-
Medical journals
- Career
Bloodless surgery and gynecological patients among Jehovah’s Witnesses
Authors: Kudela M. 1,3; Pilka R. 1; Dzvincuk P. 1; Marek R. 1; Klementova O. 2
Authors‘ workplace: Department of Obstetrics and Gynecology, Faculty of Medicine and Dentistry, Palacky University and University Hospital, Olomouc, Czech Republic 1; Department of Anesthesiology, Faculty of Medicine and Dentistry, Palacky University and University Hospital, Olomouc, Czech Republic 2; Department of Health Care Sciences, Faculty of Humanities, Tomas Bata University in Zlin, Zlin, Czech Republic 3
Published in: Ceska Gynekol 2021; 86(2): 110-113
Category:
doi: https://doi.org/10.48095/cccg2021110Overview
Objective: The aim of this research is to present our experiences with the surgical treatment of gynecological patients among Jehovah’s Witnesses. Moreover, the medical, moral, and ethical problems in this regard have been highlighted. Methods: 75 Jehovah’s Witnesses patients were operated on for various benign and malignant gynecological diseases between 2007 and 2018. All of these patients were operated on according to the rules of blood-sparing surgery. Results: The operations were assessed according to the diagnosis, mode of surgery, estimated blood loss, and disease outcome. Excessive blood loss did not occur during any of these operations, and the estimated blood loss for the same procedure was 10 to 550 mL. Conclusion: Jehovah’s Witnesses gynecological patients is a group of high-risk patients because they refuse to undergo blood transfusion. Nevertheless, the principles of blood-sparing surgery should be applied to not only Jehovah’s Witnesses patients but also to all patients in general. Even if a blood transfusion is the last resort to solve issues pertaining to excessive blood loss during complicated operations, the said procedure always carries certain risks. Therefore, blood transfusion should be performed only on rare occasions. Jehovah’s Witnesses patients categorically refuse blood transfusion even if it is the only way to save one’s life. Even though the legislation of the Czech Republic deals with this problem, there are other moral and ethical aspects that need to be addressed in this regard.
Keywords:
bloodless surgery – Gynecologic surgery – Jehovah’s Witnesses – legislation – moral and ethical problems
Introduction
The surgical treatment of Jehovah’s Witnesses (JW) is only a marginal matter compared to that of the majority of the population. Nevertheless, the Church of Jehovah’s Witnesses has almost eight million followers around the world, and approximately 13,000 JW reside in the Czech Republic. The most well-known and debatable principle of their faith is the refusal of blood transfusions [1–3].Apart from the associated medical problems, there are other moral, ethical, and legislative aspects of this issue. The legislation of the Czech Republic in accordance with that of the European Union gives patients the right to refuse the suggested treatment that is against their will or religion [14]. On the other hand, doctors have the same right to refuse treatment that would pose a high risk of a patient dying due to excessive blood loss, mainly if it is not an emergency. Even though the properly formulated and signed patients’ informed consent forms clear doctors of the legal consequences in the event of the patients’ death, it does not relieve them of their own moral responsibility. The doctors who refuse to operate on JW patients should not be denounced for the lack of courage or unwillingness to bear this risk. However, one should appreciate the surgeons who are willing to take the same risk even if they do not fully agree with the reasons for which JW patients refuse blood transfusion.
Material and methods
Between 2007 and 2018, 75 JW patients were operated on for various gynecological diseases at the Department of Gynecology and Obstetrics at the University Hospital in Olomouc. These were primarily minor gynecological procedures. However, a few extensive radical operations for malignant gynecological tumors were also performed. All of these operations were performed by a team of four skilled surgeons who operated according to the rules and principles of blood-sparing surgery (BSS).
Results
The results of this study have been presented in Tab. 1.
1. Diagnosis, operation and blood loss (2007–2018).
Tab. 1. Diagnostika, operace a ztráta krve (2007–2018).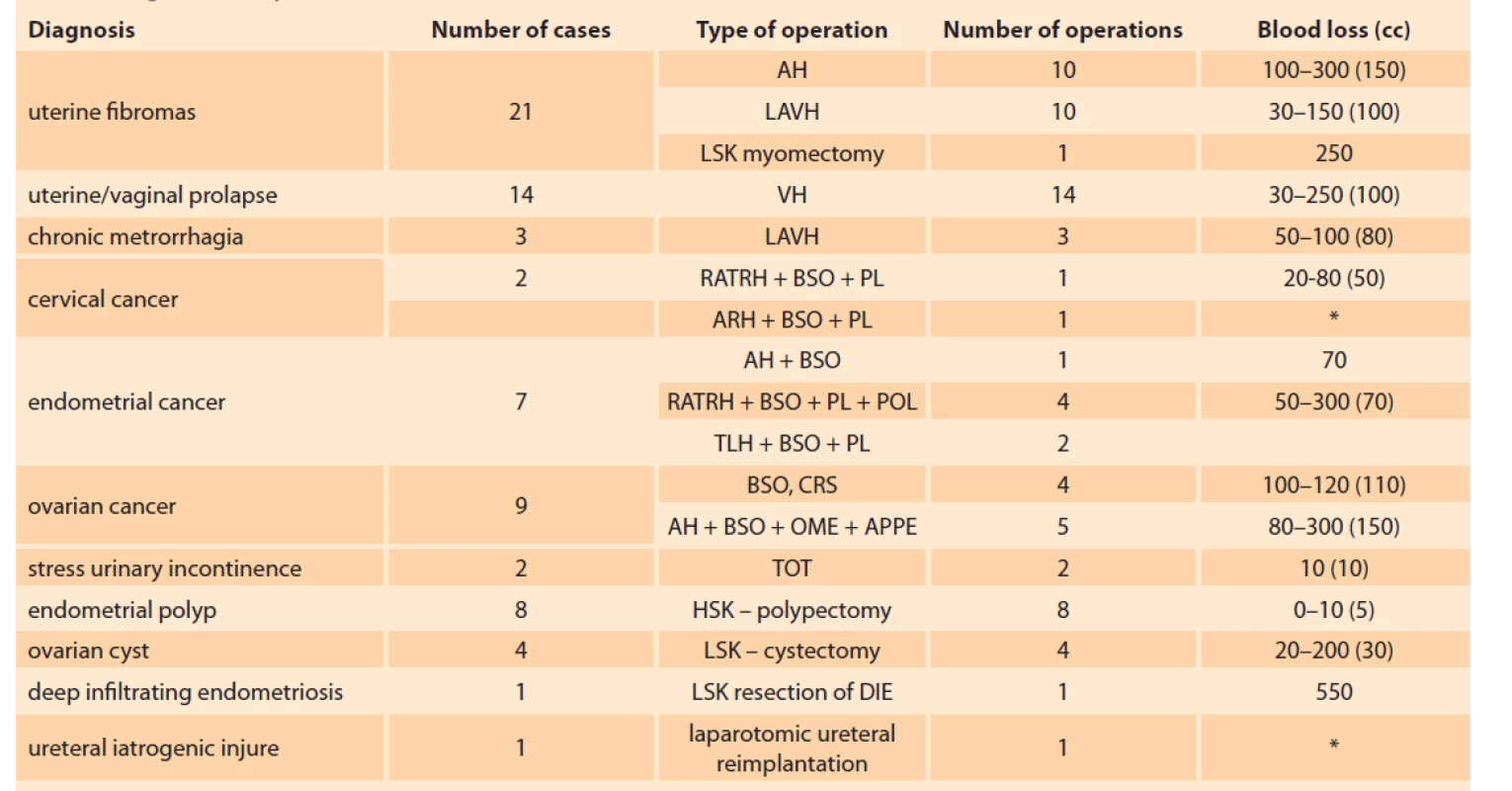
AH – abdominal hysterectomy, APPE – appendectomy, ARH – abdominal radical hysterectomy, BSO – bilateral salpingo-oophorectomy, CRS – cytoreductive surgery, HSK – polypectomy-hysteroscopis polypectomy, LAVH – laparoscopic assisted vaginal hysterectomy, LSK cystecomy – laparoscopic cystectomy, LSK myomectomy – laparoscopic myomectomy, LSK resection of DIE – laparoscopic resection of deep infi ltrating endometritis, OME – omentectomy, PL – pelvic lymphadenectomy, POL – paraaortic lymphadenectomy, RATRH – roboticly assisted total radical hysterectomy, TOT – tension free vaginal tape, VH – vaginal hysterectomy
AH – abdominální hysterektomie, APPE – appendektomie, ARH – abdominální radikální hysterektomie, BSO – bilaterální salpingo-ooforektomie, CRS – cytoreduktivní chirurgie, HSK polypectomy – hysteroskopická polypektomie, LAVH – laparoskopicky asistovaná vaginální hysterektomie, LSK cystectomy – laparoskopická cystektomie, LSK myomectomy – laparoskopická myomektomie, LSK resection of DIE – laparoskopická resekce hluboké endometriózy, OME – omentektomie, PL – pánevní lymfadenektomie, POL – paraaortální lymfadenektomie, RATRH – roboticky asistovaná totální radikální hysterektomie, TOT – vaginální tahu prostá transobturatorní páska, VH – vaginální hysterektomie
* surgical procedure performed at Urology Department – blood loss not known
* chirurgický zákrok provedený na urologickém oddělení – není známa ztráta krveNo instances of excessive blood loss, which necessitated blood transfusion, were observed for all of the operations that were performed.
Discussion
The primary principle concerning safe bloodless surgery (BS) is a thorough preoperative evaluation of the concerned disease’s extent and the assessment of the patient’s general condition for the proposed operation [5]. It is even more crucial if the said operation is, on one hand, the most effective or most reliable mode of treatment but, on the other hand, other non-surgical treatment modalities are also available. It mainly addresses the patients with malignant tumors in advanced stages of the respective disease. The radical operations performed on such patients are always associated with the risk of excessive bleeding. Thus, it is irresponsible to perform surgeries in such cases. The surgeon must always assess the extent of the disease and the possible consequences of such an operation. It is not an issue of “courage” but that of the responsible assessment of all of the risks and benefits relating to such an operation. Failure of such a surgery, along with its possible fatal consequences, would not only lead to the patient’s death but also result in immense remorse for the surgeon. Fortunately, there are only a few overconfident surgeons who boast of their ability to manage all possible dangerous complications, and they like to “parade” their surgical skills in this manner.
Nowadays, although blood transfusion is regarded to be a safe procedure, it always carries certain health risks, and there are economic considerations in this matter as well [6–8]. Several recommendations and rules have been proposed concerning the way to perform BSS. Proper BSS techniques primarily aim to not only control bleeding but also prevent it [9–11]. Today, the majority of surgical procedures are performed without the risk of heavy bleeding and the need for blood transfusion. Even cesarean sections (CS), which are always accompanied by some amount of bleeding, can be performed in such a way that may reduce blood loss to the minimal extent. Cooperation and coordination between obstetricians with invasive radiologists is a typical example of CS performed in case of placenta previa accreta [12]. Preoperative catheterization and balloon obstruction/ embolization of the internal iliac arteries may largely reduce blood loss. Another example of BSS is robotic surgery performed on patients suffering from gynecological malignant tumors. This kind of surgery evidently reduces blood loss in comparison to the classical ones [12].
The rules and principles of BSS should be applied not only in the case of JW patients but for all patients. Responsible surgeons always operate on all of their patients according to the same BSS rules. They should not rely on the fact that the concerned patient has “sufficient blood reserves” and that in case of emergencies, the option to perform blood transfusion is always available [11,13].
In all cases, collaboration between the surgeon and anesthetist is indispensable. The latter must always assess patients’ general medical conditions prior to the operation itself. Doing so is especially crucial with all JW patients. During an operation, anesthetists have to monitor and/ or control the patients’ vital signs and manage possible blood loss by means other than blood transfusion. It is obvious that anesthetists and surgeons must hold similar attitudes toward the management of JW patients [5].
Conclusion
In this study, it was noted that gynecological patients among JW refuse blood transfusion. Therefore, in case of necessary surgery, they have to be operated on according to the rules of bloodless surgery. Nevertheless, the principles of blood-sparing surgery should be applied to not only JW patients but also to all patients in general. Even if blood transfusion is the last resort to solve the issue of excessive blood loss during complicated operations, it always carries certain risks. Therefore, the technique of blood transfusion should be employed only on rare occasions. Our experiences with a group of 75 JW patients, who were operated on in our department, have been presented in this study. Even though the legislation deals with how to manage such patients who refuse blood transfusion, there are other moral and ethical aspects that must be addressed in this regard.
Submitted/ Doručeno: 25. 1 2021
Accepted/ Přijato: 15. 2. 2021
Prof. Milan Kudela, MD, PhD
Department of Obstetrics and Gynecology
Faculty of Medicine and Dentistry
Palacky University and University Hospital
I. P. Pavlova 6
775 20 Olomouc
Czech Republic
Publication ethics: The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Publikační etika: Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Conflict of interests: The authors declare they have no potential conflicts of interest concerning the drugs, products or services used in the study.
Konflikt zájmů: Autoři deklarují, že v souvislosti s předmětem studie/ práce nemají žádný konflikt zájmů.
Sources
1. Ringnes HK, Hegstad H. Refusal of medical blood transfusions among Jehovah’s Witnesses: emotion regulations of the dissonance of saving and sacrificing life. J Relig Health 2016; 55(5): 1672–1687. doi: 10.1007/ s10943-016-0236-5.
2. Sagy I, Jotkowitz A, Barski L. Reflections on cultural preference and internal medicine: the case of Jehovah’s Witnesses and the changing thresholds for blood transfusions. J Relig Health 2017; 56(2): 732–738. doi: 10.1007/ s10943-016-03 53-1
3. Yorozu T. Jehovah’s Witness patients. Masui 2010; 59(9): 1149–1152.
4. Záleská D. Právní podmínky respektování práva na odmítnutí krevní transfuze. Moderní Gynek Porod 2009; 18(4): 648–655.
5. Belaouchi M, Romero E, Mazzinari G et al. Management of massive bleeding in a Jehovah’s Witness obstetrics patient: the overwhelming importance of a pre-established multidisciplinary protocol. Blood Transfus 2016; 14(6): 541–544. doi: 10.2450/ 2016.0229-15.
6. Nagarsheth NP, Sasan F. Bloodless surgery in gynecologic oncology. Mt Sinai J Med 2009; 76(6): 589–597. doi: 10.1002/ msj.20146.
7. Shander A, Hofmann A, Ozawa S et al. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion 2010; 50(4): 753–765. doi: 10.1111/ j.1537-2995. 2009.02518.x.
8. Shander A, Javidroozi M, Perelman S et al. From bloodless surgery to patients blood management. Mt Sinai J Med 2012; 79(1): 56–65. doi: 10.1002/ msj.21290.
9. Dumousset E, Chabrot P, Rabischong B et al. Preoperative uterine artery embolization (PUAE) before uterine fibroid myomectomy. Cardiovasc Intervent Radiol 2008; 31(3): 514–520. doi: 10.1007/ s00270-005-0342-3.
10. Pafko P, Čepický P. Rozhovor s prof. MU Dr. P. Pafkem, DrSc. Moderní Gynek Porod 2009; 18(4): 643–647.
11. Rayburn WF. Prevention and management of complications from gynecologic surgery. Obstet Gynec Clinics 2010; 37(3): 427–436.
12. Shiroki R, Maruyama T, Kusaka M et al. Robot-assisted laparoscopic partial nephrectomy using daVinci S-surgical system for localized renal tumor: report of initial five cases. Nihon Hinyokika Gakkai Zasshi 2011; 102(5): 679–685. doi: 10.5980/ jpnjurol.102.679.
13. Simou M, Thomakos N, Zagouri F et al. Non-blood medical care in gynecological oncology: a review and update of blood conservation management schemes. World J Surg Oncol 2011; 9 : 142. doi: 10.1186/ 1477-7819-9-142.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicine
Article was published inCzech Gynaecology
2021 Issue 2-
All articles in this issue
- Role of umbilical interleukin-6, procalcitonin and C-reactive protein measurement in the diagnosis of fetal inflammatory response syndrome
- A new instrument to personalize ovarian stimulation: results of the CERES study after using a novel gonadotropin – follitropin delta
- Results of treatment of gestational trophoblastic neoplasia in the Slovak Republic in the years 1993–2017
- Analysis of selected perinatological indicators in the Slovak Republic in the years 2007–2018
- Giant breast fibroadenoma in pregnancy
- Obstetric anal sphincter injury and anal incontinence
- Current possibilities in the prevention and therapy of ovarian hyperstimulation syndrome
- Quality of life and sexuality in women with urinary incontinence
- Fetal lower urinary tract obstruction: a current overview of intrauterine diagnosis and treatment
- Solved problems of reproductive medicine in the Czech Republic 2020
- Bloodless surgery and gynecological patients among Jehovah’s Witnesses
- Czech Gynaecology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Current possibilities in the prevention and therapy of ovarian hyperstimulation syndrome
- Giant breast fibroadenoma in pregnancy
- Obstetric anal sphincter injury and anal incontinence
- A new instrument to personalize ovarian stimulation: results of the CERES study after using a novel gonadotropin – follitropin delta
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

