 2). Seventy ‑ five per cent of dilations (87/ 116) in patients with obstructive symptoms prior to dilation resulted in a relief of their problems with a median duration of symptom‑free interval of 10 months (range: 1 – 59). Technical success of EBD was associated with higher rate of clinical efficacy (86% vs 47%; p < 0.001) as well as with longer duration of symptom relief (mean 10 months vs 4.5 months; p < 0.001). Surgery was eventually necessary in 35 (32%) patients after a median time of nine months (range 1 – 59) since the last EBD.
2. Results of balloon dilations. Tab. 2. Výsledky balonkové dilatace. 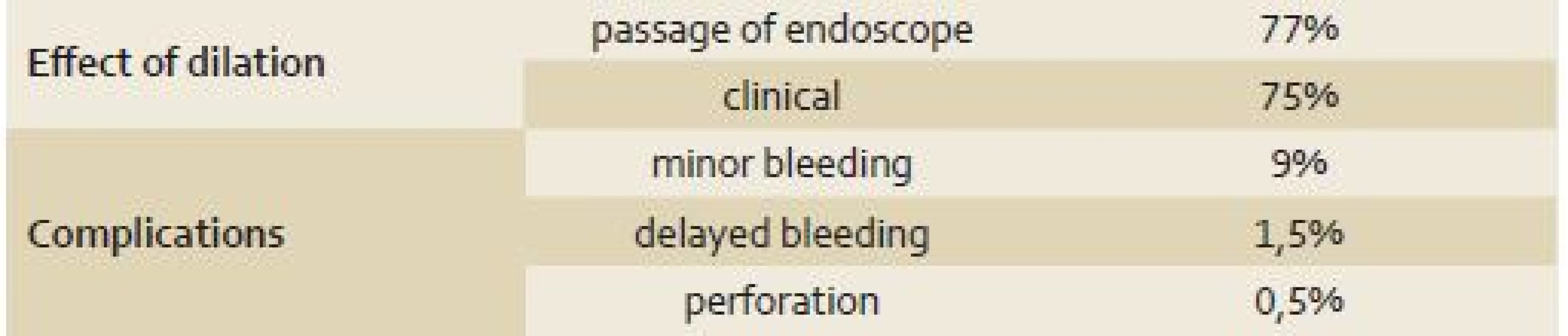
Complications were reported in 23 procedures. Nineteen (9%) dilations were complicated by bleeding immediately after dilation, which were treated endoscopically. Serious complications occurred in four (2%) procedures: delayed bleeding in three patients with a need for blood transfusion in one case and a covered perforation in one patient which was managed by parenterally administrated antibiotics. No surgical intervention was needed.
Effect of biological therapy on EBD outcome and necessity of surgery
Administration of anti‑TNFa therapy (at the time of dilation and at least three months afterwards) did not have any significant effect on EBD outcome. In patients treated with biologics clinical effect of EBD was observed in 83% of cases compared to 81% in patients without such treatment (p = 1.00). Likewise, there was no effect of biological therapy on need for surgery (24% vs 15%; p = 0.17).
Other factors affecting outcome of EBD and necessity of surgery
Type of anastomosis had significant effect on technical success of dilation in favor of end‑to ‑ end compared to end‑to ‑ side anastomosis (89% vs 61%; p = 0.01). On the contrary, duration of effect was significantly longer in patients with end‑to ‑ side anastomosis compared to patients with end‑to ‑ end anastomosis (median 17 months vs 10 months; p = 0.006).
Factors affecting necessity of surgery were localization of stenosis, technical success of EBD and type of anastomosis. Patients with anastomotic stenosis required surgery significantly less often than those with primary stenosis (11% vs 42%; p < 0.001). Only 14% of patients required surgery after successful dilations, compared to 29% of those whose dilation was not successful (p = 0.02). Finally, patients with end‑to ‑ side anastomosis required surgery more frequently than patients with end‑to ‑ end anastomosis (39% vs 7.5%; p = 0.002). Neither age of the patients, nor smoking affected EBD outcome in our cohort.
Discussion
Endoscopic balloon dilation has become an important part of the complex care for CD patients. Frequency of stenosing complications is high and an alternative to surgical resection offers patients an opportunity to postpone, or even avoid repeated resections with an increased risk of short bowel syndrome. In this study we confirm previously published data: EBD is not only effective, but also a safe method with minimal risk of complications. In 220 EBDs we observed only one covered perforation and three significant bleedings. All complications were resolved without surgical intervention and only two patients had to be admitted to the hospital (one case of bleeding and one covered perforation).
Whether EBD is as efficient and safe in primary stenoses as in anastomotic stenoses remains questionable. Primary stenosis, in the majority of cases, affects ileocaecal valve and terminal ileum. In our opinion, such primary ileocaecal stenosis is an indication for surgery (ileocaecal or ileocolonic resection). The main reason is the fact that its length usually exceeds 4 – 5 cm, i.e. the maximal length suitable for EBD, and the curved shape of the lumen in stenotic segment does not allow insertion of the balloon. Nevertheless, in the study of Gustavsson et al. the probability of surgery after EBD in patients with primary and anastomotic stenoses was the same [11]. From a technical and clinical point of view, we consider EBD reasonable for primary stenosis only in cases where stenosis is localized in proximal parts of small intestine, anorectal area or very short stenoses of ileocaecal valve (in order to assess disease extent in terminal ileum).In contrast to findings of Gustavsson et al, the incidence of surgery is significantly higher in primary stenoses compared to anastomotic stenoses in our cohort.
An important issue is the relationship between medical therapy of CD and long‑term outcome of EBD. In clinical practice the majority of patients with significant stenosis obtain intensified medical therapy after EBD, with an expectation of a decrease of inflammation within stenotic segment and prevention of restenosis. However, according to our experience and data from others, such effect is questionable. Conventional medical therapy (mesalazine, corticosteroids, immunosuppressives) have no effect on EBD outcome [10]. In our previous study, we even observed a negative effect of anti‑TNF antibodies on EBD outcome in terms of shortening the duration of EBD clinical effect and symptom‑free period [7]. Van Assche et al did not observe any effect of medical therapy, including biologics, on EBD outcome in a cohort of 138 patients followed for six years [8]. On the contrary, Honzawa et al [12] observed a decreased need for repeated dilations in patients treated with immunosuppressives at the time of dilation, when compared to patients who started immunosuppressives after the first EBD. Our results now confirm that biological therapy has no effect on EBD outcome, and its administration or intensification focused only on treatment of short, isolated stenosis seems to be useless. It should be emphasized that EBD is not only a method for relief of obstructive symptoms, but also enables examination of the gut beyond the stricture. If active inflammation is present there, an intensive therapy, including biologics, is necessary.
In contrast to our previous results, we showed in this study that technical success of dilation (passage of endoscope through the stenosis) positively affects EBD outcome. Patients after successful EBD have longer duration of clinical effect and lower risk of surgery than those with unsuccessful dilation. Most other factors assessed in our study did not have any short ‑ or long‑term effect on EBD outcome or necessity of surgery. Surprisingly, we did not observe a negative effect of smoking, although it is a well known risk factor of complicated CD course and stenosing behavior. Contrary to our results, Gustavsson et al have showed that smokers were at double risk of restenosis after EBD compared to non‑smokers [13].
The main limitation of our study is its retrospective nature. However, we are not aware of any prospective trial on this topic.
In summary, for successful EBD in patients with CD a selection of cases is required in order to increase effectivity and decrease the risk of complications. Most suitable are patients with anastomotic stenoses not exceeding 5 cm in length. The outcome of EBD is affected by technical success of dilation, while type of medical therapy has no significant effect.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE „uniform requirements“ for biomedical papers.
Submitted: 9. 1. 2015
Accepted: 8. 2. 2015
MU Dr. Igor Romanko
Klinické a výzkumné centrum
pro střevní záněty ISCARE I.V.F. a.s.
Jankovcova 1569/ 2c, 170 00 Praha 7
romanko@iscare.cz
Sources
1. Cosnes J, Cattan S, Blain A et al. Long‑term evolution of disease behavior of Crohn ́s disease. Inflamm Bowel Dis 2002; 8(4): 244 – 250.
2. Paine E, Shen B. Endoscopic therapy in inflammatory bowel diseases (with videos). Gastrointest Endosc 2013; 78(6): 819 – 835. doi: 10.1016/ j.gie.2013.08.023.
3. Peyrin‑Biroulet L, Loftus EV Jr, Colombel JF et al. The natural history of adult Crohn‘s disease in population‑based cohorts. Am J Gastroenterol 2010; 105(2): 289 – 297. doi: 10.1038/ ajg.2009.579.
4. Felley C, Vader JP, Juillerat P et al. Appropriate therapy for fistulizing and fibrostenotic Crohn’s disease: Results of a multidisciplinary expert panel – EPACT II. J Crohns Colitis 2009; 3(4): 250 – 256. doi: 10.1016/ j.crohns.2009.06.001.
5. Lewis RT, Maron DJ. Efficacy and complications of surgery for Crohn’s disease. Gastroenterol Hepatol 2010; 6(9): 587 – 596.
6. Hommes DW, van Deventer SJ. Endoscopy in inflammatory bowel diseases. Gastroenterology 2004; 126(6): 1561 – 1573.
7. Bortlík M, Bouzková E, Machková N et al. Postavení endoskopické dilatace v léčbě pooperačních stenóz u nemocných s Crohnovou chorobou. Endoskopie 2010; 19(3 a 4): 121 – 124.
8. Thienpont C, D ́Hoore A, Vermeire S et al.Long‑term outcome of endoscopic dilatation in patients with Crohn ́s disease is not affected by disease activity or medical therapy. Gut 2010; 59(3): 320 – 324. doi: 10.1136/ gut.2009.180182.
9. Costa J, Magro F, Caldeira D et al. Infliximab reduces hospitalizations and surgery interventions in patients with inflammatory bowel disease: a systematic review and meta‑analysis. Inflamm Bowel Dis 2013; 19(10): 2098 – 2110. doi: 10.1097/ MIB.0b013e 31829936c2.
10. Lukáš M, Adamec S, Bortlík M et al. Balonová dilatace pooperačních stenóz u Crohnovy choroby. Endoskopie 2004; 13 : 27 – 31.
11. Gustavsson A, Magnuson A, Blomberg B et al. Endoscopic dilation is an efficacious and safe treatment of intestinal strictures in Crohn`s disease. Aliment Pharmacol Ther 2012; 36(2): 151 – 158. doi: 10.1111/ j.1365 – 2036.2012.05146.x.
12. Honzawa Y, Nakase H, Matsuura M et al. Prior use of immunomodulatory drugs improves the clinical outcome of endoscopic baloon dilation for intestinal stricture in patients with Crohn`s disease. Dig Endosc 2013; 25(5): 535 – 543. doi: 10.1111/ den.12029.
13. Gustavsson A, Magnuson A, Blomberg B et al. Smoking is a risk factor for recurrence of intestinal stricture after endoscopic dilation in Crohn`s disease. Aliment Pharmacol Ther 2013; 37(4): 430 – 437. doi: 10.1111/ apt.12176.
Labels
Paediatric gastroenterology Gastroenterology and hepatology Surgery
Article was published inGastroenterology and Hepatology
2015 Issue 1-
All articles in this issue
- News in 2015
- Not only anti-TNF for IBD patients
- Recommended surgical treatment methods in patients with idiopathic infl ammatory bowel dis eases – part 1: pre-operative preparation
- Eradication of perianal fistulas in IBD patients using the Advancement Flap method and risk factors associated with poor healing
- Vedolizumab in the therapy of ulcerative colitis patients
- Topical treatment of inflammatory bowel diseases
- The importance of fecal calprotectin in the diagnostics and treatment of inflammatory bowel diseases
- Immunoablative therapy and autologous hematopoietic stem cell transplantation in a patient with aggressive Crohn’s disease refractory to medical therapy
- A practical contribution to the diagnostics and treatment of focal nodular hyperplasia and adenomas in the liver from the perspective of a hepatologist, radiologist, pathologist and surgeon
- Short-term results of the treatment of superficial neoplastic lesions of the stomach using endoscopic submucosal dissection
- Small intestinal bacterial overgrowth syndrome
- Exviera, Viekirax
- Nutricia enteral nutrition products for children
- New members of the editorial board
- Calling for cooperation
- VIII. Beskydy Endoscopic Workshop
- Biologic therapy does not affect results of endoscopic balloon dilations in Crohn’s disease patients
- Gastroenterology and Hepatology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- A practical contribution to the diagnostics and treatment of focal nodular hyperplasia and adenomas in the liver from the perspective of a hepatologist, radiologist, pathologist and surgeon
- Small intestinal bacterial overgrowth syndrome
- Topical treatment of inflammatory bowel diseases
- Eradication of perianal fistulas in IBD patients using the Advancement Flap method and risk factors associated with poor healing
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

